Abstract
Modern anaesthesia practice in children was made possible by the invention of the endotracheal tube (ET), which made lengthy and complex surgical procedures feasible without the disastrous complications of airway obstruction, aspiration of gastric contents or asphyxia. For decades, endotracheal intubation or bag-and-mask ventilation were the mainstays of airway management. In 1983, this changed with the invention of the laryngeal mask airway (LMA), the first supraglottic airway device that blended features of the facemask with those of the ET, providing ease of placement and hands-free maintenance along with a relatively secure airway. The invention and development of the LMA by Dr. Archie Brain has had a significant impact on the practice of anaesthesia, management of the difficult airway and cardiopulmonary resuscitation in children and neonates. This review article will be a brief about the clinical applications of supraglottic airways in children.
Keywords: Difficult airway, laryngeal mask airway, paediatric airway, proseal laryngeal mask airway, supraglottic airways
INTRODUCTION
Supraglottic airway management devices comprise a family of medical devices that facilitate oxygenation and ventilation without endotracheal intubation.[1] The word “supraglottic” means “above the glottis” or “above the larynx”. Some of the authors refer to these products as “extraglottic” devices. “Supraglottic airway” is a generic description for devices that facilitate ventilation and oxygenation with devices that do not penetrate the vocal cords. Classification of these devices can be constructed based on the laryngeal sealing mechanism of each device or by the evolution of the devices.
CLASSIFICATION FOR SUPRAGLOTTIC AIRWAYS BASED ON SEALING MECHANISMS
Perilaryngeal sealers: The LMA family, i-gel and air-Q Intubating Laryngeal Airway (airQ ILA)[2]
Pharyngeal sealers: Combitube, the Streamlined Liner of the Pharynx Airway (SLIPA), the Laryngeal Tube
Both: The Cobra Perilaryngeal Airway (CobraPLA)
CLASSIFICATION OF SUPRAGLOTTIC AIRWAY BASED ON EVOLUTION
1. First-generation devices: Simple airway tubes[2]
The laryngeal mask airway [classic LMA (cLMA)], flexible LMA (fLMA), unique LMA (ULMA) and The Cobra Perilaryngeal Airway (CobraPLA)
2. Second-generation devices: With addition of Drainage tube
Proseal LMA (PLMA), i-gel, Laryngeal tube, LMA Supreme, Streamlined Liner of the Pharyngeal Airway (SLIPA)
A variety of Supraglottic Airway Devices (SAD) have been developed that can be placed blindly, and reliably provide secure oxygenation and ventilation, some with the capability of secure conversion to an endotracheal tube. Advantages of these devices include higher seal pressures (allowing higher ventilation pressure), ease of insertion, the ability to drain gastric fluid and the ability to avoid cervical spine neck extension to visualize the larynx. New commercial supraglottic devices are regularly introduced for clinical use, and over 25 versions are currently available from multiple manufacturers. The ideal supraglottic device must be easy to insert with an easy learning curve, with the ability to ventilate at high peak pressures without gastric distension having the provision to drain the stomach. For many SADs, with the exception of the cLMA and PLMA, there is a lack of high-quality data of efficacy in children. The best evidence requires a randomized controlled trial comparing a new device against an established alternative, properly powered to detect clinically relevant differences in clinically important outcomes. Such studies in children are very rare. Safety data is even harder to establish, particularly for rare events such as aspiration. Therefore, most safety data comes from extended use rather than high-quality evidence, which inevitably biases against newer devices. For reason of these factors, claims of efficacy and, particularly, safety must be interpreted cautiously. Therefore, in this article, the Laryngeal Mask Airway and its family will be discussed in detail, with a brief mention of other SAD.
LARYNGEAL MASK AIRWAY IN CHILDREN
The Laryngeal mask airway[3] (LMA) North America Inc. has formed a very important part of the airway management of adults and, now, children. Early trials of the Pediatric LMA note that the design was a scaled down version of the adult LMA and not anatomically designed for children. Moreover, it was clear that the range of available sizes was inadequate. Since then, improvements in the design and availability of suitable sizes (from the smallest size 1 for wt. 0–5 kg to the older child, size 3 of weight 50 kg), together with favourable clinical experiences have led to the increasing use of LMA in children. As the LMA can be inserted easily without the use of muscle relaxants and provides a secure airway, it is increasingly used where a facemask was previously used. It is seen to replace the tracheal tube in a lot of situations as its use with controlled ventilation has also become accepted practice (Proseal LMA). The presence of a drain tube, which helps to empty the stomach in the Proseal version of the LMA, has set aside fears of distension of the stomach with gas during controlled or spontaneous ventilation, leading to impairment of respiration, especially in a smaller child.
