Abstract
Background
Salmonella enterica serotype Typhi is the cause of typhoid fever. It is a human-restricted pathogen, and few data exist on S. Typhi gene expression in humans.
Methodology/Principal Findings
We applied an RNA capture and amplification technique, Selective Capture of Transcribed Sequences (SCOTS), and microarray hybridization to identify S. Typhi transcripts expressed in the blood of five humans infected with S. Typhi in Bangladesh. In total, we detected the expression of mRNAs for 2,046 S. Typhi genes (44% of the S. Typhi genome) in human blood; expression of 912 genes was detected in all 5 patients, and expression of 1,100 genes was detected in 4 or more patients. Identified transcripts were associated with the virulence-associated PhoP regulon, Salmonella pathogenicity islands, the use of alternative carbon and energy sources, synthesis and transport of iron, thiamine, and biotin, and resistance to antimicrobial peptides and oxidative stress. The most highly represented group were genes currently annotated as encoding proteins designated as hypothetical, unknown, or unclassified. Of the 2,046 detected transcripts, 1,320 (29% of the S. Typhi genome) had significantly different levels of detection in human blood compared to in vitro cultures; detection of 141 transcripts was significantly different in all 5 patients, and detection of 331 transcripts varied in at least 4 patients. These mRNAs encode proteins of unknown function, those involved in energy metabolism, transport and binding, cell envelope, cellular processes, and pathogenesis. We confirmed increased expression of a subset of identified mRNAs by quantitative-PCR.
Conclusions/Significance
We report the first characterization of bacterial transcriptional profiles in the blood of patients with typhoid fever. S. Typhi is an important global pathogen whose restricted host range has greatly inhibited laboratory studies. Our results suggest that S. Typhi uses a largely uncharacterized genetic repertoire to survive within cells and utilize alternate energy sources during infection.
Author Summary
Salmonella enterica serotype Typhi is the cause of typhoid fever and infects over 21 million cases and causes 200,000 deaths each year. S. Typhi only infects humans and this has greatly limited studies of S. Typhi pathogenesis. To study bacterial gene expression in human hosts, we used Selective Capture of Transcribed Sequences (SCOTS) and array hybridization to identify S. Typhi mRNAs expressed in the blood of 5 patients with S. Typhi infection. In total, we detected the expression of 2,046 S. Typhi genes (44% of the S. Typhi genome) in human blood; of these, 1,320 (29% of the S. Typhi genome) had significantly different levels of detection in human blood compared to in vitro cultures. Our results provide insight into S. Typhi pathogenesis, identifying both previously described and novel interactions occurring between host and microbe during the natural course of human infection. Further study of these genes, especially those of unknown function, may further our understanding of S. Typhi pathogenesis and aid in vaccine, diagnostic, and/or drug target development.
Introduction
Salmonella enterica serotype Typhi is a Gram-negative bacterium and the cause of typhoid fever. Typhoid fever affects over 21 million people each year, killing 200,000 [1]. S. Typhi is a human-restricted pathogen and this has greatly limited studies of S. Typhi pathogenesis. Our current understanding of S. Typhi responses during infection is largely based on the study of murine models with the related bacterium S. Typhimurium (i.e., a bacteria that causes a typhoid-like illness in mice) [2], a separate mouse model of S. Typhi infection [3], and ex vivo macrophage and epithelial cell models of S. Typhi and S. Typhimurium [4] However, these studies have limitations, and do not fully replicate human disease. For instance, despite high sequence similarity, 13% of the genes in the S. Typhi genome are absent from S. Typhimurium, and the S. Typhi chromosome contains over 200 pseudogenes that S. Typhimurium does not [5], [6].
Here we report the application of an mRNA/cDNA capture and amplification technology, Selective Capture of Transcribed Sequences (SCOTS), combined with cDNA hybridization technology [7]–[12], to directly assess the gene expression profile of S. Typhi in the blood of humans with typhoid fever in Bangladesh. We previously applied this technology to S. Paratyphi A, the 2nd leading cause of enteric fever, and detected expression of over 1700 bacterial genes during human infection [12]. Here we report the extension of this analysis to S. Typhi.
Methods
Ethics statement
This study was approved by the Ethical and Research Review Committees of the International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh (ICDDR,B) and the Human Research Committee of Massachusetts General Hospital; the study was conducted according to the principles expressed in the Declaration of Helsinki/Belmont Report. Written informed consent was obtained from all individuals or their guardians prior to study participation.
Study subject selection and sample collection
Individuals presenting to the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) Hospital or the Kamalapur field site of ICDDR,B were eligible for enrollment if they met the following criteria at presentation: age of 1–59 years, fever duration of 3–7 days (≥39°C), no obvious focus of infection, and no alternate diagnosis. We collected 2 ml of venous blood from participants, immediately placed these specimens in TRIzol (Invitrogen Life Technologies, Carlsbad, CA) at a 1 (blood)∶2 (TRIzol) volume ratio, and stored the samples at −70°C for later analysis. We simultaneously obtained 3–5 ml of blood for microbiologic analysis using a BacT/Alert automated system. We sub-cultured positive bottles on MacConkey agar, and identified S. Typhi isolates using standard biochemical tests and reaction with Salmonella-specific antisera [13]. After we collected blood, we treated patients with parenteral ceftriaxone, oral ciprofloxacin, or oral cefixime for up to 14 days at the discretion of the attending physician.
