Abstract
Improvements in the sensitivity and quality of cross-sectional imaging have led to increasing numbers of patients being diagnosed with cystic lesions of the pancreas. In parallel, clinical, radiological, pathological and molecular studies have improved the systems for classifying these cysts. Patients with asymptomatic serous cystic neoplasms can be managed conservatively with regular monitoring; however, the clinical management of patients with intraductal papillary mucinous neoplasms and mucinous cystic neoplasms is far more challenging, as it is difficult to determine whether these lesions will progress to malignancy. Fortunately, prospective studies have helped to establish that proposed clinical and radiological criteria (the Sendai guidelines) can be used to guide the care of patients with cystic lesions of the pancreas. Despite this progress in imaging and clinical guidelines, sensitive and specific tests have not yet been developed that can reliably predict the histology and biological properties of a cystic lesion. Such biomarkers are urgently needed, as noninvasive precursors of pancreatic cancer are curable, while the vast majority of invasive pancreatic adenocarcinomas are not.
Introduction
The past decade has witnessed a dramatic increase in the number of patients being diagnosed with asymptomatic pancreatic cysts, sometimes referred to as ‘pancreatic incidentalomas’.1–4 Many of these lesions, including lymphoepithelial cysts, retention cysts and serous cyst-adenomas (SCA), are benign and can be monitored clinically if the diagnosis is certain. By contrast, research of patient outcomes in combination with meticulous histopathological studies has revealed that intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs) have the potential to progress to invasive pancreatic adenocarcinomas.
The power of modern imaging technologies to visualize even minute changes within the pancreas provides an unprecedented opportunity for the early detection and treatment of patients with pancreatic neoplasia. The importance of early detection of pancreatic cancer has been reiterated by the discovery that pancreatic cancers tend to metastasize fairly late in their genetic evolution, thus presenting a large window of opportunity for therapeutic intervention at an early, and hence potentially curable, stage.5 Although IPMNs and MCNs are generally detectable with modern imaging, our inability to predict accurately which cysts can be safely monitored, and which have an associated invasive adenocarcinoma or are likely to progress to infiltrating carcinoma remains a challenge. A major advance in the field was, therefore, the establishment of evidence-based treatment guidelines by a consortium of the International Association of Pancreatology at a meeting held in Sendai, Japan, in 2006 (Box 1).6 Although the Sendai guidelines are extremely helpful, they rely on indirect measurements of risk, such as the size of the cyst. Studies to validate these guidelines revealed clear limitations in the sensitivity and specificity of the recommended measurements, therefore, more reliable biomarkers than those used in the Sendai guidelines are needed for the optimal management of individual patients (Table 1).7–9
Box 1. Resection recommendation from the Sendai guidelines6.
All subgroups of patients with suspected mucinous cystic neoplasm of main duct intraductal papillary mucinous neoplasm should undergo resection
In patients with suspected branch duct intraductal papillary mucinous neoplasm, only those with a cyst >3 cm, with symptoms, with mural nodules or positive cytology should undergo resection
Table 1.
Studies validating the APA consensus guidelines about the treatment of IPMNs and MCNs
| Study | n | Average age | Study design | Conclusion |
|---|---|---|---|---|
| Pelaez-Luna et al. (2007)94 | 147 BD-IPMNs | 65 | Single center, retrospective | All patients with malignancy detected according to CG; specificity is low (23%) |
| Tang et al. (2008)8 | 61 (31 BD-IPMNs; 30 MD-IPMNs) | 66 | Single center, retrospective | CG recommended surgery in high-risk lesions; lesions with recommended nonsurgical treatment were low-risk |
| Sawhney et al. (2009)9 | 154 | 60 | Single center, retrospective | Some malignant cysts missed; accuracy of CG low (56%) |
Abbreviations: BD-IPMN, branch duct intraductal papillary mucinous neoplasm; CG, APA consensus guidelines; MD-IPMN, main duct intraductal papillary mucinous neoplasm.
In spite of substantial advances in perioperative outcomes, patients undergoing pancreatic resection still have an operative mortality of 2–4% and morbidity rates of ~40–50%.10 In addition, patients who undergo complete pancreatic resection will develop diabetes mellitus attributable to reduced insulin production. The mortality, morbidity and financial costs of these surgeries could potentially be reduced if patients with low-risk lesions could be identified and spared surgery.
In this Review we first discuss the salient clinicopathological and molecular features of IPMNs and MCNs, as these are the clinically most important precursor lesions of invasive pancreatic cancer. We review the latest important research accomplishments and outline new avenues for translational research that will hopefully provide attractive diagnostic and therapeutic targets within the near future. In the second section of our Review we focus on current biomarker research with a particular emphasis on pancreatic cyst fluid.
Patients with pancreatic cysts
Cystic lesions in the pancreas are actually fairly common. At the lower end of the prevalence range reported in the literature, pancreatic cystic lesions were found in just 0.2% of patients who were assessed with ultrasonography for a routine health examination or during outpatient screening,11 and another study identified cystic lesions of the pancreas in only 1.2% of the records of 24,039 patients undergoing CT or MRI scans (no more than 0.7% in the absence of pancreatitis).3 At the upper end of the spectrum, an assessment of the spin-echo MRI scans of 1,444 patients found cystic lesions in 19.6% of the patients. However, these results might be an overestimate of prevalence in the general population as the study included patients with pancreas-related symptoms.12 By contrast, an analysis of the abdominal MRI scans of 616 patients who did not have pancreas-related symptoms found at least one pancreatic cyst in 83 individuals (14%) and 40% of the pancreata of these individuals had multiple cysts.13 In this study the prevalence of incidental pancreatic cysts was strongly correlated with age: only one patient <40 years of age had a pancreatic cyst. The finding of pancreatic cysts in patients without pancreas-related symptoms is mirrored by a study from our institution published in 2008 in which CT scans revealed that 2.6% of asymptomatic patients had a pancreatic cyst.14 Today, the most accurate incidence rates of pancreatic cysts can probably be derived from meticulous necropsies. Such studies have reported incidental cystic changes in up to 25% of pancreata (many of these changes might not be seen by conventional imaging).15
Given that an estimated 50 million CT scans are performed annually in the USA, clinicians will have to familiarize themselves with the best management of patients who present with an asymptomatic pancreatic cyst.
IPMNs
Clinical appearance and morphology of IpMns
IPMNs are epithelial neoplasms in the main pancreatic duct or in one of its branches that produce mucins (Table 2, Figures 1 and 2).16,17 Noninvasive IPMNs can be divided into two clinical subtypes: those that predominantly involve the main duct and those that predominantly involve a branch duct.18 When main ducts and branch ducts are both involved sometimes the term ‘mixed-type’ or ‘combined-type’ IPMN is used.19 Main duct IPMNs mostly exhibit a more severe epithelial dysplasia and are more often associated with an infiltrating adenocarcinoma than are branch duct IPMNs.20,21 Although there is considerable overlap between main duct and branch duct IPMNs, the assessment of duct involvement during imaging before surgery enables a useful therapeutic stratification according to the Sendai criteria (see below).
Table 2.