LMA FAMILY
The different types of LMA available are: [Figure 1]
Figure 1.
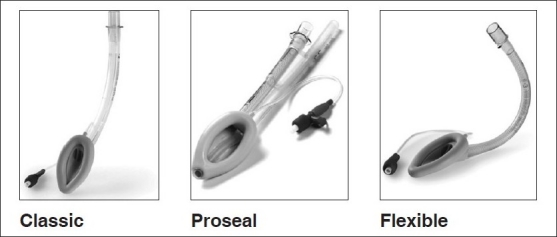
LMA family
LMA classic – available in seven sizes
LMA Proseal – seven sizes: 1, 1.5, 2, 2.5, 3, 4 and 5
LMA Unique – disposable version of classic LMA
Intubating LMA Fastrach – 3, 4 and 5
LMA Ctrach – 3, 4 and 5
Flexible LMA – minimum size is 2
The Classic and Proseal are available in sizes 1, 11/2, 2 21/2 and 3, which are suitable for children of various ages, besides the adult sizes. Fastrach and CTrach are not available in paediatric sizes, although there are reports of their use in the older child. The size of LMA to be used in a child is decided by the weight of the child, and is often written on the LMA tube close to the distal end along with the cuff volume to be used. It is as follows:
CLASSIC LARYNGEAL MASK AIRWAY
When placed properly, the cuff of the LMA sits over the laryngeal inlet, providing a seal in the pharynx that allows both spontaneous and controlled ventilation. The LMA classic allows a peak pressure of 15 cm water without a significant gas leak. The LMA classic does not protect against regurgitation. The chances of regurgitation are higher with controlled ventilation and/or if there is malpositioning of the LMA with partial ventilation of the stomach. It is preferable to use pressure control ventilation for control ventilation in children if classic LMA has to be used.[4]
PROSEAL LARYNGEAL MASK AIRWAY
The design of the Proseal LMA has two cuffs that can be inflated by a single balloon. The mask has a main cuff that seals the laryngeal opening and a pharyngeal cuff specially designed to produce a good seal so that peak pressures of up to 20 cm water can safely be used with this LMA for controlled ventilation. The Proseal LMA also has an additional drain tube situated parallel to the airway tube. When correctly positioned, the proximal end of this tube faces the upper oesophageal sphincter. A feeding tube inserted through this will directly go through the oesophagus into the stomach. So accurate is this that the ability to pass a stomach tube is one of the tests of correct positioning of the Proseal. The Proseal also has the main airway tube fully wire-reinforced, which resists kinking and ends in a 15-mm airway connector. An integral bite block has been incorporated into the airway tube to reduce the danger of airway obstruction or tube damage. The position of the drain tube inside the cuff is designed to prevent the epiglottis from occluding the airway tube. This eliminates the need for the aperture bars (as seen in the classic LMA). The accessories to the LMA proseal include a removable introducer to aid insertion without using the fingers and a dedicated deflation device to help in complete deflation before sterilization or insertion.
The double cuff arrangement allows a higher seal than the classic LMA for a given intracuff pressure. The drain tube communicates with the upper oesophageal sphincter and permits venting of the stomach and blind insertion of standard gastric tubes in any patient position without use of laryngoscopy or magills forceps. Gastric inflation causing tenting of the diaphragm is an impediment to respiration. This is an important issue of concern while using the classic LMA for prolonged periods, especially in infants, more so during controlled ventilation. This problem is solved in the Proseal that can now be safely used in children with controlled ventilation also.
The double-tube arrangement reduces the likelihood of device rotation, another important problem with the classic LMA. The revised cuff profile with the two tubes results in the device being more securely anchored in place. These features make the Proseal ideal for use in children.
