Abstract
Background:
Rocuronium produces faster neuromuscular blockade compared with other neuromuscular blocking drugs. It produces comparable intubating conditions to that of succinylcholine, but does not have the short intubation time of the latter. Hence, it may not be preferable for rapid sequence intubation, but rocuronium with priming may produce comparable intubating time and conditions to that of succinylcholine. Rocuronium with priming may be an alternative to succinylcholine in rapid sequence intubation in conditions where succinylcholine is contraindicated. The present study was conducted to compare the intubating conditions and intubation time of rocuronium with and without priming.
Methods:
Sixty patients of ASA physical status I and II, aged between 18 and 60 years, of both sexes, were divided into priming and control groups of 30 each. Patients in the priming group received 0.06 mg/kg of rocuronium and those in the control group received normal saline. All patients received fentanyl 1 μg/kg, followed by thiopentone 5 mg/kg for induction. Intubating dose of rocuronium 0.54 mg/kg in the priming group and 0.6 mg/kg in the control group were administered 3 min after priming. Onset time of intubation was assessed using a Train of Four stimuli, and the intubating conditions were compared by the Cooper scoring system.
Results:
The onset time of intubation was 50.67±7.39 s in the priming group and 94.00±11.62 s in the control group, with excellent intubating conditions in both the groups and without any adverse effects.
Conclusions:
Priming with rocuronium provides excellent intubating conditions in less than 60 s with no adverse effects.
Keywords: Endotracheal intubation, intubating conditions, priming, rocuronium
INTRODUCTION
Rapid sequence induction and endotracheal intubation using succinylcholine is an established technique in patients at risk of gastric aspiration. But, succinylcholine has a number of undesirable side-effects like muscle fasciculation, myalgia, hyperkalaemia,[1] bradyarrhythmias,[2] increased intra-ocular tension, increased intracranial tension,[3] increased intragastric pressure, anaphylaxis, malignant hyperthermia and Masseter spasm. Hence, it is not suitable in situations like neuromuscular disorders, burns, acute head injury, intracranial bleed,[4] open eye injury, spinal cord injury,[5] cerebrovascular accidents and renal diseases. The above side-effects and contraindications of succinylcholine had prompted the use of non-depolarizing muscle relaxants using various techniques for rapid sequence intubation, such as (1) timing principles,[6] (2) combination of relaxant,[7] (3) high dose of non-depolarizing muscle relaxants,[8] (4) inhalational agents to augment the effect of non-depolarizing muscle relaxants,[9] (5) use of intravenous anaesthetic agents with non-depolarizing muscle relaxants to augment neuromuscular blockade[10] and (6) priming principle.
In our study, we have used the priming principle. It is a divided dose technique of neuromuscular blocking drug, capable of producing a rapid onset of neuromuscular block and suitable intubation condition. A small priming dose (10% of intubating dose) is administrated to an awake patient. This dose is large enough to cause moderate inhibition of neuromuscular transmission but small enough to cause any unpleasant side-effects. It occupies 75% of end plate receptors. After 2–4 min, the rest of the intubating dose of the drug is administered to produce neuromuscular blockade for rapid sequence intubation.
Rocuronium bromide has the fastest onset time compared with other non-deploring neuromuscular blocking drugs. We chose rocuronium bromide with an intubating dose of 0.6 mg/kg,[11] priming dose of 0.06 mg/kg[12] (10% of intubating dose) and priming interval of 3 min[13] for our study. The present study was undertaken to evaluate the efficacy of the priming principle using rocuronium bromide in reducing the onset time of intubating and also to evaluate the intubating conditions.
We hypothesized that by using the priming principle on rocuronium bromide, the onset time of the neuromuscular bromide may be hastened as that of the succinylcholine (onset time 54 s)[14] so that it can be used in rapid sequence intubation in conditions where contraindications for succinylcholine exists.
METHODS
After “Institute Ethics committee” approval and informed consent, preliminary studies were carried out in 60 patients of ASA I and II aged between 18 and 60 years, of both sexes. It is a prospective randomized double-blind placebo-controlled study conducted between February 2007 and November 2007. Patients with neuromuscular diseases, anticipated difficult intubation (obesity, thyromental distance more than 6 cm and Mallampati grade 3 and 4, pregnancy, hepatic, renal diseases, patients receiving drugs interfering with neuromuscular action and history of allergic reaction to rocuronium were excluded from the study.
