Abstract
Genetic counselling in tribals unlike general population residing in cities and near villages is a difficult task due of their lower literacy and poor socio-economic status. However, sustained effort is essential with a close interaction in the local language, certain misbeliefs need to be removed gradually taking into account their socio-cultural background. The present communication deals with our experience in counselling for haemoglobinopathies during Neonatal Screening Programme undertaken for sickle cell disease in Kalahandi district of Orissa and Community Screening Programmes in primitive tribes of India in four States viz. Orissa, Gujarat, Tamil Nadu and Maharashtra. Counselling during neonatal screening programme was very well accepted demonstrating the benefit to the small babies as regards the morbidity. Premarital marriage counselling was also accepted by them. The success rate as followed up for 5 years is almost 50 per cent, the limitation being long follow up. Genetic counselling in these areas has to be continuous to achieve success and therefore the need for setting up of permanent centres in the tribal areas in India.
Keywords: Genetic counselling, haemoglobinopathies, neonatal screening programme, sickle cell disease, tribals
Introduction
Genetic counselling is the process by which patients or relatives, at risk of an inherited disorder, are advised of the consequences and nature of the disorder, the probability of developing or transmitting it, and the options open to them in management and family planning in order to prevent, avoid or ameliorate it and is branched into diagnostic (the actual estimation of risk) and supportive aspects. This process involves appropriately trained persons to help the individual or family to (i) comprehend the medical facts, including the diagnosis, probable course of the disorder, and the available management; (ii) appreciate the way heredity contributes to the disorder, and the risk of recurrence in specified relatives; (iii) understand the alternatives for dealing with the risk of occurrence; (iv) choose the course of action which seems to them appropriate in view of their risk, their family goals, and their ethical and religious standards, to act in accordance with that decision; and (v) to make the best possible adjustment to the disorder in an affected family member and/or the risk of recurrence of that disorder1.
Though the counsellor discusses the risk factors associated with the ongoing conception in presence of both at-risk spouses, the decision regarding the available options depends solely on the attitude and acceptance of the individuals counselled. No simple correlation has been found between the change in technology to the changes in values and beliefs towards opinion or decision2. The formulation of an informed, internally evaluated cognitive decision suggests strategies for evaluating the competence of any decision after genetic counselling. The value of a cognitive decision against a normative decision rests more on the determination of the quality of counselee-decision and the components tending to improve the process. A cognitive decision is a function of attitude (A) modified by others’ feeling and sensitivity towards the ‘taken decision’ (E) and the value adjudged to ‘others’ feeling and opinion’ shared by the counselee (V0); and is expressed as A+E(V0). Enhancing the sensitivity of counselling by approaching to gear up the educational activity related to the counselee's emotional state or by multiple visit, audio-visual aids, communicating the summary for the educational sessions by close interaction3,4 has earlier been advocated in Europe and found to be successful in a better implementation of genetic counselling. However, in our country these approaches are yet to be considered during the process of genetic counselling in spite of the fact that we have a greater risk for haemoglobinopathies and associated mortality.
During the last 30 years, the field of genetic counselling has expanded rapidly. Genetic counsellors practice in a variety of settings, including hospitals, private offices, laboratories, federal and State government offices, universities, and research units. Patients seeking genetic counselling can be younger, elderly, male or female, pregnant or newly married, affected with a disease or at risk for a disease. While on one hand, the counselling provides adequate supportive and essential aid in decision making for a particular situation that may arise due to the risk of carrying a genetic disorder in an individual; it may raise complex ethical questions on the other hand, which often do not have clear and simple answers.
A recent challenge for genetic counsellors has been the development of predictive testing for disorders. With modern genetic technology, DNA testing can indicate the relative probability that some individuals will develop a genetic disease but fails to predict the actual outcome. Thus an individual with a 75 per cent chance of developing a particular genetic disease may remain healthy throughout his or her life, while an individual with only 25 per cent probability of disease development may succumb to the disease. In addition, for some diseases (e.g. Alzheimer disease) there are no cures or treatments available regardless of predictability. In situations such as these, the benefit of predictive testing remains open to debate. In absence of such techniques for prenatal confirmation, the prediction of a foetus of its risk and fatality that may become apparent especially in at-risk couples, depends solely on the guess and chance as assumed from laboratory findings and calculation of inherited risk by the genetic counsellor. Many places of India still are away from the main stream research and diagnostic confirmation facilities. In this communication we describe our experience of genetic counselling in tribal population of Maharastra, Tamil Nadu and with special reference to Orissa. The map (Fig. 1) points the name and locations of the tribes considered for the screening of haemoglobinopathies and genetic counselling.
Fig. 1.
