Abstract
Background
The main indications for surgery for old thoracolumbar fractures are pain, progressive deformity, neurological damage, or increasing neurological deficit. These fractures have been one of the greatest therapeutic challenges in spinal surgery. Anterior, posterior, or combined anterior and posterior procedures have been successful to some extent. As far as we know, there is no report in the literature of transforaminal lumbar interbody fusion (TLIF) for old thoracolumbar fracture and dislocation.
Methods
Case report.
Results
A 26-year-old man with old fracture and dislocation of T12/L1 was treated with TLIF. At 12 months' follow-up, multi-slice computed tomography (CT) scans showed that solid fusion had been achieved between T12 and L1. Back pain had resolved completely at 2-year follow-up.
Conclusions
We performed TLIF for in a man with old fracture and dislocation of T12/L1, with good clinical outcome. TLIF might be an option in the treatment of old thoracolumbar fracture.
Keywords: Transforaminal lumbar interbody fusion, Old thoracolumbar fracture, Treatment
Introduction
Surgery for old thoracolumbar fracture focuses on the correction of deformity, decompression of neurologic tissue, rebuilding of spinal balance, and relief of persistent back pain.1–4 Anterior, posterior, or combined anterior and posterior procedures have been successful to some extent.5–7 In light of the differences in pathological conditions in each case, selection of appropriate surgical procedure is crucial. An ideal procedure should be simple, carry minimal risk, and be minimally invasive. This patient with old fracture and dislocation of T12/L1 underwent transforaminal lumbar interbody fusion (TLIF). As far as we know, there is the first published report of TLIF for old thoracolumbar fracture and dislocation.
Case report
A 26-year-old man was injured by a motor vehicle. He was diagnosed initially as having ‘lumbar fracture’ and advised to take bed rest. Six weeks later, he complained of back pain when he started to ambulate without any spinal support such as corset and bracing. Bed rest relieved the pain. Four months later, the patient revisited the clinic because of escalating pain. Radiographs showed an L1 old fracture and anterior displacement of T12 on L1. The patient was again treated conservatively. Because of persistence and aggravation of the pain, he came to our hospital 6 months after injury. Computed tomography (CT) and magnetic resonance imaging (MRI) confirmed L1 old fracture and spondylolisthesis of T12/L1 (Figs 1A–C). The patient was hospitalized for surgery.
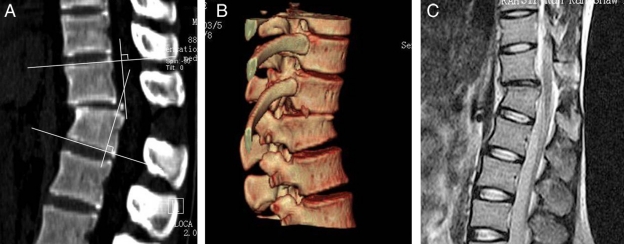
Figure 1.
(A) CT sagittal reconstruction image showing trans-injury of posterior ligamentous structures and intervertebral disk, and the preoperative Cobb angle. (B) CT three-dimensional reconstruction with volume rendering showing T12/L1 dislocation. (C) MRI showing wedged change of L1 and anterior spondylolisthesis of T12. MRI signal of vertebral body did not change significantly.
Operative and postoperative course
A left TLIF with instrumentation was performed with the patient in prone position on the operating table. Under general anesthesia, the spine was exposed through a midline incision at the level of T12/L1. The muscle was separated subperiosteally from the lamina bilaterally. Pedicle screws (Click'X, AO Synthes) were sized and inserted bilaterally at T12 and L1 under the guidance of C-arm fluoroscopic imaging. Since the left zygapophysial joints were locked, the left intervertebral foramen was decompressed. The nerve root was retracted to expose the disk. A rectangular incision was made in the disk and an interbody spacer was inserted into the intervertebral space. A maximum disk distraction was obtained by inserting the interbody spacer from 7 to 9 mm in height in 1-mm increments. Reduction was carried out by a right pedicle screws– rods system. Disk material and cartilage endplates were removed through the left intervertebral foramen, and the endplates were prepared for cage grafting. After the anterior intervertebral space was filled with granular laminar bone, harvested iliac cancellous bone chips, 9 mm in height cage (Travlos, AO Synthes) filled with granular bone, were implanted in the exact position of the intervertebral space. After confirmation of the ideal reduction and good position of cages by C-arm fluoroscopy, the screw–rod system was tightened. The construction was compressed to establish an optimal graft–bone interface and restore the physiological curve. Additionally, the right vertebral lamina was prepared for grafting bone to achieve a 270° fusion. Intraoperative monitoring of the spinal cord was used to detect any change in neurologic function during surgical manipulation.