cDNA synthesis
To generate S. Typhi cDNA from blood samples, we used TRIzol-preserved blood of patients whose initial cultures were subsequently confirmed to grow S. Typhi. To create a corresponding in vitro S. Typhi cDNA sample for comparison, we grew each patient's bacterial isolate to mid-log growth phase (OD600 0.45–0.6) in Luria Bertani (LB) broth, and preserved the samples in TRIzol at a 1 (mid-log culture)∶2 (TRIzol) volume ratio. We extracted total RNA from TRIzol preserved samples per the manufacturer's instructions (Invitrogen) and treated recovered RNA with DNase I on RNeasy columns (Qiagen Inc., Valencia, CA). We then converted 5 µg of total RNA into cDNA for each sample, as previously described with a few modifications [12]. Briefly, we used random priming (T-PCR) to obtain a representative amplifiable double-stranded cDNA population by using Superscript III (Invitrogen) with a conserved primer with a defined 5′ end terminal sequence and a random nonamer at the 3′ end [14]. We then synthesized second strands using the same primers and Klenow fragment (Invitrogen) according to the manufacturer's instructions, and then equilibrated samples based on 16S S. Typhi rRNA.
Selective Capture of Transcribed Sequences (SCOTS)
We separated bacterial cDNA from host DNA using SCOTS, as previously described [12]. Briefly, we mixed denatured biotinylated S. Typhi gDNA with blocking ribosomal S. Typhi DNA, and added this denatured mixture to both in vivo and in vitro cDNA samples. After hybridizing samples overnight at 67°C, we captured biotinylated S. Typhi gDNA-cDNA hybrids using streptavidin-coated magnetic beads (Dynabeads M-280 streptavidin, Invitrogen), eluted captured cDNA with NaOH, PCR-amplified cDNA samples with conserved primers, and purified products using Qiagen PCR column purification kits. We performed three rounds of capture and amplification to separate S. Typhi cDNA from host DNA and to generate the cDNA mixture used for microarray hybridization.
Salmonella microarray analysis
We labelled in vivo and in vitro cDNA recovered from SCOTS with Cy3 and Cy5, respectively, and hybridized these preparations to Salmonella ORF microarrays (version STv7S; McClelland Laboratory, Vaccine Research Institute of San Diego, CA, http://www.sdibr.org/Faculty/mcclelland/mcclelland-lab) in duplicate and with two dye reversals as previously described [12]. These microarrays contained gene-specific PCR-products of 4,600 ORFs from Salmonella enterica serotype Typhi CT18 (98.6% genome coverage) and 4,318 ORFs of strain Ty2 (98.0% genome coverage. The arrays also contained 1049 S. enterica ORFs absent from the S. Typhi genome. We used an equal amount of in vivo and in vitro Cy dye-labeled product on all slides for a given patient. We used ScanArray software (ScanArray express, version 3.0.1) to quantify signal intensities.
For each individual patient, we considered a gene to be detected in vivo if at least 2 of the 3 replicate gene spots on each of the four slides for that infected human was at least ten median absolute deviations greater than the median of spots on the microarray corresponding to genes absent from the S. Typhi CT18 or Ty2 genomes. For those genes we detected in vivo, we evaluated whether there was a difference in expression when compared to detection levels for in vitro grown organisms. For this latter statistical analysis, we included genes with a coefficient of variation in signal intensity less than 50% within an array, and employed repeated measures ANOVA (to within slide replicate spots) with type (in vivo versus in vitro) and dye effects to LOESS-normalized, log-transformed data. Those genes with a False Discovery Rate of less than 0.05 computed using Benjamini-Hochberg multiple testing adjustment and a 2-fold variation in signal intensity were considered differentially expressed in vivo versus in vitro. We deposited data in the NCBI Gene Expression Omnibus (GEO, www.ncbi.nlm.nih.gov/geo), accessible through GEO accession number GSE30565. We based functional classification of genes on J. Craig Venter Institute annotations (http://cmr.jcvi.org/tigr-scripts/CMR/CmrHomePage.cgi).
Quantitative PCR analysis
We used quantitative real time PCR (RT-qPCR) to confirm microarray results for a subset of genes. We compared mRNA levels in the peripheral blood (in vivo sample) of infected patients (i.e. the 5 patients included in our SCOTS array analysis and 5 additional patients) to three in vitro culture replicates of a S. Typhi isolate (from Patient 1) grown to mid-logarithmic phase in LB (in vitro sample), as previously described [12]. To maximize the likelihood of detecting differences in gene expression in comparative samples, we selected eight representative genes from operons involved in intra-cellular invasion or survival (STY4609, sopE, invasion-associated secreted protein; STY3639, trxA, thioredoxin); alternate energy usage (STY2244, pduB, putative propranediol utilization protein; STY0417, psiF, phosphate starvation-inducible protein; STY2701, eutN, a putative ethanolamine utilization protein; STY0634, fepC, a ferric enterobactin transport ATP-binding protein); and bacterial adhesion (STY0207, staA, putative fimbrial protein and STY4543, pilO, putative pilus assembly protein), focusing on genes with high baseline signals and fold-increases by SCOTS-cDNA hybridization analysis comparing in vivo (high signal) to in vitro (low signal) samples. We also quantified by RT-qPCR the expression levels of two house-keeping genes that were predicted by SCOTS-cDNA hybridization to be equally expressed in in vivo and in vitro samples (STY0724, encoding a glutaminyl-tRNA synthetase, glnS; and STY3081, encoding an enolase, eno). We were unable to reproducibly assess expression levels of genes predicted by SCOTS-cDNA hybridization to be down-regulated in blood samples compared to in vitro grown organisms. To generate cDNA for quantitative RT-PCR from TRIzol-preserved samples, we used SuperScript II (Invitrogen) with random hexamers (Sigma, St. Louis, MO) according to the manufacturer's instructions, and performed RT-qPCR analysis using iQ SYBR Green Supermix reagent (Bio-Rad; Hercules, CA) and a CFX96 Real-time PCR detection system (Bio-Rad; Hercules, CA) as previously described [12]. Primers are listed in the Supplemental Table S1. We used no-template controls and samples lacking reverse transcriptase as baseline reactions for each sample. After calculating the threshold cycle (CT) in the low/linear portion of product curves, we quantified gene copy numbers using pGEM-T Easy-based plasmids (Promega, Madison, WI) containing the gene of interest. To calculate the control gene copy number, we used plasmid size and A260 readings, and normalized gene copy numbers based on cDNA copies of 16S rRNA. We assessed singularity of product species and size by melting curve analysis, as previously described [15].