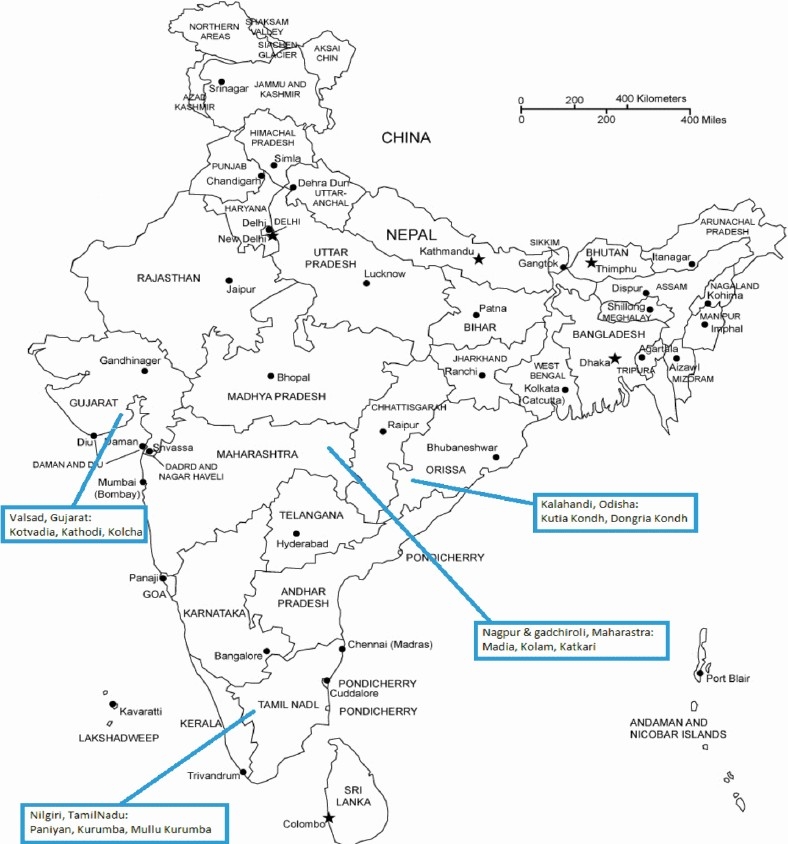
Map of India showing the locations of the tribal populations screened. Source: http://www.freeusandworldmaps.com/html/Countries/Asia%20Countries/IndiaPrint.html.
Indian tribes
India is a vast, ethnically diverse country and the people inhabiting it are as diverse as the land itself. The large Indian population is multi-ethnic and divided into subgroups. As many as over 4635 different ethnic groups form the panoramic cultural mosaic of the country5,6. A majority of populations are from the Indo-Aryan stock (72%) followed by Dravidian (25%) and Mongoloid and other 3 per cent7. People living in specific geographical isolation with distinct language, territorial distribution and cultural practices may be termed ‘indigenous’. The other term used to identify them is ‘tribal’ or ‘adivasi’. As per the Census of India, 20018, there are about 635 biological isolates (tribes and sub-tribes) that constituted 8.08 per cent (about 84.3 million) of the total population of India who are considered the original inhabitants of this ancient country. They fall under the category of Scheduled Tribes and constitute the largest tribal populace in the world. About half of the world's autochthonous people, comprising 635 tribal communities including 75 primitive tribal communities live in India. They are found in all s0 tates except Punjab, Haryana and Jammu & Kashmir9. The primitive tribal communities have been identified by the Government of India in 15 States/Union Territories on the basis of (i) pre-agricultural level of technology (ii) extremely low level of literacy; and (iii) small, stagnant or diminishing population10.
There are many tribal groups identified for their specific biological constitution, anthropogenetic characterization, distinct cultural and linguistic pattern and confined geographical localization. In many tribal groups distinct Negroid feature of appearance is seen (e.g. Jarawas, Onges of Andamans, Iruals, Paniyans of southern India) whereas in many, Mongoliod origin is traced (Khasi, Garos of north east India). In rest of the country, majority of tribals are either proto-australoids or astro-asiatic in nature.
Besides having prominent cultural and behavioural uniqueness, the tribals of India also have their characteristic individuality with respect to genetic make-up. Studies done on blood groups and immunity related genes have shown that tribals of India have sets of alleles which are exclusive to certain geography and ethnic groups11,12. Also the hypothesis that they differ distinctly in the pattern of distribution and frequency of specific sets of alleles from the non-tribal Indian populations has been empirically proved by designed population based studies on haemoglobinopathies13–16.
Haemoglobinopathies
Among all the abnormal haemoglobinopathies hitherto reported in Indian populations, HbS, the mutant gene causing the most fatal red cell haemoglobin genetic abnormality (sickle cell disorder) affecting the shape of the RBCs (changed due to a genetic lesion in the beta globin specific DNA sequence in chromosome 11) is commonly found. HbS causes maximum morbidity and mortality to many Indian communities.
After the first description of HbS in southern India in early 195217 and then in Eastern India18, extensive studies have been done on HbS gene and its fatality and impact on human survival. Clinical presentation, variability and treatment management have been given attention to in late eighties19–23. The mapping on the pattern of its distribution has been studied to a great extent. However, there has been a definite lack of population based studies. A few studies done on some of the Indian population groups postulate that the clinical presentation of the gene is comparatively benign among Indian tribes. There have been reports that the fatality related to acute chest syndrome, Vaso Occlusive Crisis (VOC) and leg ulcers are less observed in tribal sickle cell disease patients as compared to that non-tribal patients. These observations are often overshadowed with the possibility of associated alpha-thalassaemia among the tribes24,25. Besides HbS, other abnormal haemoglobin disorders found among Indian tribes and other ethnic groups in India are HbE, HbDPunjab etc26–28.
