Abstract
Intracranial fungal granulomas are rare and of the histologically verified granulomas, Aspergillus spp. is the commonest causative fungal pathogen. Most of the reported large series of aspergillus granulomas are from countries with temperate climate like India, Pakistan, Sudan, and Saudi Arabia. In contrast to disseminated aspergillosis that occurs in immunosuppressed individuals, most of the intracranial aspergillus granulomas are reported in immunocompetent individuals. The temperature, humidity, high spore content in the atmosphere during ploughing, and occupation as agricultural worker are implicated in the pathogenesis. The sinocranial spread is the most common route of intracranial extension. Extracerebral firm fibrotic lesions and skull base lesions are common. Extensive fibrosis and large number of multinucleated giant cells are the characteristic histological features and these pathological features have therapeutic relevance.
1. Introduction
Fungal infections of the central nervous system (CNS) are more frequently reported in the last few decades mostly due to increase in the population at risk, increased awareness, and better diagnostic modalities [1–4]. However, in the recent years there has been increase in the number of CNS fungal infections in immunocompetent individuals [2–12].
Fungi are ubiquitous in nature but have low virulence and cause disease usually when the host defenses are compromised. The fungi enter the CNS by hematogenous route from the systemic focus, or by contiguous spread from paranasal sinuses (PNS), ear or skull bone; or by direct inoculation during trauma or surgical procedure [1–5]. The pathology depends upon the route of spread, host immunity, and type of fungus, hyphae, or yeast.
The fungi may involve any part of the neuroaxis, and the pathology includes meningitis, encephalitis, abscess, granuloma, and vasculitis with associated infarction and hemorrhage and aneurysmal formation [1–4, 13]. The type of pathology, to some extent, determines the presenting clinical manifestations. This paper will discuss the experience with intracranial Aspergillus granuloma.
2. Epidemiology
The incidence of CNS fungal infections parallels the incidence of systemic fungal infections. The estimated annual incidences of invasive fungal infections caused by Aspergillus species are 12–34 [17]. The reported incidence of CNS involvement associated with invasive aspergillosis is about 4–6% [18]. Intracranial Aspergillus granulomas are rare space occupying intracranial lesions [2–4, 7, 9, 11, 13, 16–21] and most of the reported large series are from countries with temperate climate like India, Pakistan, Sudan, and Saudi Arabia [2–4, 6–8, 10, 12–14, 16–26].
Among the intracranial fungal granulomas, Aspergillus granuloma is the most commonly reported granuloma [2–4, 13, 14, 20–25] (Table 1). The prevalence of intracranial fungal mass lesions in major neurosurgical centers in India is around one to two per years [27], and Aspergillus spp. is the commonest causative fungal pathogen accounting for 56% to 69% of the intracranial fungal mass lesions [2, 19, 20], whereas it was the causative fungus in 5% of the fungal mass lesions in the series from USA [28] (Table 2).
Table 1.
Intracranial Aspergillus granulomas.
| Kak et al. 1989 [14] | Camarata et al. 1992 [15] | Naim-Ur-Rahman et al. 1996 [16] | Murthy et al. 2001 [7] | Alrajhi et al. 2001 [6] | Siddiqui et al. 2004 [8] | Sundaram et al. 2006 [2] | |
|---|---|---|---|---|---|---|---|
| Number | 62 | 13 | 9 | 21 | 23 | 35 | 130 |
| Age in years | 12–48 | 26–66 | 19–65 | 9–. 61 | 14–74 | 5–75 | |
| M: F | NA | NA | 1 : 08 | 10 : 06 | 14 : 09 | 23 : 02 | 1.8 : 1 |
| Predisposing Factors | Nil | Nil | Nil | DM-2 | DM-4 | Nil | Nil |
| Route of spread | Sino-orbital 10 Hematogenous 52 |
Sinocranial 9 Hematogenous 4 |
Sinocranial 9 | Sinocranial 16 | Sinocranial 9 | Sinonasal 35 | Sinocranial 103 Hematogenous 20 Others 7 |
| Pathology | Granulomas 28 Disseminated 34 |
Granulomas 12 Disseminated 01 |
Granulomas 9 | Granulomas 16 Disseminated 5 |
Granulomas 23 | NA | Granulomas 68 |
| Culture | 9 | NA | — |
A. flavus 4 A. fumigatus 2 |
A. flavus 15 A. fumigatus 2 |
15 |
A. flavus 10 A. fumigatus 5 A. niger 2 A. terreus 1 Sterile 3 |
NA: Not available, DM: Diabetes Mellitus.