Clinical features of cystic precursor lesions of pancreatic cancer
| Feature | IPMN | MCN |
|---|---|---|
| Predominant age | 60–70 years | 40–50 years |
| Sex ratio (female:male) | 2:3 | 20:1 |
| Predominant intrapancreatic localization | Head | Body and/or tail |
| Multifocal growth | Frequently | Rare |
| Communication of the cysts with larger pancreatic ducts | Arises in major or branch ducts | Rare |
| Stroma | Collagen rich | Ovarian type |
| Cyst fluid quality | Mucoid | Mucoid |
| Mucin oozing from papilla | Yes | No |
| Characteristic ERCP finding | Dilated pancreatic duct and filling defects | Displaced or compressed pancreatic duct |
Abbreviations: ERCP, endoscopic retrograde cholangiopancreatography; IPMN, intraductal papillary mucinous neoplasm; MCN, mucinous cystic neoplasm.
Figure 1.
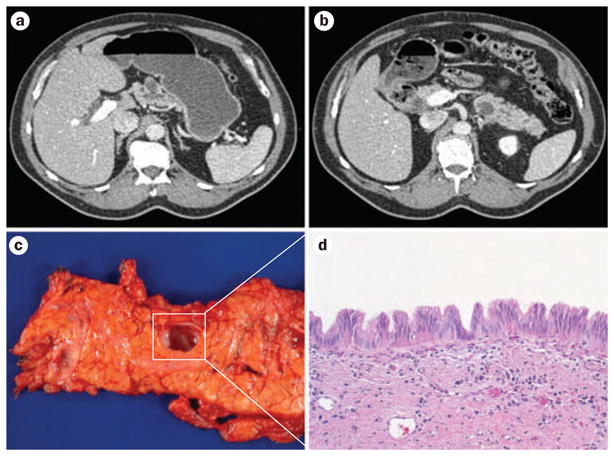
Multifocal intraductal papillary mucinous neoplasms (IPMNs) within a pancreas. CT imaging before surgery reveals multicystic changes involving the a | body of the pancreas and b | tail of the pancreas. c | After distal pancreatectomy six independent branch duct IPMNs can grossly be identified. d | Histologically the lesions show low to intermediate grade dysplasia and a characteristic gastric foveolar epithelial subtype (hematoxylin and eosin staining, 100× original magnification).
Figure 2.
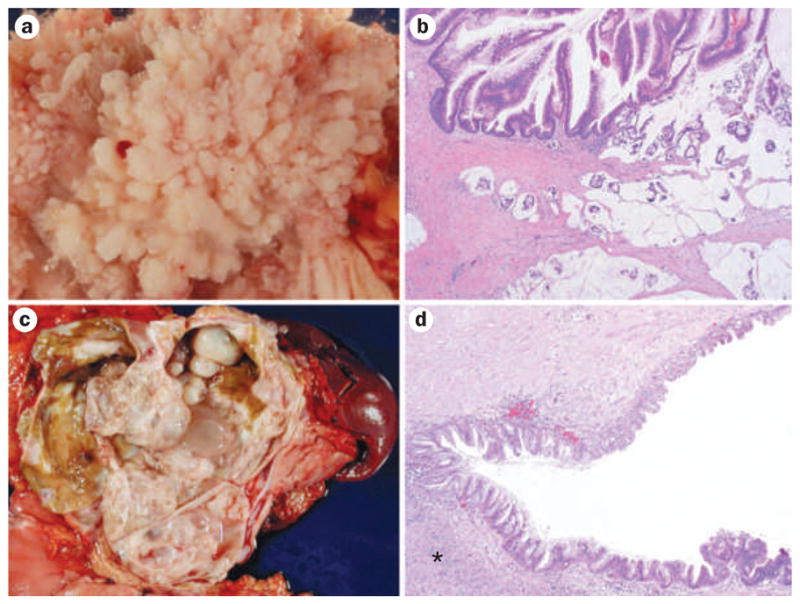
Cystic precursor lesions of pancreatic cancer. a | An extensive intraductal papillary growth of a large intraductal papillary mucinous neoplasm (IPMN) (image taken with specimen immersed in water). b | Histology displays finger-like papillae and high-grade dysplasia (upper part of image) with an invasive colloid adenocarinoma (lower part of image); these lesions are often located in the main pancreatic duct and show characteristic intestinal differentiation (hematoxylin and eosin staining, 20× original magnification). c | A large multicystic mucinous cystic neoplasm (MCN) in the pancreatic tail. d | A diagnostic sign for MCN ovarian-like stroma (indicated with an asterisk) underlies the neoplastic epithelium. The latter often shows abrupt transition in the degree of dysplasia; note the flat epithelium with mild cytoarchitectural atypia at the upper part of the image versus the more dysplastic and papillary growth pattern in the lower part of the image (hematoxylin and eosin staining, 40× original magnification).
On the basis of the predominant direction of differentiation within the lining epithelium, IPMNs can also be categorized as being of the gastric foveolar, intestinal, or pancreatobiliary subtypes. Main duct IPMNs are often larger in size than branch duct IPMNs and exhibit an intestinal or pancreatobiliary subtype in their lining epithelium; IPMNs of the branch duct are usually relatively small and are almost always of the gastric foveolar subtype.21 Usually, the intestinal IPMN subtype shows increased MUC2 expression, whereas the pancreatobiliary IPMN subtype expresses MUC1. The gastric foveolar IPMN subtype typically expresses MUC5AC and does not exhibit MUC1 or MUC2 expression.22,23 CDX2, a transcription factor crucial in intestinal development, is expressed by the majority of IPMNs of the intestinal subtype, suggesting the existence of an intestinal pathway of differentiation for some IPMNs. By contrast, IPMNs of the pancreatobiliary subtype, as well as pancreatic intraepithelial neoplasia (PanIN), which are also predominantly MUC1 positive, lack CDX2 expression.24,25
IPMNs are slightly more frequent in men than in women (~3:2 ratio). The age of patients presenting with an invasive IPMN is often 3–5 years older than the average age of presentation (60–70 years) in patients with a noninvasive IPMN. In addition, many patients with an IPMN develop symptoms attributable to their IPMN several months, and up to 10 years, before they are diagnosed.26,27 These observations suggest that there is a substantial window of opportunity to detect and treat noninvasive IPMNs before they progress to invasive cancer.28 The importance of detecting these neoplasms early is underscored by studies of patients who have undergone surgical resection that have reported a 5-year survival of >90% for patients with noninvasive IPMNs compared to survival of ~50% if the IPMN has an associated invasive carcinoma.26,29 Family history is a well-established risk factor for the development of IPMNs. Inherited predispositions for IPMNs include Peutz–Jeghers syndrome, which is caused by germ-line-inactivating mutations in the STK11 gene (also known as LKB1), and the less-well defined clinical entity of familial pancreatic cancer.30–32 Symptoms of IPMNs include abdominal pain, back pain, anorexia, weight loss and recurrent episodes of pancreatitis. However, the symptoms are usually nonspecific, which highlights the challenge of establishing an early diagnosis without reliable biomarkers.
A variety of diagnostic approaches are available to evaluate a potential IPMN. Some centers rely heavily on magnetic resonance cholangiopancreatography (MRCP), although high-resolution CT and endoscopic ultrasound (EUS) are emerging as the most accurate modalities.2,14 A CT of an IPMN will usually reveal a pancreatic cyst with ectasia of the main pancreatic duct or multiple cysts attributable to dilatation of side branch ducts with occasional multicentric growth (Figure 1a,b). Some patients will present with a mixed-type lesion with characteristics of both main duct and branch duct IPMNs. EUS might reveal mucus secretion from a prominent papilla of Vater sometimes referred to as ‘fish mouth papilla’ because of its patulous appearance. Endoscopic retrograde cholangiopancreaticography (ERCP) might reveal dilated pancreatic ducts or nodules in the cyst wall that represent a potential invasive transformation of the epithelium. Increased serum levels of tumor markers, such as carcinoembryonic antigen (CEA) or cancer antigen 19-9 (CA19-9), are sometimes detected in patients with an IPMN with an associated invasive carcinoma.33 The current status of cyst fluid biomarkers is outlined later in this article.
