Abstract
Cytotoxic T lymphocytes and natural killer cells utilize the perforin/granzyme cytotoxic pathway to kill virally-infected cells and tumors. Human regulatory T cells also express functional granzymes and perforin and can induce autologous target cell death in vitro. Perforin-deficient mice die from excessive immune responses after viral challenges, implicating a potential role for this pathway in immune regulation. To further investigate the role of granzyme B in immune regulation in response to viral infections, we characterized the immune response in wild-type, granzyme B deficient, and perforin deficient mice infected with Sendai virus. Interestingly, granzyme B deficient mice, and to a lesser extent perforin deficient mice, exhibited a significant increase in the number of Ag-specific CD8+ T cells in the lungs and draining lymph nodes of virally infected animals. This increase was not the result of failure in viral clearance since viral titers in granzyme B-deficient mice were similar to wild-type mice and significantly less than perforin-deficient mice. Regulatory T cells from WT mice expressed high levels of granzyme B in response to infection, and depletion of regulatory T cells from these mice resulted in an increase in the number of Ag-specific CD8+ T cells, similar to that observed in granzyme B-deficient mice. Furthermore, granzyme B-deficient regulatory T cells displayed defective suppression of CD8+ T cell proliferation in vitro. Taken together these results suggest a role for granzyme B in the regulatory T cell compartment in immune regulation to viral infections.
Introduction
Cytotoxic CD8+ T cells and NK cells utilize granzyme (Gzm) and perforin (Prf) molecules packaged in cytotoxic granules to kill virally-infected cells and tumors. Gzms are known to activate target cell apoptosis through caspase-dependent and independent pathways1, while Prf is implicated in the delivery of these cytotoxic molecules into target cells2. Among the Gzm family, GzmB, which cleaves target proteins after aspartate residues, has the strongest proapoptotic function2 resulting in DNA fragmentation and rapid loss of membrane integrity. While perforin deficient (Prf1−/− ) mice are susceptible to a variety of viruses and tumor models, GzmA (Gzma−/−) or GzmB-deficient (Gzmb−/−) mice show variable resistance to viral and tumor challenges3–7. This can be explained by the redundancy of granzymes, while there is no redundant molecule for perforin. When mice are deficient in both GzmB and GzmA they exhibit greater susceptibility to certain pathogens compared to Gzma−/− or Gzmb−/− mice8–9.
While the role of Prf and Gzms in viral clearance is well-defined, recent evidence suggests a paradoxical role for this pathway in immune regulation, as demonstrated by the human disease Hemophagocytic Lymphohistiocytosis (HLH). Patients with HLH exhibit uncontrolled immune responses after viral infections evidenced by elevated levels of proinflammatory cytokines, subsequent activation of macrophages, phagocytosis of hematopoietic cells, and tissue damage10–12. All genetic mutations underlying primary HLH are in proteins that are critical for either the functional degranulation of cytotoxic granules (e.g. SAP, Munc13-4, Lyst, Rab27A, Syntaxin 11), or the delivery of their cytotoxic contents into target cells as is the case in Prf deficiency10;12. Prf1−/− mice infected with lymphocytic choriomeningitis virus (LCMV) or murine cytomegalovirus (MCMV) develop a HLH-like syndrome due to uncontrolled expansion of Ag-specific CD8+ T cells, and excessive production of the proinflammatory cytokines IFN-γ and TNF-α9;13. While persistence of Ags due to failure in viral clearance likely contributes to the exaggerated immune response, the possibility remains that Prf and other components of the cytotoxic granule pathway may be involved in regulating CD8+ T cell responses. This possibility is further supported by recent evidence that GzmB and Prf can be used by T regulatory (Treg) cells to regulate immune responses.
Treg cells are a subset of CD4+ T cells that have been shown to control the immune response to auto-, allo-, pathogen-derived, and tumor Ags14–17. They account for 5–10% of CD4+ T cells in the periphery, constitutively express CD2518–20, and utilize a variety of mechanisms to suppress immune responses, including cytotoxicity through the Prf/Gzm pathway21–23. Two recent reports have demonstrated that murine CD4+CD25+ Treg cells upregulate GzmB in response to TCR activation, and can suppress proliferation of CD4+CD25− T cells and LPS-activated B cells in a GzmB-dependent manner24–25. Furthermore, CD4+CD25− T cells that overexpress the physiologic GzmB inhibitor serine protease inhibitor 6 (Spi6) are resistant to Treg cell suppression26–29. Additionally, in vitro activated human Treg cells have been shown to differentially upregulate Gzms, and display Prf-dependent cytotoxicity against a variety of autologous target cells including mature and immature dendritic cells, CD14+ monocytes, and activated CD8+ and CD4+ T cells21.
