Abstract
Currently, the role of ultrasound (US) in anaesthesia-related airway assessment and procedural interventions is encouraging, though it is still ill defined. US can visualise anatomical structures in the supraglottic, glottic and subglottic regions. The floor of the mouth can be visualised by both transcutaneous view of the neck and also by transoral or sublinguial views. However, imaging the epiglottis can be challenging as it is suspended in air. US may detect signs suggestive of difficult intubation, but the data are limited. Other possible applications in airway management include confirmation of correct endotracheal tube placement, prediction of post-extubation stridor, evaluation of soft tissue masses in the neck prior to intubation, assessment of subglottic diameter for determination of paediatric endotracheal tube size and percutaneous dilatational tracheostomy. With development of better probes, high-resolution imaging, real-time picture and clinical experience, US has become the potential first-line noninvasive airway assessment tool in anaesthesia and intensive care practice.
Keywords: Airway, ultrasonography, upper respiratory tract
INTRODUCTION
Ultrasound (US) imaging technique has recently emerged as a novel, simple, portable, noninvasive tool helpful for airway assessment and management. Initial few reports published were on soft tissue imaging of neck, focussing on pre-tracheal structure and anterior tracheal wall. In the last few years, there have been some reports and a study that described various roles of US imaging in airway management.[1–4] It helps in rapid assessment of the airway anatomy, not only in operation theatre but also in the intensive care unit and emergency department. Various clinical applications of US imaging of the upper airway include identification of endotracheal tube (ETT) placement,[5] guidance of percutaneous tracheostomy[6,7] and cricothyroidotomy,[8] detection of subglottic stenosis,[9] prediction of difficult intubation[10] and post-extubation stridor,[11] prediction of paediatric ETT[12] and double-lumen tube (DLT) size.[13] This article highlights briefly the review of various published data on the role of US in airway assessment and management.
Accurate interpretation of US images requires a basic understanding of the physical principles involved in US image generation. In addition, transducer selection, orientation and anatomy of airway relevant to US imaging is important to evaluate anatomy of the airway.
US is the acoustic frequency above the threshold for human hearing (20 kHz). In medical practice, high-frequency pulses of sound waves are used (2.5–10 MHz).[14] The probe that generates this wave contains material that produces piezoelectric effect. Lower the frequency, higher is the penetrance of tissues but lower is the potential image resolution. Depending on the shape and configuration of the probe, different shaped fields of view are generated. Two types of probes commonly used are linear and curved. Standard 7.5 MHz linear probe and 5 MHz curved array probe are commonly used for visualisation of superficial and deeper structures of the airway, respectively. Reflection, refraction, scatter, absorption and transmission of sound occur as it passes through soft tissue structures, allowing characterisation of the shape and internal architecture of that structure in addition to those behind it. Reflection of sound is marked at interfaces between tissues of different acoustic impedance. The image is built from the reflected sound signals.
POSITION OF THE PATIENT
Patients should be placed in supine sniffing position with a pillow under the occiput to achieve optimum head extension and neck flexion.
ORIENTATION OF TRANSDUCER IN NECK
Sagittal view (longitudinally in the midline)
Parasagittal view (longitudinally lateral to the midline)
Transverse view (transversely across the anterior surface of the neck)
APPEARANCES OF DIFFERENT MEDIUMS OF THE AIRWAY
Air is a poor US medium and does not allow visualisation of deeper structures. Intraluminal air produces both comet tail and reverberation artefacts. Bony structures like mentum, rami of the mandible, hyoid bone, and sternum appear as bright hyperechoic linear structures with a hypoechoic acoustic shadow underneath. Cartilaginous structures (thyroid and cricoid cartilages) are homogeneously hypoechoic. Muscle and connective tissue have hypoechoic, heterogeneous striated appearance. Fat and glandular structures are homogeneous and mildly to strongly hyperechoic in comparison with adjacent soft tissues, depending on the fat content in the glandular parenchyma. Air–mucosa (A–M) interface has a bright hyperechoic linear appearance.
SONOANATOMY OF THE UPPER AIRWAY
Oral and nasal cavities, pharynx, larynx, and trachea are nearly completely filled with air. However, various other structures can be visualised in relation to their anatomic location.