Sickle cell haemoglobin abnormality has been predominantly seen in the Gond group of tribes in central and east central part of India and Dravidian tribes from southern India, whereas another severe variant, the HbE is found in higher frequencies among northeast Indian tribes like the Toto, Khasi, etc. Besides, beta-thalassaemia gene has also been reported in higher frequencies in many of these tribes except tribes from western India and southern India29. Based on these findings, a belt for HbS, HbE and beta-thalassaemia has been mapped for Indian tribes which stretches from Gujarat in west through Madhya Pradesh and Orissa in central east up to Assam, Meghalaya and Manipur in northeast and Karnataka and Kerala in south.
Orissa tribes & haemoglobinopathies
Orissa (now known as Odisha), placed at one corner of this virtual haemoglobinopathies belt has the largest number of tribal communities residing in mostly rural and hilly parts. Of the reported 62 tribal communities from Orissa, 13 are most primitive and are distinct in their identity and appearance30. Extensive studies done on Orissa tribes reveal that most of the tribes have specific lifestyle, practice and language or dialect. Inhabiting mostly the inaccessible parts of the State, these tribes have been self sustaining on their own by their exclusive dependency on natural resources and reclusive living pattern and self defined economic and political systems.
Each tribal group separates itself from others by virtue of specific identity based on a clan-like division exclusive to their own. Within themselves also, these identities are considered as exogamous unit thus discouraging inbreeding and close relative marriages. Mostly, the tribal groups are agriculture based and have taken local agriculture as primary occupation though food gathering and occasional hunting are still practiced. There have been documented distinctions in practice of specific rituals related to new birth or death or beginning of agricultural season. The health care practices are very specific in these tribes. Traditional medicine men (ojha) are believed to practice a few ethno-medicine procedures mostly based on Ayurveda which are relied upon during any health related problems. Most of the Orissa tribes reside in places with noted endemicity of falciparum malaria.
Earlier postulations and description of HbS gene being only limited to tribal and lower caste population have been changed as this gene has been found in almost all the communities in India with preponderance among the Indian tribes. In Orissa, the sickle cell gene is highly prevalent among the general castes (0.3-20.7%), scheduled castes (0-8.9%) and scheduled tribes (0-5.5%)25,27.
The tribes share a very innate social structure with a strong interpersonal relation between and among the members of the society. A village/settlement is like a compact and extended family with a close and transparent exchange of social responsibility. Close relative marriage is generally discouraged. They, on the other hand are also strict in practice of endogamy.
Experience from Orissa
Neonatal screening: Although it is now well established that Orissa is at higher risk for sickle cell and thalassaemia haemoglobinopathies, there is a lack of appropriate approach to initiate a large scale population based study with a dedicated genetic counselling aim. We explored Kalahandi, a tribal dominated western Orissa district under a project on newborn screening. The main primitive tribal group in Kalahandi is the Kondh, although other tribes like Savaras, Lanjia, etc. are also found in lesser number. The distribution of the Kondhs; a proto-australoid tribe in Kalahandi is definitely patchy but is found in clusters of a few villages (gudaa) on the hilltops. The exact population of the Kutia Kondh are not available but the number of Dongria Kondhs as estimated in 2001 census is about 8000 individuals31,32. They practice polygyny and have gotra like divisions which are exclusively exogamous. The literacy rate in the tribal (mostly Dongria Kondhs and Kutia Kondhs) was found to be negligible. Only a few children born after 1997 are attending primary schools and educational platform provided by the Sarvasikshya Aviyan, a drive to facilitate education for all. The exposure to outer main stream and other domains among these tribes is quite limited. The visitors are either from the government people or a few dedicated non government organizations (NGO) personnel working in the vicinity. Recently after the auxillary nursing midwife (ANW) and accredited social health workers (ASHA) networks became implemented, a few Integrated Child Development Services (ICDS) health workers and primary school teachers are also being recognized and accepted. We initially took help from these already recognized persons to enter and to get introduced.
The programme had three main parts; (i) Initial workout on regular visit and community interactive sittings, (ii) meeting the parents of detected babies with genetic disorder, and (iii) follow up and family screening. The initial interactions were made as friendly as possible so as to develop a positive gesture regarding our presence. Unlike the close-to-city tribal villages, these settled tribal pockets are far off from the minimum facility centres, and are quite sensitive to external interactions and generally avoid accepting newer provisions including optimum health care services. This is more acute especially in tribals with a primitive way of life, or those who still are mostly dependent on forest based economy and livelihood. Tribes from Andhra Pradesh and Kerala are worst sufferers from many disorders33–36 including sickle cell haemoglobinopathies. But as shown by a recent study37 majority of these scattered tribal pockets are deprived of the minimum health care facilities even though their villages are located within a close proximity to the block level health centres. Most implementations are not well accepted by the tribals due to unknown or undisclosed causes which might be due to a lack of proper exchange of facts and truths regarding the facilities from the provider side.
Keeping this in mind the initial village meets were organized with the help of local bodies and these were aimed mainly at building up awareness related to sickle cell disease and the importance of infant screening through close interaction.
Selection of villages & samples: The programme was parted into two divisions, one of which was training in social work, field work paradigms and strategy makings and the second one was collection of blood samples and analysis of genotypes in newborns. The interactions were targeted to villagers with different status and social hierarchy to increase impact. Grandparents were involved in different stages of village and family meets. The impact was assessed qualitatively by attendance of villagers, attendance of both parents, frequency of interaction from their side, recollection capability of earlier discussions and open ended suggestion with reference to sickle cell disease prevention. About one third of mothers (with one or two children) expressed their interest to get at least one of their babies tested. While testing newly born babies was initially not a common agreement, after elaborated in detail about the benefits and appropriateness of newborn screening during the consecutive sittings, majority of parents accepted. With increasing consent to screen newborn babies, the task to attend every village where a birth was recorded, also increased.
