Abstract
Objectives:
Total white blood cells (WBCs) decrease slightly in the elderly. In response to an acute infection, the number of WBCs increases and in sepsis, the increase is very dramatic. There are some reports about the effects of increased number of WBCs as a predisposing factor of bacteremia. An association between neutrophilia and eucopenia and increased mortality rate in the elderly has also been observed. We compared peripheral WBC counts in young and elderly patients with sepsis.
Methods:
A case-control study was carried out on 130 admitted patients who were divided into two groups based on age, ≥ 65 years (case group) and < 65 years (control group). All patients were hospitalized with the diagnosis of sepsis in two teaching hospitals in Tehran, Iran, 2001-2006.
Results:
Mean WBC counts at admission time were 17061.5 ± 14240.2 /μl in the case group and 13567.7 ± 9888.0 /ml in the control group. There were statistically significant associations between age and history of infection and history of hospitalization during the last month in the case group and also between age and source of infection (P < 0.05).
Conclusions:
The history of infection and the history of hospitalization during the last month with sepsis are important risk factors in elders.
Keywords: Sepsis, Leukocytosis, Elderly
INTRODUCTION
In both hospital and community, bacteremia is more common in the elderly period.1 The presence of co-morbid conditions is clearly a determinant of mortality associated with bacteremic illnesses.2 Compared to younger infected patients, elderly patients with bacteremia had fewer signs or symptoms and were without fever.3,4
White blood cells or leukocytes produce, transport, and distribute antibodies as a part of the immune system response. Normal values of white blood cells are 4500-10,000 in adults. In the elderly, total WBC will decrease slightly.5 In response to acute infection, trauma or inflammation, the number of WBCs increases and in some diseases, such as sepsis, the increase in WBC is so dramatic that resembles leukemia (leukemoid reaction).5
There are some reports about eucopenia, lymphopenia, increase of WBC band forms, and neutrophilia in the elderly patients.4,6,7 The site of acquisition of infection, source of blood stream infection, sex, neutrophilia, and older age are factors associated with increased mortality rate.2,8
Increased survival was observed in patients treated with appropriate antimicrobial agents regardless of age, source of infection, or bloodstream isolates.2 Chronic renal failure, urinary tract infection, severe sepsis, leukocytosis, eosinopenia and thrombocytopenia were identified as risk factors of bacteremia.9
There are some reports about the effects of increased number of WBCs as a predisposing factor of bacteremia, and also common changes of WBC during sepsis,5,10 association of neutrophilia and increased mortality rate in the elderly,10 the relationship of eucopenia and bacteremia in the elderly,4,8 and altered classic presentation in older age.4 In order to examine these issues in the elderly, we compared peripheral WBC counts in young and elderly patients with sepsis.
METHODS
A case-control study was designed to include 130 patients admitted to Loghman-e-Hakim Hospital and Boo Ali Hospital during 2001-2006 in Tehran, Iran. The patients were divided into two groups: the case group consisted of 65 patients over 65 years of age with the diagnosis of sepsis based on the definition of sepsis,10 and the control group included 65 patients less than 65 years of age diagnosed with sepsis.
Patients with HIV, immunosuppression therapy and malignant diseases were excluded and others compatible with the above definition were enrolled in this study.
Evaluation of symptoms, signs and laboratory data was performed at the time of admission before starting the antibiotics. Sampling was done based on sequential method on the available cases. Statistical analysis was performed using SPSS12(SPSS Inc, Chicago, IL) by t-test and chi-square test. P < 0.05 was considered significant.
RESULTS
One hundred and thirty patients were divided based on age to ≥ 65 years (case group) and < 65 years (control group). The case group included 32 (49%) women and 33 (51%) men with the mean age of 79.43 ± 7.46 years. The control group included 24 (37%) women and 41 (63%) men with the mean age of 42.5 ± 14.8 years.
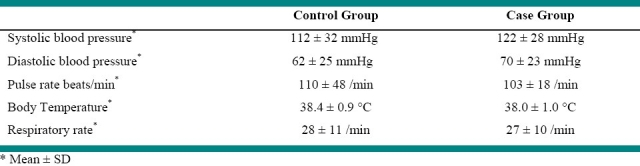
Table 1 and 2 show medical history and vital signs at the time of admission in patients of both groups. A systolic blood pressure ≤ 90 mmHg was perceived in 15.5% of the case group and 26% of the control group. A diastolic blood pressure ≤ 60 mmHg was found in 34% of the case group and 46% of the control group; also a body temperature ≥ 38°C was observed in 60% of the case group and 63% of the control group. A body temperature < 37.2°C was seen in 15 elderly patients.
Table 1.
Distribution of septic patients based on history of underlying diseases, Tehran, Iran, 2001-2006.