The patients were randomized into two groups; namely, group “C” (control group) and group “P” (priming group) by computer-generated randomized numbers.
In the operation theatre, the intravenous cannula was secured and balanced salt solution was started. Midazolam 0.03 mg/kg was given intravenously to all patients in both groups 10 min prior to the priming dose. Blood pressure cuff was applied to the contralateral upper limb. After explaining about the nerve stimulation technique, the supramaximal stimulus was set with a peripheral nerve stimulator. Total intubating dose of rocuronium bromide 0.6 mg/kg was diluted to 5 ml. In group “C,” 2 ml of normal saline was taken in a 2 ml syringe. In group “P,” 0.5 ml of rocuronium bromide was taken from the 5 ml syringe (containing total dose) and diluted to 2 ml with normal saline, and the remaining 4.5 ml was diluted to 5 ml with normal saline. Drugs were loaded, labelled and administered by another experienced anaesthesiologist. The intubating anaesthesiologist was blinded to the study and diluting protocols.
After pre-oxygenation, the priming dose of rocuronium bromide 0.06 mg/kg (10% of intubating dose) or normal saline was given 3 min before the intubating dose as per randomization. The patients were enquired about the ptosis, double vision, difficulty in swallowing and difficulty in breathing. Fentanyl 1 μg/kg body weight was given intravenously 1 min after the priming dose. Two and half minutes after giving the priming dose, patients were induced with intravenous thiopentone sodium 5 mg/kg body weight given over 20 s. The intubating dose of rocuronium bromide was injected 3 min after the priming or normal saline injection. After giving the intubating dose of rocuronium, a supramaximally set Train of Four (TOF) stimuli was applied over the ulnar nerve at the wrist through surface electrodes and was repeated every 10 s and assessed visually for loss of adduction of thumb and disappearance of T1 of TOF stimuli. Time interval between the intubating dose and the loss of T1 of TOF stimuli was considered as “onset time of intubation.”
After loss of T1 of TOF stimuli, the trachea was intubated and intubating conditions were noted and intubation score recorded using an intubation scoring system. Intubating conditions were graded[15] as excellent when intubating scores were between 8 and 9, good with 6–7, fair with 3–5 and poor with 0–2 (Cooper et al.).
All patients were monitored with electrocardiogram, non-invasive blood pressure and oxygen saturation with pulse-oximetry. Data noted included onset time of intubation, intubating conditions at the time of intubation (using Cooper et al.'s scoring system), heart rate, mean arterial blood pressure and oxygen saturation with pulse oximetry. The above data were recorded at baseline, immediately after induction, 1 min and 5 min after endotracheal intubation.
Statistical analysis
Descriptive statistics for continuous variables such as age, weight and onset time of intubation were presented as mean and standard deviation while the inferential statistics for hypothesis testing were preformed with the Unpaired “t” test. Categorical data were compared using the Chi-square test. Graphical representation was presented by bar diagrams and statistical analysis was performed using SPSS 10.0 (SPSS Inc. Chicago, IL, USA) statistical package. Statistical significance was considered if P<0.05.
RESULTS
In the present study, 60 ASA grade I and II patients of either sex and aged between 18 and 60 years were selected and randomized into two groups, the control group (normal saline and intubating dose of rocuronium 0.6 mg/kg as intubating dose) and priming group (0.06 mg/kg of rocuronium as priming dose and 0.54 mg/kg of rocuronium as intubating dose) of 30 in each. The patients in both the groups were compared with respect to age, weight, onset time of intubation and intubation scores.
There were no significant differences; both the groups were comparable with respect to age, weight and sex [Table 1]. Age range was 18–58 years (mean age was 37.47 years) in group “C” and 20 years and 58 years (mean age was 36.40 years) in group “P.” Minimum weight was 42 kg and maximum weight was 79 kg (mean weight 57.33 kg) in group “C” and 42 kg and 78 kg (mean weight 59.00 kg), respectively, in group “P.” The Intubation score was 8–9 in both the groups, which comes under the excellent grade of Cooper's score. The intubation score was recorded in two groups after loss of T1 response of TOF. The onset time of intubation (T-i) was 50.67±7.39 s in group P compared with 94±11.626s in group C [Figure 1].