With a disfavoured education and minimum amenities, the primitive tribes of Kalahandi are in a definite need of awareness related to health care and child health practices. Improvised ICDS services and encouraging growth in Anganwadi workers (AWW) network though are promising to provide better supportive mother-child health (MCH) and reproductive & child health (RCH) initiatives, but looking at a comparatively closed social structure of these people, a painstaking one-to-one system of approach may be a good replacement to the existing protocol for village based implementation of health services.
The information of births was collected from the Block hospitals, PHCs and AWW centres using pre-tested schedules. Non-institutional deliveries were noted as reported by ASHA or AWWs of concerned panchayats. Only those villages were included in this study where either the number of households was more than 50 or number of newborn was more than 3 or number of surviving HbSS children exceeds three. A preliminary interview based survey was made before organizing the meet by the social workers to understand the general understanding about the disease and number of cases suffering from the disease in each village.
A blood collection camp was scheduled only when the decision of the camp was unanimously taken up in the village meeting. The villages were categorized on the basis of number of village meets organized in each village against the proportion of babies screened in that village.
Selection of families was done simply by randomly choosing at least five households and all the family members of these families were called to attend the village meet. All the families with HbSS children (if any in the village) were also intimated to attend the meet.
Observations
Response: In all the 49 villages in the study area at Lanjigarh block, Kalahandi, the frequency of HbS in newborns was found equally high. The average number of children surviving with HbSS disease (does not include the newborns detected as HbSS in our study) was found to be 2.18 (Table). A total of 255 families from 49 different tribal villages from two blocks of Kalahandi were contacted and 547 individuals were interviewed on some basic facts about sickle cell disease and its consequences. It was seen that villages with lesser number of HbSS children interestingly were more focused in screening programme than the villages with higher number of diseased babies. In contrast, villages with more number of surviving HbSS babies attended in higher number during the meets and blood collection camps were organized easily in those villages. This observation may be attributed to the fact that the parents of the HbSS children in these villages were already exposed to the problems of the disease and their main intention in attending the meetings was mainly to get some information or some possible aid regarding the health of their children. In 24 villages the situation was interesting, where in spite of a huge number of individuals and families were interacted with regards to the disease, and where the number of HbSS children were also high, comparatively less number of couples did attend our meetings (Table).
Table.
Details of village meetings and response to interaction in the study area at Lanjigarh block, Kalahandi
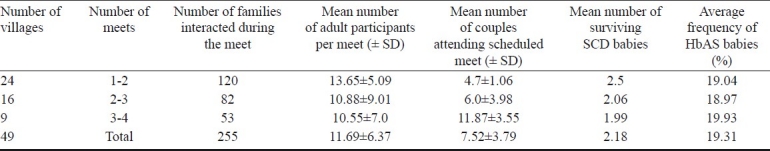
There were some villages where more number of meetings were required to sensitize people. These villages were having lesser number of incidences of HbSS children, whereas other villages where HbSS babies (indicated by symptoms) were more, required lesser number of sensitizing meets and also lesser effort to convince the couples for blood collection of their newborn babies. After initial effort to sensitize people, the number of participant couples increased.
Level of awareness: In spite of difficulties in gathering information from the tribal families regarding personal opinion, the level of awareness and perception regarding benefits of genetic testing were found out (about NBS only) using simple interactive questions to selected individuals.
The individuals were chosen randomly from each village who had not attended our meets and who were over 18 yr of age from both genders. Females were less interested to interact (158 of 547; 28.9%). Only 46 per cent of respondents never heard of the disease before and of the remaining 54 per cent respondents who had heard the name of the disease, about three fifth (61.9%) of respondents were really interested to know more about the disease. They also informed that they know the pain and problems with this disease, as been visible and known in the children with HbSS in their villages. The most interesting finding was that about 36 per cent of mothers (between 25 to 39 yr age) expressed their interest to get their babies tested for sickle cell disease after interaction. All these 57 mothers, who did not attend village meets were not aware of the facts and details on sickle cell disease prior to this interview. The only knowledge about the ailment and sufferings they heard about sickle cell was from the parents of the HbSS babies in their villages. This indicates that there has been a definite lack of sharing information regarding diseases and their detection facilities in rural Orissa. Given a situation enabling in-depth and informative interaction, the awareness level is expected to enhance. Also this will allow genetic counselling to be accepted by the tribal individuals and societies returning the benefit of such effort and programmes.
Rejection: In our study, about one eighth of villages rejected our meet after the first sitting. The only cause of it which could be made out was that the village head and other elder persons did not want to get influenced by explanations and elaborations about something they did not recognize as a part of their society and health.