FLEXIBLE LARYNGEAL MASK AIRWAY
The flexible or reinforced LMA is designed specially for use in oral and head and neck surgeries. It consists of a wire-reinforced tube connected to a standard laryngeal mask. It is available in sizes 2, 2.5, 3, 4 and 5. In each size, the cuff is the same as the classic LMA, but the tube is longer and of smaller diameter than the classic. The flexi LMA allows positioning away from the surgical field without losing the seal and is resistant to kinking. Insertion might require the introducer or a stylet.
INSERTION OF LARYNGEAL MASK AIRWAY
The standard insertion technique recommended by Brain using a fully deflated cuff has demonstrated a varying degree of successful insertion on the first attempt – 67-90% – in children. Partial inflation of the cuff has led to a higher rate of successful insertion in paediatric patients. Nonetheless, the LMA still follows a midline path, whereby it slides over the tongue, with possibility of posterior displacement of the tongue and epiglottis in the final stage. Insertion of LMA by the lateral approach as proposed by Kundra et al.,[5] with a partially deflated cuff, facilitates easier insertion with a higher success rate. A rotation of the LMA by 45° pushes the tongue to one side and the LMA slides down with a lesser degree of mouth opening. The lateral approach takes less time, and a grade 1–2 endoscopic view with the fibreoptic bronchoscope was seen in all cases. The study suggests a higher degree of injury to the uvula and posterior pharyngeal wall when LMA is inserted via a midline approach. In the reverse technique of LMA insertion, The LMA is rotated 180° with the cuff facing upward, opposite of traditional technique, and then advanced and rotated into position. Partial inflation of the mask to smooth the edges and then insertion by midline or lateral approach improved success of insertion. Jaw thrust maneuver and laryngoscope-guided placement have also been advocated to ease placement of the classic LMA.
As far as the Proseal LMA is concerned, the rotational technique was found to have no advantage over the standard technique in children.[6] The Proseal can also be inserted using the introducer tool, which is similar to the technique used for the intubating LMA. The laryngoscope-guided, gum elastic bougie-guided technique is a technique unique to the PLMA, which involves railroading the drain tube along a gum elastic bougie placed in the proximal oesophagus under direct vision. This success of insertion was higher with the bougie technique.
Although we have described various techniques, it is important to remember that the insertion of an LMA, be it classic or otherwise, is successful only if the child is adequately anaesthetized, either breathing spontaneously or paralyzed and ventilated. The most common causes of failure to effectively ventilate with an LMA are inadequate depth of anaesthesia and wrong size. Too small a size produces a large leak while too large an LMA will not go beyond the posterior pharynx.
CORRECT PLACEMENT OF LARYNGEAL MASK AIRWAY
LMA (airway tube) coming out 1 cm on inflation of cuff (classic)
Good chest rise with manual ventilation
End tidal carbon dioxide (ETCO2) showing square wave
No audible leak with peak airway pressure of 20 cm H2O. A leak below 20 cm was considered a malposition with PLMA.[7]
Gel displacement test for PLMA[8] (done by placing a blob of gel at the tip of the drain tube and noting the airway pressure at which it was ejected)
Expired tidal volume of more than 8 ml/kg
Checking with fibreoptic bronchoscope
The most commonly practiced methods are the ETCO2 and visual inspection of chest rise.
