Abstract
Objective:
To examine self-reported knowledge, attitude, and preventive practices on cancer among Saudis.
Materials and Methods:
Data was collected from Saudis aged 15 years or more, who attended one of the randomly selected 20 Primary Health Centers (PHC) or the four major private hospitals located in the Riyadh region, either as patients or their escorts. The association between the variables was evaluated by the Chi square test.
Results:
The study population consisted of 618 males and 719 females. Among the female respondents 23.1% reported that they practiced breast self-examination (BSE); 14.2 and 8.1%, respectively, had clinical breast examination (CBE) and mammography. However, 10.0 and 16.1% of the females, aged 40 years and older, reported having had mammograms and CBE, respectively. The BSE performers were more educated, knew someone with cancer, and had heard of the cancer warning signal. Both educational level and ‘heard of cancer warning signal’ were significantly related to CBE. Cancer information was received from television / radio by 65.1% and from the physician by 29.4%. Even though 69.4% believed that cancer could be detected early, a vast majority (95.8%) felt early detection of cancer was extremely desirable and 55.1% said their participation was definite in any screening program. A majority of the respondents (92.6%) insisted on the need for physician recommendation to participate and 78.1% expected that any such program should be conducted in the existing hospitals / clinics.
Conclusion:
Culturally sensitive health education messages should be tailored to fulfill the knowledge gap among all population strata. Saudis will benefit from partnerships between public health educators and media to speed up the dissemination of cancer information.
Keywords: Attitude, breast self-examination, clinical breast examination, cancer prevention, cancer knowledge, mammography
INTRODUCTION
It has been estimated that nearly 12.7 million new cases and 7.6 million deaths had occurred worldwide due to cancer in 2008.[1] In Saudi Arabia the total number of cancer cases among Saudis, in 2006, as reported by the Saudi Cancer Registry (SCR), was 8,054. For the first time, since the establishment of the SCR in 1994, cancer was more among women than men, with a female to male ratio of 1 : 0.94. The age standardized incidence rate of all cancers among Saudi women (82.8 / 100,000) was slightly lower than men (83.6 / 100,000). Cancer of breast, thyroid, colorectal, and Non-Hodgkin's lymphoma, were the most common cancers among women, while colorectal, Non-Hodgkin's lymphoma, leukemia, and liver cancers were common among men.[2]
Several studies have shown a decrease in cancer mortality through early detection and advances made in its treatment.[3–5] In Saudi Arabia, despite the unavailability of an organized national screening program there exist several programs / activities such as: The public awareness of breast cancer, through lectures, in a major hospital in Riyadh,[6] a year-round, well-designed public awareness program, and the first organized population-based screening mammography program in the Al Qassim region.[7] It was crucial that in a recent publication[8] the results of the pilot round of the Al-Qassim screening mammography program were compared with the international standards, to confirm that the program was achieving its goals. However, a high participation level of the general population was essential for the prevention programs to succeed. The key to achieving adequate compliance was informing the community about the nature and extent of the disease, as well as the preventive measures to be used, through an educational campaign.[9] Different studies conducted in the kingdom showed that the knowledge of females regarding breast cancer and its screening was low, and exhibited a wide range of prevailing preventive health practices such as breast self-examination (BSE), Clinical Breast Examination (CBE), and Mammography.[6,10–14] Some of these studies were based on selected groups, like students[11,13] and teachers.[14] Another study showed that the awareness of cervical cancer, among women in Saudi Arabia, was far behind that in the developed countries.[15] Furthermore, only few studies[12,14] assessed the attitude toward preventive practices on cancer, and those too were based on females only. This article reports findings of a study on the knowledge about and attitude toward cancer and its prevention among Saudis. The aim of this exploratory study was to examine self-reported knowledge, attitude, and preventive practices on cancer, and to provide information to educators and policy makers, which is necessary for guidance toward preventive campaigns. These findings are important for two reasons. First of all very little information exists on the perception and beliefs about cancer control in this indigenous population. Second, to improve cancer control it is important to understand what Saudis know about the disease and its early detection and treatment.