Before closing the incision, a drainage tube was placed in the surgical decompressed field. The tube was removed at 36 hours after surgery. There were no intraoperative and postoperative complications. Anteroposterior and lateral radiographs taken on the second postoperative day showed that the position of screws and cages was good and the dislocation was well reduced (Figs 2A and B). The patient was encouraged to ambulate wearing rigid bracing on the second day after surgery (Figs 2C and D). The patient was checked by multi-slice CT scans at 12 months after surgery, and showed that the solid fusion was achieved between T12 and L1. Back pain had resolved completely at 2-year follow-up. Spinal alignment was corrected and maintained effectively. The preoperative Cobb was −23°, and the corrected Cobb was −5° at 12 months after surgery.
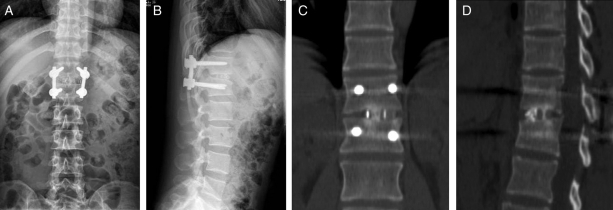
Figure 2.
(A) Anteroposterior radiographic image on the third postoperative day showing good position of screws and cages. (B) Lateral radiographic image on the third postoperative day showing good position of screws and cages and reduced dislocation. (C) Coronal CT image reconstruction at 12 months after surgery showing that bony trabeculation crossed the endplate interfaces and a solid fusion was achieved. (D) Sagittal CT image reconstruction at 12 months after surgery showing that bony trabeculation crossed the endplate interfaces and a solid fusion was achieved. The postoperative Cobb angle was measured.
Discussion
Improper treatment or occult instability may result in serious complications such as internal fixation failure, segment instability, progressive deformity, neurological damage, and increasing pain in patients with thoracolumbar fractures. These complications have been one of the greatest therapeutic challenges to spinal surgery.5,8–10 Keene et al.11 reported that of 106 patients who had operative stabilization of thoracolumbar fractures, 16 (15%) underwent surgery again 4 months to 16 years later for chronic instability. Vaccaro et al.5 believed that the injuries involving the posterior ligamentous structures, such as advanced burst flexion-compression injuries or flexion-distraction injuries, were prone to posttraumatic deformity and increasing pain if preventive measures were not taken. The current case was B1.2.2 according to AO classification, and the posterior ligamentous structures and intervertebral disk were trans-injured after the wedged fracture of L1 and anterior dislocation of T12/L1. Conservative treatment for this injury was inadequate. Furthermore, ambulation without any spinal support 6 weeks later might also be one of the causes for persistent symptoms.
For old thoracolumbar fractures, pain, progressive deformity, neurological damage, or increasing neurological deficit are the main indications for surgery.4,12,13 The objective of surgery is to correct deformity, decompress neurologic tissue, rebuild spinal balance, and relieve the persistent back pain.1–4 This patient had pain that was refractory to conservative treatment 6 weeks after initial trauma, and CT and MRI confirmed the instability of T12/L1 and anterior spondylolisthesis of T12. Hence, surgical intervention was clearly indicated.
The proposed surgical procedures include anterior, posterior, or combined anterior and posterior procedures.5–7,13 Because of lack of anterior column support, posterolateral fusion with internal fixation may expose the instrumentation to excessive tension, the fixed segment being especially prone to kyphosis. Long-term complications including failure of internal fixation and pseudoarthrosis might occur.4 In this case, posterolateral fusion was precluded by the severely degenerative disk, narrowed intervertebral space, and local kyphosis. Posterior osteotomy has been used in the treatment of rigid kyphotic deformity.13 In this case, instability was caused by injury of the posterior ligamentous structures and disk, osteotomy was not indicated. If surgery is restricted to an anterior approach, correction of the dislocation and deformity is limited by proximity to posterior structures, and the absence of posterior tension band owing to the injury of ligamentous structures might bring about long-term complications, such as kyphotic deformity or internal fixation failure.1 Combination of posterior and anterior approaches has some advantages, including complete decompression and good reduction. But this technique requires two separate procedures, with increased operative time and morbidity.14
In this patient, preoperative CT and MRI did not reveal stenosis of the central canal and intervertebral foramina and the function of the spinal cord was also normal after trauma. The pain was closely related to posture, and the segment instability was verified. The pain might be due to spinal instability and its abnormal forces on soft tissue. Therefore, surgery was performed to reduce dislocation of T12/L1 and rebuild spinal stability. The fracture of L1 has healed and collapse of the vertebral body was minimal. The change in shape of the L1 body was similar to the sacral dome in spondylolisthesis of L5/S1. It was felt that treatment using surgical methods for lumbosacral spondylolisthesis could be beneficial in this patient. Thus, the popular TLIF procedure was selected. In contrast to other surgical procedures, TLIF has the following advantages: (1) spinal alignment and physiological curve return to normal. Anterior column support and posterior tension band are achieved to maintain reduction; (2) most posterior column structures are preserved; (3) it is unnecessary to retract the nerve roots and thecal sac; (4) through a single approach, the procedure is easy to perform with shorter operative time and less trauma and risk; (5) a larger area is provided for grafting bone, and a 270° fusion can be performed.