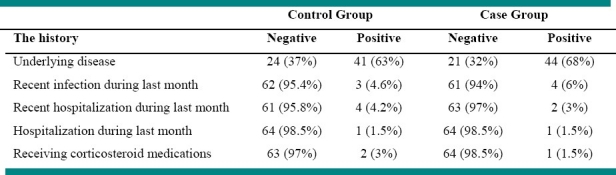
Table 2.
Distribution of septic patients based on vital signs, Tehran, Iran, 2001-2006.
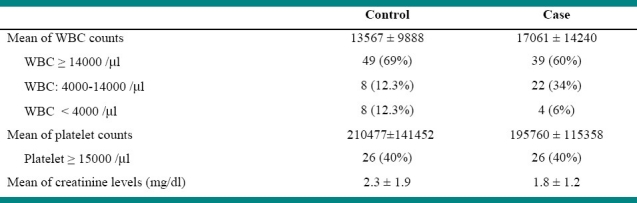
A serum creatinine > 1.2 mg/dl was present in 60% of the case group and 45.5% of the control group. Table 3 shows white blood cells, platelets and serum creatinine in the two groups.
Table 3.
Distribution of septic patients based on white blood cells, platelets and creatinine levels, Tehran, Iran, 2001-2006.
The source of infection was unknown in 19 patients (29%) of the case group and 25 patients (38.5%) of the control group. Distribution of patients according to the source of infection is illustrated in Figure 1.
Figure 1.
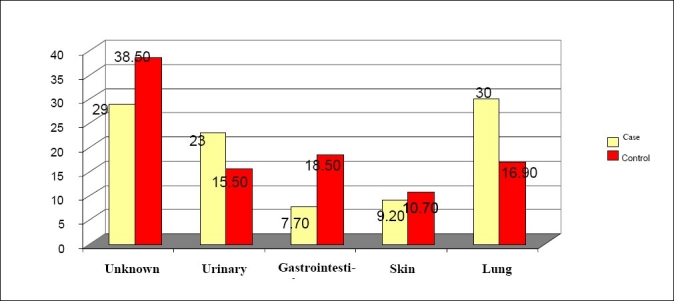
Distribution of septic patients based on the source of infection
There were significant correlations between age and the history of recent infection during the last month (P < 0.05), age and the history of hospitalization during the last month (P < 0.05) in the case group. Moreover, this finding was more frequent in patients aged 85-95 years. There were insignificant correlations between age and the history of recent infection during the last month in the case group and age and the history of hospitalization during the last month in the control group.
There was a significant correlation between the source of infection and WBC counts in the case group (P < 0.05), i.e. WBC count ≥ 14,000 was more common in urinary tract, gastrointestinal and skin infections. This correlation was not found in the control group. Unlike the case group, there was a significant correlation between WBC count and age in the control group (P < 0.05), i.e. WBC ≥ 12,000 was more common in patients aged 45-64 years, and WBC < 4000 was more frequent in young patients aged less than 30 years.
Death was observed in 33 patients of the case group (51%) and in 33 patients of the control group (51%). There was no significant association between WBC count and death or death and probable source of infection in any group.
There was no significant difference between the two groups in the mean of WBC counts based on independent sample t-test analysis.
No significant difference was detected between the mean platelet counts, mean systolic blood pressure, mean diastolic blood pressure, mean respiratory rate and mean serum creatinine levels between the two groups.
There was a significant difference between the mean pulse rate and also mean body temperature between the two groups based on independent t-test analysis (P < 0.05), i.e. pulse rate and body temperature were higher in the control group.
DISCUSSION
A previous study showed the change of normal body temperature with age, that is, elderly people have lower normal body temperatures compared with young people.11 In addition, some elderly patients with bacteremia were found afebrile.3 In the present study, body temperature ≥ 38°C was more common in the control group compared with the case group (63% vs. 60%, respectively) and body temperature < 37.2°C was found in 23% of the elderly patients. There was not any significant difference between the two groups in this regard.
In this study, the most common sources of infection in the elderly patients were lung (31%) and urinary tract (23%), while in the control group the most common probable sources of infection were gastrointestinal tract (18.5%), and lung (17%). In Ismail et al. research, lung, and urinary tract were the most common sources of infection in the elderly patients. No significant correlation was found between death and source of infection in any group. Ismail et al. noticed higher mortality rate in patients with lung infection. They also observed good prognosis in those with urinary tract infection.8 This difference could be due to nosocomial infection in 33% of the patients. However, Tal et al. detected a high mortality rate in patients with urinary tract infection.12 The difference between the two studies could be due to the different method used by the latter. Chassange et al. perceived more clinical evidence of infection in the elderly patients with bacteremia than in those without bacteremia.4 We found clinical evidence of infection in 71% of the elderly patients versus 61.5% of the control group, which shows the severity of disease in elderly patients. In the present research, WBC count ≤14000 /ml was seen in 60% of the case group and 68% of the control group. Additionally, a WBC count < 4000 /ml was found in 6% of the case group and 12.3% of the control group. There was not any significant difference between the mean WBC counts of the two groups.