Results
Patient samples
Of the 89 patients enrolled for blood sample collection, we identified 10 patients with confirmed S. Typhi bacteremia at the time of TRIzol-preserved blood collection. We performed SCOTS-cDNA hybridization screening analysis using samples from patients 1–5, and performed RT-qPCR on samples from patients 1–10, as sample quantity permitted.
S. Typhi transcripts detected in the blood of infected humans
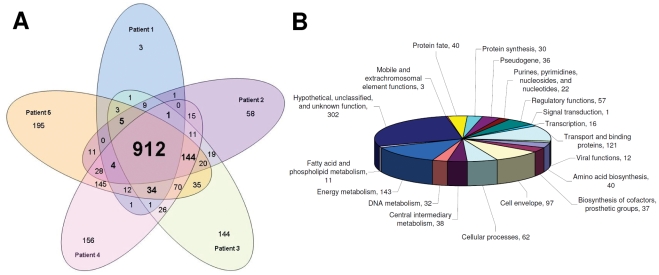
Using SCOTS-cDNA hybridization technology, we detected expression of 2046 S. Typhi genes in the blood of bacteremic patients. This represents approximately 44% of the S. Typhi ORFeome (Figure 1A, Supplemental Table S2). Of these, we detected expression of 912 genes in all 5 patients (45% of detected transcripts), and 1100 in at least 4 of the 5 patients (54% of detected transcripts).
Figure 1. S. Typhi mRNA detected in vivo by SCOTS-microarray analysis.
(A) Venn diagram of the 2046 S. Typhi transcripts detected in vivo by patient, and (B) functional classification of proteins encoded by the 1100 S. Typhi transcripts detected in 4 or more patients.
The products encoded by the 1100 genes identified in 4 or more patients fell into a number of functional categories (Figure 1B). The most highly represented group were genes currently annotated to encode hypothetical proteins or proteins designated as unknown or unclassified. The next most highly represented groups were genes that encode products involved with energy metabolism, transport and binding, followed by genes encoding products of the cell envelope or associated with cellular processes and pathogenesis. Ninety-five of the 1100 genes were located within known Salmonella pathogenicity islands (SPI 1–7, 9, 10, 13, and 16), and 29 are known components of the PhoP regulon, a major virulence regulon in Salmonella, involved in intra-macrophage survival.
S. Typhi transcripts with a different level of detection in in vivo versus in vitro bacterial samples
A total of 31 genes were detected in 4 or more patients in vivo, but not detected in any in vitro sample (Table 1). The majority of these genes are involved with survival in nutrient-limited conditions including psiF, a phosphate starvation-inducible protein; bioF and thiG involved in vitamin biosynthesis; eutD, oadG, and pduB involved in use of alternative carbon sources; and fepD involved in iron acquisition.
Table 1. S. Typhi transcripts detected only in in vivo samples.