LARYNGEAL MASK AIRWAY IN ANAESTHETISING CHILDREN
The LMA has been used for a variety of surgical procedures where previously the face mask was used. It has also come to replace the endotracheal tube for short procedures. The LMA is the ideal device in situations where it is inconvenient to hold the mask, as for procedures on the face and neck. Except for Intra abdominal major surgery, where we would expect a lot of stomach contents to move up, many other procedures like limb surgeries, plastic surgery, lower abdominal procedures and urology can all be done with Proseal LMA with spontaneous or controlled ventilation. It is always ideal to plan a regional anaesthetic along with LMA insertion, especially if the child is going to be breathing spontaneously. With reports of pressure control[9] and pressure support ventilation being effectively done with the Proseal, the uses and indications are ever increasing. There are many reports coming, and we also found that the Proseal LMA can be safely used for laparoscopic procedures in children if ETCO2 and respiratory mechanics is monitored.[10]
LARYNGEAL MASK AIRWAY AND DIFFICULT AIRWAY
If a child is not breathing, what do you do before you introduce the tube? Ventilate. What do you do after you introduce the tube? Ventilate. What do you really have to do if you cannot intubate? Ventilate. That is why bag-mask ventilation is so important. But, the skill is not as easy to master as many imagine. The LMA has revolutionized difficult airway management. It can bypass obstruction at the supraglottic level and allow rescue oxygenation and ventilation, provided that mouth opening is sufficient. The LMA can be inserted completely deflated if space is limited. Head and neck vascular malformations, Pierre-Robin, Treacher-Collins, Goldenhar and mucopolysaccharidoses are examples of conditions that have been successfully managed with the LMA. This approach avoids excessive airway instrumentation, minimizes the risk of trauma and further airway obstruction by bleeding or oedema and circumvents the ‘Can’t intubate can’t ventilate’ scenario. LMA has revolutionized difficult airway management in children. It forms an important part in the care of children with congenital facial anomalies who, in the past, would have been difficult to intubate and ventilate. The LMA has been used as a tool for use both in the non-emergency (can ventilate can’t intubate) and the emergency pathway (can’t ventilate/can’t intubate) of the ASA Difficult Airway Algorithm. It can be used in an awake child after adequate local anaesthesia for the mouth and pharynx (LMA insertion in awake infant with Pierre Robin syndrome) and in the anaesthetized child with known or suspected difficult airway. It can be used as the definitive airway for a short procedure in a child with a difficult airway, in experienced hands. Once inserted, it can be used as a conduit for intubation either as a temporizing measure before a more secure surgical airway is achieved or other permanent options are pursued. Intubation through the LMA is either with a fibreoptic bronchoscope or following insertion of bougie through LMA, which is later used to guide an endotracheal (ET) tube.[11,12] Now, with the Intubating LMA, this process is even easier. The intubating LMA is a rigid, anatomically curved variant of the laryngeal mask designed to facilitate tracheal intubation. It is available in three sizes as a single use or reusable item. The paediatric version (size 3) can be used in children weighing 30–50 kg.
LARYNGEAL MASK AIRWAY IN PAEDIATRIC RESUSCITATION
There is insufficient evidence to recommend for or against the routine use of LMA during cardiac arrest. When endotracheal intubation is not possible, the LMA is an acceptable adjunct for experienced providers (class IIb), but it is associated with higher incidence of complications in young children. Although the guidelines are cautious in their recommendations for the LMA,[13] those well versed in LMA use will find it a valuable asset, especially in difficult airway situations.
LARYNGEAL MASK AIRWAY IN NEWBORN
The Neonatal Resuscitation guidelines[14] suggest that there is insufficient evidence to support the routine use of LMA as the primary airway device during neonatal resuscitation in the setting of meconium-stained amniotic fluid, when chest compressions are required, in very low birth weight (VLBW) babies or for delivery of emergency intratracheal medication. A few reports of surfactant administration in newborns via LMA[15] suggest that its applications are ever increasing. The problem with sitting and maintaining ventilation in a newborn with a classic LMA is that it can get displaced very easily and inflation of the stomach from even minimal malposition will impede respiration in the newborn. Proseal LMA can be used in newborns as it is more stable and we can vent the stomach with a stomach tube. (Proseal LMA size 1 is now available in the market in India.) LMA availability and user competence by paediatricians is, however, still low.
ADVANTAGES OF LARYNGEAL MASK AIRWAY OVER THE ENDOTRACHEAL TUBE
The ease of insertion that helps in providing a secure airway rapidly is the outstanding feature.
Laryngoscopy and muscle relaxants are not needed.
Haemodynamic and intra ocular pressure (IOP) changes are less when compared with the endotracheal tube.
Time for insertion is less.
Incidence of sore throat is less.
Is less-stimulating when compared with endotracheal tube in a reactive airway.
ADVANTAGES OVER FACEMASK
Fewer episodes of desaturation while using an LMA as compared with face mask.
Work of breathing (WOB) is less with the LMA.
It is easier to obtain an airtight seal with an LMA.
Better airway protection against regurgitation when compared with the facemask.