These studies implicate the Gzm/Prf pathway in immune regulation, possibly through the Treg cell compartment. Since little is known about the role of GzmB in immune regulation following viral infections, we set out to characterize the immune response of wild-type (WT) mice, Gzmb−/− mice, and Prf1−/− mice to Sendai Virus (SeV). SeV is a mouse parainfluenza type I virus that causes severe descending bronchiolitis in rodents30–32. Resolution of primary SeV infection is strictly CD8+ T cell-dependent33;34, and infection of WT C57BL/6 mice with SeV is known to elicit a potent CD8+ T cell response that is almost exclusively directed at a single Kb-restricted nucleoprotein epitope (NP 324–332)35–38. This allows the use of a class I tetramer loaded with NP 324–332 to characterize Ag-specific CD8+ T cell responses to SeV infection. Using this model, we found that SeV-infected Gzmb−/− mice displayed great weight loss compared with WT mice that correlated with an increase in the number of Ag-specific CD8+ T cells despite efficiently clearing the virus. Furthermore, this phenotype was Treg cell-dependent suggesting that GzmB is important for the ability of Treg cells to regulate Ag-specific CD8+ T cell responses.
Materials and Methods
Mice
WT C57BL/6J mice were obtained from the Jackson Laboratory (Bar Harbor, ME). Prf1−/− mice containing the “Kagi” mutation3 and Gzmb−/− mice39 were a kind gift from Timothy J. Ley, and were backcrossed for eleven generations onto the C57BL/6J strain. The Gzmb−/− mice were the Gzmb−/−-Cre mice, and thus only Gzmb−/− was deficient. Foxp3EGFP mice contain a bicistronic FoxP3 locus that express GFP under the control of the endogenous/enhancer elements of FoxP3, a transcription factor required for the development and function of Treg cells16. Foxp3EGFP mice were a kind gift from Talal A. Chatila (University of California-Los Angeles) and were crossed to Gzmb−/− mice and Prf1−/− mice. All mice were bred and housed under specific pathogen-free conditions, and all experiments were conducted in accordance with the guidelines of the institutional Animal Research Committee at the Medical College of Wisconsin.
Viral infection
Male mice of 6–12 weeks of age were anesthetized with ketamine and xylazine, and inoculated intranasally with 6×104 PFU of SeV (Fushimi strain, ATCC) in 30μl of PBS. This dose was used since preliminary experiments with 2×105 PFU resulted in excessive mortality in Prf1−/− mice. Individual mice were weighed before and every day after infection. Percentage of baseline weight loss was calculated using the following formula: [weight/weight at day 0] * 100%.
Lung SeV titer
Lungs were harvested from mice sacrificed at day 10, flash frozen in liquid nitrogen, then homogenized in TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA) to extract RNA. cDNA was synthesized from 4 μg of RNA using QuantiTect Reverse Transcription cDNA synthesis kit (Applied Biosystems, Foster City, CA), and SeV nucleocapsid gene expression was measured by real-time quantitative PCR using Taqman PCR Master Mix (Applied Biosystems). The primers and probes were developed in Dr. Michael Holtzman’s laboratory at Washington University in St. Louis40. The gapdh house keeping gene was detected in the cDNA samples using Gapdh primers and probe (Applied Biosystems). Construct standard curves were used for quantification as previously described32.
Antibodies
Fluorochrome-labeled antibodies were utilized according to the manufacturers’ recommendations as follows: Pacific Blue anti-CD4 (RM4-5), Pacific Orange anti-CD8a (5H10), and R-PE anti-Granzyme B (GB12) were from Invitrogen Life Technologies(Carlsbad, CA); PE-Cy7 anti-CD11c (HL3), PE-Cy7 anti-IFN-γ (XMG1.2), PE-Cy7 anti-CD25 (PC61) were from BD PharMingen (San Diego, CA); PE-Cy5.5 anti-CD19 (eBio1D3), PE anti-CD62L (MEL-14), PE-Cy7 anti-NK1.1 (PK136) were from eBioscience (San Diego, CA); Alexa 700 anti-CD44 (IM7) was from Biolegend (San Diego, CA); functional grade Rat IgG1 (HRPN) was from Bio X Cell (West Lebanon, NH). PC61 (anti-CD25 mAb) and 2C11 (anti-CD3 mAb) hybridomas were purchased from the American Tissue Culture Collection (Manassas, VA), and Abs were generated and purified from tissue-cultured supernatants.