The clinically relevant pathologic features in IPMNs are the degree of dysplasia and the presence or absence of an associated invasive carcinoma. The degree of architectural and cytological atypia is used to subclassify IPMNs into low-grade dysplasia, intermediate dysplasia and high-grade dysplasia.34 Approximately one-third of IPMNs are associated with an invasive carcinoma. These invasive carcinomas are usually colloid adenocarcinomas or ductal adenocarcinomas. Colloid adenocarcinomas are characterized by abundant extracellular pools of mucin, in which floating neoplastic epithelium can be observed.35 Colloid cancers are generally associated with intestinal IPMNs that express MUC2, while the ductal adenocarcinomas are associated with pancreatobiliary lesions that express MUC1. Gastric IPMNs are only rarely associated with malignant progression; this observation supports a conservative treatment approach to most branch duct IPMNs where neoplastic epithelium is usually present.25 However, given the marked difference in 5-year survival between patients with noninvasive and invasive IPMNs (90% versus 50%, respectively),36 the presence of an invasive component should be excluded by careful histopathological examination of the entire specimen.
On the basis of these correlative observations, a consensus conference of the International Association of Pancreatology has proposed guidelines for the management of patients with pancreatic cysts suspected to be IPMNs (the Sendai guidelines). These guidelines use the results of radiology before surgery and/or the diagnosis from an endoscopic biopsy sample (Box 1).6 The proposed consensus criteria recommend resection of all cysts of the main pancreatic duct, and of side branch duct IPMNs measuring >3 cm on imaging, those that demonstrate nodules in the cystic wall (also termed ‘mural’ nodules) and those that cause symptoms. As always, these general recommendations must be tempered by the general medical condition of the patient, as well as their predicted life expectancy. Most lesions in branch ducts that do not meet these Sendai guidelines for resection can be monitored conservatively.37,38
Importantly, some IPMNs of the pancreas might be multifocal (Figure 1). Even if the primary cyst is removed by partial pancreatectomy, there is a risk of progression of existing synchronous lesions or the development of new metachronous lesions, including invasive cancer, in the remnant pancreas.39–41 Thus, patients who retain a portion of their pancreas following the resection of an IPMN need to be carefully followed up with periodic imaging of the pancreas. Of interest, patients with an IPMN might also have an increased risk of developing malignancies in other organs, such as the colon or stomach.42
Molecular alterations in IpMns
Cancer is fundamentally a genetic disease, and the genetic changes in IPMNs can provide additional insight into the nature of these lesions. Studies have identified a variety of genetic changes in IPMNs, some of these are distinct from those that occur in PanINs. Using array comparative genomic hybridization (CGH), IPMNs have been found to harbor recurrent cytogenetic alterations (on chromosomes 5q, 6q and 11q) that are distinct from those characteristically found in pancreatic ductal adenocarcinoma (PDAC).43 Grade for grade, the incidence of mutations in the KRAS gene is reported to be lower in IPMNs than in PanINs.44 Furthermore, the SMAD4 (also known as DPC4) gene is usually intact in noninvasive IPMNs, but can be lost in invasive IPMNs.45 The STK11 gene, which is usually mutated in the germ line DNA of patients with Peutz–Jeghers syndrome, also shows loss of expression in about one-quarter of sporadic IPMN lesions.30,46 As another example, activating mutations in the PIK3CA gene, involved in Akt oncogenic signaling, are found in 10% of IPMNs.47
As more is discovered about the molecular alterations in IPMNs the heterogeneity of this entity becomes more obvious. High-throughput molecular analyses, such as next-generation sequencing or serial analysis of gene expression, should enable further useful sub-classifications of IPMNs, especially with regard to elucidation of diagnostic and therapeutic targets. As such, high-throughput gene expression studies have detected differentially expressed genes, such as CLDN4, CXCR4, S100A4 and MSLN, that are overexpressed in the associated adenocarcinomas as compared to the intraductal component of the IPMN.48 The proteins of these overexpressed genes, therefore, are potentially important in the development of invasive disease from the noncancerous ductal epithelium.
MCNs
Clinical appearance and morphology of MCns
MCNs are the least frequent of the three known precursor lesions of pancreatic cancer. For example, low-grade PanINs are extremely common, and can be found in as many as 50% of pancreata in individuals >65 years.49 Although the exact prevalence of mucinous cysts is difficult to assess, some studies suggest their prevalence to be approximately half that of IPMNs.36 By definition, MCNs have two components—a mucin-producing epithelium and a dense ovarian-like stroma subjacent to the lining epithelium. In fact, the presence of the latter is a requirement for establishing a diagnosis of MCN. In MCNs, the contents of the cyst typically include fluid rich in mucin or hemorrhagic fluid. MCNs are considerably more frequent in women than men (~9:1 ratio) and patients are usually between 40 and 50 years of age when a primary diagnosis is made (Table 2).50 Symptoms of an underlying MCN can be vague, and include abdominal discomfort or sensations of an epigastric mass. Similarly to IPMNs, patients with invasive MCNs are, on average, approximately a decade older than those with noninvasive MCNs, presenting at a median age of ~55 years.51 Thus far, risk factors other than female sex are largely unknown for MCN.
On imaging, such as CT or MRI, and conventional ultrasound or EUS, MCNs appear as well circumscribed cystic lesions, with thick septae. In contrast to IPMNs, however, the main pancreatic duct is not dilated, and the lesion does not demonstrate any obvious communication with the ductal system. MCNs are usually located in the pancreatic body or tail. Levels of circulating tumor markers, such as CEA or CA19-9, are normal if there is no associated invasive component. However, levels of these markers might be raised in the cyst fluid aspirate of both noninvasive and invasive MCNs (see below).52,53
Histologically, the epithelial lining of an MCN consists of mucin-producing columnar cells with varying degrees of dysplasia.54 MCNs with low-grade dysplasia demonstrate few architectural and cytological changes. The lining cells contain abundant mucin overlying basally oriented nuclei, and are strongly labeled with antibodies to MUC5AC. In MCNs with intermediate (moderate) dysplasia, the nuclei begin to lose polarity and vary in morphology and size. MCN lesions with high-grade dysplasia (carcinoma in situ) demonstrate marked architectural and cytological abnormalities. An interesting feature that might be observed in the cyst lining is an abrupt transition between areas of severe and mild dysplasia. As previously stated, a diagnostic sine qua non of MCNs is the presence of an ovarian-like stroma underlying the neoplastic epithelium.55 The stroma expresses progesterone and estrogen receptors, and can even undergo luteinization akin to the actual ovarian stroma.