Epiglottis Epiglottis (E) in the transverse and parasagittal views through the thyrohyoid membrane (THM) is visible as a hypoechoic curvilinear structure[2] [Figures 1 and 2]. Its anterior border is demarcated by the hyperechoic pre-epiglottic space (PES) and its posterior border by a bright linear A–M interface. Any interface between the mucosa lining the upper airway and the air within it produces a bright hyperechoic linear appearance. Epiglottis can be easily identified in almost all individuals in the transverse plane with a varying cephalad or caudad angulation of the linear transducer. Due to acoustic shadowing by the hyoid bone, it is not easy to visualise epiglottis in the parasagittal plane.[2] Extended submandibular sagittal view (between the hyoid bone and mentum) using a curved transducer can also identify epiglottis [Figure 3]. Identification of the epiglottis can be facilitated by tongue protrusion and swallowing, when it becomes visible as a discrete mobile structure inferior to the base of the tongue.[2]
Figure 1.
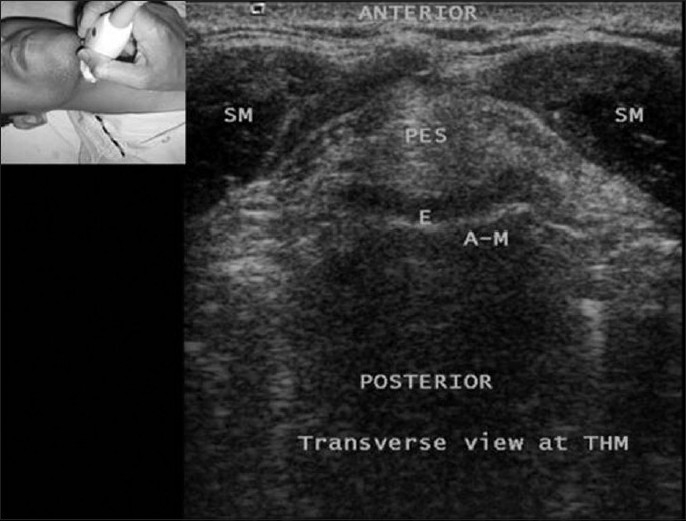
Transverse view at thyrohyoid membrane (THM). E = Epiglottis, A–M = Air–mucosal interface, PES = Pre-epiglottic space, SM = Strap muscles
Figure 2.
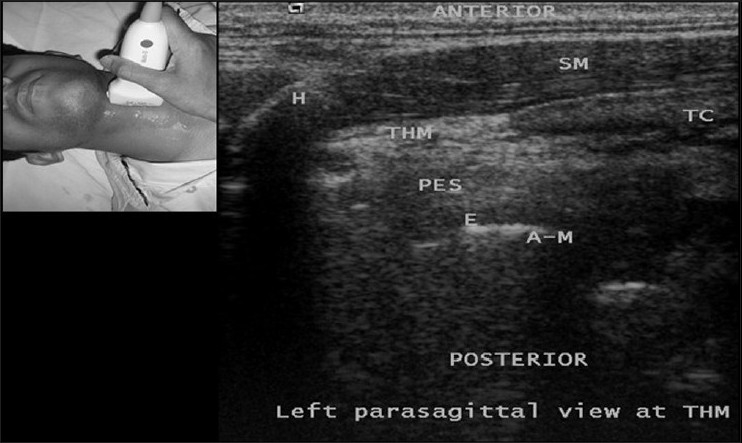
Left parasagittal view at thyrohyoid membrane (THM). H = Hyoid bone, SM = Strap muscles, THM = Thyrohyoid membrane, TC = Thyroid cartilage, PES = Pre-epiglottic space, E = Epiglottis, A–M = Air mucosal interface
Figure 3.