Table 1.
Demographic data and onset time of intubation (Ti)
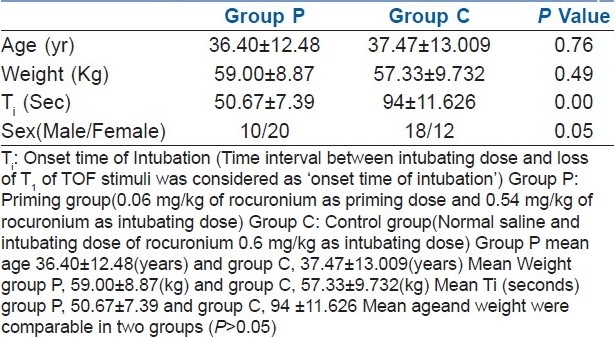
Figure 1.
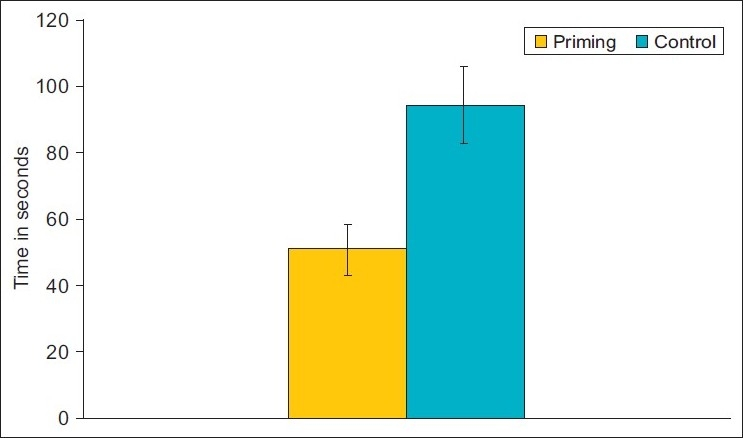
Onset time of intubation (Ti)
The heart rate and mean arterial pressure were increased at 1 min after intubation, but a statistically significant level was not attained. This heightened response could be due to stress response to endotracheal intubation [Figures 2 and 3].
Figure 2.
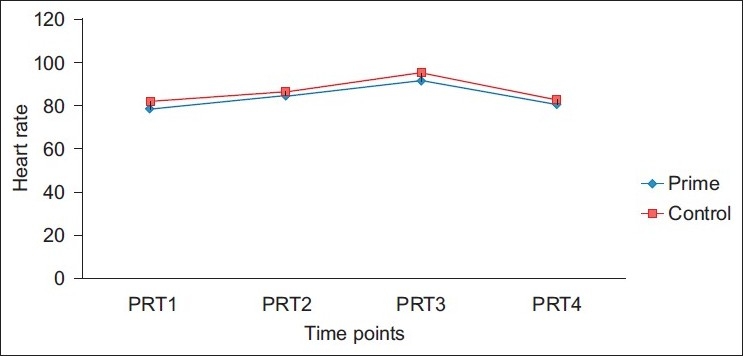
Changes in heart rate
Figure 3.