Similar to IPMNs, approximately one-third of reported MCNs are associated with an invasive adenocarcinoma, usually of the ductal type.36 The percentage of MCNs associated with an invasive cancer might be falling, which is partly attributable to changing diagnostic criteria, particularly the strict adherence to the requirement for the presence of an ovarian-like stroma. Patients who undergo resection for an MCN with an associated invasive cancer have a 5-year survival of 50–60%. By comparison, patients who undergo resection for a noninvasive MCN usually have an excellent outcome, with a disease-specific 5-year survival of almost 100%.51,56 The excellent survival of patients with surgically resected MCN relative to patients with surgically resected IPMN is because, in contrast to IPMNs, MCNs are typically unifocal lesions. Identifying the presence of an invasive component is critical in the resection specimen, since noninvasive MCNs, including those with severe dysplasia, are usually cured following surgical resection.51,54,56
As MCNs are rare, it is not clear which clinical criteria can be used to safely follow-up patients with known or suspected MCN. Many centers have adopted a resectional approach if the diagnosis of MCN is known or suspected; nonetheless, the risk of malignancy is largely proportional to the size of the lesion and, therefore, other centers have suggested following the Sendai guidelines for IPMNs.57
Molecular alterations in MCns
Understanding the molecular pathology of MCNs is a work in progress, partly because of the infrequency with which these lesions occur. Mutations that activate KRAS are observed even in low-grade dysplasia, while mutations in TP53 and SMAD4 usually occur in more advanced dysplasias, including in any associated invasive components.58,59 The cellular apomucins MUC5AC and MUC2 are expressed in noninvasive MCNs, while expression of MUC1 is associated with the acquisition of invasive properties.60 Global expression profiling has detected a range of differentially expressed transcripts in either the epithelium or the ovarian-like stroma of MCNs.61 Thus, potential oncogenes, such as S100P, PSCA, MYC, MET and CTSE, are upregulated in the neoplastic epithelial cells, while the steroidogenic acute regulatory protein and estrogen receptor 1 are expressed in the stroma. Furthermore, transcripts corresponding to protein jagged 1 and the transcription factor HES1, key components of Notch signaling, are overexpressed, which suggests that this ‘druggable’ pathway is reactivated in MCN.
Translational research
In vitro and in vivo models of cystic neoplasia
Although the pancreas was the first organ in which transgenesis was successfully accomplished,62,63 the development of a genetically engineered mouse model that closely mimics the full range of pathology observed in humans had been surprisingly challenging for over two decades. In 2003, Tuveson and colleagues developed the first genetically engineered mouse model of PDAC that recapitulated the multistep progression of the cognate human disease, including the presence of mouse PanINs (mPanINs) of various histological grades.64,65 Since that time, multiple genetic cooperation models have been developed that demonstrate higher penetrance of invasive cancer and shorter latency than the original ‘mutant Kras’ model.66–68 Although the overwhelming majority of these models progress to invasive cancer on the backdrop of extensive mPanINs, the generation of bona fide mouse models of cystic precursors has been considerably sparser.
Schmid and colleagues were one of the first groups to report a genetically engineered mouse model for cystic pancreatic neoplasms in 2007. Specifically, they generated compound heterozygous mice with transgenic expression of transforming growth factor (TGF) using a rat elastase promoter, in conjunction with expression of a knockin mutant KrasG12D allele from its endogenous locus. The resulting mice displayed the entire pancreatic progression spectrum, from mPanIN lesions to invasive adenocarcinomas with associated metastases, but at the same time, the pancreata of these mice had cystic papillary lesions that resembled human IPMNs.69 Since TGF is a ligand for the epidermal growth factor pathway, this study indicated a critical role for abnormal signaling of the epidermal growth factor receptor in IPMN development that is probably synergistic with oncogenic mutations in Kras. Most other genetically engineered mouse models that have yielded pancreatic cystic neoplasia involve co-expression of a mutant Kras allele concomitant with abrogation of the intracellular transforming growth factor β (TGF-β) transcriptional machinery, specifically through deletion of the gene that encodes the Smad cofactor Smad4 (also known as Dpc4). Smad4 binds to the receptor-regulated Smads (such as Smad1 or Smad2) upon engagement of TGF-β with its receptors, and the resulting heteromeric complex is translocated to the nucleus for initiating a TGF-β-induced transcriptional program. Loss of SMAD4 is observed in 55% of PDACs, and as noted previously, can be seen in invasive adenocarcinomas that arise in association with IPMNs or MCNs.
Curiously, in mice, the cystic neoplasms observed upon loss of Smad4 can resemble either IPMNs or MCNs, depending on gene dosage. Thus, loss of both Smad4 alleles in conjunction with mutant KrasG12D expression results in cystic lesions that resemble IPMNs70–72 while loss of one Smad4 allele (haploinsufficiency) co-expressed with mutant KrasG12D results in development of MCN-like cysts in the mouse pancreas.72 Of note, the second Smad4 allele is lost upon progression to invasive adenocarcinomas in the latter model. Thus, either haploinsufficiency or complete loss of intracellular TGF-β checkpoint control seems to be a prerequisite for developing cystic precursor lesions in the context of mutant Kras expression. As loss of SMAD4 is a late event in human IPMNs and MCNs, the relevance of these models to the cognate diseases remains uncertain. One awaits the complete sequencing of the genomes of IPMNs and MCNs to identify additional candidates that might be modeled in mice in cooperation with a mutant KrasG12D allele to yield more faithful models of cystic neoplasia than those currently available.
Xenograft models derived from human tumors are another potential platform that can be used to study tumor biology in vivo. Patient-derived tumors can be grown ex vivo to yield stroma-free epithelial cell lines, which can then be injected in vivo in immunocompromised mice to generate xenografts. Alternatively, patient-derived lesions can be directly implanted into immunodeficient mice and grown across generations, without the use of in vitro methods. Both modalities have been used for generating cystic precursor models. Thus, a cell line was generated from an invasive IPMN harboring mutations in KRAS and p53, and confirmed the ability of the cell line to engraft in immunodeficient mice.43 Similarly, the ability of IPMNs, including non-invasive lesions, to engraft in vivo has been confirmed by the successful establishment of eight xenografts from patient tumors directly implanted in highly immunodeficient (NOD/SCID/IL2Rγ0) mice; one of the explanted IPMNs was then established as an immortalized cell line.73 Finally, the first ex vivo model of MCN, denoted as MCC1 has been created. MCC1 is a cell line established from a noninvasive lesion with high-grade dysplasia.74 MCC1 has mutations of KRAS, CDKN2A and p53, and is capable of engrafting as xenografts in mice. These various cell line and xenograft models will hopefully serve as avenues for a variety of preclinical studies in cystic precursors, such as experimental therapeutics and gene discovery.
Cyst fluid—a key to diagnosis?
In spite of improved imaging modalities and emerging clinical awareness of pancreatic cysts, there is currently no assay for use before surgery available with the sensitivity and specificity needed to accurately predict the biological behavior of a pancreatic cyst. In some instances, neoplastic and non-neoplastic cysts can be readily distinguished by imaging, while in other patients this can be considerably challenging. The development of readily applicable guidelines to unequivocally determine which pancreatic cystic lesions can be conservatively managed with regular monitoring and which require surgical resection would be a major advance.36 Pancreatic cystic lesions, both neoplastic and non-neoplastic, are nearly always amenable to aspiration of cystic contents, which provides a unique opportunity for biomarker discovery in biospecimens proximate to lesional tissue.
Cyst fluid can be obtained by EUS-based fine needle aspirate for cytology, but the diagnostic benefit of such aspirations is often hampered by contamination from non-neoplastic tissues (such as the gastric mucosa) as well as by the inability to gather a sufficiently representative sample from a heterogeneously septated cyst. Moreover, EUS-based fine needle aspirate samples from cysts are often lacking adequate cellularity, reducing the chances of obtaining an accurate diagnosis on cytology of the aspirated material. Thus, sampling errors by EUS-based fine needle aspirate might result in false negative diagnosis of an absence of high-grade dysplasia or carcinoma, an outright criterion for resection. Nevertheless, cytologic preparations from fine needle aspirates can aid in the diagnosis of pancreatic cysts. Fine needle aspirates of IPMNs and MCNs cannot usually be distinguished because the ovarian-like stroma of MCNs is usually not present in aspirates. A more general diagnosis of mucin-producing neoplasm, therefore, is often used. Two components predominate in these aspirates: mucin and epithelium. Particularly thick, tenacious, colloid-like mucin is highly suggestive of a mucin-producing cystic lesion. The second component, the epithelium, is needed to establish the diagnosis of a neoplasm. The epithelial cells are typically columnar, and they can form flat sheets or papillary structures. The degree of dysplasia within aspirates often underestimates the degree of dysplasia identified in subsequent resection specimens, presumably because of the considerable heterogeneity that is often present in these lesions.
