Abstract
This study describes deep sedations performed for painful procedures completed in the emergency department at an academic tertiary care hospital during an 18-month period. One hundred consecutive cases were retrospectively reviewed to describe indications, complications, procedural lengths, medication dosing, and safety of these sedations. Propofol and etomidate were the preferred agents. We found that there were relatively few complications (10%), with only 2 of these (2%) being major complications. All complications were brief and did not adversely affect patient outcomes. This data further demonstrate the safety profile of deep sedation medications in the hands of emergency physicians trained in sedation and advanced airway techniques.
INTRODUCTION
Once only the purview of anesthesiologists and critical care specialists, deep sedative medications have been used in the emergency department (ED) for the last decade. The use of these medications has stemmed from the understanding that many procedures in the ED are extremely painful and that minimal to moderate sedation leads to inadequate management of the patient's pain. To this end, several studies have been completed using deep sedative medications such as propofol and etomidate. Their use has been shown to be safe and effective for procedural sedation within the ED.1–18 However, many residency-trained and board-certified emergency physicians are still unable to use these medications because of local hospital policies or regulations forbidding anything greater than “conscious” or moderate sedation. The American Society of Anesthesiologists' practice guidelines state, “Because sedation/analgesia constitutes a continuum, practitioners…intending to administer deep sedation should be able to rescue patients who enter a state of general anesthesia. Therefore…the consultants strongly agree with the immediate availability (1–5 min away) of an individual with advanced life support skills (eg tracheal intubation, defibrillation, and use of resuscitation medications) for moderate sedation and in the procedure room itself for deep sedation.”19 Since tracheal intubation is a basic skill of the emergency physician, it is reasonable and appropriate that deep sedation be considered an essential emergency physician skill. This study will contribute further support to the literature by describing deep sedation used by emergency medicine physicians in an academic medical center ED over the course of 18 months.
METHODS
After obtaining institutional review board approval and waived consent, we performed a retrospective review of deep sedations performed in the ED over the course of 18 months. The records for this review were obtained through a search of the departmental sedation log and the electronic medical records for this time period. Sedation levels were considered deep sedation from the providers' documentation as such in the medical record. The total number of deep sedations performed during this time period was 100 and there were no charts excluded from this review. The only medications used for deep sedation in the ED during this time period were propofol and etomidate. All sedations occurred under the direct supervision of an emergency medicine residency-trained or board-certified emergency physician. Data were obtained by 2 of the authors by using a standardized data retrieval form with the data points defined before the review process began. They independently reviewed the electronic medical records, sedation notes, nursing flow sheets, and paper records when available. As determined by the protocol, all missing data were given worst case numbers. For instance, if the end of the procedure was not documented, but the time back to baseline mental status was recorded, we labeled the end of the procedure as the time back to baseline with the understanding that this would most likely make our procedural lengths appear longer than in reality. Data were recorded on an Excel (Microsoft Corp, Redmond, Washington) spreadsheet by using a code list that was generated to protect private health information. The data were analyzed using SPSS (SPSS Inc, Chicago, Illinois).
Complications were defined as major or minor. Major complications were defined as apnea, oxygen saturation levels less than 80% at any time, oxygen saturation levels less than 90% for greater than 5 minutes, aspiration, dysrhythmia, unanticipated admission, need for bag-valve-mask (BVM) ventilation, or need for intubation. Minor complications were defined as oxygen saturation levels less than 90% for less than 5 minutes, vomiting without aspiration, need for airway manipulation such as jaw thrust or nasal trumpet insertion, a requirement for increased oxygen delivery, transient blood pressure decrease, or myoclonus (although it is a known side effect of etomidate).
RESULTS
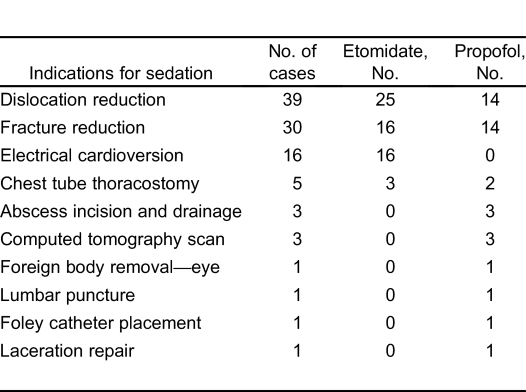
Of the 100 consecutive deep sedation cases reviewed, etomidate was used in 60 of the cases and propofol in the other 40 cases. Demographic features differed between the 2 groups. Patient age ranged from 11 to 85 years (mean, 41 years) in the etomidate group, and 2 to 73 years (mean, 21.9 years) in the propofol group. Mean weight demonstrated a nearly 30-kg difference between the propofol (58.6 kg; range, 10.6–110 kg) and etomidate (86.6 kg; range, 32–150 kg) groups. The indications for sedation in the 2 groups are displayed in Table 1.