Blood collection and laboratory analysis: After the initial phase of interaction and finalization of camp place and date, heel prick blood was collected using sterile lancets (BD, NJ, USA) on dried blood spot in S & S 903 filter paper (Whatman Inc, Part of GE healthcare, USA). The cards were customized for recording relevant data regarding mother's health, demographic details and baby's birth and health information. After careful blotting of spots and drying the cards were sealed appropriately as per the manufacturer's instruction and transported back to the laboratory within 24 h. HPLC was done from the 3mm punch from each sample by Variant II (Bio-Rad Inc. Hercules, USA) using beta- thalassaemia short programme reorder pack within 72 h. The reports generated were interpreted on the basis of the haemoglobin windows and retention time38. In cases of suspicion, parents’ whole blood was availed after at least two interactive sessions with the family and was analysed for complete blood count and haemoglobin pattern. DNA analyses were performed by ARMS-PCR for β thalassaemia and HbS wherever required. Genetic cards carrying the report in local language were given to parents of all babies enrolled in our programme.
The reports were given in bilingual language, one being the Oriya. The reports carried information about the status of the baby with respect to sickle cell disorder, the names of parents, address and a few lines about the disease. The card also carried the contact details of our scientific personnel, in case of communication for the doctors who would be treating the baby. All the data records of HPLC and other details including genealogical details (wherever collected) were archived and kept for future reference.
As it becomes irrational to provide card with written results to a primitive Kondh tribe who most likely may never read and understand the result, we shaded the cards with colours to recognize the message and the possible risk for sickle cell disorder associated in the individual without reading the results and findings. The pink colour card were given for normal individuals with the results written on the back side, whereas the sickle cell disease (SCDs) cards were full yellow in colour. The HbAS or heterozygotes were half pink and half yellow (Fig. 2). This colour-coding interpretation was highly accepted by the people of the study area and was easily remembered.
Fig. 2.
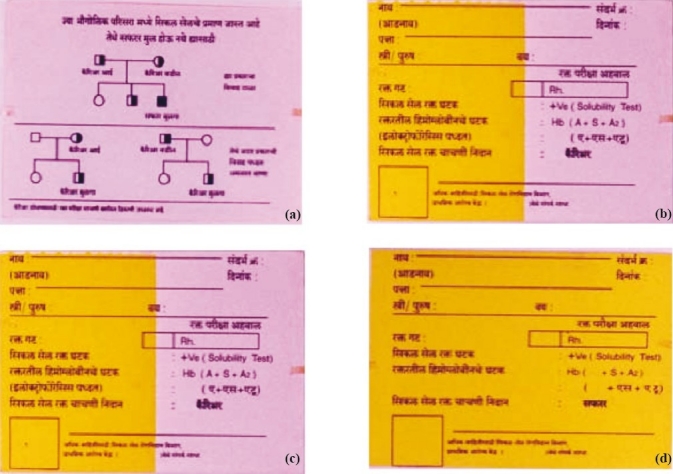
Colour coded genetic cards showing different shades for different genotypes identified at individual level. (a): Full pink report card for HbAA (Normal) with sketch representation of pattern of inheritance of HbS gene on the back side. (b) & (c): Half-pink-half-yellow report cards for HbAS (heterozygote). (d): Full yellow report card for HbSS (SCD) patient.
While elaborating the results to the parents of the baby tested, simple words were used to convey the ‘risk/no-risk’ associated with the card type. It was explained that the full yellow cards, which symbolizes HbSS (sickle cell anaemia) carry risks and encumbrance needing careful medical intervention to manage a near healthy life, whereas the other two types i.e. the half-yellow and half-pink and also the full pink cards symbolizes individuals without any serious disease. Moreover, during interaction the possible risk of a marriage between two carriers (carrying half yellow-half pink cards) was also explained to them using stepwise easy paradigms. This became a common and accepted approach of understanding the inheritance of HbS among Kondh tribes.
The babies detected to be SCD were indexed and located in the village map and the locations, names and references were noted by the social workers for follow up which had three components. The health care workers and doctors of the area were also informed. (i) Initial visit by social worker and sense the status of the family members and negotiating for a meeting (with or without village head) followed consecutively by at least three sittings with the parents of the baby. (ii) Medication and advices recommended after a thorough medical checkup by physician. (iii) Initiation and compliance to penicillin therapy, periodical clinical and haematological testing of the baby up to one year, followed by pneumococcal vaccination.
After confirmation of the status of the disease in a child, the family was visited at least twice a month to interact and sensitize parents regarding sickle cell disease, its consequence and motivate them to avail the medical facility in time.
The success of the programme was an outcome of initial elaborated interaction programme and village level meetings organized prior to blood collection camps and intervention. The only difficulty we faced was the inaccessibility to many tribal dominated villages in Kalahandi. This resulted in coverage of only 27 per cent of non-institutional deliveries. However, 68 per cent of all institutional deliveries were screened for sickle cell disease and 32 per cent were missed due to diverse causes (data not presented). The commitment for continued treatment-management for babies detected with SCD was maintained cautiously and prophylaxis penicillin (Penicillin V 125 mg BD/baby) along with folic acid supplement was provided. A total of 30 cases of sickle cell disease (HbSS) and four cases of HbS-beta thalassaemia babies have been detected and enrolled. The parents of these sickle cell disease babies are counselled.
Experience from Maharashtra, Tamil Nadu and Gujarat Community Screening Programme
In a tribal society the different socio-cultural activities revolve around gods and spirits. They have specific gods for their health and diseases, for calamities, for good harvest, cattle, etc. Therefore, the possibilities of introducing the concept of god during genetic counselling was explored. Those who were detected to have sickle cell gene, were asked to tattoo their hands in the form of god and they were told that they should not get married to another individual with similar god. This worked out very well amongst the young tribal adolescents of the Satpura hills among whom the selection of partners is still done by the young girls and boys themselves and not by their parents (the practice is known as Ghotul).