Children with a difficult mask fit do well with an LMA. Oropharyngeal airway obstruction is avoided.
LMA frees the anaesthetists’ hands to do other tasks.
It reduces operating room pollution as waste gases can be scavenged.
The LMA insertion technique is easy to master and can be taught to emergency personnel.
LIMITATIONS AND COMPLICATIONS OF LMA USE IN CHILDREN
Airway obstruction can occur due to malpositioning, obstruction by the epiglottis, biting on the tube, laryngospasm or kinking of the tube. Light plane of anaesthesia can also lead to laryngospasm and airway obstruction in children. Lingual oedema following extubation can cause a problem.
Aspiration of stomach contents is a potential complication, especially in cases at high risk of regurgitation as the LMA does not form an airtight seal around the larynx. Limiting the use of LMA to fasted patients and preventing gastric distention can avoid this problem. The Proseal LMA has a drain tube through which stomach contents can be vented, which addresses this problem. The younger and smaller the child, the higher the risk of complications.[16,17] Most problems came with use of the size 1 laryngeal mask. The subspecialty with the highest problem rate was ear, nose and throat surgery. There was a significant decrease in problems with increasing experience.[18]
REMOVAL OF LARYNGEAL MASK AIRWAY
Timing of removal of the LMA in children is controversial. Experts have advocated both awake and deep removal. Awake removal ensures return of protective reflexes, but with the attendant problems of airway reactivity. The LMA should not be removed in light planes as this may cause coughing and laryngospasm.[19] Removing the LMA when the child is deep avoids the problems of coughing and laryngospasm. The LMA can be removed at a plane that would allow an endotracheal tube to be removed.
COMMON MISCONCEPTIONS ABOUT LARYNGEAL MASK AIRWAY USE IN CHILDREN
LMA can easily be displaced, so unsuitable for long procedures.
Cannot use LMA for controlled ventilation.
Cannot use LMA in newborns (<5 kg).
Besides the LMA and its related devices, there are a wide variety of airway devices that are now available and can be added to the armamentarium of the paediatric anaesthesiologist.
I-GEL AIRWAY
The i-gel™ (Intersurgical, Wokingham, UK) is a single-use, supraglottic airway management device that is made from a medical grade thermoplastic elastomer [Figure 2]. i-gel has been designed to create a non-inflatable, anatomical seal of the pharyngeal, laryngeal and perilaryngeal structures while avoiding compression trauma. i-gel is currently available in seven sizes and is supplied in a colour-coded polypropylene “protective cradle”. The manufacturers claim that the cuff is “anatomically shaped” and the airway seal improves as the device warms to body temperature. The stem is elliptical in cross-section to minimize axial rotation and provide greater stability. It contains both airway and drainage tubes, and an integral bite block. The i-gel device, due to its stability, allows the child to be placed in the lateral decubitus position to perform caudal anaesthesia, without this causing a leak or the displacement of the supralaryngeal device.[20] i-gel is very easy to insert and that no learning curve is needed before a high success insertion rate is obtained and appears to be safe for paediatric management.[21] Although it has all the advantages and more stability, there very few controlled randomized studies comparing Proseal LMA in children.
Figure 2.

I Gel airway
AIR-Q INTUBATING LARYNGEAL AIRWAY
The air-Q™ Intubating Laryngeal Airway (ILA) (Cookgas LLC, Mercury Medical, Clearwater, FL, USA) is a supraglottic device [Figure 3] used for both airway maintenance during routine anaesthesia and as a conduit for tracheal intubation for patients with a difficult airway.[22,23] The air-Q ILA (Cookgas LLC, Mercury Medical, Clearwater, FL, USA) is a new SAD with similar usage indications as the LMA. Unlike the LMA, the ILA was designed primarily to allow for the passage of conventional cuffed tracheal tubes when used for blind tracheal intubation, and has the option for subsequent removal. It also shares some structural features with the Intubating LMA. In comparison with the LMA, the ILA allows for straightforward passage of a cuffed tracheal tube when used as a conduit for tracheal intubation because of the following design differences. First, the airway tube of the ILA is wider, more rigid and curved. Second, removal of the detachable 15-mm proximal connector effectually increases the internal diameter of the airway tube. Third, its shorter length allows for easier removal after successful tracheal intubation. The air-Q ILA is available in six sizes (1, 1.5, 2, 2.5, 3.5, 4.5) for single use and in four sizes (2.0, 2.5, 3.5, 4.5) for reusable use. Sizing of the paediatric air-Q ILA is similar to the LMA, in that it is weight-based: A size 1 is designed for patients <5 kg, size 1.5 for 5–10 kg, size 2 for 10–20 kg. Self-pressurized air-Q ILA_ (ILA-SP). The self pressurized air–Q ILA (ILA-SP) is a new first-generation supraglottic airway for children with a self-adjusting cuff and lack of a pilot balloon. A newer version of the ILA-SP, has recently been introduced into our practice for routine airway maintenance in children.[24] The ILA is currently the only available supraglottic device in paediatric patients designed to act as a conduit for tracheal intubation with cuffed tracheal tubes.