Table 2.
Intracranial fungal granuloma: series from temperate climate.
| Anandi et al. 1993 [25] | Santosh et al. 1996 [3] | Dubey et al. 2005 [20] | Sundaram et al. 2006 [2] | |
|---|---|---|---|---|
| n | 4/41 | 15/65 | 40 | 74/130 |
| Occupation | NA | Agricultural worker | NA | Agricultural worker, Manual labourer |
| Organism | Aspergillus (4) |
Aspergillus 10 Cryptococcus 2 Phaeohyphomycosis 3 |
Aspergillus 25 Cryptococcus 3 Phaeohyphomycosis 4 Zygomycosis 7 Candidiasis 1 |
Aspergillus 68 Cryptococcus 1 Phaeohyphomycosis 1 Zygomycosis 1 Candidiasis 2 Mixed 1 |
n: Number of cases, NA: Not Available.
3. Pathogenesis
Aspergillus spp. are the most clinically significant moulds and are ubiquitous throughout the world. They are present in soil, water, decaying vegetation, and organic debris. A. fumigatus causes most disease followed by A. flavus and A. terreus. A. flavus is the commonest agent when the infection extends from PNS to CNS [1–4].
Brain is remarkably resistant to fungal infections due to the abundant blood supply and also due to the relatively impermeable blood-brain barrier. Despite the fact that the brain and subarachnoid space are protected by anatomic and functional barriers, under special conditions and immune system abnormalities, fungal pathogens breach these barriers [29]. Invasive disease is seen mostly in patients who are significantly immunocompromised: patients with prolonged neutropenia, hematological malignancies or advanced AIDS, and hematopoietic stem cell transplant and solid organ transplant [30, 31]. However, Aspergillus granulomas in countries with temperate climates are most commonly reported in immunocompetent individuals [2, 7, 13].
Aspergillus moulds enter the CNS by hematogenous route from the systemic focus, mostly from the lung or by contiguous spread from paranasal sinuses (PNS), ear or skull bone or by direct inoculation during trauma or surgical procedure [1–5]. The sinocranial form of CNS aspergillosis is often reported from countries with temperate climate [2, 7, 13]. In countries with temperate climate, the temperature and humidity favor the growth of the fungus. Ploughing during agriculture works or construction activities results in aerosolization of number of spores into the environment.
High spore content in the atmosphere exposes the agriculture workers and workers in the construction activity to inhale the fungal spores.
The spores are colonized in the lungs, nose, PNS, mastoid air cells, and ear canal. Closed cavity and anaerobic atmosphere promote growth of the fungus. There may be local altered immunity which promotes the mucosal invasion of the fungus [1–4]. The immunopathogenesis of CNS fungal infections remains incompletely studied, with most of the knowledge coming from studies on experimentally infected animals. The activation of brain resident cells such as microglia, astrocytes, and endothelial cells combined with relative expression of immune-enhancing and immune-suppressing cytokines and chemokines may play a determinant role in immunopathogenesis [29].