MATERIALS AND METHODS
In this survey, data was collected from Saudis aged 15 years or more, who attended one of the 20 Primary Health Centers (PHC) or the four major private hospitals located in the Riyadh region, either as patients or their escorts. More details can be found elsewhere.[16] In brief, to ensure participation of residents from each area, four PHCs from each of the East, West, North, South, and Central area was selected randomly out of the 80 PHCs scattered in the Riyadh region. The patients seen at these centers consisted of both new and follow-up patients. The individuals were identified randomly from the Reception of the Outpatient Clinics and care was taken to obtain an equal number of subjects in each gender and across all five-year age categories (15 – 19, 20 – 24, 25 – 29, and so on) from each PHC and private hospital. The minimum sample size required for the study was estimated assuming that 40% of the Riyadh population had knowledge about cancer, with a 95% confidence limit, and a precision level of ±4%. Taking into account the design effect the calculated sample size came to 1260.
In this combined community and hospital-based study, a pre-tested Arabic questionnaire was used for data collection. The questionnaire was designed based on a comprehensive review of the literature. The questionnaire was piloted mainly to assess the logistical issues such as presence of any difficulties or ambiguities, and more importantly for any culturally sensitive questions. Personal characteristics of respondents such as age, sex, marital status, educational level, and details on knowing someone with cancer, were included in the questionnaire. Knowledge on cancer diagnosis, treatment, early warning signs, common cancers in Saudi Arabia, and a question on where the respondents had obtained the information on these matters was also included. The subjects were also asked about their perception on cancer screening tests, expectations, and attitude related to prevention and early detection programs. The questionnaire had both open-ended and close-ended questions. All the interviewers in the 20 PHCs were centrally trained and the interviewers in the private hospitals were trained individually by the same trainer. This was to ensure that the survey was carried out according to the protocol and that operative procedures were identical across the centers. Data collection was carried out during the period of March 2007 to October 2008.
Eligible participants were given assurance about the confidentiality and purpose of research before getting a verbal consent to participate in the study. The study was approved by the Institutional Review Board at the King Faisal Specialist Hospital and Research Center, Riyadh. Completed questionnaires were coded and entered into a database using the SIR software (SIR Relational Database Management System 2002, SIR Pty Ltd, Australia). The quality was assured by using double data entry procedures and a system for detecting data entry errors. Frequency distributions were employed to describe the data. The association between the variables was evaluated by the Chi square test and any P value less than 0.05 was considered statistically significant. All analyses were done using the SAS Enterprise Guide 4.2 (SAS Institute Inc., Cary, NC, USA) software program.
RESULTS
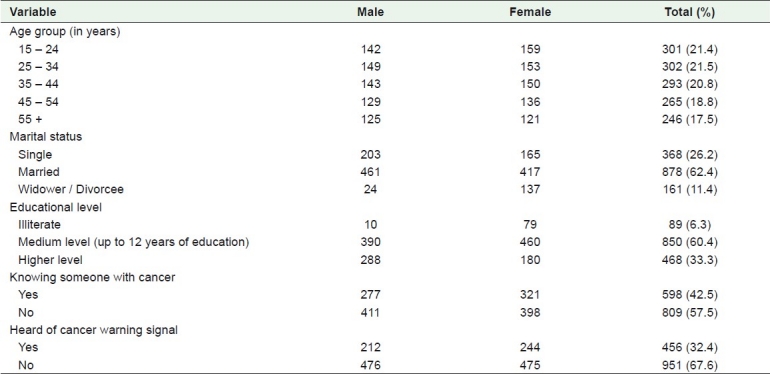
In all, the study population consisted of 618 males and 719 females. The age of the respondents ranged from 15 to 87 years, with a mean of 38.5 (S.D. 14.4) years. Out of a total of 1407 individuals, 1217 (86.5%) were interviewed from PHCs and the remaining from private hospitals. Table 1 presents the distribution of subjects by gender according to major age categories, educational level, marital status, and selected characteristics. A fair proportion (42.5%) of the respondents knew someone affected with cancer. Of those who knew someone with cancer, 16.9% reported that their first-degree relatives (parents, siblings, and offspring) had cancer, for another 23.7% it was friends or neighbors or some known persons, and the rest included aunty, uncle, cousin, and so on. Leukemia, breast, and liver cancer were the most affected malignancy among these known persons. More than two-thirds of the participants had not heard of any cancer warning signal, and when they were asked to mention the factors that caused cancer, about two-thirds (918; 65.2%) stated that it was smoking. Other factors such as, ‘unhealthy food’, ‘family history / genetics’, and ‘pollution’ were mentioned only by 268 (19.0%), 137 (9.7%), and 134 (9.5%) subjects. Another 135 (9.6%) believed the occurrence of cancer was due to fate or God's will. When the respondents were asked about the most common cancer in Saudi Arabia, close to three-fourths (1039; 73.8%) and half (673; 47.8%) of the subjects, respectively, said it was breast and uterus cancer among women, whereas only 554 (39.4%) and 410 (29.1%) subjects said it was lung cancer and leukemia among men. Although lung cancer among men was not within the top five cancers, the respondents said so, probably to exhibit their concern toward smoking.