The reporting of status in colour coded cards was initially adopted in Nagpur, Maharashtra, Nilgiri hills, Tamil Nadu and Valsad district of Gujarat during screening and counselling for genetic blood disorders. The colour coded report cards were distributed to all the individuals whose blood was tested. Counselling through printed materials and interaction through communication in person were done in local language and tribal dialect in practice. The message pertaining to avoidance of marriages between two carriers for haemoglobinopathies particularly the thalassaemia and sickle cell disorders was described during long sessions of interactions. The usefulness of testing before marriage was also explained with the help of patterns of inheritance charts wherever possible, especially in the Kondhs of Odisha. The risk at individual youth level was also discussed in presence of other family members. All the carrier youths in Gadchiroli and Chandrapur district areas of Maharashtra were periodically followed up for a period of five years after initial counselling. During this period, 12 marriages took place. Of these, in seven marriages the spouses had their sickle cell disease status known prior to marriage negotiation. Interestingly, six HbAS individuals had chosen to marry to normal individuals after checking their status by observing full pink cards. Only in one case the HbAS individual had chosen to marry with an unscreened spouse. The remaining five marriages were among unscreened person. The scenario is more or less similar in more advanced tribes in Kotagiri (Nilgiri hills).
During counselling in both the situations, in the adult tribals of Maharastra, Gujarat and Tamil Nadu as well as in the parents of babies with the disorders in Orissa, we tried to communicate and wanted the people to understand and accept was that (i) SCD is a hereditary disorder and can only become fatal in children when both the parents carry the genes; (ii) The disease severity may also vary; (iii) Diet patterns are neither the cause of the disease nor are restricted in the diseased individuals; (iv) Weakness and poor health in individuals with SCD may be caused by associated iron deficiency anaemia which can very well be corrected by appropriate medical treatment; (v) In case of newborns detected with SCD, the disease may express its severity after only a particular age and a timely early course of medication (e.g., penicillin prophylaxis, folic acid prophylaxis) and vaccines (e.g., pneumococcal vaccine, meningococcal vaccines, Haemophilus influenzae vaccine along with the immunization chart listed vaccines) may save the child from severe consequences and even death; and (vi) Simple daily practices of drinking enough water with little salt and sugar, lesser exposure to extremes of temperatures and avoiding exertion may become very much helpful in minimizing the disease course in patients with SCD. Also it was noticed in Orissa that the uptake of the facts becomes better in situations where the tribals were involved to participate and share in interaction programme. A close follow up is essential for achieving the desired results in counselling. The holistic approach towards awareness, counselling has been depicted in Fig. 3.
Fig. 3.
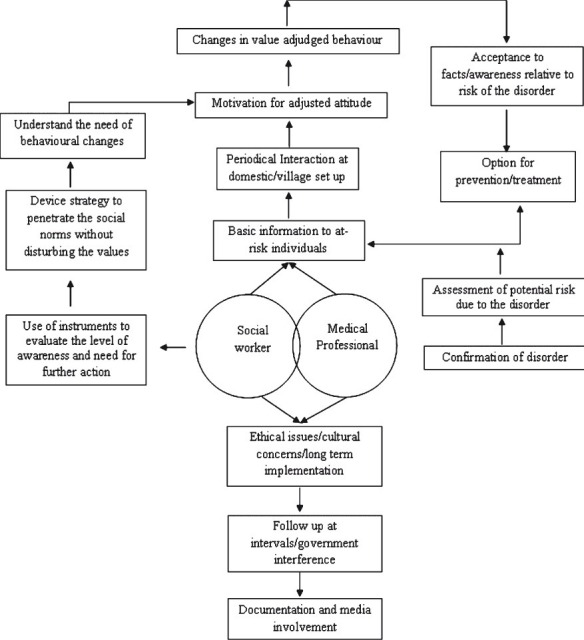
Diagrammatic representation of the possible effect of village based awareness programmes for haemoglobinopathies.
Our experience at the National Institute of Immunohaematology (NIIH), Mumbai, in adult screening and counselling in States of Maharashtra, Gujarat and Nilgiri hills, Tamil Nadu, revealed that there has been increasing demand for prenatal diagnosis of SCDs in last four to five years although these facilities are available at NIIH, Mumbai, since last two decades. Following counselling and exchange of information and attempt to improve the cognitive decision making behaviour regarding prenatal diagnosis in young couples with assessed risk of SCD foetus, between 2000 to 2010 we could provide prenatal diagnosis in 238 pregnancies at risk, of which 193 were for sickle cell homozygotes, 44 for sickle cell β-thalassaemia disease and one for sickle cell HbD disease (unpublished observation). Though the majority of the couples were from different parts of Maharastra and neighbouring States and were non tribals, but interestingly a significant number of couples (about 20%) who gave consent for prenatal diagnosis were from tribal groups inhabiting in rural districts of Maharastra. Majority of them after detection of the risk associated with the foetus opted for termination and prevent the birth of sickle cell anaemia babies (unpublished data). This is a reflection of intense counselling and prolonged interaction with people from all around Maharashtra and other s0 tates and mass antenatal screening programmes undertaken by NIIH, Mumbai39.