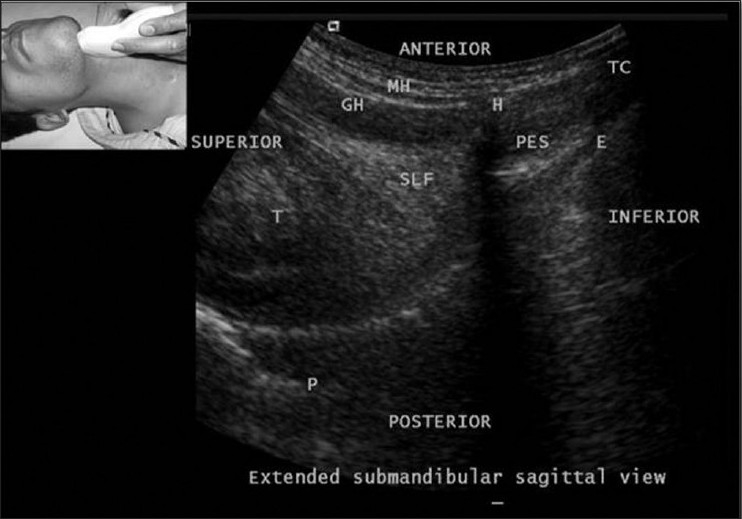
Extended submandibular sagittal view using a curved transducer. T = Tongue, H = Hyoid bone, E = Epiglottis, GG = Genioglossus, GH = Geniohyoid, MH = Mylohyoid, PES = Pre-epiglottic space, P = Palate, TC = Thyroid cartilage
Tongue and floor of the mouth
The tongue (T) can be visualised deeper to the muscles of the floor of the mouth [Figures 3 and 4]. The dorsal surface of the tongue has a curvilinear hyperechoic appearance due to an A–M interface. The intrinsic muscles of the tongue give it a striated appearance on sonography. On the other hand, extrinsic muscles of the tongue that can be visualised with sonography are geniohyoid (GH), genioglossus (GG), and hyoglossus (HG). Rest of the muscles is obscured by the mandibular ramus and the mastoid. In sagittal view, the mylohyoid (MH) and geniohyoid muscles appear as linear hypoechoic bands extending between the mandible and the hyoid bone. The genioglossus and hyoglossus muscles lay deep to the geniohyoid muscle and are seen running in a fanlike fashion towards the dorsal surface of the tongue[2] [Figure 4].
Figure 4.
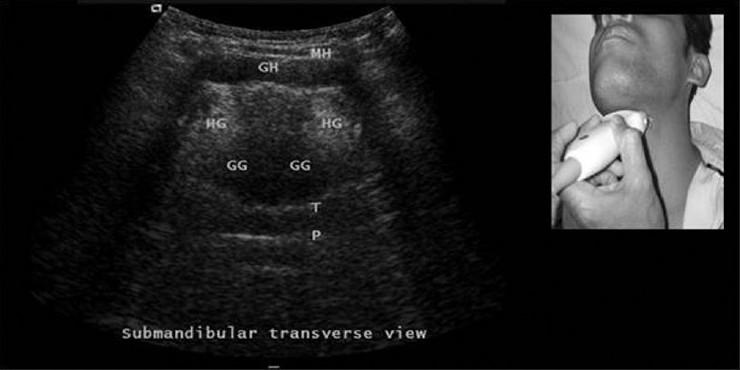
Transverse views at the submandibular position. GG = Genioglossus, GH = Geniohyoid, MH = Mylohyoid, HG = Hyoglossus, T = Tongue, P = Palate
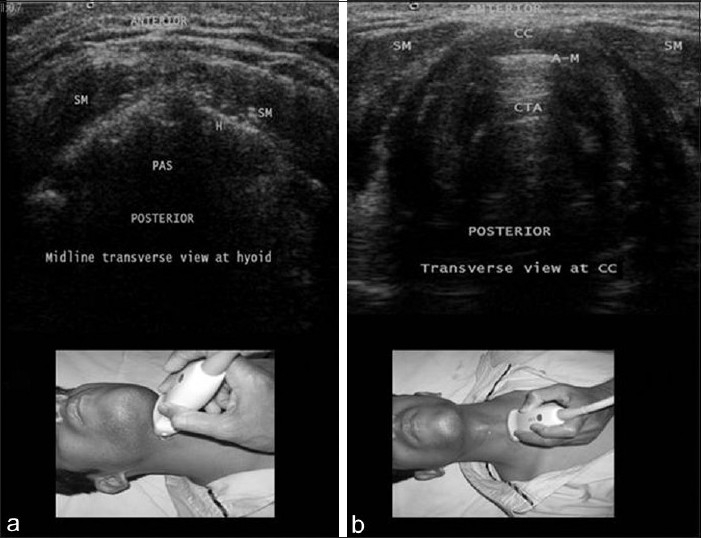
Hyoid bone
Both transverse and sagittal views can be used for visualisation of hyoid bone. The hyoid bone (H) is visible on the transverse view as a superficial hyperechoic inverted U-shaped linear structure with posterior acoustic shadowing [Figure 5a]. On the sagittal, parasagittal and extended submandibular views, the hyoid bone has a narrow hyperechoic curved structure that casts an acoustic shadow [Figure 2]. In the sublingual imaging approach described by Tsui et al., hyperechoic structure originally thought to be the epiglottis was actually the hyoid bone.[3,4]
Figure 5.