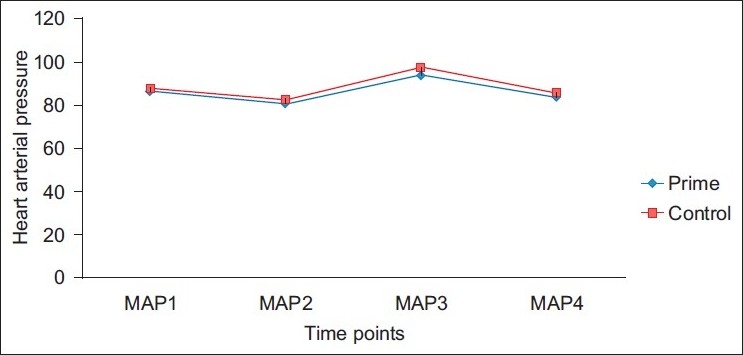
Changes in mean arterial pressure
DISCUSSION
Succinylcholine has an established role in rapid sequence intubation, but it is not without disadvantages. Rocuronium with priming could be an alternative to succinylcholine. Our study was conducted to compare the onset time of intubation and intubating conditions between rocuronium with priming and without priming. Rocuronium bromide is a steroidal non-depolarizing muscle relaxant that is useful to produce a rapid onset of action. Studies comparing rocuronium and succinylcholine in the onset time and quality of intubation have yielded varying results. McCourt et al.[16] found that rocuronium 1 mg/kg and succinylcholine 1 mg/kg have shown excellent intubating conditions at 60 s. Singh et al.[17] had shown that with 0.6 mg/kg rocuronium and 1.5 mg/kg succinylcholine, the time to achieve maximum blockade was 87.94 and 65.59 s, respectively. The intubating conditions were comparable in the two groups at 60 s. Naguib et al.[14] had given the priming dose as 0.06 mg/kg rocuronium or 0.015 mg/kg mivacurium followed by an intubating dose of 0.54 mg/kg of rocuronium. On priming with rocuronium and mivacurium, the onset times were 73 and 58 s, respectively. In the other group, 1 mg/kg succinylcholine was administered and the onset time was found to be 54 s. Intubating conditions were similar in all three groups. It was concluded that priming rocuronium with either rocuronium or mivacurium resulted in neuromuscular blockade comparable to that of succinylcholine in both the onset of action and intubating conditions. Griffith et al.[12] compared priming with non-priming by giving a priming dose of 0.06 mg/kg rocuronium followed 2 min later by 0.54 mg/kg rocuronium and another group given directly 0.6 mg/kg rocuronium. Onset times were compared, which were 34±6 s with priming and 59±14 s without priming. Jose et al.[18] found that the priming interval of 4 min allowed the fastest onset time compared with the 2- and 6-min priming intervals. Yavascaoglu et al.[13] has proved that priming with the 3-min priming interval was more effective than the 2-min priming interval when rapid tracheal intubation with rocuronium was necessary.
In our study, using the 2 × ED95 dose of rocuronium showed that with priming (priming with 10% of the intubating dose with 3-min priming interval), the onset time of intubation (onset of maximum block) was 50.67±7.39 s in the priming group and 94.00±11.62 s in the control group with comparable intubating conditions in both groups at the time of intubation, i.e. after loss of T1 of TOF.
One of the major drawbacks of priming dose is the occurrence of adverse effects such as weakness, diplopia, dysphagia, generalized discomfort and breathing difficulties. Aziz et al.[19] explained the effects of priming with vecuronium and rocuronium in younger and elderly patients. Total number of patients was 10 in each group in young and elderly in both rocuronium and vecuronium groups. In younger patients, 7 in vecuronium and 6 in rocuronium developed ptosis, 5 in vecuronium and 4 in rocuronium developed difficulty in swallowing, expiratory reserve volume reduced by 20–25%, O2 saturation was decreased but decrease was minimal in younger patients compared with the elderly. In elderly patients, 8 in vecuronium and 7 in rocuronium developed ptosis, 5 in vecuronium and 4 in rocuronium developed difficulty in swallowing, expiratory reserve volume reduced by 30–40%, O2 saturation was decreased but decrease was higher in elderly patients than in younger patients.
None of the patients in our study had evidence of such adverse effects of priming. The subtle symptoms of adverse effect of priming could not have been felt due to the administration of midazolam 10 min prior to the priming dose and fentanyl 1 min after the priming dose. The priming dose of rocuronium is advantageous in patients where succinylcholine is contraindicated for providing better quality of intubation with faster onset of action.