Figure 3.

Air Q intubating laryngeal airway
CONCLUSION
SAD have become prevalent in children because they typically are more user-friendly than a face mask and avoid many of the problems associated with endotracheal intubation. The LMA Classic and the LMA ProSeal have an established record of safety and efficacy for routine cases in paediatric patients. The LMA ProSeal may provide a better airway seal and protection against aspiration than the LMA Classic. Over the last two decades, the enormous success of the LMA has been followed by the proliferation of other SAD, each claiming advantages over devices already in use. Many new SADs, with the exception of the PLMA, appear to offer little or no benefit for the clinician or patient, over existing ones, and evidence supporting efficacy and safety is often absent or inadequate. The PLMA has yet to be outperformed by any other SAD, making it the premier SAD in children and the benchmark by which newer second-generation devices should now be compared. Recently developed non-inflatable devices, the SLIPA and the i-gel, await more clinical trials to establish their suitability in children. In the quest for an ideal SAD, the newest devices that separate the alimentary and respiratory tracts are uniquely innovative. The routine use of SAD with gastric access may be evolving to new standard of care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.White C, Cook TM, Peter A. Stoddart, A critique of elective pediatric supraglottic airway Devices. Pediatr Anesth. 2009;19(Suppl. 1):55–65. doi: 10.1111/j.1460-9592.2009.02997.x. [DOI] [PubMed] [Google Scholar]
- 2.Miller DM. A proposed classification and scoring system for supraglottic sealing airways: A brief review. Anesth Analg. 2004;99:1553–9. doi: 10.1213/01.ANE.0000134798.00069.2B. [DOI] [PubMed] [Google Scholar]
- 3.Brain AI. The laryngeal mask-a new concept in airway management. Br J Anaesth. 1983;55:801–5. doi: 10.1093/bja/55.8.801. [DOI] [PubMed] [Google Scholar]
- 4.Sinha A, Sharma B, Sood J. Pressure vs. Volume Control Ventilation: Effects on Gastric Insufflation with Size-1 LMA. Pediatr Anesth. 2010;20:1111–7. doi: 10.1111/j.1460-9592.2010.03450.x. [DOI] [PubMed] [Google Scholar]
- 5.Kundra P, Deepak R, Ravishankar M. Laryngeal Mask insertion in children: A rational approach. Paediatr Anaesth. 2003;13:685–90. doi: 10.1046/j.1460-9592.2003.01134.x. [DOI] [PubMed] [Google Scholar]
- 6.Wheeler M, Cote CJ, David I. 4th ed. Philadelphia: Saunders; 2008. Todres in Paediatric Airway, in a practice of anaesthesia for infants and children – cote, Lerman, Todres; pp. 254–7. [Google Scholar]
- 7.Bimla S, Chand S, Abhijit B, Kumra VP, Jayashree S. Proseal laryngeal mask airway - A study of 100 consecutive cases of laparoscopic surgery. Indian J Anaesth. 2003;47:467–72. [Google Scholar]
- 8.Lopez-Gill M, Brimacombe J. The ProSeal laryngeal mask airway in children. Pediatr Anaesth. 2005;15:229–34. doi: 10.1111/j.1460-9592.2005.01427.x. [DOI] [PubMed] [Google Scholar]
- 9.Goldmann K, Roettger C, Wulf H. Use of the ProSealTM laryngeal mask airway for pressure-controlled ventilation with and without positive end-expiratory pressure in paediatric patients: A randomized, controlled study. Br J Anaesth. 2005;95:831–4. doi: 10.1093/bja/aei246. [DOI] [PubMed] [Google Scholar]