(a) Midline transverse view at hyoid. (b) Transverse view at cricoid cartilage. SM = Strap muscles, CC = Cricoid cartilage, A–M = Air mucosal interface, CTA = Comet tail artefacts, PAS = Posterior acoustic shadow
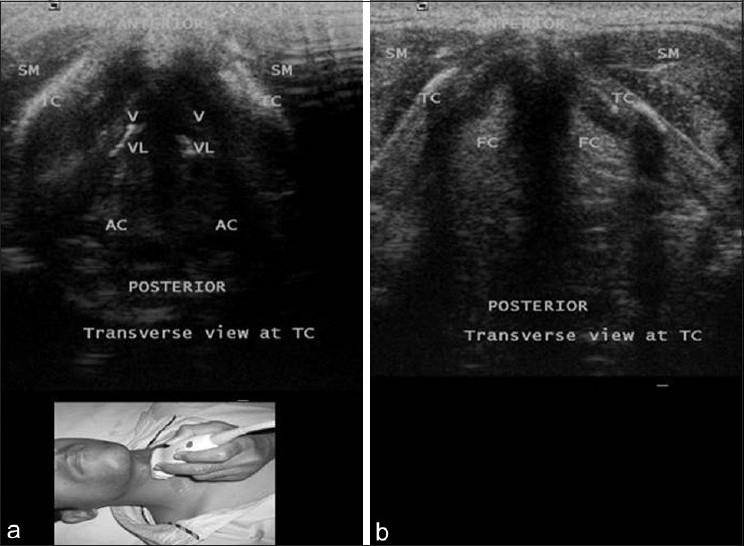
Vocal cords
Thyroid cartilage (TC) provides the best window to view the vocal cords. Vocal cords are seen forming an isosceles triangle with a central tracheal shadow. Vocal cords are delineated medially by the hyperechoic vocal ligaments (VL).[2,5] The false vocal cords (FC) lie parallel and cephalad to the true cords and are more hyperechoic in appearance [Figure 5a and b]. During phonation, the true cords oscillate and move towards the midline when compared to the false cords, which remain relatively immobile. Vocal cord movement can be better visualised with a 3D probe with fluid interface (water bath) between the 3D probe and skin [Figure 6].
Figure 6.
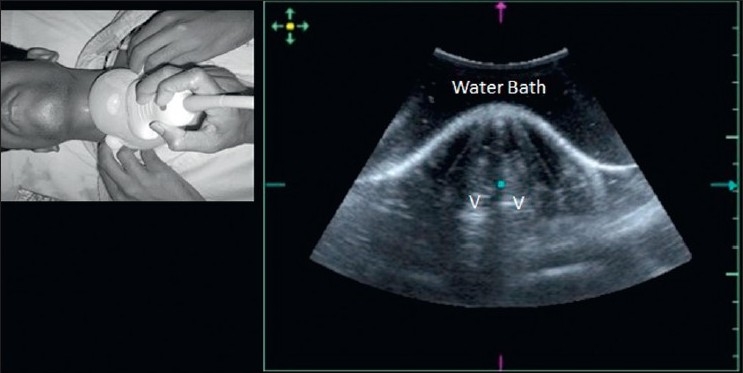
Vocal cords view with 3D probe with fluid interface (water bath) between probe and skin. V = Vocal cord
Cricoid cartilage and cricothyroid membrane
The cricoid cartilage (CC) has an oval hypoechoic appearance in the parasagittal view [Figure 7a and b] and can be seen as a hump in the transverse view [Figure 8b]. The posterior surface of its anterior wall is delineated by a bright A–M interface as well as reverberation artefacts from intraluminal air (CTA). The cricothyroid membrane (CTM) is seen on sagittal and parasagittal views as a hyperechoic band linking the hypoechoic thyroid and cricoid cartilages[2] [Figure 7b]. The tracheal rings (T1, T2, T3) have a hyperechoic appearance. On the parasagittal and sagittal views, they resemble a “string of beads” [Figure 7a and b] and on the transverse view they form an inverted U highlighted by a linear hyperechoic A–M interface and reverberation artefact posteriorly.[2,11]
Figure 7.