Table 1.
Selected characteristics of the study population by gender
Nearly half of the respondents (678; 48.2%) believed that mere laboratory work was adequate to diagnose cancer [Table 2]. Out of the 79 who were categorized in to ‘other methods′, 59 mentioned methods like bone marrow, specimen, and endoscopy. More than two-thirds of the participants (983; 69.9%) did mention chemotherapy as one of the treatment modalities, when they were asked to mention the modalities of cancer treatment. Surgery and radiotherapy were also mentioned by 254 (18.1%) and 134 (9.5%) individuals as treatment modalities for cancer. However, the respondent identified various measures that were not within the conventional methods of treatment, which included reading the Quran. Only 185 (13.1%) individuals believed that reading the Quran was sufficient as a treatment for cancer [Table 2]. Another 87 (6.2%) individuals mentioned various types, such as, having herbal treatment, taking honey, drinking camel milk, having healthy foods, and hormonal treatment. However, 968 (68.8%) individuals, equivalent to those who mentioned proper modalities of cancer treatment, knew that the modality of cancer treatment depended on the type and stage of cancer. The majority of the respondents (65.1%) received cancer information from television / radio. Friends / relatives were the next common source of information (55.4%), closely followed by newspaper / magazine (52.9%). Other sources included physician (29.4%) and primary healthcare worker (7.9%) [Table 2].
Table 2.
Responses of the study population for selected variables
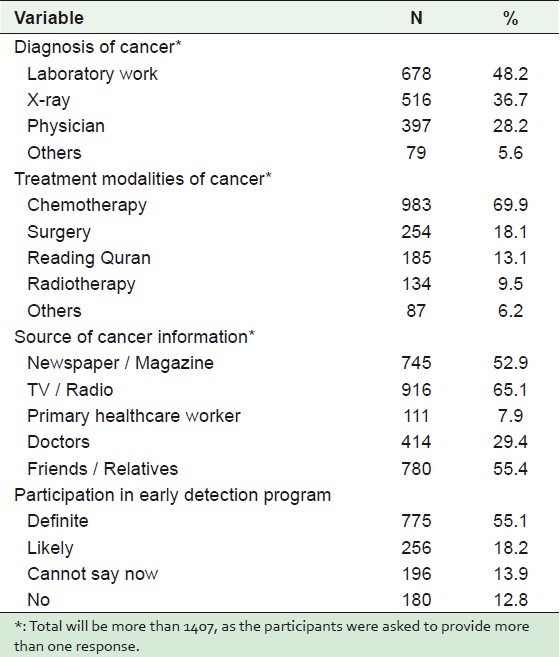
Even though 977 (69.4%) believed that cancer could be detected early, a vast majority (1348; 95.8%) felt early detection of cancer was extremely desirable. When the study population was asked about their participation in any future early detection program, more than half said it would be definite, but 32.1% were not sure about their participation, and only12.8% said they would not participate [Table 2]. In fact, for 61.3% of the male respondents the participation was definite as against 49.1% of the females. Irrespective of their status on participation, 90.9% said that they could motivate their friends to participate in the early detection program, if any. More females (95.4%) than males (89.7%) insisted on the need for a physician recommendation, to participate in any screening program. Furthermore, a majority (78.1%) expected that such programs should be conducted in the existing hospitals / clinics, while the remaining 21.9% needed some special clinic for that purpose. About 83% of the respondents felt that women would practice BSE if the PHC physician advised them to do so. More than half of our respondents (56.7%) indicated that they would like to have more information about cancer, as it would decrease the fear about cancer.