The diagnostic potential of protein expression patterns in cyst fluid has been extensively investigated. The most promising tumor markers include CEA, CA19-9 and carbohydrate antigen 125 (CA125). Of those, CEA (with a cut off of 200 ng/ml) is most frequently used to distinguish between cysts that produce mucin (IPMNs and MCNs) and nonmucinous cysts. However, a distinction between a noninvasive and an invasive cystic lesion is currently impossible using only the levels of CEA.75–77 Allen et al. screened cyst fluid specimens by means of a commercially available and custom designed multiplex protein assay using a biomarker panel developed for pancreatic cancer.78 Protein expression profiles were used to discriminate accurately between SCA and IPMN in 92% of patients. Interestingly, the only proteins overexpressed in the cyst fluid of patients with mucin-producing neoplasms were CEA and CA72.4. The majority of the other proteins included in the assay were downregulated in IPMN and MCN fluid specimens, compared to SCA fluid specimens.78 The same group of investigators evaluated the use of cyst fluid CEA analysis in the diagnosis of mucin-producing cysts by correlating clinicopathological and outcome data with CEA levels in cyst fluid collected during EUS. A cut off level of CEA >192 ng/ml proved to be capable of predicting the presence of a mucin-producing cyst with a sensitivity of 73% and a specificity of 65%. However, CEA levels were again not predictive of a malignant mucin-producing cyst or radiographic progression of the lesion.79 By contrast, in a study published in 2010, the value of CEA assessment before surgery for differentiating between a mucin-producing cyst and a nonmucinous cystic lesion has been questioned. The investigators found considerably raised levels of CEA (>450 ng/ml) in 3 of 9 lymphoepithelial cysts, which are benign lesions.80
Levels of amylase in the cyst fluid is another potential parameter in differentiating, for example, a pseudocyst, in which high levels of amylase are usually present, from a cyst that did not arise from pancreatic epithelium, such as a lymphangioma, which usually show low levels of amylase. In addition, SCAs generally have low levels of amylase in their cyst fluid. Since levels of amylase in IPMNs and MCNs are often increased, a differentiation from pseudocysts might not be possible using this analyte alone.81 Thus far, neither CEA nor amylase have been approved by the FDA for biomarker purposes in cyst fluid. These tests, therefore, have to be regarded as off-label applications.1,82
Not surprisingly, there have also been attempts to assess DNA-based markers in cyst fluid as a means of diagnostic stratification. For example, a pilot study used the amount of DNA in cyst fluid and molecular alterations in the DNA to facilitate the underlying diagnosis. A mutation in KRAS followed by microsatellite loss of heterozygosity at hot spots seemed to be most predictive of the presence of malignancy in a pancreatic cyst.83 Similarly, KRAS mutations and a panel of microsatellite markers were found to correlate with the degree of dysplasia in cysts.84 These initial attempts were expanded into a multicenter trial—the Pancreatic Cyst DNA Analysis Study (PANDA study), which included 113 patients with pancreatic cysts who underwent surgical resection or had diagnostic aspiration cytology.85 The cysts were classified as benign (nonmucinous) or mucinous, with the latter being further subdivided into pre-malignant and malignant (those with carcinoma in situ or invasive adenocarcinoma, respectively). Cyst fluid DNA was obtained by EUS, and in addition to analysis of mutations in KRAS, the overall fraction of alleles deemed as lost compared to the germ line (mean allelic loss amplitude or MALA) was determined.
In the PANDA study, the presence of a mutant KRAS or an MALA >65% were predictive of a mucinous lesion by both univariate and multivariate analysis, and DNA analysis improved the sensitivity of cyst fluid CEA. Notably mutation of KRAS was by itself not predictive of malignancy in mucin-producing cysts (probably a reflection of these mutations occurring early), although an MALA >82%, as well as the combination of KRAS and high MALA were associated with high-grade cysts that produced mucin. Although the PANDA study provides some rationale for coopting DNA-based analyses in diagnosis of pancreatic cysts, there were inherent weaknesses in the study design that diminish the overall significance of the results.86,87 For example, the study cohort had a selection bias towards high-grade cysts than are typically observed in a nonselected population; additionally, it was unclear from the trial if DNA analysis (an expensive addition to health-care costs) would add value to optimally applied Sendai criteria alone. Finally, there is concern that allelic loss amplitude can be confounded by DNA degradation as well as a number of variables attributable to underlying heterogeneity in cyst fluid composition. One anticipates that genomic profiling of IPMNs and MCNs by next-generation technologies will elucidate improved and cost-effective diagnostic biomarkers that can fill the current void in this area.
In addition to genomic alterations, epigenetic abnormalities, such as DNA methylation and microRNA (miRNA) expression profiles, have also been examined as potential biomarkers in cyst fluid samples.88,89 miRNAs are noncoding RNAs, ~21–23 nucleotides in length, that are involved in transcriptional regulation of coding genes.90 Aberrant miRNA expression has emerged as one of the hallmarks of human neoplasia, including pancreatic cancer.91–93 Our group assessed the relative expression levels of a panel of 12 miRNAs known to be upregulated in PDAC in 15 noninvasive IPMNs. miR-21 (mean 12.1-fold increase) and miR-155 (mean 11.6-fold increase) were identified as the most promising biomarker candidates. Furthermore, upregulation of miR-155 transcripts were observed in 6 of 10 IPMN-associated pancreatic fluid specimens compared with none of the specimens from control individuals.88 Analysis of the levels of miRNA expression in cyst fluid samples, therefore, might serve as an important tool in the diagnostic and prognostic classification of pancreatic cysts. This approach deserves further investigation.
Conclusions
The dramatic increase in the number of patients diagnosed with incidental pancreatic cysts through improved imaging is a unique chance to detect and treat cystic precursor lesions before the onset of malignancy. However, without reliable and cost-effective biomarkers the limited diagnostic accuracy of modern high-resolution imaging is a double-edged sword. Small pancreatic cysts can be detected with relative ease, but many are clinically irrelevant and will not harm the patient. Moreover, patients who have clinically benign lesions are at risk of over-treatment and morbidity and mortality from unnecessary intervention. Thus, it is believed that research using cyst fluid (a readily available clinical specimen) will provide diagnostic targets that will eventually enable appropriate treatment stratification of patients with pancreatic cysts. Thus far, it seems that a panel of molecular markers, rather than a single biomarker, will eventually enable screening of high sensitivity and specificity for pancreatic cystic lesions using cyst fluid samples.
Key points.