Conclusion
The moral risks associated at individual as well as family and society level have always been in question leading to improper consequences and often refutation. The answers to the queries of the people are generally avoided deliberately and the issues arising thereby are kept unattended. Persistent misconceptions and illegitimate guidance have misled the understanding and insinuation regarding haemoglobinopathies by imposing certain wrong social values evasion and unhealthy interaction at individual level.
Often, it is observed that the introduction of newer facts about the risk associated with one's haemoglobinopathies status at individual level is progressively affected and shaped by a multitude of negative influence and rejection from the family, society and cultural spheres. In context of the achievement of education and exposure to developing world, the Indian tribes are far from using the ‘freedom in choice’ which basically relies on the dissemination of accuracy in information and sharing that at social and familial level. Delicate and proper understanding of the very sensitive psycho-social determinants and aspiration of the tribal societies need to be considered before implementing any counselling effort pertaining to haemoglobinopathies in India.
References
- 1.Epstein Charles J, Childs B, Clarke FF, McKusick VA, Miller JR, Motulsky AG, et al. Genetic Counseling. Am J Hum Genet. 1975;27:240–2. [PMC free article] [PubMed] [Google Scholar]
- 2.Singer Eleanor, Couper Mick P, Van Hoewyk Trivellore Raghunathan J, Antonucci Toni. Trends in US attitudes toward genetic testing, 1990-2004. Public Opin Q. 2008;72:446–58. doi: 10.1093/poq/nfn033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsia YE. Genetic responsibility. In: Lipkin M, Rowley PT, editors. Genetic responsibility. New York: Plenum Press; 1974. pp. 43–59. [Google Scholar]
- 4.Antley RM. Genetic Counseling: problems of socio-psychological research in evaluating the quality of decision making. Am J Med Genet. 1979;4:1–4. doi: 10.1002/ajmg.1320040102. [DOI] [PubMed] [Google Scholar]
- 5.Singh K.S, editor. Scheduled Tribes. Vol. 3. New Delhi: Anthropological Survey of India; 1994. People of India, National Series. [Google Scholar]
- 6.Singh K.S, editor. The biological variation in indian population. Vol. 10. New Delhi: Anthropological Survey of India; 1994. People of India, National Series. [Google Scholar]
- 7.Report of Central Intelligence Agency (CIA), Field Listing: Ethnic groups, CIA world facebook. 2009. Mar 12, [accessed on June 17, 2011]. Available from: https://www.cia.gov .
- 8.New Delhi, India: Govt of India, Ministry of Home Affairs, Office of the Register General and Census Commissioner; 2001. Census of India 2001: Table A10 - State Primary Census Abstract for Individual Scheduled Caste and State Primary Census Abstract for Individual Scheduled Tribe. [Google Scholar]
- 9.Report of the Steering committee on Empowering the scheduled tribes for The tenth five year plan (2002-2007). TFYP steering committee sl. no. 5/2001. Planning commission. Govt of India. 1. [accessed on July 17, 2011]. p. 120. (URL: http://planningcommission.nic.in/aboutus/committee/strgrp /stgp_woman.pdf. )
- 10.Basu SK. Health problems and health care of the tribal population of India. In: Mahanty N, editor. Tribal economy, health and wasteland development. New Delhi: Inter-India Publications; 1994. p. 137. [Google Scholar]
- 11.Bhatia HM, Rao VR. Genetic atlas of Indian tribes. Mumbai: Institute of Immunohaematology, Indian Council of Medical Research; 1986. [Google Scholar]
- 12.Das MK, Singh SS, Adak T, Vasantha K, Mohanty D. The Duffy blood groups of Jarawas - the primitive and vanishing tribe of Andaman and Nicobar Islands of India. Transfus Med. 2005;15:237–40. doi: 10.1111/j.1365-3148.2005.00583.x. [DOI] [PubMed] [Google Scholar]
- 13.Murhekar KM, Murhekar MV. Absence of Haemoglobinopathies and G6PD deficiency among the Jarawas, a primitive Negretoid tribes of Andaman and Nicobar Islands. Indian J Hum Genet. 2004;10:29–30. [Google Scholar]
- 14.Reddy PH, Petrou M, Reddy PA, Tiwary RS, Modell B. Hereditary anaemias and iron deficiency in a tribal population (the Baiga) of central India. Eur J Haematol. 1995;55:103–9. doi: 10.1111/j.1600-0609.1995.tb01818.x. [DOI] [PubMed] [Google Scholar]
- 15.Pande PL, Singh MPSS, Tiwary RS. Prevalence of haemoglobinopathies among the Pando and Kodku tribes of Sarguja district, Madhya Pradesh. J Hum Ecol. 1999;10:443–4. [Google Scholar]
- 16.Pande PL, Singh MPSS, Tiwary RS. Distribution of ABO and Rh blood groups among the Kodku tribe of Sarguja district, Madhya Pradesh. J Hum Ecol. 1999;10:445–6. [Google Scholar]