4. Pathology
Mostly these lesions, because of the sinocranial spread of the infection, are extraparenchymal and skull base in location. Skull base location includes anterior and middle cranial fossae, orbit, orbital apex, cavernous sinus, and rarely posterior fossa (Figure 1). Rarely these lesions can be primarily intraparenchymal, involving frontal and temporal lobes [19, 21]. The location of the lesions probably explains the clinical syndromes. Histologically the granulomas show dense fibrosis and an infiltrate of lymphocytes, plasma cells, and mononuclear cells. The multinucleate giant cells are foreign body type and contain slender septate, acute angle branching hyphae of Aspergillus spp. The extracerebral granulomas differ from intraparenchymal granulomas in having extensive fibrosis [19–21]. Aspergillus granuloma on haematoxylin and eosin staining sometimes may be mistaken for tuberculous granuloma. However, the prominence of multinucleated giant cells with admixture of neutrophils, plasma cells and eosinophils and relatively less number of epitheloid cells differentiates tuberculous granuloma from Aspergillus granuloma. Good scanning of the biopsy may reveal fungal hyphae within giant cells.
Figure 1.
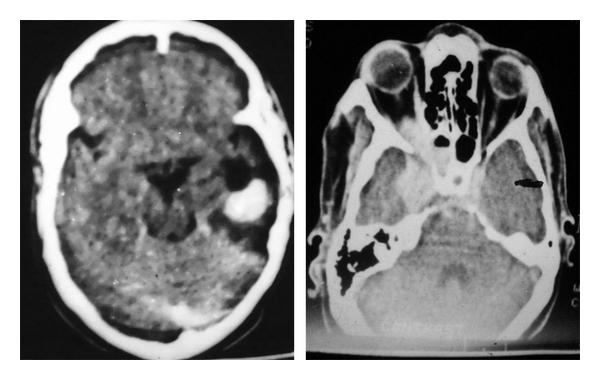
Contrast CT scans showing densely enhancing left temporal intraparenchymal Aspergillus granuloma (a) and enhancing mass lesion in the ethmoid sinuses, right orbital apex, right extraparenchymal temporall fossa and left cavernous sinus skull base Aspergillus granuloma (b).
Gomori's methenamine silver (GMS) and Periodic Acid Schiff (PAS) stains demonstrate the slender septate hyphae with acute angle branching of the Aspergillus spp. in Aspergillus granuloma [19–21] (Figure 2). The extensive fibrosis observed in the extraparenchymal, sinocranial Aspergillus granulomas has therapeutic relevance. Extensive fibrosis does not allow effective penetration of systemically administered antifungal agents. Thus these lesions need extensive radical excision to achieve cure [16, 19]. The other approach to achieve effective therapeutic concentration of the antifungal agents will be intralesional administration of the antifungal agents by Ommaya reservoir [16, 19]. The pathology of haematogenous dissemination to CNS, because of angioinvasive character of Aspergillus, includes ischemic infarction and haemorrhage, and the pathology in the sinocranial aspergillosis is characterized by well-formed granuloma [2].
Figure 2.
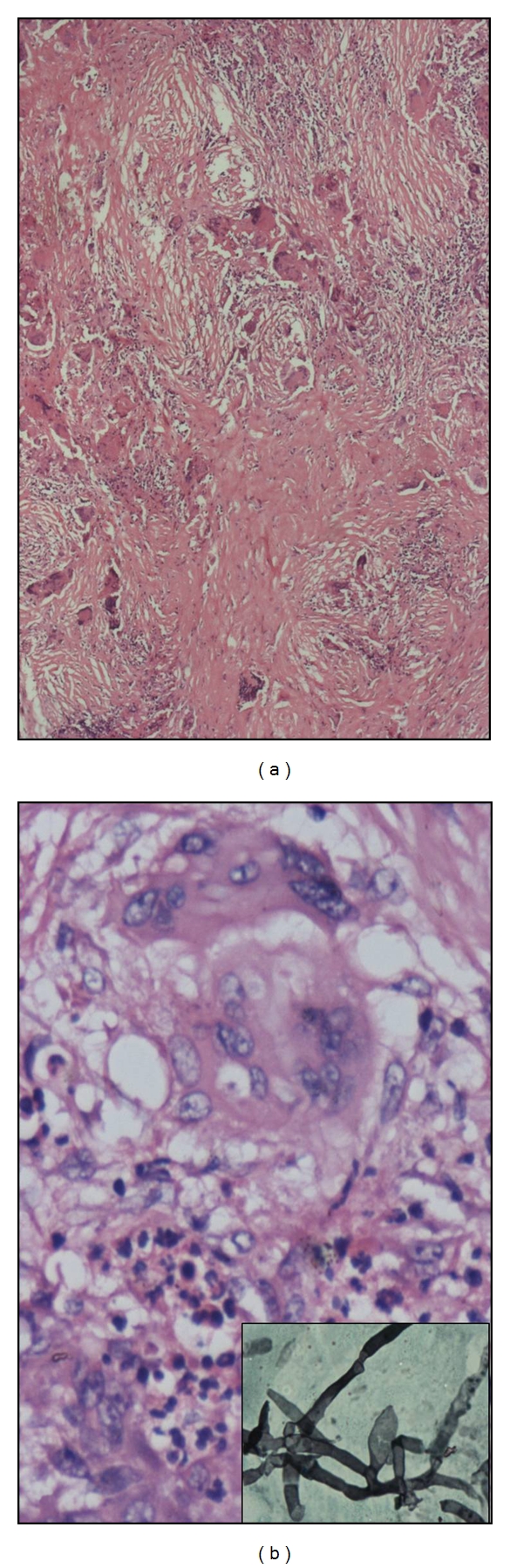
Histological sections of Aspergillus granuloma. (a) Giant cell rich granulomas with dense fibrosis (H&E; X40). (b) Giant cell with intracytoplasmic negative staining hyphae (H&E; X200). Inset: Gomori's silver methenamine stain highlighting slender septate hyphae of Aspergillus spp. (GMS; X400).
5. Sinocranial Aspergillus Granuloma—Pathological Features—Therapeutic Relevance