The number of patients being diagnosed with pancreatic cysts is increasing dramatically owing to the widespread use of high resolution imaging modalities
Although some pancreatic cysts are benign, others (such as intraductal papillary mucinous neoplasms or mucinous cystic neoplasms) are precursor lesions of invasive pancreatic cancer that might undergo malignant transformation
Diagnosis and risk assessment of pancreatic cystic lesions before surgery is challenging, which hampers the implementation of an appropriate therapeutic stratification
Ongoing research is trying to discover diagnostic targets to enable a tailor-made approach to the treatment of patients with pancreatic cystic lesions
The discovery of biomarkers in pancreatic cyst fluid (a readily available clinical specimen) is believed to provide diagnostic targets for translation into improved clinical management of patients with pancreatic cysts
Review criteria.
This Review is based on the professional experience of the authors as well as topic-related literature collected by the authors. Furthermore, we performed a PubMed search using the terms “pancreas”, “cyst”, “cyst fluid”, “IPMN”, “MCN”, “biomarker” and “SCA” either alone or in combination to select appropriate literature for our review article. The references of identified articles were scrutinized for additional relevant publications. We did not limit our search regarding publication dates or languages. The reference list was updated December 10th 2010.
Acknowledgments
The authors wish to thank Dr Karen M. Horton (Johns Hopkins University) for the CT scan of multifocal IPMN used in Figure 1. The authors would like to acknowledge the support of grants P50CA062924 and R01CA113669 (A. Maitra) and a research fellowship grant from Deutsche Krebshilfe, Bonn, Germany (H. Matthaei), the Sol Goldman Pancreatic Cancer Research Center and the Michael Rolfe Foundation for Pancreatic Cancer Research. C. P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape, LLC-accredited continuing medical education activity associated with this article.
Footnotes
Author contributions
All authors contributed equally to all aspects of this review.
Competing interests
The authors, the journal Chief Editor N. Wood and the CME questions author C. P. Vega declare no competing interests.
References
- 1.Brugge WR, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004;126:1330–1336. doi: 10.1053/j.gastro.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Fernández-del Castillo C, et al. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003;138:427–434. doi: 10.1001/archsurg.138.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spinelli KS, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004;239:651–659. doi: 10.1097/01.sla.0000124299.57430.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winter JM, et al. Periampullary and pancreatic incidentaloma: a single institution’s experience with an increasingly common diagnosis. Ann Surg. 2006;243:673–683. doi: 10.1097/01.sla.0000216763.27673.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yachida S, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467:1114–1117. doi: 10.1038/nature09515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32. doi: 10.1159/000090023. [DOI] [PubMed] [Google Scholar]
- 7.Park WG, et al. Diagnostic performance of cyst fluid carcinoembryonic antigen and amylase in histologically confirmed pancreatic cysts. Pancreas. 2011;40:42–45. doi: 10.1097/MPA.0b013e3181f69f36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang RS, et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol. 2008;6:815–819. doi: 10.1016/j.cgh.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Sawhney MS, et al. International consensus guidelines for surgical resection of mucinous neoplasms cannot be applied to all cystic lesions of the pancreas. Clin Gastroenterol Hepatol. 2009;7:1373–1376. doi: 10.1016/j.cgh.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 10.Winter JM, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10:1199–1211. doi: 10.1016/j.gassur.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda M, et al. Morphologic changes in the pancreas detected by screening ultrasonography in a mass survey, with special reference to main duct dilatation, cyst formation, and calcification. Pancreas. 1994;9:508–512. doi: 10.1097/00006676-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Zhang XM, Mitchell DG, Dohke M, Holland GA, Parker L. Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology. 2002;223:547–553. doi: 10.1148/radiol.2232010815. [DOI] [PubMed] [Google Scholar]
- 13.Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010;105:2079–2084. doi: 10.1038/ajg.2010.122. [DOI] [PubMed] [Google Scholar]
- 14.Laffan TA, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008;191:802–807. doi: 10.2214/AJR.07.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimura W, Nagai H, Kuroda A, Muto T, Esaki Y. Analysis of small cystic lesions of the pancreas. Int J Pancreatol. 1995;18:197–206. doi: 10.1007/BF02784942. [DOI] [PubMed] [Google Scholar]
- 16.Ohhashi K, Murakami F, Maruyama M. Four cases of mucous secreting pancreatic cancer. Prog Dig Endosc. 1982;203:348–351. [Google Scholar]
- 17.Belyaev O, et al. Intraductal papillary mucinous neoplasms of the pancreas. J Clin Gastroenterol. 2008;42:284–294. doi: 10.1097/MCG.0b013e3180500761. [DOI] [PubMed] [Google Scholar]
- 18.Bassi C, Sarr MG, Lillemoe KD, Reber HA. Natural history of intraductal papillary mucinous neoplasms (IPMN): current evidence and implications for management. J Gastrointest Surg. 2008;12:645–650. doi: 10.1007/s11605-007-0447-x. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka M, Kobayashi K, Mizumoto K, Yamaguchi K. Clinical aspects of intraductal papillary mucinous neoplasm of the pancreas. J Gastroenterol. 2005;40:669–675. doi: 10.1007/s00535-005-1646-4. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt CM, et al. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg. 2007;246:644–651. doi: 10.1097/SLA.0b013e318155a9e5. [DOI] [PubMed] [Google Scholar]
- 21.Furukawa T, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447:794–799. doi: 10.1007/s00428-005-0039-7. [DOI] [PubMed] [Google Scholar]
- 22.Yonezawa S, Nakamura A, Horinouchi M, Sato E. The expression of several types of mucin is related to the biological behavior of pancreatic neoplasms. J Hepatobiliary Pancreat Surg. 2002;9:328–341. doi: 10.1007/s005340200037. [DOI] [PubMed] [Google Scholar]
- 23.Moriya T, et al. Biological similarities and differences between pancreatic intraepithelial neoplasias and intraductal papillary mucinous neoplasms. Int J Gastrointest Cancer. 2005;35:111–119. doi: 10.1385/IJGC:35:2:111. [DOI] [PubMed] [Google Scholar]
- 24.Adsay NV, et al. Pathogenesis of colloid (pure mucinous) carcinoma of exocrine organs: coupling of gel-forming mucin (MUC2) production with altered cell polarity and abnormal cell-stroma interaction may be the key factor in the morphogenesis and indolent behavior of colloid carcinoma in the breast and pancreas. Am J Surg Pathol. 2003;27:571–578. doi: 10.1097/00000478-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Adsay NV, et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol. 2004;28:839–848. doi: 10.1097/00000478-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Salvia R, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–687. doi: 10.1097/01.sla.0000124386.54496.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tollefson MK, et al. Intraductal papillary mucinous neoplasm: did it exist prior to 1980? Pancreas. 2003;26:e55–e58. doi: 10.1097/00006676-200304000-00023. [DOI] [PubMed] [Google Scholar]