The autonomic safety ratio of rocuronium for vagal block is about 10-times less than that of vecuronium. No haemodynamic changes (blood pressure, heart rate) were seen in humans, and there was no increase in plasma histamine concentrations after doses of up to four-times ED95. Slight to moderate increase in heart rate may be due to either the fact that recuronium produces pain on injection or to its weak vagolytic effect. The heart rate increase may be controlled by the prior administration of fentanyl.[20]
Heier et al.[21] had given midazolam 0.01 mg/kg, alfentanil 10 μg/kg and thiopentone 4 mg/kg. It was followed by various doses of rocuronium bromide for rapid sequence induction and intubation. He mentioned the cardiovascular changes with doses of rocuronium bromide with intubating doses of 0.4, 0.8, 1.2, 1.6 and 2 mg/kg, and thereafter the changes in percentage of BP were 30, 24, 29, 22 and 17, respectively, and percentage change in heart rate were 7, 8, 7, 7 and 5, respectively.
Shorten[21] compared elderly patients given rocuronium 0.9 mg/kg with patients given vecuronium 0.12 mg/kg, and found no significant change in heart rate, arterial blood pressure or plasma epinephrine concentrations in either group.
In our study, any increase in heart rate or blood pressure after rocuronium administration was not observed, and this may be due to prior administration of fentanyl. Slight increase in heart rate and mean arterial pressure at 1 min post-intubation may be due to stress response to intubation.
Naguib et al.[15] had given priming dose as 0.06 mg/kg rocuronium or 0.015 mg/kg mivacurium followed by intubating dose of 0.54 mg/kg rocuronium. On priming with rocuronium and mivacurium, the onset times were 73 and 58 s, respectively. In another group, succinylcholine 1 mg/kg was given and the onset time was found to be 54 s. Intubating conditions were similar in all groups. It was concluded that priming a rocuronium with either rocuronium or mivacurium resulted in a neuromuscular block comparable to that of succinylcholine in both the onset of action and intubating conditions.
In our study, it was observed that onset time of intubation (using priming principle on rocuronium) was 50.67±7.39 s.
In scenarios where anticipated difficult intubation and contraindication of succinylcholine co-exist, due to its own adverse effects, rocuronium with priming principle can be safely used. Therefore, rocuronium with priming principle can be an alternative to succinylcholine for rapid sequence intubation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Birch AA, Jr, Mitchell GD, Playford GA, Lang CA. Changes in serum potassium response to succinylcholine following trauma. JAMA. 1969;210:490–3. [PubMed] [Google Scholar]
- 2.Stoelting RK, Peterson C. Heart slowing and junctional rhythms following intravenous succinycholine with and without intramuscular atropine preanaesthetic medication. Anesth Analg. 1975;54:705–9. doi: 10.1213/00000539-197511000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Minton MD, Grosslight K, Stirt JA. Increase in intracranial pressure from succinylcholine: Prevention by prior non-depolarizing blockade. Anesthesiology. 1986;65:165–9. doi: 10.1097/00000542-198608000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Stevenson PH, Birch AA. Succinylcholine induced hyperkalemia in patient with a closed head injury. Anesthesiology. 1979;51:89–90. doi: 10.1097/00000542-197907000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Savarese JJ, Caldwell JE, Lien CA, Miller RD. Pharmacology of muscle relaxants and their antagonists. In: Miller, editor. 6th ed. Vol. 1. Philadelphia: Churchill Livingstone; 2004. p. 490. [Google Scholar]
- 6.Suzuki T, Aono M, Fukano N, Kobayashi M, Saeki S, Ogawa S. Effectiveness of the timing principle with high-dose rocuronium during rapid sequence induction with lidocaine, remifentanil and propofol. J Anesth. 2010;24:177–81. doi: 10.1007/s00540-010-0880-y. [DOI] [PubMed] [Google Scholar]