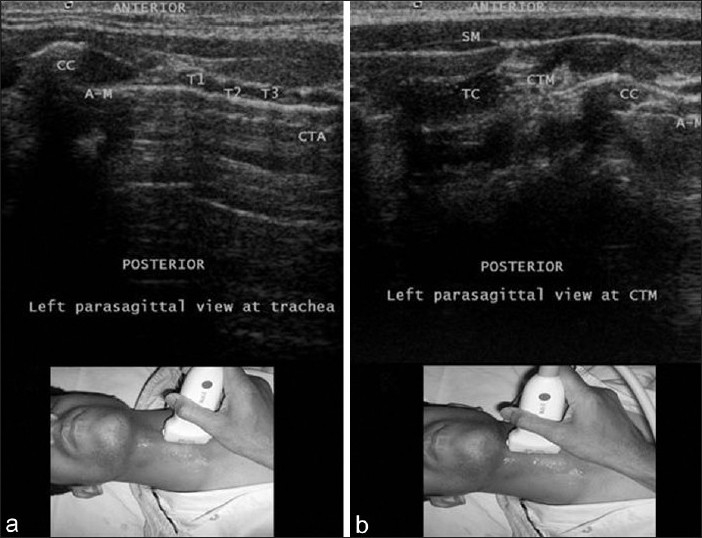
(a) Left parasagittal view at trachea. (b) Left parasagittal view at cricothyroid membrane. CC = Cricoid cartilage, T1–T3 = Tracheal cartilages, A–M = Air-mucosal interface, CTA = Comet tail artefact
Figure 8.
Transverse view at thyroid cartilage. AC = Arytenoid cartilage, TC = Thyroid cartilage, SM = Strap muscles, VL = Vocal ligaments, V = Vocalis muscle, FC = False cord
Thyroid gland
At the level of the suprasternal notch (SSN) in the transverse view, the two lobes and isthmus (Is) of the thyroid gland (TG) can be visualised anterolateral to the trachea [Figures 9 and 10a]. The normal thyroid parenchyma has a characteristically homogeneous US appearance which is more echogenic (hyperechoic) than the adjacent strap muscle. In the oblique transverse view [Figure 10b], other relevant neck structures like oesophagus (Eo), vertebral bodies (VB) and internal carotid artery (ICA) can be easily identified lying lateral to the thyroid gland.
Figure 9.
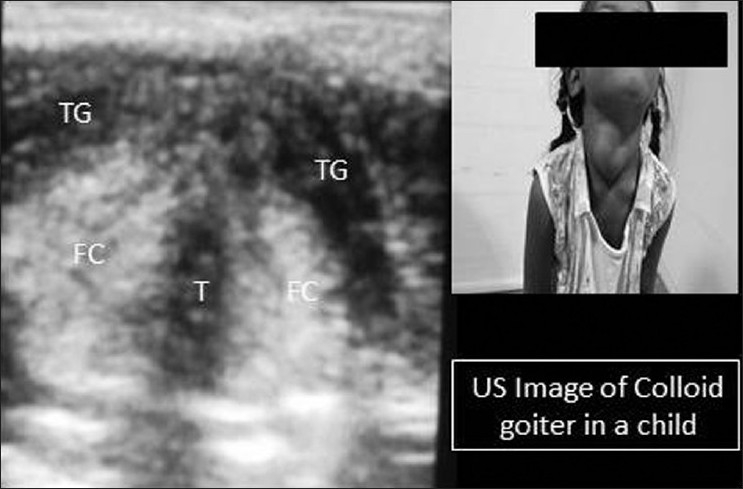
Transverse view of US image at thyroid cartilage (TC) in a child with colloid goitre. TG = Thyroid gland (colloid), FC = False cord, T = Trachea
Figure 10.
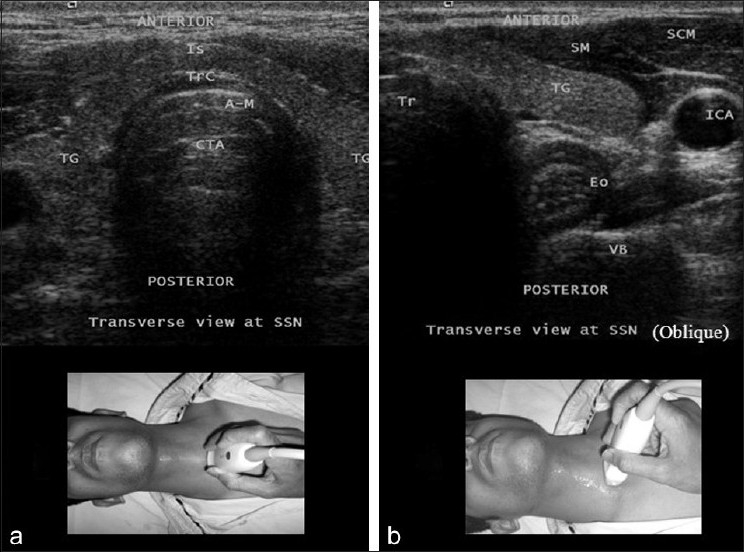
Transverse (a) and oblique transverse view (b) at the level of the suprasternal notch (SSN) showing trachea, thyroid gland, and oesophagus. TG = Thyroid gland, Tr = Trachea, Trc = Tracheal cartilage, A–M = Air–mucosal interface, CTA = Comet tail artefact, ICA = Internal carotid artery, Eo = Oesophagus, SCM = Sternocleidomastoid muscle, SM = Strap muscle, VB = Vertebral body
Oesophagus
Oesophagus is seen in the oblique transverse view at the level of the suprasternal notch posterolateral to the trachea [Figure 10b]. The identification of the oesophagus can be made easy by asking the patient to swallow, which results in visible peristaltic movement of the oesophageal lumen.[2]
APPLICATIONS OF THE ULTRASOUND IN AIRWAY MANAGEMENT
Assessment of the diameter of the subglottic upper airway and prediction of endotracheal tube size
Ultrasonography has emerged as a reliable tool for assessing the narrowest diameter of the cricoid lumen (transverse diameter). Lakhal et al.,[9] compared the transverse diameter of the cricoid lumen assessed by ultrasonography and magnetic resonance imaging in healthy young adults and found it a reliable tool to assess the diameter of the subglottic upper airway. Age-dependent calcification of the laryngeal cartilages begins to occur in the third decade of life, creating an acoustic shadow, an important limitation of laryngeal ultrasonography in older patients.[9] In paediatric patients, subglottic upper airway diameter measured by ultrasonography is a good predictor of correct cuffed and uncuffed ETT sizes.[12]