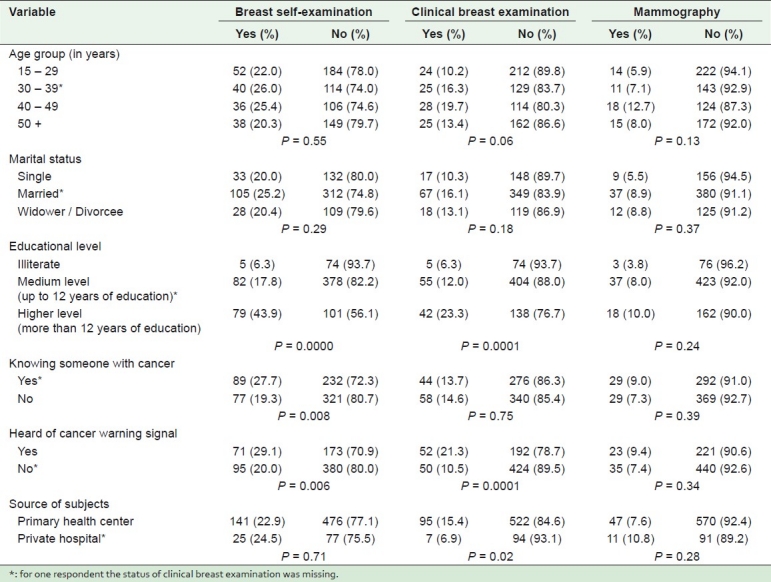
Among the female respondents 23.1% reported that they practiced BSE and only 14.2 and 8.1%, respectively, had clinical breast examination and mammography. However, 10.0% of the females aged 40 years and older reported having had a mammogram; 12.6% of females aged less than 40 years and 16.1% of those aged 40 and above reported having had a CBE. A Chi-square test was used to evaluate the relationship between BSE, CBE or mammogram practice and age, marital status, education, knowing someone with cancer, and ‘having heard of the cancer warning signal’ [Table 3]. Although having had a mammogram was not related to any of these factors, both educational level and ‘heard of cancer warning signal’ were significantly related to CBE (P = 0.0001). Knowing someone with cancer (P = 0.008), having heard of the cancer warning signal (P = 0.006), and education (P = 0.0000) were significantly related to practising BSE. Practising BSE and CBE was higher among the highly educated than among the illiterate and medium-level educated persons. Significantly (P = 0.02) more CBEs were performed among those interviewed in the PHC rather than in the private hospitals, while a non-significant (P = 0.28) higher proportion was reported to have had mammograms from private hospital interviewers. Neither the age nor the marital status was significantly related to the practices of BSE, CBE or mammography.
Table 3.
Practice of early detection methods of Saudi women according to their sociodemographic variables
DISCUSSION
If cancer patients avoid seeking care until their disease is undeniably extensive, they create a self-fulfilling prophecy by virtue of the fact that the disease is truly incurable at that point. Moreover, advanced cancer requires aggressive treatment that results in side-effects further adding to the fears and barriers that keep patients from seeking care. In the worst-case scenario, the public comes to believe that the treatment, rather than the cancer, causes death. These beliefs, which are difficult to overcome once established in the social network, can undermine, if not shut down any ministry efforts toward early detection programs.[17] Taking this into consideration, this study has focused on the basic essential knowledge that would affect screening and treatment practices as well as common local myths and misconceptions about cancer. In the absence of any organized screening program, hardly any studies have looked into the public viewpoint. We identified the following content areas in the decision-making process: Intentions / attitudes toward screening, motivating factors to undergo screening, and preferences for information. Such information will help in designing, implementing, and evaluating a health education program, to know about the risk factors and prevention / screening of cancer in Saudi Arabia.