A. fumigatus elaborates a substance called fumagillin which is responsible for fibrosis [13]. Many allergens present in A. fumigatus are present at high levels of homology in A. flavus. A. flavus causes majority of the sinocranial infections. A. flavus produces many more allergic proteins than the two currently known proteins (Asp fl 13 and Asp fl 18) and may possess an allergen component similar to that of A. fumigatus [35]. A. flavus seems to be more virulent and more resistant to antifungal drugs than most of the other Aspergillus species.
The extensive fibrosis observed in the extraparenchymal, sinocranial Aspergillus granulomas has therapeutic relevance. Extensive fibrosis does not allow effective penetration of systemically administered antifungal agents. Thus these lesions need extensive radical excision to achieve cure [8, 16, 19, 30, 32]. The other approach to achieve effective therapeutic concentration of the antifungal agents will be intralesional administration of the antifungal agents by Ommaya reservoir [7, 15, 33].
References
- 1.Chimelli L, Mahler-Araújo MB. Fungal infections. Brain Pathology. 1997;7(1):613–627. doi: 10.1111/j.1750-3639.1997.tb01078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sundaram C, Umabala P, Laxmi V, et al. Pathology of fungal infections of the central nervous system: 17 Years’ experience from Southern India. Histopathology. 2006;49(4):396–405. doi: 10.1111/j.1365-2559.2006.02515.x. [DOI] [PubMed] [Google Scholar]
- 3.Santosh V, Yasha TC, Khanna N, et al. Fungal infections of the nervous system—a pathological study. Neurological Infections and Epidemiology. 1996;1:69–79. [Google Scholar]
- 4.Chakrabarti A. Epidemiology of central nervous system mycoses. Neurology India. 2007;55(3):191–197. doi: 10.4103/0028-3886.35679. [DOI] [PubMed] [Google Scholar]
- 5.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clinical Microbiology Reviews. 2000;13(2):236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alrajhi AA, Enani M, Mahasin Z, Al-Omran K. Chronic invasive aspergillosis of the paranasal sinuses in immunocompetent hosts from Saudi Arabia. American Journal of Tropical Medicine and Hygiene. 2001;65(1):83–86. doi: 10.4269/ajtmh.2001.65.83. [DOI] [PubMed] [Google Scholar]
- 7.Murthy JMK, Sundaram G, Prasad VSSV, Purohit AK, Rammurti S, Laxmi V. Sinocranial aspergillosis: a form of central nervous system aspergillosis in South India. Mycoses. 2001;44(5-6):141–145. doi: 10.1046/j.1439-0507.2001.00643.x. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui AA, Shah AA, Bashir SH. Craniocerebral aspergillosis of sinonasal origin in immunocompetent patients: clinical spectrum and outcome in 25 cases. Neurosurgery. 2004;55(3):602–611. doi: 10.1227/01.neu.0000134597.94269.48. [DOI] [PubMed] [Google Scholar]
- 9.Nadkarni TD, Menon RK, Desai KI, Goel A. A solitary cryptococcal granuloma in an immunocompetent host. Neurology India. 2005;53(3):365–367. doi: 10.4103/0028-3886.16950. [DOI] [PubMed] [Google Scholar]