Prediction of difficult laryngoscopy in obese patients
US measurement of anterior neck soft tissues helps in predicting difficult laryngoscopy in obese patients. The distance from the skin to the anterior aspect of the trachea is measured at three levels: Vocal cords, thyroid isthmus, and suprasternal notch. The amount of soft tissue at each level can be calculated by averaging the amount of soft tissue in millimetres obtained in the central axis of the neck and 15 mm to the left and right. The authors found that pretracheal soft tissue at the level of the vocal cords is a good predictor of difficult laryngoscopy in obese patients. Patients who had more pretracheal soft tissue (28 mm) and a greater neck circumference (50 cm) at the level of vocal cords had difficulty in laryngoscopy.[10]
Role of ultrasound in percutaneous dilatational tracheostomy
Accurate identification of anterior neck structures during percutaneous dilatational tracheostomy can eliminate potential dreaded complications like haemorrhage, tracheal stenosis, erosion into high mediastinal vessels and injury to the thyroid isthmus.[6,7] Although structures within or behind the trachea are not seen, much useful information may be obtained regarding pre- and para-tracheal anatomy using US. Before proceeding for percutaneous dilatational tracheostomy, the pretracheal area should be examined for tracheal midline, approximate level of tracheal cartilages, anterior jugular veins (its diameter and location, i.e. in or near the midline), thyroid isthmus, vulnerable thyroid vessels and any other aberrant vessels. With advanced US technology, it will be possible in the future to have the real-time guidance in the placement of dilators and tracheostomy tubes.
Prediction of post-extubation stridor
Laryngeal ultrasonography is a useful noninvasive tool for the evaluation of vocal cords and laryngeal morphology in intubated patients. The air-column width measured by US may potentially identify patients at risk for post-extubation stridor, in whom caution should be exercised after extubation.[11] The authors identified that after cuff deflation, an air-column width of 4.5 (0.8) mm was associated with post-extubation stridor while patients who did not develop stridor had an air-column width of 6.4 (2) mm.
Elective transtracheal cannulation and emergency cricothyrotomy
Successful location of the trachea plays an important part in managing the difficult airway for both elective and emergency cases. US imaging helps to identify the trachea prior to both elective transtracheal cannulation and emergency cricothyrotomy.[8] This is particularly helpful in situations where localising the trachea is difficult due to neck mass or any other swelling, for example, huge thyroid swelling, Ludwig's angina, etc.