Early breast cancer detection through mammogram, clinical breast examination, and breast self-examination is critical in reducing breast cancer-related morbidity and mortality.[18] In this study 23.1% of the female sample indicated that they were performing BSE. A previous study from Saudi Arabia found that only 18.7% of the women practiced BSE within the previous year, but a majority of women (69.7%) had never heard of BSE.[12] The practice of BSE found in our study is similar to a study done in the neighboring country, Qatar (24.9%), but much higher than in a study done in Egypt (10.4%).[19,20] The very low rate observed in the Egyptian study may be because that study was based on newly diagnosed breast cancer patients. In another three studies, 34.9% Nigerian women, 58.1% Korean American women, and 90.3% women from Sao Paulo claimed to have ever practiced BSE,[18,21,22] which clearly suggests that obvious differences and lower rates of BSE performance have been reported from developing countries.
Our results also show that women have low rates of CBE and mammography. An earlier study[10] found that clinical breast examinations were carried out by 16.1% and mammography by 14.9% Saudi women in the Al Hassa governorate, both higher than those found in the current study (14.2% had CBE, and only 8.1% had a mammogram). However, both these studies from Saudi Arabia reported a very low CBE rate compared to the US (78%) and the neighboring country Qatar (23.3%) and also a very low mammogram rate (US: 53% and Qatar: 22.5%).[18,20] Although the screening activities of the concerned countries might contribute to such variations, the role of some other underlying factors, such as cultural difference, lack of breast health awareness in women, and the like, should not be neglected. According to the guidelines of the American Cancer Society, for the early detection of breast cancer in average-risk women, annual mammography is recommended, beginning at the age of 40 years.[23] Although all medical services are free for nationals, mammography in particular, is given free or is part of the insurance coverage, alarming and serious is the practice and request for mammogram for those below 40 years of age. It was disturbing to find that 25 (6.4%) women less than 40 years of age reported to have mammography. Out of these 25, 17 were interviewed in PHCs and the rest in private hospitals. On the contrary, among those aged 40 years and above, 30 were interviewed in PHCs and three in private hospitals, and they all had a mammogram. An earlier study from Saudi Arabia assessing the doctor's perception and attitude toward breast health examination, found that breast examination was not included in the physical examination and only 11.3% had done it routinely for their patients and request for mammogram for those above 40 years of age was performed in only 34% of the cases.[24] For mammography to be useful, it must be available to the population at risk.
This study did not find any significant association between the different age groups and BSE or CBE or mammogram, which was inconsistent with the study by Dunder et al.[25] There were studies with conflicting results as well, some studies associated the practice of BSE with older age,[26] while others with younger age.[20] The practice of BSE and CBE was found more often among Saudi women with a higher level of education, which was similar to others’ observations.[20,26,27] In fact, the results suggested that women who had a higher education, knew someone with cancer, or had heard of the cancer warning signal, were more likely to perform BSE. Having known someone with cancer could have heightened one's awareness of the disease and resulted in a preventive practice.