- 10.Sundaram C, Mahadevan A, Laxmi V, et al. Cerebral zygomycosis. Mycoses. 2005;48(6):396–407. doi: 10.1111/j.1439-0507.2005.01167.x. [DOI] [PubMed] [Google Scholar]
- 11.Gologorsky Y, DeLaMora P, Souweidane MM, Greenfield JP. Cerebellar cryptococcoma in an immunocompetent child. Case report. Journal of Neurosurgery. 2007;107(4):314–317. doi: 10.3171/PED-07/10/314. [DOI] [PubMed] [Google Scholar]
- 12.Shamim M, Siddiqui A, Enam S, Shah A, Jooma R, Anwar S. Craniocerebral aspergillosis in immunocompetent hosts: surgical perspective. Neurology India. 2007;55(3):274–281. doi: 10.4103/0028-3886.35689. [DOI] [PubMed] [Google Scholar]
- 13.Shankar S, Mahadevan A, Sundaram C, et al. Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurology India. 2007;55(3):198–215. doi: 10.4103/0028-3886.35680. [DOI] [PubMed] [Google Scholar]
- 14.Kak VK, Banerjee AK, Radotra BD. Cerebral aspergillosis. Distinct clinicopathological pattern in 62 cases. Neurology India. 1989;37(supplement):p. 239. [Google Scholar]
- 15.Camarata PJ, Dunn DL, Farney AC, et al. Continual intracavitary administration of amphotericin B as an adjunct in the treatment of Aspergillus brain abscess: case report and review of the literature. Neurosurgery. 1992;31(3):575–579. doi: 10.1227/00006123-199209000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Naim-Ur-Rahman, Jamjoom A, Al-Hedaithy SSA, Jamjoom ZAB, Al-Sohaibani MO, Aziz SA. Cranial and intracranial aspergillosis of sino-nasal origin. Report of nine cases. Acta Neurochirurgica. 1996;138(8):944–950. doi: 10.1007/BF01411283. [DOI] [PubMed] [Google Scholar]
- 17.Pfaller MA, Pappas PG, Wingard JR. Invasive fungal pathogens: current epidemiological trends. Clinical Infectious Diseases. 2006;43(1):S3–S14. [Google Scholar]
- 18.Kethireddy S, Andes D. CNS pahrmacokinetics of antifungal agents. Expert Opinion on Drug Metabolism and Toxicology. 2007;3:573–581. doi: 10.1517/17425225.3.4.573. [DOI] [PubMed] [Google Scholar]
- 19.Sharma BS, Prasad KSM, Banerjee AK, et al. Intracranial fungal granuloma. Surgical Neurology. 1997;47(5):489–497. doi: 10.1016/s0090-3019(96)00209-1. [DOI] [PubMed] [Google Scholar]
- 20.Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A. Intracranial fungal granuloma: analysis of 40 patients and review of the literature. Surgical Neurology. 2005;63(3):254–260. doi: 10.1016/j.surneu.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 21.Challa S, Uppin S, Purohit A. Isolated cerebral Aspergillus granuloma with no obvious source of infection. Neurology India. 2007;55(3):289–291. doi: 10.4103/0028-3886.35691. [DOI] [PubMed] [Google Scholar]
- 22.Milosev B, el-Mahgoub S, Aal OA, el-Hassan AM. Primary aspergilloma of paranasal sinuses in the Sudan. A review of seventeen cases. British Journal of Surgery. 1969;56(2):132–137. doi: 10.1002/bjs.1800560213. [DOI] [PubMed] [Google Scholar]