Ultrasound-guided upper airway anaesthesia to facilitate awake intubation
Superior laryngeal nerve, located between the hyoid bone and thyroid cartilage, can be easily visualised on transverse ultrasonographic section across the hyoid bone. The membrane between the hyoid bone and thyroid cartilage is an isoechogenic line (with hyperechogenic air below) from both sides of the hyoid bone.[15]
Endotracheal intubation, oesophageal intubation and double-lumen bronchial tube (DLT) placement
Most frequently used methods of confirmation of endotracheal intubation are auscultation of chest, end-tidal carbon dioxide detection and by oesophageal intubating devices. US imaging can visualise the motion of the diaphragm and pleura indicating lung expansion, an indirect but dynamic anatomic evidence of the correct physiologic function of the ETT in paralysed or apnoeic patients. Bilateral equal motion of the diaphragm towards the abdomen can be seen by US if the ETT is inside the trachea. Further, with intercostal ultrasonographic view at the lung–chest wall interface, “to-and-fro” movement of the pleura synchronised with ventilation (lung-sliding sign) can be visualised.[1,16,17]
Oesophageal intubation will result in an immobile or paradoxical state of the diaphragm. Ventilation through oesophageal-positioned ETT can also result in a paradoxical motion of the diaphragm, in which the diaphragm moves towards the chest due to increased intra-abdominal pressure as a result of distension of stomach caused by the positive pressure ventilation.[1]
Endobronchial intubation also can be diagnosed by movement of the diaphragm and presence of lung-sliding sign on the ventilated lung (endobronchial) and absent or restricted movement of the diaphragm and absence of lung-sliding sign on the contralateral side (non-ventilated lung).[1]
Cuff inflation with saline instead of air to detect position of the ETT in case of an already trachea-intubated patient has been described.[5] The authors suggested that a longitudinal view combined with a slight to-and-fro motion could improve visualisation. They concluded that this technique was beneficial particularly in pregnant women or patients receiving frequent chest radiographs to monitor ETT position.
Real-time characteristic ultrasonographic findings of the normal paediatric airway during tracheal intubation have been described using the following criteria: 1) identification of the trachea and tracheal rings, 2) visualisation of vocal cords, 3) widening of glottis as the tracheal tube passes through, and 4) tracheal tube position above carina and demonstration of sliding sign after manual ventilation of the lungs. The authors conclude that US of the paediatric airway can be easily used to assess correct tracheal tube position and to detect oesophageal intubation.[18]
Predicting the size of a left double-lumen bronchial tube: Measurement of the outer tracheal width by US can be a useful method for predicting the diameter of left main bronchus and for selecting a left-side double-lumen bronchial tube. The authors found a strong correlation between tracheal widths as measured by US and tracheal width and left main bronchus width as measured by computed tomography (CT).[13]
Detection of laryngeal mask airway position
Ultrasonography has been used to confirm the position of the laryngeal mask airway (LMA) cuff. Proper cuff position to seal the larynx is required for adequate ventilation through the LMA. The LMA cuff was inflated with fluid and the position of the LMA cuff was seen by US from the lateral approach. If the LMA was not visualised by US equally on both sides of the larynx, it can be subsequently repositioned correctly.[14]
Diagnosis of upper airway pathologies
Maxillary sinusitis can be detected before planning for nasal intubation.[19] The maxillary sinus is bounded by the orbital floor superiorly, the hard palate inferiorly, the nasal wall medially, and the zygoma laterally. Normally, sinus is air filled, thus impairing the transmission of US. The only part seen is the anterior wall, with some artefact known as acoustic shadowing which obscures all the underlying structures. When filled with fluid, US penetrates the anterior wall, “travels” through the fluid, and strikes the posterior or lateral walls and “reflects” back to the transducer, resulting in an image of the sinus cavity. This is known as a “sinusogram”. A partial sinusogram, where only the posterior wall or a side wall is seen, can occur due to the presence of an air–fluid level in the sinus or mucosal thickening. Patient should be positioned in a semi-recumbent or upright position, so that the fluid (if present) will follow gravity and cover the floor of the sinus, coming in contact with the anterior wall.[20]