- 17.Lehmann H, Catbush M. Sickle Cell Trait in Southern India. Br Med J. 1952;1:289–90. doi: 10.1136/bmj.1.4755.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunlop KJ, Mazumder UK. The occurrence of sickle cell anemia among group of tea garden labourers of Upper Assam. Indian Med Gaz. 1952;87:387–91. [PMC free article] [PubMed] [Google Scholar]
- 19.Sarma PS, Viswanathan KA, Mukherjee MM. Death patterns in sickle cell disease from a steel city. J Assoc Physicians India. 1986;34:192–4. [PubMed] [Google Scholar]
- 20.Kar BC, Kulozik AE, Sirr S, Satapathy RK, Kulozik M, Serjeant BE, et al. Sickle cell disease in Orissa state, India. Lancet. 1986;328:1198–201. doi: 10.1016/s0140-6736(86)92205-1. [DOI] [PubMed] [Google Scholar]
- 21.Kulozik AE, Kar BC, Satpathy BE, Serjeant GR, Weatherall DJ. Fetal haemoglobin level and BS globin haplotypes in Indian population with sickle cell disease. Blood. 1987;69:1742–6. [PubMed] [Google Scholar]
- 22.Mukherjee MB, Surve RR, Ghosh K, Colah RB, Mohanty D. Clinical diversity of sickle cell disease in Western India: Influence of genetic factors. Acta Haematol. 2000;103:122–3. doi: 10.1159/000041032. [DOI] [PubMed] [Google Scholar]
- 23.Mohanty D, Mukherjee MB. Sickle cell disease in India. Curr Opin Hematol. 2002;9:117. doi: 10.1097/00062752-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Mukherjee MB, Chang YL, Rolande D, Gangakhedkar RR, Colah RB, Kadam MD, et al. Effect of α-thalassemia on sickle-cell anemia linked to the Arab-Indian haplotype in India. Am J Haematol. 1997;55:104–9. doi: 10.1002/(sici)1096-8652(199706)55:2<104::aid-ajh9>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 25.Patel DK, Patel M, Mason RS, Patel S, Dash Preetinanda M, Das BS. Clinical and molecular characterization of βS and GγAγδβ Thalassaemia in eastern India. Haemoglobin. 2010;34:604–9. doi: 10.3109/03630269.2010.526890. [DOI] [PubMed] [Google Scholar]
- 26.Saha N, Banerjee B. Incidence of abnormal hemoglobins in different ethnic groups of India. Hum Genetik. 1971;11:300–3. doi: 10.1007/BF00278657. [DOI] [PubMed] [Google Scholar]
- 27.Saha N, Banerjee B. Haemoglobinopathies in the Indian subcontinent. Acta Genet Med Gemellol. 1973;22:117–38. doi: 10.1017/s1120962300017650. [DOI] [PubMed] [Google Scholar]
- 28.Sukumaran PK, Master HR. The distribution of abnormal haemoglobin in the Indian population. Proceedings of First Conference of Indian Society of Human Genetic, Bombay. 1974;1:91–111. [Google Scholar]
- 29.Sengupta M. Thalassemia among the tribal communities of India. Int J Biol Anthropol. 2008;1:2. [Google Scholar]
- 30.Chhotray GP. Health status of primitive tribes of Orissa. ICMR Bull. 2003;33:99–104. [Google Scholar]
- 31.Dongria Kondh population. Available from http://assets.survivalinternational.org/ documents/386/DK_numbers.pdf .
- 32.Saxena NC, Parasuraman S, Kant Promode, Baviskar A. Report of the four member committee for investigation into the proposal submitted by the Orissa mining company for bauxite mining in Niyamgiri. New Delhi: Ministry of Environment & Forest, Govt. of India; 2010. p. 5. [Google Scholar]
- 33.Babu BV, Leela BL, Kusuma YS. Sickle cell disease among tribes of Andhra Pradesh and Orissa, India. Anthropol Anz. 2002;60:169–74. [PubMed] [Google Scholar]
- 34.Ramana GV, Chandak GR, Singh L. Sickle cell gene haplotypes in Relli and Thurpu Kapu populations of Andhra Pradesh. Hum Biol. 2000;72:535–40. [PubMed] [Google Scholar]
- 35.Feroze M, Aravindan KP. Sickle cell disease in Wayanad, Kerala: gene frequencies and disease characteristics. Natl Med J India. 2001;14:267–70. [PubMed] [Google Scholar]
- 36.The Hindu, Focus on sickle cell anaemia among tribals. 2007. Jan 31, [accessed on June 10, 2011]. Available from: http://www.thehindu.com/2007/01/31/stories/2007013105730300.htm .
- 37.Brindha B, Vidyalaksmi R, Menon M, Raj Kumar S, Prashanti Devi M. Assessment of the health inequities in Sickle cell anemia surveys: A GIS based approach to map tribal patients in Nilgiris. In: 4th Internatioanl congress on sickle cell disease at Raipur, India. 2010 Nov 22-27; Oragnised by the Department of Biochemistry, Pt. J.L. Nehru Medical College, Raipur and Govt of Chhattisgarh. Poster No 74, Abstract book: 153. [Google Scholar]
- 38.Riou J, Godart C, Hurtrel D, Mathis M, Bimet C, Bardakdjian-Michau J, et al. Cation-exchange HPLC evaluated for presumptive identification of hemoglobin variants. Clin Chem. 1997;43:34–9. [PubMed] [Google Scholar]
- 39.Colah R. Prenatal diagnosis of sickle cell disorders in India. In: 4th Internatioanl congress on sickle cell disease at Raipur, India. 2010 Nov 22-27; Oragnised by the Department of Biochemistry, Pt. J.L. Nehru Medical College, Raipur and Government of Chhattisgarh. Abstract book: 59. [Google Scholar]