| CT18 Locus | Ty2 Locus | Gene | Function |
| Biosynthesis of cofactors, prosthetic groups, and carriers | |||
| STY0828 | t2092 | bioF | 8-amino-7-oxononanoate synthase |
| STY3725 | t3471 | thiG | thiamine biosynthesis protein |
| Cell envelope | |||
| STY1609 | t1379 | hypothetical protein | |
| STY4620 | t4314 | nucD2 | putative lysozyme |
| Central intermediary metabolism | |||
| STY0417 | t2480 | psiF | phosphate starvation-inducible protein PsiF |
| STY2702 | t0393 | eutD | putative phosphate acyltransferase |
| STY4773 | t4468 | ppa | inorganic pyrophosphatase |
| Energy metabolism | |||
| STY1917 | t1086 | hyaE | hydrogenase-1 operon protein HyaE |
| STY2316 | t0768 | manB | Phosphomannomutase |
| Fatty acid and phospholipid metabolism | |||
| STY2700 | t0395 | eutE | putative aldehyde dehydrogenase |
| Protein synthesis | |||
| STY4360 | t4067 | rplW | 50S ribosomal subunit protein L23 |
| Regulatory functions | |||
| STY3707 | t3448 | yifE | conserved hypothetical protein |
| Transport and binding proteins | |||
| STY0065 | t0058 | oadG | oxaloacetate decarboxylase gamma chain |
| STY0123 | t0110 | yabJ | hypothetical ABC transporter |
| STY0636 | t2276 | fepD | ferric enterobactin transport protein FepD |
| STY2341 | t0744 | mdtC | putative RND-family transporter protein |
| Hypothetical, Unclassified and Unknown proteins | |||
| t3166 | hypothetical protein | ||
| STY0321 | t2569 | Rhs-family protein | |
| STY1058-60,1063-64,1069 | putative prophage proteins | ||
| STY1323 | t1640 | conserved hypothetical protein | |
| STY1548 | t1434 | conserved hypothetical protein | |
| STY1732 | t1256 | ydhZ | conserved hypothetical protein |
| STY1916 | t1087 | hyaD | hydrogenase-1 operon protein HyaD |
| STY2244 | t0835 | pduB | putative propanediol utilization protein PduB |
| STY2608 | t0487 | conserved hypothetical protein | |
| STY3448 | t3185 | yraN | conserved hypothetical protein |
S. Typhi transcripts detected in the blood of 4 or more of 5 patients, but not in bacterial samples grown in vitro.
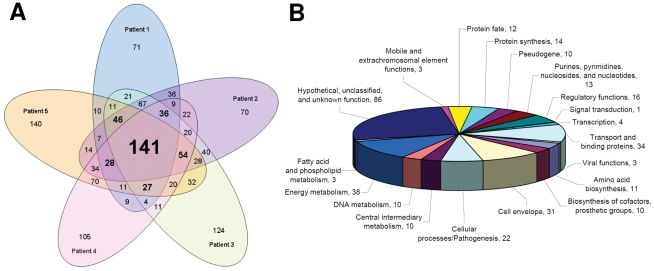
Of the 2046 transcripts detected in human blood samples, 1320 (representing 29% of S. Typhi ORFeome) had significantly different levels of detection in in vivo samples compared to bacterial samples grown in vitro (Figure 2A, Table S2). Detection levels for 141 transcripts were significantly different between in vivo and in vitro samples in all 5 patients, and 331 in at least 4 patients. These 331 encode products that fall into a number of functional categories (Figure 2B). The most highly represented group included proteins annotated as hypothetical, unknown, or unclassified. Other highly represented groups included energy metabolism, transport and binding, the cell envelope, and cellular processes and pathogenesis.
Figure 2. S. Typhi mRNA with different levels of detection in vivo versus in vitro bacterial samples by SCOTS-microarray analysis.
(A) Venn diagram of the 1320 S. Typhi transcripts with significantly different levels of detection between in vivo and in vitro bacterial samples by patient, and (B) functional classification of proteins encoded by the 331 S. Typhi transcripts with significantly different levels of detection in 4 or more patients.
Quantitative Real Time-PCR analysis
To confirm S. Typhi mRNA expression levels in human blood compared to in vitro grown bacteria, we used RT-qPCR to assess the copy number of the following eight genes that had high in vivo baseline reactivity as well as fold-change between in vivo and in vitro samples by SCOTS array analysis: thioredoxin, trxA (STY3639); a putative fimbrial protein, staA (STY0207); an invasion-associated secreted protein, sopE (STY4609); a putative propranediol utilization protein, pduB (STY2244); a putative pilus assembly protein, pilO (STY4543); an phosphate-inducible starvation protein, psiF (STY0417); a putative ethanolamine utilization protein, eutN (STY2701); and a ferric enterobactin transport ATP-binding protein, fepC (STY0634). Compared to expression levels in in vitro grown bacteria, we found increased expression of all 8 genes in the blood of infected humans, including in humans not analyzed by the SCOTS-cDNA hybridization screening protocol (Figure 3, A–H). As predicted by our SCOTS screening, we found no differences by RT-qPCR in the expression of housekeeping genes glnS (STY0724) and eno (STY3081) in blood versus in vitro bacterial samples (Figure 3, I-J).
Figure 3. Quantitative RT-PCR S. Typhi mRNA expression profiles in human blood compared to in vitro bacterial samples.
Quantitative real time-PCR analysis of S. Typhi genes (A–H) comparing RNA recovered from blood of bacteremic patients to an in vitro culture of the corresponding clinical isolate. Genes represented in A–H were identified by SCOTS-cDNA as being more highly expressed in human blood samples than in in vitro grown organisms; genes I–J had equivalent levels of detection in in vivo versus in vitro samples by SCOTS. Mean copies of mRNA per copy of 16S rRNA and standard error of the mean are presented. * p<0.05; †p<0.01. RT-qPCR was performed on a minimum of 5 patients as sample quantity permitted.
Discussion
S. Typhi is a human-restricted pathogen, the cause of typhoid fever, and a significant cause of global morbidity and mortality. Despite this, there are limited data on bacterial events within humans infected with S. Typhi. Here we describe the application of a cDNA capture-amplification approach combined with microarray hybridization technology to assess S. Typhi gene expression directly in the blood of infected humans. In total, we detected 2046 S. Typhi transcripts in human blood (45% of S. Typhi transcriptome); we detected 1100 in at least 4 of 5 patients. Two major virulence determinants of Salmonella are the ability to invade host cells and the ability to survive and replicate within host cells. The PhoPQ-two component regulatory system is involved in intra-macrophage survival and antimicrobial resistance [16], and Salmonella pathogenicity island-1 (SPI-1) and SPI-2 encode type three secretion systems (T3SSs) involved in invasion of host cells and intracellular survival and replication, respectively [17], [18]. In our analysis, we identified 29 genes involved in the PhoP regulon as more highly expressed in human samples, including the two component regulator itself, phoPQ; virk, a virulence protein; mgtBC, involved in magnesium transport; pmrF, a antimicrobial resistance protein; and slyB, an outer membrane lipoprotein [19], [20]. We also identified 95 genes located within previously described SPIs, including SPI-1 and 2, as well as genes within SPI-3–7, 9, 10, 13, and 16.