- 28.Ferrone CR, et al. Current trends in pancreatic cystic neoplasms. Arch Surg. 2009;144:448–454. doi: 10.1001/archsurg.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sohn TA, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–799. doi: 10.1097/01.sla.0000128306.90650.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sato N, et al. STK11/LKB1 Peutz-Jeghers gene inactivation in intraductal papillary-mucinous neoplasms of the pancreas. Am J Pathol. 2001;159:2017–2022. doi: 10.1016/S0002-9440(10)63053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chetty R, et al. Expression of Wnt-signaling pathway proteins in intraductal papillary mucinous neoplasms of the pancreas: a tissue microarray analysis. Hum Pathol. 2006;37:212–217. doi: 10.1016/j.humpath.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Brune K, et al. Multifocal neoplastic precursor lesions associated with lobular atrophy of the pancreas in patients having a strong family history of pancreatic cancer. Am J Surg Pathol. 2006;30:1067–1076. [PMC free article] [PubMed] [Google Scholar]
- 33.Fernández-del Castillo C, Alsfasser G, Targarona J, Brugge WR, Warshaw AL. Serum CA 19–9 in the management of cystic lesions of the pancreas. Pancreas. 2006;32:220. doi: 10.1097/01.mpa.0000202946.72493.74. [DOI] [PubMed] [Google Scholar]
- 34.Bosman FT, Carneiro F, Hruban R, Theise N. WHO Classification of Tumours of the Digestive System. World Health Organization; Lyon: 2010. [Google Scholar]
- 35.Adsay NV, et al. Colloid (mucinous noncystic) carcinoma of the pancreas. Am J Surg Pathol. 2001;25:26–42. doi: 10.1097/00000478-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Crippa S, et al. Mucin-producing neoplasms of the pancreas: an analysis of distinguishing clinical and epidemiological characteristics. Clin Gastroenterol Hepatol. 2010;8:213–219. doi: 10.1016/j.cgh.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodriguez JR, et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology. 2007;133:72–79. doi: 10.1053/j.gastro.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salvia R, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut. 2007;56:1086–1090. doi: 10.1136/gut.2006.100628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chari ST, et al. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology. 2002;123:1500–1507. doi: 10.1053/gast.2002.36552. [DOI] [PubMed] [Google Scholar]
- 40.Kobayashi G, et al. Mode of progression of intraductal papillary-mucinous tumor of the pancreas: analysis of patients with follow-up by EUS. J Gastroenterol. 2005;40:744–751. doi: 10.1007/s00535-005-1619-7. [DOI] [PubMed] [Google Scholar]
- 41.Salvia R, et al. Intraductal papillary mucinous neoplasms of the pancreas with multifocal involvement of branch ducts. Am J Surg. 2009;198:709–714. doi: 10.1016/j.amjsurg.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 42.Reid-Lombardo KM, Mathis KL, Wood CM, Harmsen WS, Sarr MG. Frequency of extrapancreatic neoplasms in intraductal papillary mucinous neoplasm of the pancreas: implications for management. Ann Surg. 2010;251:64–69. doi: 10.1097/SLA.0b013e3181b5ad1e. [DOI] [PubMed] [Google Scholar]
- 43.Fritz S, et al. Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals significant molecular differences compared to ductal adenocarcinoma. Ann Surg. 2009;249:440–447. doi: 10.1097/SLA.0b013e31819a6e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schönleben F, et al. BRAF and KRAS gene mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/IPMC) of the pancreas. Cancer Lett. 2007;249:242–248. doi: 10.1016/j.canlet.2006.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iacobuzio-Donahue CA, et al. Dpc-4 protein is expressed in virtually all human intraductal papillary mucinous neoplasms of the pancreas: comparison with conventional ductal adenocarcinomas. Am J Pathol. 2000;157:755–761. doi: 10.1016/S0002-9440(10)64589-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sahin F, et al. Loss of Stk11/Lkb1 expression in pancreatic and biliary neoplasms. Mod Pathol. 2003;16:686–691. doi: 10.1097/01.MP.0000075645.97329.86. [DOI] [PubMed] [Google Scholar]
- 47.Schönleben F, et al. PIK3CA mutations in intraductal papillary mucinous neoplasm/carcinoma of the pancreas. Clin Cancer Res. 2006;12:3851–3855. doi: 10.1158/1078-0432.CCR-06-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sato N, et al. Gene expression profiling identifies genes associated with invasive intraductal papillary mucinous neoplasms of the pancreas. Am J Pathol. 2004;164:903–914. doi: 10.1016/S0002-9440(10)63178-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cubilla AL, Fitzgerald PJ. Morphological lesions associated with human primary invasive nonendocrine pancreas cancer. Cancer Res. 1976;36:2690–2698. [PubMed] [Google Scholar]
- 50.Klimstra DS. Cystic, mucin-producing neoplasms of the pancreas: the distinguishing features of mucinous cystic neoplasms and intraductal papillary mucinous neoplasms. Semin Diagn Pathol. 2005;22:318–329. doi: 10.1053/j.semdp.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 51.Crippa S, et al. Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Ann Surg. 2008;247:571–579. doi: 10.1097/SLA.0b013e31811f4449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Buscaglia JM, et al. Patient- and cyst-related factors for improved prediction of malignancy within cystic lesions of the pancreas. Pancreatology. 2009;9:631–638. doi: 10.1159/000181173. [DOI] [PubMed] [Google Scholar]
- 53.Garcea G, et al. Cystic lesions of the pancreas. A diagnostic and management dilemma. Pancreatology. 2008;8:236–251. doi: 10.1159/000134279. [DOI] [PubMed] [Google Scholar]
- 54.Fernández-del Castillo C. Mucinous cystic neoplasms. J Gastrointest Surg. 2008;12:411–413. doi: 10.1007/s11605-007-0347-0. [DOI] [PubMed] [Google Scholar]
- 55.Wilentz RE, Albores-Saavedra J, Hruban RH. Mucinous cystic neoplasms of the pancreas. Semin Diagn Pathol. 2000;17:31–42. [PubMed] [Google Scholar]
- 56.Wilentz RE, et al. Pathologic examination accurately predicts prognosis in mucinous cystic neoplasms of the pancreas. Am J Surg Pathol. 1999;23:1320–1327. doi: 10.1097/00000478-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Yamao K, et al. Clinicopathological features and prognosis of mucinous cystic neoplasm with ovarian-type stroma: a multi-institutional study of the Japan pancreas society. Pancreas. 2011;40:67–71. doi: 10.1097/MPA.0b013e3181f749d3. [DOI] [PubMed] [Google Scholar]
- 58.Jimenez RE, et al. Sequential accumulation of K-ras mutations and p53 overexpression in the progression of pancreatic mucinous cystic neoplasms to malignancy. Ann Surg. 1999;230:501–511. doi: 10.1097/00000658-199910000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Iacobuzio-Donahue CA, et al. Dpc4 protein in mucinous cystic neoplasms of the pancreas: frequent loss of expression in invasive carcinomas suggests a role in genetic progression. Am J Surg Pathol. 2000;24:1544–1548. doi: 10.1097/00000478-200011000-00011. [DOI] [PubMed] [Google Scholar]
- 60.Lüttges J, Feyerabend B, Buchelt T, Pacena M, Klöppel G. The mucin profile of noninvasive and invasive mucinous cystic neoplasms of the pancreas. Am J Surg Pathol. 2002;26:466–471. doi: 10.1097/00000478-200204000-00008. [DOI] [PubMed] [Google Scholar]