In our study a vast majority (92.6%) thought that a physician's recommendation was necessary to comply with screening programs. Earlier studies identified that the main reason given for not attending screening services was that it was not suggested by the doctor.[9,28] On the other hand, Friedman et al.[29] had shown that physician recommendation of screening was the strongest predictor for having obtained a mammogram, CBE, monthly BSE, digital rectal examination, and fecal occult blood test. The family physician was often the first doctor that a woman consulted for general medical ailments. She built a rapport and friendship with the physician and was therefore more comfortable and more amenable to advice from him / her.[30] This put the family physician in an ideal position to inform and educate the woman with regard to health checks and screening mammograms. Although the respondents reported gaining information from a variety of sources, they demonstrated very high levels of trust in their physicians. Physicians need to make people aware of the increasing incidence of cancer during routine patient visits, and cancer prevention practices must be reinforced. With regard to 83% of the female respondents willing to undergo BSE if the PHC physician advises it, is in accordance with several studies, suggesting that the primary care physicians can significantly alter the behavior of their patients with regard to regular breast examinations.[31,32]
A majority of the respondents listing television / radio as the best source of information for cancer is in accordance with the earlier studies from Saudi Arabia,[6,12] which underscores the potential effectiveness of the television/ radio in modifying health behavior in Saudi Arabia. Although we are unaware of any published evidence, public knowledge and information on cancer prevention now seems influenced largely by television / radio rather than by information provided directly by health professionals. As the public spends considerably more time in front of the television / radio, than with their healthcare providers, media represents an important strategic tool in the dissemination of health information. Also, it is a considerable finding that health professionals are a relatively poor information source, accounting for only 37.3%. Although the main responsibilities of the primary health center in Saudi Arabia include child care, pregnancy follow-up, and reproductive health problems, they are yet to succeed in the role of providing health information on cancer to the general public.
Our findings concerning the attitude toward screening programs are encouraging. The attitudinal questions measured important concepts in cancer control, such as, beliefs about the importance of early detection and prevention of cancer and fear of the disease. The participants had a positive attitude toward cancer education, which is encouraging.
The results of this study should be interpreted in light of some potential limitations. Dearth of information, such as, whether the BSE was performed on a regular basis or not, purpose of CBE and mammogram (whether routine or diagnostic), and frequency of these procedures, resulted in providing an incomplete scenario of preventive practices among Saudis. Although this descriptive study has its own limitations, for the first time, it provided new insights into the perceptions, knowledge, beliefs, attitudes, and practices of Saudis toward cancer and its prevention practices. Our aim is not to comment on the beliefs, perception or ideas, but to highlight the presence and prevalence of these. The main reason for including both men and women in our sample selection was that attention should be paid to all in order to further increase the understanding of cancer and the performing of appropriate preventive practices. Furthermore, due to the traditional values of the society males had control over the decision on health practices. This study is unique because it has examined factors associated with the participation in screening among Saudis, which will certainly help to guide the development of focused health education and promotional programs that target this population.
CONCLUSION
Prevailing beliefs and attitudes have a great impact, at every stage of the cancer continuum, from prevention and early detection to access and response to treatment, rehabilitation, and survivorship / palliative care, and end-of-life care.[33] A high level of motivation for the women to participate in a preventive health strategy such as screening comes from the appreciation of the beneficial effects of the intervention and a preventive health-seeking behavior of the target population.[34] As screening can also lead to harm such as overtreatment, they need to understand the potential benefits of these screening programs before they can make informed decisions about participating. Ideally, physicians, health pamphlets, and other information sources should assist in clarifying the actual size of the benefits.[35] Change in perception, however, will require directed efforts in health education. On the basis of the findings of this study, it is strongly recommended that there should be a well-designed health education program to tackle the observed knowledge deficits, in order to raise awareness toward cancer, with emphasis on the role of prevention and screening. Practitioners must continue to remind and update women about breast disease, and women's cancer-screening practices. Indeed the focus of the primary healthcare providers should be to raise awareness about breast care among women and to encourage them to report any unusual changes in their breasts to their family or healthcare physicians. Our results suggest that Saudis will benefit from partnerships between public health educators and the media, to speed up the dissemination of cancer information. The participation of non-governmental and charitable organizations in creating awareness about cancer will also be helpful in solving these problems.
ACKNOWLEDGMENTS
Funding for this project was provided by a grant from the King Abdulaziz City for Science and Technology (KACST). The authors acknowledge the following for their support in data collection: Dr. Mansour Ali Al-Yousef, Director, Primary Health Care Services in Riyadh; Mr. Lafy Barak Al-Enazi, Al-Falah Hospital; Dr. Mostafa Hamdy, Al-Mubarak Hospital; Dr. Kamal S El-Rady, Al-Obeid Specialized Hospital, and Dr. Abd Al-hakim Al-Shiekh, Al-Osrah International Hospital. Special thanks and appreciation goes to Dr. Ahmad Razzaq Bafarat from the Primary Health Care Services in Riyadh for his cooperation and extra effort in collecting the data from the PHCs.