The role of SPI-1 in invasion of epithelial cells has been well established [21]. We detected a number of transcripts associated with SPI-1 genes, including a number that encode effector proteins injected into eukaryotic cells via the SPI-1 T3SS, such as SipB. We also detected a number of transcripts encoding SPI-1 T3SS effector proteins expressed from other SPIs, including sopE (expressed from SPI-7) and sopB/sigD (expressed from SPI-5); SopB/sigD is involved in creation and maintenance of the Salmonella Containing Vacuole (SCV), crucial to intra-cellular survival of Salmonella in eukaryotic cells [22]. Of note, we similarly identified SPI-1 transcripts in our recent analysis of S. Paratyphi A cDNA in the blood of infected humans in Bangladesh [12]. Our detection of these transcripts in the blood of infected humans builds upon recent suggestions that the SPI-1 T3SS is involved in pathogenic events beyond intestinal epithelial cell invasion during enteric fever [23]–[25]. In addition to sopE, we also detected transcripts from the Type IV pilus operon encoded within SPI-7, including pilL, pilO, pilQ, pilR, pilU, and pilV, which facilitates invasion of Salmonella into epithelial cells and monocytes [26], [27]. Identification of SPI-7 genes in our analysis is of particular interest since SPI-7 is absent from S. Typhimurium and S. Paratyphi A, but present in S. Typhi, S. Paratyphi C, and S. Dublin [28].
In addition to those associated with SPIs and the PhoPQ regulon, we detected transcripts from a number of virulence-associated Salmonella genes in human blood. These include aromatic amino acid biosynthesis pathway genes (aroG, aroD, aroH, aroE, aroB); mutations in this pathway have been the basis of live attenuated S. Typhi vaccines [29]. We also detected transcripts from genes involved in purine biosynthesis (guaB, purG, purA) [30] and divalent cation transport including Mg2+ (corA, mgtBC) [31]–[33], and Fe 2+ and Mn2+ uptake systems (sitBC and mntH) [34] that have all been associated with virulence in Salmonella.
In order to adapt to the intracellular environment, Salmonella must alter its metabolism to available nutrient and energy sources. We detected transcripts of genes involved in the use of alternative carbon sources, the coenzyme B12-dependent 1,2-propranediol utilization pathway (encoded by the pdu operon), and the ethanolamine utilization pathway (encoded by the eut operon). We also found these operons to be up-regulated in our analysis of S. Paratyphi A genes detected in the blood of humans [12], and mutations in these operons result in attenuation of virulence in S. Typhimurium infection models [35]–[37]. We also identified transcripts expressed from genes encoding three NiFe-uptake hydrogenases that have been associated with virulence in S. Typhimurium, including hydrogenase A, B and D [38]. Prior studies have shown that the hya and hyd operons are upregulated in murine and human phagocytes; hya genes are required for survival within macrophages, and both hya and hyd genes were detected in mice using the RIVET (Resolvase In-Vivo Expression Technology) reporter system that identifies genes expressed in vivo [39]. Our analysis shows that these genes are also expressed by S. Typhi during human infection. Other potential virulence-associated genes that we identified included genes involved in thiamine biosynthesis (e.g. thiG, thiJ, abpA), biotin biosynthesis (e.g. bioB, bioF, kbl), iron acquisition via siderophore biosynthesis (e.g. iroA gene cluster, fes, fepECDB), and phosphate transport (ugpBAEC operon), many of which were also detected in our transcriptional analysis of S. Paratyphi A in infected humans [12].
In addition to survival in nutrient-limited conditions, Salmonella must also be able to survive the action of antimicrobial peptides, oxidative killing, and nitric oxide in various ecologic niches within the human body. We detected genes that may be involved in survival of stressful environments, including a number involved in antimicrobial resistance (e.g. pqaB, virK, pmrF, smvA, bacA, emrA, mdtC) [40]–[45], oxidative stress (e.g. trxA) [46], resistance to acid tolerance (e.g. narZYWV operon) [47], and genes involved in DNA recombination and repair (e.g. recA, recBD, recN, recG, xthA) [48]. Of note, the most highly represented group were genes currently annotated to encode hypothetical proteins or proteins designated as unknown or unclassified.
When comparing expression levels of S. Typhi genes detected in our analysis in humans to expression levels of S. Typhi genes in in vitro grown cultures, equilibrating for S. Typhi 16S rRNA, we noted differing levels of S. Typhi mRNA for 65% of the genes detected in humans. In total, 331 S. Typhi transcripts had significantly different levels of detection in at least 4 patients compared to in vitro cultures, and 141 had significant differences in all 5 patients compared to mRNA detected in in vitro cultures. Identified genes were involved in iron (fepB, fepC, fepD), thiamine (thiG), and biotin (bioF) metabolism; use of alternative carbon sources including ethanolamine (eutB, eutC, eutD, eutA, and eutN), oxacelatate (oadAB and oadG), and propranediol (pduB and pduK); and antimicrobial resistance (bacA, mdtC). We also identified these operons in our analysis of S. Paratyphi A, further supporting a potential role of these operons in the pathogenesis of enteric fever [12]. In addition, we identified 24 genes with significantly different levels of expression in in vivo compared to in vitro samples that are not present in the S. Typhimurium genome and may play an important role in S. Typhi pathogenesis, including genes encoded within the Type IV pilus cluster of SPI-7 (i.e. pilO and pilL), and fimbrial proteins staA and steD. Of note, the largest grouping of S. Typhi genes identified in our comparison encoded proteins of unknown or unclassified function.