Although a high rate of mortality was observed in both groups of this study, there was not any significant correlation between WBC count and death in the two groups. Ismail et al. showed a poorer outcome in leukopenic patients.8 Our findings indicate a significant correlation between the source of infection and WBC counts in the case group (P < 0.05), i.e. WBC count ≥ 14000 /ml was more common in urinary tract, gastrointestinal and skin infections. There was no such correlation in the control group. Also, thrombocytopenia ≥ 150000 was seen in 40% of the elderly patients, but no significant correlation existed between platelet counts and death.
Raz identified leukocytosis and thrombocytopenia as risk factors of bacteremia and questioned the usefulness of performing blood cultures in elderly patients with sepsis.9 The present research found a significant correlation between age and the history of recent infection in the last month in the case group. This is in agreement with McBean and Meyers that demonstrated bacteremia to be more common in aged people both in hospital and community.1,2
Our findings showed a systolic blood pressure ≤ 90 mmHg in 15.5% of the case group and 26% of the control group. There was not any significant difference in mean systolic blood pressure between the two groups. No significant correlation between systolic hypotension and mortality was discovered in the two groups. Ismail et al. indicated a poor clinical outcome in hypotensive elderly patients with bacteremia.8
CONCLUSION
Elderly patients with sepsis can be afebrile. They may also have lower pulse rates compared to young septic patients. It is important to ask the history of recent infection and the history of hospitalization during the last month in evaluation of elderly patients with sepsis. In the presence of leukocytosis more than 14000 more attention should be paid to urinary, gastrointestinal, and skin infections in elderly patients with sepsis.
Footnotes
Conflict of interest statement: All authors declare that they have no conflict of interest.
Source of funding: None.
REFERENCES
- 1.McBean M, Rajamani S. Increasing rates of hospitalization due to septicemia in the US elderly population, 1986-1997. J Infect Dis. 2001;183(4):596–603. doi: 10.1086/318526. [DOI] [PubMed] [Google Scholar]
- 2.Meyers BR, Sherman E, Mendelson MH, et al. Bloodstream infections in the elderly. Am J Med. 1989;86(4):379–84. doi: 10.1016/0002-9343(89)90333-1. [DOI] [PubMed] [Google Scholar]
- 3.Gleckman R, Hibert D. Afebrile bacteremia.A phenomenon in geriatric patients. JAMA. 1982;248(12):1478–81. doi: 10.1001/jama.248.12.1478. [DOI] [PubMed] [Google Scholar]
- 4.Chassagne P, Perol MB, Doucet J, et al. Is presentation of bacteremia in the elderly the same as in younger patients? Am J Med. 1996;100(1):65–70. doi: 10.1016/s0002-9343(96)90013-3. [DOI] [PubMed] [Google Scholar]
- 5.White blood cell count and differential. Available from: URL: http://www.answers.com/topic/whiteblood-cell-count-and-differential .
- 6.Fontanarosa PB, Kaeberlein FJ, Gerson LW, Thomson RB. Difficulty in predicting bacteremia in elderly emergency patients. Ann Emerg Med. 1992;21(7):842–8. doi: 10.1016/s0196-0644(05)81032-7. [DOI] [PubMed] [Google Scholar]
- 7.Pfitzenmeyer P, Decrey H, Auckenthaler R, Michel JP. Predicting bacteremia in older patients. J Am Geriatr Soc. 1995;43(3):230–5. doi: 10.1111/j.1532-5415.1995.tb07327.x. [DOI] [PubMed] [Google Scholar]
- 8.Ismail NH, Lieu PK, Lien CT, Ling ML. Bacteremia in the elderly. Ann Acad Med Singapore. 1997;26(5):593–8. [PubMed] [Google Scholar]
- 9.Raz R, Ben Israel Y, Gronich D, Granot E, Colodner R, Visotzky I. Usefulness of blood cultures in the management of febrile patients in long-term care facilities. Eur J Clin Microbiol Infect Dis. 2005;24(11):745–8. doi: 10.1007/s10096-005-0046-2. [DOI] [PubMed] [Google Scholar]
- 10.Munford RS. Sepsis, Severe Sepsis, and Septic Shock. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. Philadelphia: Churchill Livingstone; 2005. pp. 906–10. [Google Scholar]
- 11.Tehran, Iran: Iranian Proceedings of the 9th Congress on Infectious Disease and Tropical Medicine; 2001. Relationship of Age with normal temperature in healthy people; pp. 14–6. [Google Scholar]
- 12.Tal S, Guller V, Levi S, et al. Profile and prognosis of febrile elderly patients with bacteremic urinary tract infection. J Infect. 2005;50(4):296–305. doi: 10.1016/j.jinf.2004.04.004. [DOI] [PubMed] [Google Scholar]