- 23.Veress B, Malik OA, El Tayeb AA, et al. Further observations on the primary paranasal Aspergillus granuloma in the Sudan. A morphological study of 46 cases. American Journal of Tropical Medicine and Hygiene. 1973;22(6):765–772. doi: 10.4269/ajtmh.1973.22.765. [DOI] [PubMed] [Google Scholar]
- 24.Banerjee AK, Singh MS, Kak VK. Cerebral aspergillosis: report of 8 cases. Indian Journal of Pathology and Microbiology. 1977;20(2):91–99. [PubMed] [Google Scholar]
- 25.Anandi V, Ajay K, John J. Central nervous system fungal infections. A review of 6 years experience at vellore. In: Abraham J, editor. Progress in Clinical Neurosciences. Vol. 8. Madras, India: Guardian press; 1993. pp. 36–46. [Google Scholar]
- 26.Jamjoom AB, Al-Hedaithy SAS, Jamjoom ZAB, et al. Intracranial mycotic infections in neurosurgical practice. Acta Neurochirurgica. 1995;137(1-2):78–84. doi: 10.1007/BF02188786. [DOI] [PubMed] [Google Scholar]
- 27.Rajshekhar V. Surgical management of intracranial fungal masses. Neurology India. 2007;55(3):267–273. doi: 10.4103/0028-3886.35688. [DOI] [PubMed] [Google Scholar]
- 28.Parker JC, Jr., McCloskey JJ, Lee RS. The emergence of candidosis. The dominant postmortem cerebral mycosis. American Journal of Clinical Pathology. 1978;70(1):31–36. doi: 10.1093/ajcp/70.1.31. [DOI] [PubMed] [Google Scholar]
- 29.Dotis J, Roilides E. Immunopathogenesis of central nervous system fungal infections. Neurology India. 2007;55(3):216–220. doi: 10.4103/0028-3886.35681. [DOI] [PubMed] [Google Scholar]
- 30.Satishchandra P, Mathew T, Gadre G, et al. Cryptococcal meningitis: clinical, diagnostic and therapeutic overviews. Neurology India. 2007;55(3):226–232. doi: 10.4103/0028-3886.35683. [DOI] [PubMed] [Google Scholar]
- 31.Mylonakis E, Paliou M, Sax PE, Skolnik PR, Baron MJ, Rich JD. Central nervous system aspergillosis in patients with human immunodeficiency virus infection: report of 6 cases and review. Medicine. 2000;79(4):269–280. doi: 10.1097/00005792-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Selvam M, Pande A, Chakravarthy VM, Ramamurthi R. Invasive rhino-cerebral fungal granuloma. Neurology India. 2010;58(2):270–276. doi: 10.4103/0028-3886.63805. [DOI] [PubMed] [Google Scholar]
- 33.Young RF, Gade G, Grinnell V. Surgical treatment for fungal infections in the central nervous system. Journal of Neurosurgery. 1985;63(3):371–381. doi: 10.3171/jns.1985.63.3.0371. [DOI] [PubMed] [Google Scholar]
- 34.Haran RP, Chandy MJ. Intracranial Aspergillus granuloma. British Journal of Neurosurgery. 1993;7(4):383–388. doi: 10.3109/02688699309103492. [DOI] [PubMed] [Google Scholar]
- 35.Hedayati MT, Pasqualotto AC, Warn PA, Bowyer P, Denning DW. Aspergillus flavus: human pathogen, allergen and mycotoxin producer. Microbiology. 2007;153(6):1677–1692. doi: 10.1099/mic.0.2007/007641-0. [DOI] [PubMed] [Google Scholar]