Assessment and diagnosis of inflammatory conditions of the upper airway like epiglottitis, presence of mucosal swelling and vocal cord function have also been assessed using an US.[21]
The scope of US application in anaesthesia has widened considerably. A sound knowledge of the sonoanatomy of the upper airway can help the anaesthetist to use US in many airway-related conditions. Transverse and parasagittal views can help diagnose supraglottic, glottic and infraglottic airway conditions and aid the anaesthetist in airway management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sustic A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med. 2007;3:173–7. doi: 10.1097/01.CCM.0000260628.88402.8A. [DOI] [PubMed] [Google Scholar]
- 2.Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: An observational study. J Ultrasound Med. 2010;29:79–85. doi: 10.7863/jum.2010.29.1.79. [DOI] [PubMed] [Google Scholar]
- 3.Tsui BC, Hui CM. Sublingual airway ultrasound imaging. Can J Anaesth. 2008;55:790–1. doi: 10.1007/BF03016357. [DOI] [PubMed] [Google Scholar]
- 4.Tsui BC, Hui CM. Challenges in sublingual airway ultrasound interpretation. Can J Anaesth. 2009;56:393–4. doi: 10.1007/s12630-009-9077-y. [DOI] [PubMed] [Google Scholar]
- 5.Raphael DT, Conard FU., 3rd Ultrasound confirmation of endotracheal tube placement. J Clin Ultrasound. 1987;15:459–62. doi: 10.1002/jcu.1870150706. [DOI] [PubMed] [Google Scholar]
- 6.Hatfield A, Bodenham A. Portable ultrasonic scanning of the anterior neck before percutaneous dilatational tracheostomy. Anaesthesia. 1999;54:660–3. doi: 10.1046/j.1365-2044.1999.00859.x. [DOI] [PubMed] [Google Scholar]
- 7.Sustić A, Kovac D, Zgaljardić Z, Zupan Z, Krstulović B. Ultrasound-guided percutaneous dilatational tracheostomy: A safe method to avoid cranial misplacement of the tracheostomy tube. Intensive Care Med. 2000;26:1379–81. doi: 10.1007/s001340000589. [DOI] [PubMed] [Google Scholar]
- 8.Orr JA, Stephens RS, Mitchell VM. Ultrasound-guided localization of the trachea. Anaesthesia. 2007;62:972–3. doi: 10.1111/j.1365-2044.2007.05244.x. [DOI] [PubMed] [Google Scholar]
- 9.Lakhal K, Delplace X, Cottier JP, Tranquart F, Sauvagnac X, Mercier C, et al. The feasibility of ultrasound to assess subglottic diameter. Anaesth Analg. 2007;104:611–4. doi: 10.1213/01.ane.0000260136.53694.fe. [DOI] [PubMed] [Google Scholar]
- 10.Ezri T, Gewurtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58:1111–4. doi: 10.1046/j.1365-2044.2003.03412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ding LW, Wang HC, Wu HD, Chang CJ, Yang PC. Laryngeal ultrasound: A useful method in predicting post-extubation stridor. A pilot study. Eur Respir J. 2006;27:384–9. doi: 10.1183/09031936.06.00029605. [DOI] [PubMed] [Google Scholar]
- 12.Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113:819–24. doi: 10.1097/ALN.0b013e3181ef6757. [DOI] [PubMed] [Google Scholar]
- 13.Sustić A, Miletić D, Protić A, Ivancić A, Cicvarić T. Can ultrasound be useful for predicting the size of a left double-lumen bronchial tube? Tracheal width as measured by ultrasonography versus computed tomography. J Clin Anesth. 2008;20:247–52. doi: 10.1016/j.jclinane.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Hatfield A, Bodenham A. Ultrasound: An emerging role in anaesthesia and intensive care. Br J Anaesth. 1999;83:789–800. doi: 10.1093/bja/83.5.789. [DOI] [PubMed] [Google Scholar]
- 15.Green JS, Tsui BC. Applications of ultrasonography in ENT: Airway assessment and nerve blockade. Anesthesiol Clin. 2010;28:541–53. doi: 10.1016/j.anclin.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Lichtenstein D, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill: Lung sliding. Chest. 1995;108:1345–8. doi: 10.1378/chest.108.5.1345. [DOI] [PubMed] [Google Scholar]
- 17.Chun R, Kirkpatrick AW, Sirois M, Sargasyn AE, Melton S, Hamilton DR, et al. Where's the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med. 2004;19:366–9. doi: 10.1017/s1049023x00002004. [DOI] [PubMed] [Google Scholar]
- 18.Marciniak B, Fayoux P, Hébrard A, Krivosic-Horber R, Engelhardt T, Bissonnette B. Airway management in children: Ultrasonography assessment of tracheal intubation in real time? Anesth Analg. 2009;108:461–5. doi: 10.1213/ane.0b013e31819240f5. [DOI] [PubMed] [Google Scholar]
- 19.Lichtenstein D, Biderman P, Meziere G, Gepner A. Sinusogram, a real time ultrasound sign of maxillary sinusitis. Intensive Care Med. 1998;24:1057–61. doi: 10.1007/s001340050716. [DOI] [PubMed] [Google Scholar]
- 20.Butcher C. Ultrasound evaluation of the neck and upper respiratory system. In: Levitov A, Mayo P, Slonim A, editors. Critical Care Ultrasonography. 1st ed. USA: McGraw.Hill; 2010. pp. 235–8. [Google Scholar]
- 21.Friedman EM. Role of ultrasound in the assessment of vocal cord function in infants and children. Ann Otol Rhinol Laryngol. 1997;106:199–209. doi: 10.1177/000348949710600304. [DOI] [PubMed] [Google Scholar]