In old thoracolumbar fracture, the dura mater might adhere to the surrounding tissues. During surgery, especially in the process of reduction, the spinal cord might be stimulated or be at risk of damage. Therefore, the spinal cord should be monitored intraoperatively to detect any change in neurologic function. In this case, no neurological complications were found in intraoperatively or postoperatively. Hence, with carefully performing and monitoring the spinal cord, TLIF for old thoracolumbar fracture should be safe.
Conclusion
In conclusion, TLIF has been widely used to treat lumbar degenerative diseases. However, to our knowledge, there are no published reports of TLIF for old thoracolumbar fracture. We found that the procedure was applicable with good clinical outcome in this case. TLIF might be a treatment option for old thoracolumbar fracture.
References
- 1.Been HD, Poolman RW, Ubags LH. Clinical outcome and radiographic results after surgical treatment of post-traumatic thoracolumbar kyphosis following simple type A fractures. Eur Spine J 2004;13(2):101–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khoueir P, Oh BC, Wang MY. Delayed posttraumatic thoracolumbar spinal deformities: diagnosis and management. Neurosurgery 2008;633 Suppl:117–24 [DOI] [PubMed] [Google Scholar]
- 3.Regnicolo L, Messori A, Polonara G, Burroni E, Perugini S, Salvolini U. MRI assessment of post-traumatic spinal instability. Eur J Radiol 2002;42(2):154–9 [DOI] [PubMed] [Google Scholar]
- 4.Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J 2008;8(4):666–77 [DOI] [PubMed] [Google Scholar]
- 5.Vaccaro AR, Silber JS. Post-traumatic spinal deformity. Spine 2001;2624 Suppl:S111–8 [DOI] [PubMed] [Google Scholar]
- 6.Zelle BA, Dorner J. Management of late posttraumatic kyphosis with anterior Z-plate instrumentation. Am J Orthop 2008;37(2):76–80 [PubMed] [Google Scholar]
- 7.Suk SI, Kim JH, Lee SM, Chung ER, Lee JH. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine 2003;28(18):2170–5 [DOI] [PubMed] [Google Scholar]
- 8.Koller H, Acosta F, Hempfing A, Rohrmüller D, Tauber M, Lederer S, et al. Long-term investigation of nonsurgical treatment for thoracolumbar and lumbar burst fractures: an outcome analysis in sight of spinopelvic balance. Eur Spine J 2008;17(8):1073–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Briem D, Behechtnejad A, Ouchmaev A, Morfeld M, Schermelleh-Engel K, Amling M, et al. Pain regulation and health-related quality of life after thoracolumbar fractures of the spine. Eur Spine J 2007;16(11):1925–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briem D, Lehmann W, Ruecker AH, Windolf J, Rueger JM, Linhart W. Factors influencing the quality of life after burst fractures of the thoracolumbar transition. Arch Orthop Trauma Surg 2004;124(7):461–8 [DOI] [PubMed] [Google Scholar]
- 11.Keene JS, Lash EG, Kling TF., Jr Undetected posttraumatic instability of ‘stable’ thoracolumbar fractures. J Orthop Trauma 1988;2(3):202–11 [DOI] [PubMed] [Google Scholar]
- 12.Illés T, de Jonge T, Domán I, Dóczi T. Surgical correction of the late consequences of posttraumatic spinal disorders. J Spinal Disord Tech 2002;15(2):127–32 [DOI] [PubMed] [Google Scholar]
- 13.Shimode M, Kojima T, Sowa K. Spinal wedge osteotomy by a single posterior approach for correction of severe and rigid kyphosis or kyphoscoliosis. Spine 2002;27(20):2260–7 [DOI] [PubMed] [Google Scholar]
- 14.Swan J, Hurwitz E, Malek F, van den Haak E, Cheng I, Alamin T, et al. Surgical treatment for unstable low-grade isthmic spondylolisthesis in adults: a prospective controlled study of posterior instrumented fusion compared with combined anterior-posterior fusion. Spine J 2006;6:606–14 [DOI] [PubMed] [Google Scholar]