Footnotes
Source of Support: King Abdulaziz City for Science and Technology (KACST),
Conflict of Interest: Nil.
REFERENCES
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Lyon, France: International Agency for Research on Cancer; 2010. GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet] Available from: http://globocan.iarc.fr . [Google Scholar]
- 2.Saudi Cancer Registry. Cancer incidence report, Saudi Arabia – 2006. Kingdom of Saudi Arabia: Ministry of Health. 2010 [Google Scholar]
- 3.Jatoi I. The impact of advances in treatment on the efficacy of mammography screening. Prev Med. 2011;53:103–4. doi: 10.1016/j.ypmed.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 4.Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Swedish two-county trial: Impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011;260:658–63. doi: 10.1148/radiol.11110469. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Vital signs: Colorectal cancer screening, incidence, and mortality - United States, 2002--2010. MMWR Morb Mortal Wkly Rep. 2011;60:884–9. [PubMed] [Google Scholar]
- 6.Alam AA. Knowledge of breast cancer and its risk and protective factors among women in Riyadh. Ann Saudi Med. 2006;26:272–7. doi: 10.5144/0256-4947.2006.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abulkhair OA, Al Tahan FM, Young SE, Musaad SM, Jazieh AR. The first national public breast cancer screening program in Saudi Arabia. Ann Saudi Med. 2010;30:350–7. doi: 10.4103/0256-4947.67078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akhtar SS, Nadrah HM, Al-Habdan MA, El Gabbani SA, El Farouk GM, Abdelgadir MH, et al. First organized screening mammography programin Saudi Arabia: Preliminary analysis of pilot round. East Mediterr Health J. 2010;16:1025–31. [PubMed] [Google Scholar]
- 9.Sessa A, Abbate R, Di Giuseppe G, Marinelli P, Angelillo IF. Knowledge, attitudes, and preventive practices about colorectal cancer among adults in an area of Southern Italy. BMC Cancer. 2008;8:171. doi: 10.1186/1471-2407-8-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amin TT, Al Mulhim AR, Al Meqihwi A. Breast cancer knowledge, risk factors and screening among adult Saudi women in a primary health care setting. Asian Pac J Cancer Prev. 2009;10:133–8. [PubMed] [Google Scholar]
- 11.Alsaif AA. Breast self-examination among Saudi female nursing students in Saudi Arabia. Saudi Med J. 2004;25:1574–8. [PubMed] [Google Scholar]
- 12.Jahan S, Al-Saigul AM, Abdelgadir MH. Breast cancer.Knowledge, attitudes and practices of breast self examination among women in Qassim region of Saudi Arabia. Saudi Med J. 2006;27:1737–41. [PubMed] [Google Scholar]
- 13.Sait WA, Al-Amoudi SM, Tawtai DA, Abduljabbar HS. The knowledge of breast cancer among young Saudi females. Saudi Med J. 2010;31:1242–4. [PubMed] [Google Scholar]
- 14.Dandash KF, Al-Mohaimeed A. Knowledge, attitudes, and practices surrounding breast cancer and screening in female teachers of Buraidah, Saudi Arabia. Int J Health Sci (Qassim) 2007;1:61–71. [PMC free article] [PubMed] [Google Scholar]
- 15.Sait KH. Attitudes, knowledge, and practices in relation to cervical cancer and its screening among women in Saudi Arabia. Saudi Med J. 2009;30:1208–12. [PubMed] [Google Scholar]
- 16.Ravichandran K, Mohamed G, Al-Hamdan NA. Public knowledge on cancer and its determinants among Saudis in the Riyadh region of Saudi Arabia. Asian Pac J Cancer Prev. 2010;11:1175–80. [PubMed] [Google Scholar]
- 17.Boyle P, Levin B, editors. Lyon: International agency for research on cancer; 2008. World Cancer Report 2008. [Google Scholar]