Our findings are similar to prior Salmonella transcriptional analyses. We previously applied SCOTS-microarray analysis to S. Paratyphi A in the blood of infected humans, and the homologs of 75% of the bacterial transcripts identified in S. Paratyphi A infected patients were also identified in S. Typhi infected patients [12]. SCOTS analysis has also been previously applied to S. Typhi using an ex vivo macrophage model system by Faucher et al. [9]. Similar to our current analysis using blood of infected patients, the ex vivo analysis also detected transcripts of genes involved in intracellular survival including a number of genes encoded within SPI-2, mgtBC in SPI-3, the SPI-1 effector, sopE, and genes involved in antimicrobial peptide resistance. Both analyses suggested a role of SPI-1 beyond invasion of the intestinal epithelium and the potential role of alternative carbon sources in S. Typhi pathogenesis. In contrast to Faucher's analysis, we found higher levels of transcripts of genes involved in iron acquisition and transport in vivo including fes, fhu, feo, iro, and ent. Our detection of these genes may reflect a greater complexity or degree of iron-limitation in the blood of infected humans versus in a cultured macrophage model system.
To our knowledge there has not been a prior analysis of S. Typhi gene expression across the transcriptome in humans. Our results highlight potential survival adaptations of S. Typhi within the human host, including expression of genes required for utilization of alternative carbon and energy sources, divalent cation transport, antimicrobial resistance, and oxidative stress resistance, as well as many genes whose function is currently unknown. Further study of these genes, especially those of unknown function, may further our understanding of S. Typhi pathogenesis and aid in vaccine, diagnostic, and/or drug target development.
Supporting Information
qPCR Primer sequences.
(DOC)
S. Typhi genes whose transcripts were detected in the blood of humans with typhoid fever.
(XLS)
Footnotes
The authors have declared that no competing interests exist.
This work was supported by the ICDDR,B and grants from the National Institutes of Health, including the National Institute of Allergy & Infectious Diseases (AI072599, AI077883 [ETR]; AI058935 [SBC]; AI052237, AI073971, AI075093, AI083964, AI039557, AI077645, AI083646, and BARD IS-4267-09 [MMCC]; A148635 [JEG]; ICDDR,B core funds (FQ, WAB); the PneumoADIP Project of the Johns Hopkins Bloomberg School of Public Health (WAB); a ICDDRB-US Centers for Disease Control and Prevention Cooperative Agreement (WAB); a Training Grant in Vaccine Development from the Fogarty International Center (TW05572 [AS, MSB, FQ]); an American Recovery and Reinvestment Act (ARRA) FIC Post-doctoral Fellowship in Global Infectious Diseases (TW005572-S1 [RCC]); Career Development Awards from the Fogarty International Center (K01 TW007409 [JBH], K01 TW07144 [RCL]), and NIAID (K08 AI089721 [RCC]); and a Physician Scientist Early Career Award from the Howard Hughes Medical Institute (RCL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82:346–353. [PMC free article] [PubMed] [Google Scholar]
- 2.Watson KG, Holden DW. Dynamics of growth and dissemination of Salmonella in vivo. Cell Microbiol. 2010;12:1389–1397. doi: 10.1111/j.1462-5822.2010.01511.x. [DOI] [PubMed] [Google Scholar]
- 3.Song J, Willinger T, Rongvaux A, Eynon EE, Stevens S, et al. A mouse model for the human pathogen Salmonella typhi. Cell Host Microbe. 2010;8:369–376. doi: 10.1016/j.chom.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haraga A, Ohlson MB, Miller SI. Salmonellae interplay with host cells. Nat Rev Microbiol. 2008;6:53–66. doi: 10.1038/nrmicro1788. [DOI] [PubMed] [Google Scholar]
- 5.McClelland M, Sanderson KE, Spieth J, Clifton SW, Latreille P, et al. Complete genome sequence of Salmonella enterica serovar Typhimurium LT2. Nature. 2001;413:852–856. doi: 10.1038/35101614. [DOI] [PubMed] [Google Scholar]
- 6.Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, et al. Complete genome sequence of a multiple drug resistant Salmonella enterica serovar Typhi CT18. Nature. 2001;413:848–852. doi: 10.1038/35101607. [DOI] [PubMed] [Google Scholar]
- 7.Daigle F, Graham JE, Curtiss R., 3rd Identification of Salmonella typhi genes expressed within macrophages by selective capture of transcribed sequences (SCOTS). Mol Microbiol. 2001;41:1211–1222. doi: 10.1046/j.1365-2958.2001.02593.x. [DOI] [PubMed] [Google Scholar]
- 8.Faucher SP, Curtiss R, 3rd, Daigle F. Selective capture of Salmonella enterica serovar Typhi genes expressed in macrophages that are absent from the Salmonella enterica serovar Typhimurium genome. Infect Immun. 2005;73:5217–5221. doi: 10.1128/IAI.73.8.5217-5221.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faucher SP, Porwollik S, Dozois CM, McClelland M, Daigle F. Transcriptome of Salmonella enterica serovar Typhi within macrophages revealed through the selective capture of transcribed sequences. Proc Natl Acad Sci U S A. 2006;103:1906–1911. doi: 10.1073/pnas.0509183103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Graham JE, Clark-Curtiss JE. Identification of Mycobacterium tuberculosis RNAs synthesized in response to phagocytosis by human macrophages by selective capture of transcribed sequences (SCOTS). Proc Natl Acad Sci U S A. 1999;96:11554–11559. doi: 10.1073/pnas.96.20.11554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daigle F, Hou JY, Clark-Curtiss JE. Microbial gene expression elucidated by selective capture of transcribed sequences (SCOTS). Methods Enzymol. 2002;358:108–122. doi: 10.1016/s0076-6879(02)58083-6. [DOI] [PubMed] [Google Scholar]