Table 1.
Indications for use of deep sedatives.
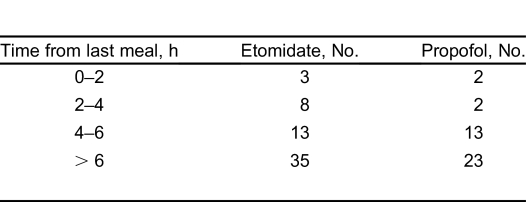
Most patients (84%) had fasted for more than 4 hours before sedation (Table 2). Five patients (5%) had fasted for less than 2 hours and 10 (10%) had fasted between 2 and 4 hours. Of those sedations completed on individuals fasting less than 4 hours, there were no episodes of vomiting or aspiration. One major and 1 minor complication occurred in the group fasting less than 4 hours. The major complication involved a patient who had a last meal between 2 and 4 hours before the sedation and required less than 1 minute of BVM ventilation for an oxygen desaturation to 90%. No vomiting or aspiration occurred and intubation was not necessary. This patient had an ankle dislocation for which the benefits of timely relocation were considered greater than the potential risk of aspiration. The minor complication involved a brief systolic blood pressure drop of 20% in a patient who had also fasted between 2 and 4 hours. There was 1 patient for whom time from last meal was not documented. There were no complications in those individuals fasting less than 2 hours.
Table 2.
Fasting data.
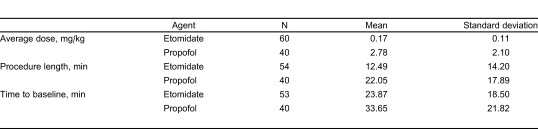
The average dose of the drugs, as well as mean procedural length and mean time to return to baseline mentation, are shown in Table 3. For the 60 etomidate cases, there were 6 missing data points for procedural length and 7 missing data points for time to baseline mentation. These missing data points were omitted from analysis as we were unable to find any useful associated times (ie, discharge time, procedure end time, or any other documentation specifying a return to baseline mentation). There were no missing data points for cases involving propofol. This relatively thorough collection of data points was the result of specific physician and nursing sedation notes, checklists, and electronic medical records used to record data. These notes specifically mandate the recording of the time of the last meal, complications as previously described, and interventions performed for sedation or airway issues such as increased oxygen delivery, airway manipulation, respiration assistance with BVM, or use of reversal agents. Furthermore, vital signs are recorded electronically into a nursing flow sheet. Length of procedure, however, is not a mandated data item in the notes.
Table 3.
Dosing, procedure length, and sedation length.
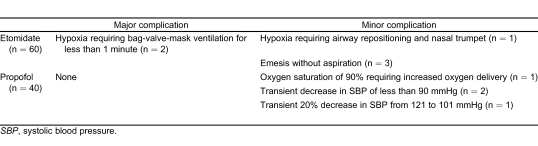
The complications for each of the medications are listed in Table 4. There was a 10% complication rate (6 of 60 cases) noted in those patients receiving etomidate. Two of these (3.3%) were considered major complications because they required BVM ventilation, but each episode lasted less than 1 minute. The remaining 4 (6.7%) were minor complications, including 1 that required only airway repositioning and nasal trumpet insertion with subsequent resolution of hypoxia. This patient's oxygen saturation dropped to 89% for less than 10 seconds and no other complications occurred. The final 3 minor complications involved emesis, with 1 case occurring during the procedure and the other 2 occurring in the postprocedural period. In all 3 of these cases, there was no aspiration and all nausea was resolved with antiemetics.
Table 4.
Complications for each medication.