- 61.Fukushima N, et al. Characterization of gene expression in mucinous cystic neoplasms of the pancreas using oligonucleotide microarrays. Oncogene. 2004;23:9042–9051. doi: 10.1038/sj.onc.1208117. [DOI] [PubMed] [Google Scholar]
- 62.Ornitz DM, Hammer RE, Messing A, Palmiter RD, Brinster RL. Pancreatic neoplasia induced by SV40 T-antigen expression in acinar cells of transgenic mice. Science. 1987;238:188–193. doi: 10.1126/science.2821617. [DOI] [PubMed] [Google Scholar]
- 63.Quaife CJ, Pinkert CA, Ornitz DM, Palmiter RD, Brinster RL. Pancreatic neoplasia induced by ras expression in acinar cells of transgenic mice. Cell. 1987;48:1023–1034. doi: 10.1016/0092-8674(87)90710-0. [DOI] [PubMed] [Google Scholar]
- 64.Hruban RH, et al. Pathology of genetically engineered mouse models of pancreatic exocrine cancer: consensus report and recommendations. Cancer Res. 2006;66:95–106. doi: 10.1158/0008-5472.CAN-05-2168. [DOI] [PubMed] [Google Scholar]
- 65.Hingorani SR, et al. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell. 2003;4:437–450. doi: 10.1016/s1535-6108(03)00309-x. [DOI] [PubMed] [Google Scholar]
- 66.Hingorani SR, et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell. 2005;7:469–483. doi: 10.1016/j.ccr.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 67.Bardeesy N, et al. Both p16(Ink4a) and the p19(Arf)-p53 pathway constrain progression of pancreatic adenocarcinoma in the mouse. Proc Natl Acad Sci USA. 2006;103:5947–5952. doi: 10.1073/pnas.0601273103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pasca di Magliano M, et al. Hedgehog/Ras interactions regulate early stages of pancreatic cancer. Genes Dev. 2006;20:3161–3173. doi: 10.1101/gad.1470806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Siveke JT, et al. Concomitant pancreatic activation of Kras(G12D) and Tgfa results in cystic papillary neoplasms reminiscent of human IPMN. Cancer Cell. 2007;12:266–279. doi: 10.1016/j.ccr.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 70.Kojima K, et al. Inactivation of Smad4 accelerates Kras(G12D)-mediated pancreatic neoplasia. Cancer Res. 2007;67:8121–8130. doi: 10.1158/0008-5472.CAN-06-4167. [DOI] [PubMed] [Google Scholar]
- 71.Bardeesy N, et al. Smad4 is dispensable for normal pancreas development yet critical in progression and tumor biology of pancreas cancer. Genes Dev. 2006;20:3130–3146. doi: 10.1101/gad.1478706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Izeradjene K, et al. Kras(G12D) and Smad4/Dpc4 haploinsufficiency cooperate to induce mucinous cystic neoplasms and invasive adenocarcinoma of the pancreas. Cancer Cell. 2007;11:229–243. doi: 10.1016/j.ccr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 73.Kamiyama H, et al. In vivo and in vitro propagation of intraductal papillary mucinous neoplasms. Lab Invest. 2010;90:665–673. doi: 10.1038/labinvest.2010.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sorio C, et al. Mucinous cystic carcinoma of the pancreas: a unique cell line and xenograft model of a preinvasive lesion. Virchows Arch. 2005;446:239–245. doi: 10.1007/s00428-004-1167-1. [DOI] [PubMed] [Google Scholar]
- 75.Brugge WR, Lauwers GY, Sahani D, Fernández-del Castillo C, Warshaw AL. Cystic neoplasms of the pancreas. N Engl J Med. 2004;351:1218–1226. doi: 10.1056/NEJMra031623. [DOI] [PubMed] [Google Scholar]
- 76.Walsh RM, et al. Prospective preoperative determination of mucinous pancreatic cystic neoplasms. Surgery. 2002;132:628–634. doi: 10.1067/msy.2002.127543. [DOI] [PubMed] [Google Scholar]
- 77.Lewandrowski KB, Southern JF, Pins MR, Compton CC, Warshaw AL. Cyst fluid analysis in the differential diagnosis of pancreatic cysts. A comparison of pseudocysts, serous cystadenomas, mucinous cystic neoplasms, and mucinous cystadenocarcinoma. Ann Surg. 1993;217:41–47. doi: 10.1097/00000658-199301000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Allen PJ, et al. Pancreatic cyst fluid protein expression profiling for discriminating between serous cystadenoma and intraductal papillary mucinous neoplasm. Ann Surg. 2009;250:754–760. doi: 10.1097/SLA.0b013e3181bd7f20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nagula S, et al. Evaluation of cyst fluid CEA analysis in the diagnosis of mucinous cysts of the pancreas. J Gastrointest Surg. 2010;14:1997–2003. doi: 10.1007/s11605-010-1281-0. [DOI] [PubMed] [Google Scholar]
- 80.Raval JS, et al. Pancreatic lymphoepithelial cysts express CEA and can contain mucous cells: potential pitfalls in the preoperative diagnosis. Mod Pathol. 2010;23:1467–1476. doi: 10.1038/modpathol.2010.144. [DOI] [PubMed] [Google Scholar]
- 81.Pelaez-Luna M, Chari ST. Cyst fluid analysis to diagnose pancreatic cystic lesions: an as yet unfulfilled promise. Gastroenterology. 2006;130:1007–1009. doi: 10.1053/j.gastro.2005.11.056. [DOI] [PubMed] [Google Scholar]
- 82.van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: a pooled analysis. Gastrointest Endosc. 2005;62:383–389. doi: 10.1016/s0016-5107(05)01581-6. [DOI] [PubMed] [Google Scholar]
- 83.Khalid A, et al. The role of pancreatic cyst fluid molecular analysis in predicting cyst pathology. Clin Gastroenterol Hepatol. 2005;3:967–973. doi: 10.1016/s1542-3565(05)00409-x. [DOI] [PubMed] [Google Scholar]
- 84.Schoedel KE, Finkelstein SD, Ohori NP. K-Ras and microsatellite marker analysis of fine-needle aspirates from intraductal papillary mucinous neoplasms of the pancreas. Diagn Cytopathol. 2006;34:605–608. doi: 10.1002/dc.20511. [DOI] [PubMed] [Google Scholar]
- 85.Khalid A, et al. Pancreatic cyst fluid DNA analysis in evaluating pancreatic cysts: a report of the PANDA study. Gastrointest Endosc. 2009;69:1095–1102. doi: 10.1016/j.gie.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 86.Anderson MA, Kwon RS, Scheiman JM. PANDA cyst-fluid analysis: eats, shoots and leaves? Gastrointest Endosc. 2009;69:1103–1105. doi: 10.1016/j.gie.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 87.Polkowski M. Endoscopic ultrasonography. Endoscopy. 2010;42:68–72. doi: 10.1055/s-0029-1215223. [DOI] [PubMed] [Google Scholar]
- 88.Habbe N, et al. MicroRNA miR-155 is a biomarker of early pancreatic neoplasia. Cancer Biol Ther. 2009;8:340–346. doi: 10.4161/cbt.8.4.7338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hong SM, et al. Multiple genes are hypermethylated in intraductal papillary mucinous neoplasms of the pancreas. Mod Pathol. 2008;21:1499–1507. doi: 10.1038/modpathol.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Croce CM, Calin G. A miRNAs, cancer, and stem cell division. Cell. 2005;122:6–7. doi: 10.1016/j.cell.2005.06.036. [DOI] [PubMed] [Google Scholar]
- 91.Szafranska AE, et al. MicroRNA expression alterations are linked to tumorigenesis and non-neoplastic processes in pancreatic ductal adenocarcinoma. Oncogene. 2007;26:4442–4452. doi: 10.1038/sj.onc.1210228. [DOI] [PubMed] [Google Scholar]
- 92.Lee EJ, et al. Expression profiling identifies microRNA signature in pancreatic cancer. Int J Cancer. 2007;120:1046–1054. doi: 10.1002/ijc.22394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bloomston M, et al. MicroRNA expression patterns to differentiate pancreatic adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA. 2007;297:1901–1908. doi: 10.1001/jama.297.17.1901. [DOI] [PubMed] [Google Scholar]
- 94.Pelaez-Luna M, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. 2007;102:1759–1764. doi: 10.1111/j.1572-0241.2007.01224.x. [DOI] [PubMed] [Google Scholar]