- 7.Lebowitz PW, Ramsey FM, Savarese JJ, Ali HH. Potentiation of neuromascular block in man produced by combination of pancuronium and metocurine or pancuronium and d-tubocurarine. Anesth Analg. 1980;59:604. [PubMed] [Google Scholar]
- 8.Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid sequence induction of anesthesia in adult patients. Anesthesiology. 1993;79:913–8. doi: 10.1097/00000542-199311000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Savarese JJ, Caldwell JE, Lien CA, Miller RD. Pharmacology of muscle relaxants and their antagonists. In: Miller, editor. 5th ed. Vol. 1. Philadelphia: Churchill Livingstone; 2004. 424 pp. [Google Scholar]
- 10.Lowry DW, Mirakhur RK, McCarthy GJ. Neuromuscular effects of rocuronium during sevoflurane, isoflurane and intravenous anaesthesia. Anesth Analg. 1998;87:936–40. doi: 10.1097/00000539-199810000-00036. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs-Burder T, Tassonyl E. Intubating conditions and time course of rocuronium induced neuromuscular block in children. Br J Anaesth. 1996;77:335–8. doi: 10.1093/bja/77.3.335. [DOI] [PubMed] [Google Scholar]
- 12.Huizinga AC, Vandenbrom RH, Wieda JM, Hommes FD, Hennis PJ. Intubating conditions and onset of neuromuscular block of rocuronium: A comparison with suxamethonium. Acta Anesthesiol Scand. 1992;36:463–8. doi: 10.1111/j.1399-6576.1992.tb03498.x. [DOI] [PubMed] [Google Scholar]
- 13.Griffith KE, Joshi GP, Whiteman PF, Garg SA. Priming with rocuronium accelerates the onset of neuromuscular blockade. J Clin Anesth. 1997;9:204–7. doi: 10.1016/s0952-8180(97)00034-2. [DOI] [PubMed] [Google Scholar]
- 14.Yavascaoglu B, Cebelli V, Kelebek N, Uckunkaya N, Kutlay O. Comparison of different priming techniques on the onset time and intubating conditions of rocuronium. Eur J Anaesthesiol. 2002;19:517–21. doi: 10.1017/s0265021502000844. [DOI] [PubMed] [Google Scholar]
- 15.Naguib M. Different priming techniques, including mivacurium, accelerate the onset of rocuronium. Can J Anesth. 1994;41:902–7. doi: 10.1007/BF03010932. [DOI] [PubMed] [Google Scholar]
- 16.Misra MN, Agarwal M, Pandey RP, Gupta A. A comparative study of rocuronium, vecuronium and succinylcholine for rapid sequence induction of anaesthesia. Indian J Anaesth. 2005;49:469–73. [Google Scholar]
- 17.McCourt KC, Salmela L, Mirakhur RK. Comparison of rocuronium and suxamethonium for use during rapid sequence induction of anaesthesia. Anaesthesia. 1998;53:867–71. doi: 10.1046/j.1365-2044.1998.00342.x. [DOI] [PubMed] [Google Scholar]
- 18.Singh A, Bhatia PK, Tulsiani KL. Comparison of onset time, duration of action and intubating conditions achieved with suxamethonium and rocuronium. Indian J Anaesth. 2004;48:129–33. [Google Scholar]
- 19.Jose A, Rupp SM, Miller RD. Refining the priming principle for vecuronium during rapid sequence intubation of anaesthesia. Anesthesiology. 1986;64:243. doi: 10.1097/00000542-198602000-00019. [DOI] [PubMed] [Google Scholar]
- 20.White DA, Reitan JA, Kien ND, Thorup SJ. Decrease in vascular resistance in the isolated canine hindlimb after graded doses of alfentanil, fentanyl, and sufentanil. Anesth Analg. 1990;71:29–34. doi: 10.1213/00000539-199007000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Aziz L, Jahangir SM, Chandhary SN, Rahman K, Ohta Y, Hirakawa M. The effect of priming with vecuronium and rocuronium on young and elderly patients. Anesth Analg. 1997;85:663–6. doi: 10.1097/00000539-199709000-00032. [DOI] [PubMed] [Google Scholar]
- 22.Heier T, Caldwell JE. Rapid tracheal intubation with large dose rocuronium: A probability – based approach. Anesth Analg. 2000;90:175–9. doi: 10.1097/00000539-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 23.Shorten GD, Uppington J, Comunale ME. Changes in plasma catecholamine concentrations and haemodynamic effects of rocuronium and vecuronium in elderly patients. Eur J Anaesthesiol. 1998;15:335–41. doi: 10.1046/j.1365-2346.1998.00302.x. [DOI] [PubMed] [Google Scholar]