There was a 10% complication rate (4 of 40 cases) for patients receiving propofol. There were no major complications. There were 4 (10%) minor complications. One involved increasing the oxygen delivery from 4-L oxygen by nasal cannula to a nonrebreather mask for an oxygen saturation of 90% that “quickly improved” without any other time specified. The other 3 minor complications were transient decreases in systolic blood pressure (SBP). Two patients had SBPs less than 90 mmHg and 1 had a 20% drop in SBP from the initial measurement, dropping from 121 to 101 mmHg. The 2 patients with SBP drops below 90 mmHg required normal saline boluses (1,000 mL and 700 mL), while the third (20% SBP reduction) required no intervention.
DISCUSSION
In July 2005, the emergency physicians at our institution were granted the privilege to perform deep sedation for emergent and urgent procedures within the ED. Emergency physicians and nurses were trained on the proper approach to deep sedation and the details of the deep sedative agents. We recommended that our physicians use an initial dose of etomidate of 0.1 mg/kg for sedation. We also developed a propofol-dosing schedule unique to the literature. In an attempt to decrease the percentage of respiratory depression events discussed in the literature with 1.0 to 2.0 mg/kg initial boluses of propofol, we required a dosing protocol beginning with a 0.75 mg/kg bolus of propofol, followed by 0.5 mg/kg boluses every 1 to 3 minutes as needed. We found that an average of 0.17 mg/kg of etomidate was used per sedation. Most sedations were initially started with a 0.1 mg/kg bolus, followed by 0.05 mg/kg boluses as needed. We used an average of 2.78 mg/kg of propofol (approximately 5 separate boluses) per sedation.
The indications for sedation in our population are similar to those of other studies and include both painful and anxiety-provoking procedures (Table 2). Our physicians used etomidate exclusively in patients in need of electrical cardioversion. Fracture and dislocation reductions were also common indications for sedation. Both drugs were used in these situations and the literature indicates no preference, although etomidate may have a lower rate of procedural success and causes a greater incidence of myoclonus.18
Our review demonstrates that most of our deep sedations were completed on patients who were fasting for more than 4 hours, but about 15% were completed on patients with food intake within 4 hours. To maximize patient safety, emergency physicians ask about last food intake, but in reality there are no data to support a specified period of fasting. The American College of Emergency Physicians' guideline on procedural sedation states, “Recent food intake is not a contraindication for administering procedural sedation and analgesia, but should be considered in choosing the timing and target level of sedation.”20 Given the potentially significant morbidity and mortality associated with aspiration, the timing of last meal intake should be considered for each situation, with the risk and benefits based on the urgency of the potential procedure. Using guidelines made for nonemergent, elective operative procedures is impractical and potentially harmful by delaying timely care in an emergent setting. Green et al21 recently published a consensus-based clinical practice advisory regarding fasting and emergency department sedation. This advisory attempts to elucidate target levels of sedation depth and timing in relation to fasting status and individual patient risk factors. This article will likely define the standard of practice for emergency medicine; however, as stated in their practice advisory, “it is expected that emergency physicians will at times appropriately deviate from it according to individualized judgment and unique clinical circumstances.”21
When measuring procedural length and time to baseline mentation for the 2 medications, there was a significant difference in time for these 2 variables. Mean procedure time with etomidate was 12.5 minutes and the time to baseline was 23.9 minutes. Propofol use was associated with lengthier procedure times, with a mean time of 22.1 minutes and an increased time to baseline mentation of 33.7 minutes. The reason for this is unknown, but we suspect there are 2 primary reasons for this difference. First, the patient demographics are quite different, with younger, lighter patients receiving propofol. This patient selection may indicate that the emergency physicians chose propofol for the young person with a forearm fracture, which takes a longer period of time to reduce and cast, while choosing etomidate for the older patient with tenuous vital signs in need of a quick cardioversion. Second, our reduced dosing algorithm for propofol (0.75 mg/kg initial bolus, followed by 0.5 mg/kg boluses) probably caused the time to adequate sedation to increase. Our times for both etomidate and propofol were longer than reported in the literature. This is most likely due to the retrospective nature of the study. We effectively chose to make these times longer by using sedations that had missing data points. When the specific “end-of-procedure” or “back-to-baseline” times were not recorded, we erred with the potentially longer rather than shorter time period. In some cases, for instance, we used the time the patient was discharged from the ED as the time for the end of the procedure and the return to baseline mentation because no other information was available. Additionally, procedure length in our study was determined by measuring the time from when the first sedative agent was given to the time the procedure was documented as finished. Most values in the literature use medication induction times, not administration times, which were not documented in our charts. For this reason we could not compare our times to those in the literature.