- 18.Lee EE, Fogg LF, Sadler GR. Factors of breast cancer screening among Korean immigrants in the United States. J Immigr Minor Health. 2006;8:223–33. doi: 10.1007/s10903-006-9326-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdel-Fattah M, Zaki A, Bassili A, el-Shazly M, Tognoni G. Breast self-examination practice and its impact on breast cancer diagnosis in Alexandria, Egypt. East Mediterr Health J. 2000;6:34–40. [PubMed] [Google Scholar]
- 20.Bener A, El Ayoubi HR, Moore MA, Basha B, Joseph S, Chouchane L. Do we need to maximise the breast cancer screening awareness.Experience with an endogamous society with high fertility? Asian Pac J Cancer Prev. 2009;10:599–604. [PubMed] [Google Scholar]
- 21.Okobia MN, Bunker CH, Okonofua FE, Osime U. Knowledge, attitude and practice of Nigerian women toward breast cancer: A cross-sectional study. World J Surg Oncol. 2006;4:11. doi: 10.1186/1477-7819-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carelli I, Pompei LM, Mattos CS, Ferreira HG, Pescuma R, Fernandes CE, et al. Knowledge, attitude and practice of breast self-examination in a female population of metropolitan São Paulo. Breast. 2008;17:270–4. doi: 10.1016/j.breast.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 23.Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011: A review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2011;61:8–30. doi: 10.3322/caac.20096. [DOI] [PubMed] [Google Scholar]
- 24.Al-Amoudi SM, Sait WA, Abduljabbar HS. Health care provider's role in facing the future burden of breast cancer in Saudi. Saudi Med J. 2010;31:1359–62. [PubMed] [Google Scholar]
- 25.Dündar PE, Ozmen D, Oztürk B, Haspolat G, Akyildiz F, Coban S, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Med J. 2009;50:132–8. [PubMed] [Google Scholar]
- 28.Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med Princ Pract. 2009;18:35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- 29.Friedman LC, Puryear LJ, Moore A, Green CE. Breast and colorectal cancer screening among low-income women with psychiatric disorders. Psychooncology. 2005;14:786–91. doi: 10.1002/pon.906. [DOI] [PubMed] [Google Scholar]
- 30.Tan SM, Evans AJ, Lam TP, Cheung KL. How relevant is breast cancer screening in the Asia / Pacific region.? Breast. 2007;16:113–9. doi: 10.1016/j.breast.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 31.Giveon S, Kahan E. Patient adherence to family practitioners’ recommendations for breast cancer screening: A historical cohort study. Fam Pract. 2000;17:42–5. doi: 10.1093/fampra/17.1.42. [DOI] [PubMed] [Google Scholar]
- 32.Gorin SS, Ashford AR, Lantigua R, Hossain A, Desai M, Troxel A, et al. Effectiveness of academic detailing on breast cancer screening among primary care physicians in an underserved community. J Am Board Fam Med. 2006;19:110–21. doi: 10.3122/jabfm.19.2.110. [DOI] [PubMed] [Google Scholar]
- 33.Kagawa-Singer M. A Socio-cultural Perspective on Cancer Control Issues for Asian Americans. Asian Am Pac Isl J Health. 2000;8:12–7. [PMC free article] [PubMed] [Google Scholar]
- 34.Basu P, Sarkar S, Mukherjee S, Ghoshal M, Mittal S, Biswas S, et al. Women's perceptions and social barriers determine compliance to cervical screening: Results from a population based study in India. Cancer Detect Prev. 2006;30:369–74. doi: 10.1016/j.cdp.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Gigerenzer G, Mata J, Frank R. Public knowledge of benefits of breast and prostate cancer screening in Europe. J Natl Cancer Inst. 2009;101:1216–20. doi: 10.1093/jnci/djp237. [DOI] [PMC free article] [PubMed] [Google Scholar]