- 10.Sinha A, Sharma B, Sood J. ProSeal as an alternative to endotracheal intubation in pediatric laparoscopy. Pediatr Anesth. 2007;17:327–32. doi: 10.1111/j.1460-9592.2006.02127.x. [DOI] [PubMed] [Google Scholar]
- 11.Walker RW, Allen DL, Rothera MR. A fibreoptic intubation technique for children with mucopolysaccharidoses using the laryngeal mask airway. Paediatr Anaesth. 1997;7:421–6. doi: 10.1046/j.1460-9592.1997.d01-102.x. [DOI] [PubMed] [Google Scholar]
- 12.Cardwell M, Walker RW. Management of the difficult paediatric airway. BJA CEPD Rev. 2003;3:167–70. [Google Scholar]
- 13.Pediatric Advanced Life Support. Circulation. 2005;112:IV167–87. [Google Scholar]
- 14.Neonatal Resuscitation Guidelines. Circulation. 2005;112:IV188–95. [Google Scholar]
- 15.Brimacombe J, Gandini D, Keller C. The laryngeal mask airway for administration of surfactant in two neonates with respiratory distress syndrome. Pediatr Anesth. 2004;14:188–90. doi: 10.1046/j.1460-9592.2003.01173.x. [DOI] [PubMed] [Google Scholar]
- 16.Mason DG, Bingham RM. The laryngeal mask airway in children. Anaesthesia. 1990;45:760–3. doi: 10.1111/j.1365-2044.1990.tb14449.x. [DOI] [PubMed] [Google Scholar]
- 17.Lopez-Gil M, Brimacombe J, Alvarez M. Safety and efficacy of the laryngeal mask airway: A prospective survey of 1400 children. Anaesthesia. 1996;51:969–72. doi: 10.1111/j.1365-2044.1996.tb14968.x. [DOI] [PubMed] [Google Scholar]
- 18.Sanders JC, Olumu PN, Furman JR. Detection, frequency and prediction of problems in the use of the proseal laryngeal mask airway in children. Pediatr Anesth. 2008;18:1183–9. doi: 10.1111/j.1460-9592.2008.02784.x. [DOI] [PubMed] [Google Scholar]
- 19.Laffon M, Plaud B, Dubousset AM, Ben R. Haj’hmida removal of laryngeal mask airway: Airway complications in Children anesthetized versus awake. Pediatr Anesth. 1994;4:35–7. [Google Scholar]
- 20.Bopp C, Carrenard G, Chauvin C, Schwaab C, Diemunsch P. New Orleans, USA: American Society of Anesthesiologists (ASA) Annual Meeting; 2009. Oct 17-21, The I-gel in paediatric surgery: Initial series; p. A 147. [Google Scholar]
- 21.Beylacq L, Bordes M, Semjen F, Cros AM. The i-gel, a single-use supraglottic airway device with a non-inflatable cuff and an esophageal vent: An observational study in children. Acta Anaesthesiol Scand. 2009;53:376–9. doi: 10.1111/j.1399-6576.2008.01869.x. [DOI] [PubMed] [Google Scholar]
- 22.Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air-Q intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: A case series. Pediatr Anesth. 2009;19:618–22. doi: 10.1111/j.1460-9592.2009.02990.x. [DOI] [PubMed] [Google Scholar]
- 23.Jagannathan N, Kozlowski RJ, Sohn LE, Langen KE, Roth AG, Mukherji II, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesth Analg. 2011;112:176–82. doi: 10.1213/ANE.0b013e3181fe0408. [DOI] [PubMed] [Google Scholar]
- 24.Jagannathan N, Sohn LE, Mankoo R, Langen KE, Roth AG, Hall SC. Prospective evaluation of the self-pressurized air-Q intubating laryngeal airway in children. Pediatr Anesth. 2011;21:673–80. doi: 10.1111/j.1460-9592.2011.03576.x. [DOI] [PubMed] [Google Scholar]