- 12.Sheikh A, Charles RC, Rollins SM, Harris JB, Bhuiyan MS, et al. Analysis of Salmonella enterica serotype Paratyphi A gene expression in the blood of bacteremic patients in Bangladesh. PLoS Negl Trop Dis. 2010;4:e908. doi: 10.1371/journal.pntd.0000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giannella RA. Salmonella. In: Baron S, editor. Medical Microbiology. Galveston, Texas: University of Texas Medical Branch at Galveston; 1996. [Google Scholar]
- 14.Froussard P. A random-PCR method (rPCR) to construct whole cDNA library from low amounts of RNA. Nucleic Acids Res. 1992;20:2900. doi: 10.1093/nar/20.11.2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rollins SM, Peppercorn A, Young JS, Drysdale M, Baresch A, et al. Application of in vivo induced antigen technology (IVIAT) to Bacillus anthracis. PLoS One. 2008;3:e1824. doi: 10.1371/journal.pone.0001824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charles RC, Harris JB, Chase MR, Lebrun LM, Sheikh A, et al. Comparative proteomic analysis of the PhoP regulon in Salmonella enterica serovar Typhi versus Typhimurium. PLoS One. 2009;4:e6994. doi: 10.1371/journal.pone.0006994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galan JE. Interaction of Salmonella with host cells through the centisome 63 type III secretion system. Curr Opin Microbiol. 1999;2:46–50. doi: 10.1016/s1369-5274(99)80008-3. [DOI] [PubMed] [Google Scholar]
- 18.Groisman EA. The pleiotropic two-component regulatory system PhoP-PhoQ. J Bacteriol. 2001;183:1835–1842. doi: 10.1128/JB.183.6.1835-1842.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kato A, Groisman EA Howard Hughes Medical Institute. The PhoQ/PhoP regulatory network of Salmonella enterica. Adv Exp Med Biol. 2008;631:7–21. doi: 10.1007/978-0-387-78885-2_2. [DOI] [PubMed] [Google Scholar]
- 20.Monsieurs P, De Keersmaecker S, Navarre WW, Bader MW, De Smet F, et al. Comparison of the PhoPQ regulon in Escherichia coli and Salmonella typhimurium. J Mol Evol. 2005;60:462–474. doi: 10.1007/s00239-004-0212-7. [DOI] [PubMed] [Google Scholar]
- 21.Galan JE. Molecular genetic bases of Salmonella entry into host cells. Mol Microbiol. 1996;20:263–271. doi: 10.1111/j.1365-2958.1996.tb02615.x. [DOI] [PubMed] [Google Scholar]
- 22.Hernandez LD, Hueffer K, Wenk MR, Galan JE. Salmonella modulates vesicular traffic by altering phosphoinositide metabolism. Science. 2004;304:1805–1807. doi: 10.1126/science.1098188. [DOI] [PubMed] [Google Scholar]
- 23.Ibarra JA, Steele-Mortimer O. Salmonella–the ultimate insider. Salmonella virulence factors that modulate intracellular survival. Cell Microbiol. 2009;11:1579–1586. doi: 10.1111/j.1462-5822.2009.01368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giacomodonato MN, Uzzau S, Bacciu D, Caccuri R, Sarnacki SH, et al. SipA, SopA, SopB, SopD and SopE2 effector proteins of Salmonella enterica serovar Typhimurium are synthesized at late stages of infection in mice. Microbiology. 2007;153:1221–1228. doi: 10.1099/mic.0.2006/002758-0. [DOI] [PubMed] [Google Scholar]
- 25.Knodler LA, Vallance BA, Celli J, Winfree S, Hansen B, et al. Dissemination of invasive Salmonella via bacterial-induced extrusion of mucosal epithelia. Proc Natl Acad Sci U S A. 2010;107:17733–17738. doi: 10.1073/pnas.1006098107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan Q, Zhang XL, Wu HY, He PW, Wang F, et al. Aptamers that preferentially bind type IVB pili and inhibit human monocytic-cell invasion by Salmonella enterica serovar Typhi. Antimicrob Agents Chemother. 2005;49:4052–4060. doi: 10.1128/AAC.49.10.4052-4060.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang XL, Tsui IS, Yip CM, Fung AW, Wong DK, et al. Salmonella enterica serovar Typhi uses type IVB pili to enter human intestinal epithelial cells. Infect Immun. 2000;68:3067–3073. doi: 10.1128/iai.68.6.3067-3073.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pickard D, Wain J, Baker S, Line A, Chohan S, et al. Composition, acquisition, and distribution of the Vi exopolysaccharide-encoding Salmonella enterica pathogenicity island SPI-7. J Bacteriol. 2003;185:5055–5065. doi: 10.1128/JB.185.17.5055-5065.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stocker BA. Auxotrophic Salmonella typhi as live vaccine. Vaccine. 1988;6:141–145. doi: 10.1016/s0264-410x(88)80017-3. [DOI] [PubMed] [Google Scholar]
- 30.McFarland WC, Stocker BA. Effect of different purine auxotrophic mutations on mouse-virulence of a Vi-positive strain of Salmonella dublin and of two strains of Salmonella Typhimurium. Microb Pathog. 1987;3:129–141. doi: 10.1016/0882-4010(87)90071-4. [DOI] [PubMed] [Google Scholar]