For propofol, our data indicate that we have fewer episodes of respiratory depression than reported in the literature, with only 1 case (2.5%) requiring an increase in supplemental oxygen. Reported values for propofol-induced hypoxia appear to range from 5% to 50%.15–17 Apnea has been noted to occur in about 4% of cases. A recent study showed an increase in supplemental oxygen in 5.5% of propofol sedations and in BVM use in 4.6%.18 There has been only 1 reported case requiring intubation.15 That patient was subsequently extubated after 32 minutes with no apparent adverse outcome. We had no reported episodes of apnea or BVM use in our sample.
Our rate of hypotension with propofol sedations (7.5%) falls within the range quoted in the literature of 3.5% to 12%.15–17 These episodes were brief and resolved within a short period of time or with only a small amount of intravenous fluids. While hypotension in our patients did not appear clinically significant, caution should be taken when using propofol as a sedative agent in patients who may not be hemodynamically stable. Similar considerations should be made with adjuvant medications that may lower blood pressure, such as fentanyl. Finally, care should be taken not to administer propofol too quickly, as hypotension is more likely to occur. Administering each dose within 45 to 60 seconds is the preferred method. In the etomidate sedations performed at our center, we noted a 10% overall complication rate. Five percent of the cases involved minor hypoxia, defined as a pulse oximeter reading measuring less than 90%. This complication rate is less than the rates cited in the literature, with oxygen desaturation occurring in 10% to 20% of cases.10 Of those 3 cases, 2 resolved with BVM ventilation and the last resolved with airway repositioning and nasal trumpet insertion. There were no intubations required for these episodes. A recent trial comparing propofol and etomidate described the use of BVM and airway repositioning in etomidate sedations to be 3.8% and 13.3%, respectively.18
The other complication of etomidate noted in our study was vomiting. One case occurred during the procedure and 2 cases, postprocedurally. These were not associated with notable aspiration. Our emesis complication rate of 7.5% with etomidate falls within the range reported in the literature, which is approximately 2% to 8%.22
LIMITATIONS
There are several limitations to this study. The principal limitation is the retrospective nature of the study. Retrospective reviews are fraught with inadequacies due to lack of controls, lack of randomization, inaccuracies in documentation, incomplete documentation, as well as a potential bias to not report adverse events. We describe differences between propofol and etomidate only in the descriptive sense because there was no direct comparison between these 2 medications. This study had a relatively small sample size, although on par for most studies published on sedation. Concurrent use of analgesics was not standardized among patients and could have interfered with the results of the study.
CONCLUSION
In conclusion, both etomidate and propofol appear safe for use in our ED setting when used by board-certified or residency-trained emergency physicians for a variety of ED procedures. The complication rates with these agents were less than or equal to those reported in the literature. Because such complications are well within the scope of practice of emergency physicians, they were recognized and treated without adverse outcomes. Both medications are noted to induce respiratory depression, although seemingly less with propofol in our reduced dosing regimen. Propofol carries a higher risk of hypotension, and therefore should be used with caution in select patients.
Footnotes
Supervising Section Editor: Brandon K. Wills, DO, MS
Volume 12, no. 4 : XXXX 2011
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The opinions and assertions contained herein are the private views of the author and should not be construed as official or as reflecting the views of the Department of Army or the Department of Defense.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
- 1.Ruth WJ, Burton JH, Bock AJ. Intravenous etomidate for procedural sedation in emergency department patients. Acad Emerg Med. 2001;;8:13–18. doi: 10.1111/j.1553-2712.2001.tb00539.x. [DOI] [PubMed] [Google Scholar]