- 31.Blanc-Potard AB, Groisman EA. The Salmonella selC locus contains a pathogenicity island mediating intramacrophage survival. EMBO J. 1997;16:5376–5385. doi: 10.1093/emboj/16.17.5376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papp-Wallace KM, Nartea M, Kehres DG, Porwollik S, McClelland M, et al. The CorA Mg2+ channel is required for the virulence of Salmonella enterica serovar Typhimurium. J Bacteriol. 2008;190:6517–6523. doi: 10.1128/JB.00772-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith RL, Kaczmarek MT, Kucharski LM, Maguire ME. Magnesium transport in Salmonella typhimurium: regulation of mgtA and mgtCB during invasion of epithelial and macrophage cells. Microbiology. 1998;144(Pt 7):1835–1843. doi: 10.1099/00221287-144-7-1835. [DOI] [PubMed] [Google Scholar]
- 34.Zaharik ML, Cullen VL, Fung AM, Libby SJ, Kujat Choy SL, et al. The Salmonella enterica serovar Typhimurium divalent cation transport systems MntH and SitABCD are essential for virulence in an Nramp1 G169 murine typhoid model. Infect Immun. 2004;72:5522–5525. doi: 10.1128/IAI.72.9.5522-5525.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klumpp J, Fuchs TM. Identification of novel genes in genomic islands that contribute to Salmonella typhimurium replication in macrophages. Microbiology. 2007;153:1207–1220. doi: 10.1099/mic.0.2006/004747-0. [DOI] [PubMed] [Google Scholar]
- 36.Stojiljkovic I, Baumler AJ, Heffron F. Ethanolamine utilization in Salmonella typhimurium: nucleotide sequence, protein expression, and mutational analysis of the cchA cchB eutE eutJ eutG eutH gene cluster. J Bacteriol. 1995;177:1357–1366. doi: 10.1128/jb.177.5.1357-1366.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conner CP, Heithoff DM, Julio SM, Sinsheimer RL, Mahan MJ. Differential patterns of acquired virulence genes distinguish Salmonella strains. Proc Natl Acad Sci U S A. 1998;95:4641–4645. doi: 10.1073/pnas.95.8.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maier RJ, Olczak A, Maier S, Soni S, Gunn J. Respiratory hydrogen use by Salmonella enterica serovar Typhimurium is essential for virulence. Infect Immun. 2004;72:6294–6299. doi: 10.1128/IAI.72.11.6294-6299.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zbell AL, Maier SE, Maier RJ. Salmonella enterica serovar Typhimurium NiFe uptake-type hydrogenases are differentially expressed in vivo. Infect Immun. 2008;76:4445–4454. doi: 10.1128/IAI.00741-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cain BD, Norton PJ, Eubanks W, Nick HS, Allen CM. Amplification of the bacA gene confers bacitracin resistance to Escherichia coli. J Bacteriol. 1993;175:3784–3789. doi: 10.1128/jb.175.12.3784-3789.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishino K, Latifi T, Groisman EA. Virulence and drug resistance roles of multidrug efflux systems of Salmonella enterica serovar Typhimurium. Mol Microbiol. 2006;59:126–141. doi: 10.1111/j.1365-2958.2005.04940.x. [DOI] [PubMed] [Google Scholar]
- 42.Parra-Lopez C, Baer MT, Groisman EA. Molecular genetic analysis of a locus required for resistance to antimicrobial peptides in Salmonella Typhimurium.. EMBO J. 1993;12:4053–4062. doi: 10.1002/j.1460-2075.1993.tb06089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gunn JS, Ryan SS, Van Velkinburgh JC, Ernst RK, Miller SI. Genetic and functional analysis of a PmrA-PmrB-regulated locus necessary for lipopolysaccharide modification, antimicrobial peptide resistance, and oral virulence of Salmonella enterica serovar Typhimurium. Infect Immun. 2000;68:6139–6146. doi: 10.1128/iai.68.11.6139-6146.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baker SJ, Gunn JS, Morona R. The Salmonella typhi melittin resistance gene pqaB affects intracellular growth in PMA-differentiated U937 cells, polymyxin B resistance and lipopolysaccharide. Microbiology. 1999;145(Pt 2):367–378. doi: 10.1099/13500872-145-2-367. [DOI] [PubMed] [Google Scholar]
- 45.Detweiler CS, Monack DM, Brodsky IE, Mathew H, Falkow S. virK, somA and rcsC are important for systemic Salmonella enterica serovar Typhimurium infection and cationic peptide resistance. Mol Microbiol. 2003;48:385–400. doi: 10.1046/j.1365-2958.2003.03455.x. [DOI] [PubMed] [Google Scholar]
- 46.Bjur E, Eriksson-Ygberg S, Aslund F, Rhen M. Thioredoxin 1 promotes intracellular replication and virulence of Salmonella enterica serovar Typhimurium. Infect Immun. 2006;74:5140–5151. doi: 10.1128/IAI.00449-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spector MP, Garcia del Portillo F, Bearson SM, Mahmud A, Magut M, et al. The rpoS-dependent starvation-stress response locus stiA encodes a nitrate reductase (narZYWV) required for carbon-starvation-inducible thermotolerance and acid tolerance in Salmonella typhimurium. Microbiology. 1999;145(Pt 11):3035–3045. doi: 10.1099/00221287-145-11-3035. [DOI] [PubMed] [Google Scholar]
- 48.Buchmeier NA, Lipps CJ, So MY, Heffron F. Recombination-deficient mutants of Salmonella typhimurium are avirulent and sensitive to the oxidative burst of macrophages. Mol Microbiol. 1993;7:933–936. doi: 10.1111/j.1365-2958.1993.tb01184.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
qPCR Primer sequences.
(DOC)
S. Typhi genes whose transcripts were detected in the blood of humans with typhoid fever.
(XLS)