- 2.American College of Emergency Physicians. Clinical policy: evidence-based approach to pharmacologic agents used in pediatric sedation and analgesia in the emergency department. Ann Emerg Med. 2004;;44:342–377. doi: 10.1016/j.annemergmed.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Coll-Vinent B, Sala X, Fernandez C, et al. Sedation for cardioversion in the emergency department: analysis of effectiveness in four protocols. Ann Emerg Med. 2003;;42:767–772. doi: 10.1016/s0196-0644(03)00510-9. [DOI] [PubMed] [Google Scholar]
- 4.Dickinson R, Singer AJ, Carrion W. Etomidate for pediatric sedation prior to fracture reduction. Acad Emerg Med. 2001;;8:74–77. doi: 10.1111/j.1553-2712.2001.tb00558.x. [DOI] [PubMed] [Google Scholar]
- 5.Hunt GS, Spencer MT, Hays DP. Etomidate and midazolam for procedural sedation: prospective, randomized trial. Am J Emerg Med. 2005;;23:299–303. doi: 10.1016/j.ajem.2005.02.042. [DOI] [PubMed] [Google Scholar]
- 6.Vinson DR, Bradbury DR. Etomidate for procedural sedation in emergency medicine. Ann Emerg Med. 2002;;39:592–598. doi: 10.1067/mem.2002.123695. [DOI] [PubMed] [Google Scholar]
- 7.Miner JR, Martel ML, Meyer M, et al. Procedural sedation of critically ill patients in the emergency department. Acad Emerg Med. 2005;;12:124–128. doi: 10.1197/j.aem.2004.08.054. [DOI] [PubMed] [Google Scholar]
- 8.Burton JH, Bock AJ, Strout TD, et al. Etomidate and midazolam for reduction of anterior shoulder dislocation: a randomized, controlled trial. Ann Emerg Med. 2002;;40:496–504. doi: 10.1067/mem.2002.126607. [DOI] [PubMed] [Google Scholar]
- 9.Keim SM, Erstad BL, Sakles JC, et al. Etomidate for procedural sedation in the emergency department. Pharmacotherapy. 2002;;22:586–592. doi: 10.1592/phco.22.8.586.33204. [DOI] [PubMed] [Google Scholar]
- 10.Falk J, Zed PJ. Etomidate for procedural sedation in the emergency department. Ann Pharmacother. 2004;;38:1272–1277. doi: 10.1345/aph.1E008. [DOI] [PubMed] [Google Scholar]
- 11.Bahn EL, Holt KR. Procedural sedation and analgesia: a review and new concepts. Emerg Med Clin N Am. 2005;;23:503–517. doi: 10.1016/j.emc.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Miner JR, Biros MH, Seigel T, et al. The utility of the bispectral index in procedural sedation with propofol in the emergency department. Acad Emerg Med. 2005;;12:190–196. doi: 10.1197/j.aem.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Guenther E, Pribble CG, Junkins EP, Jr, et al. Propofol sedation by emergency physicians for elective pediatric outpatient procedures. Ann Emerg Med. 2003;;42:783–791. doi: 10.1016/s0196-0644(03)00634-6. [DOI] [PubMed] [Google Scholar]
- 14.Bassett KE, Anderson JL, Pribble CG, et al. Propofol for procedural sedation in children in the emergency department. Ann Emerg Med. 2003;;42:773–782. doi: 10.1016/s0196-0644(03)00619-x. [DOI] [PubMed] [Google Scholar]
- 15.Frazee BW, Park RS, Lowery D, et al. Propofol for deep procedural sedation in the ED. Am J Emerg Med. 2005;;23:190–195. doi: 10.1016/j.ajem.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Burton JH, Miner JR, Shipley ER, et al. Propofol for emergency department procedural sedation and analgesia: a tale of three centers. Acad Emerg Med. 2006;;13:24–30. doi: 10.1197/j.aem.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Frank LR, Strote J, Hauff SR, et al. Propofol by infusion protocol for ED procedural sedation. Am J Emerg Med. 2006;;24:599–602. doi: 10.1016/j.ajem.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 18.Miner JR, Danahy M, Moch A, et al. Randomized clinical trial of etomidate versus propofol for procedural sedation in the emergency department. Ann Emerg Med. 2007;;49:15–22. doi: 10.1016/j.annemergmed.2006.06.042. [DOI] [PubMed] [Google Scholar]
- 19.American Society of Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;;96:1004–1017. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 20.American College of Emergency Physicians. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2005;;45:177–196. doi: 10.1016/j.annemergmed.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Green SM, Roback MG, Miner JR, et al. Fasting and emergency department procedural sedation and analgesia: a consensus-based clinical practice advisory. Ann Emerg Med. 2007;;49:454–461. doi: 10.1016/j.annemergmed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 22.Di Liddo L, D'Aneglo A, Nguyen B, et al. Etomidate versus midazolam for procedural sedation in pediatric outpatients: a randomized controlled trial. Ann Emerg Med. 2006;;48:433–440. doi: 10.1016/j.annemergmed.2006.03.004. [DOI] [PubMed] [Google Scholar]