Flow cytometry
Lungs and draining lymph nodes were harvested at indicated time points. Lungs were minced, and digested at 37°C for 60 min in media containing DMEM supplemented with 10% FBS, 1% glutamine, 1% non essential amino acids, 1% sodium pyruvate, 1% penicillin/streptomycin, 10 mM HEPES (Invitrogen Life Technologies), 250 U/ml collagenase I, 50 U/ml DNase I (Worthington Biomedical, Lakewood, NJ), and 0.01% hyaluronidase (Sigma-Aldrich, St. Louis, MO). During the last 15 min of incubation time, EDTA (Fisher Scientific, Hanover Park, IL) was added to the medium to a final concentration of 2 mM. After digestion, single-cell suspensions were obtained by passing the cell mixture through a 40μm cell strainer, then erythrocytes were removed by hypotonic lysis. Recovered cells were then enumerated for total cell count and stained for cell surface markers. Ag-specific CD8+ T cells were detected using a MHC-peptide tetramer specific for SeV nucleoprotein NP324–332 provided by the National Institute of Allergy and Infectious Disease Tetramer Core Facility (Bethesda, MD). Intracellular staining for GzmB was conducted using BD Cytofix/Cytoperm and BD Perm/Wash buffers (BD Biosciences, San Jose, CA) according to the manufacture’s recommendations. To detect intracellular IFN- γ, cells isolated from infected lungs were incubated with 50 ng/ml PMA (Sigma-Aldrich), 500 ng/ml ionomycin (Sigma-Aldrich), and 10 mg/ml brefeldin A (Sigma-Aldrich) for 4 h at 37°C and stained as described earlier. Samples were analyzed on an LSRII (BD Biosciences) and FlowJo software (Tree Star, Ashland, OR). A minimum of 1×106 live cell events were collected per sample.
Treg cell depletion with a blocking anti-CD25 mAb
Mice were depleted of Treg cells by intraperitoneal injection of 300μg of anti-CD25 (PC61) mAb (or rat IgG1 control Ab) at day -3 and day -1 of SeV infection. This mAb is known to antagonize Treg cell function and results in a reduction in the number of CD4+ CD25+ Treg cells in the peripheral lymphoid tissues41–42.
CD8 + T Suppression assays
CD4+ T cells were enriched from whole splenocytes by magnetic cell sorting using CD4 Microbeads and MACS columns (Miltenyl Biotec Inc., Auburn, CA), and CD4+EGFP+ Treg cells were further purified by cell sorting using a FACS ARIA (BD Biosciences). CD8+ T cells were isolated by cell sorting. Cell purity was more that 97% for all experiments. T-cell depleted splenocytes (TdS) were irradiated with 5000 rad. Purified cell populations were suspended in DMEM supplemented with 10% (v/v) fetal bovine serum (FBS), 1% glutamine, 1% non essential amino acids, 1% sodium pyruvate, 1% penicillin/streptomycin, and 10 mM HEPES. 5×104 CD8+ T cells were added to each well in flat-bottom microtiter plates, and were cultured in the presence of 1.5 x105 APCs and 5μg/ml of anti-CD3 Ab, with either WT or Gzmb−/− Treg cells to achieve the indicated suppressor cells to target cells ratios (S:T). Cultures were incubated for 72 h at 37°C with 5% CO2, pulsed with 0.2 μCi/well [3H] thymidine for an additional 18 h, harvested onto fiber filtermats using a Micro96 harvester (Skatron), and counted.
Statistical analysis
Student’s unpaired t test (for comparison of two groups), or one-way or two-way ANOVA (for comparison of multiple groups) followed by Tukey’s multiple comparison test were performed using Prism software (Graph Pad, San Diego, CA) to determine significance. Unless otherwise stated, all data are presented as mean ± SEM.
Results
SeV infection and viral clearance in Gzmb−/− mice and Prf1−/− mice
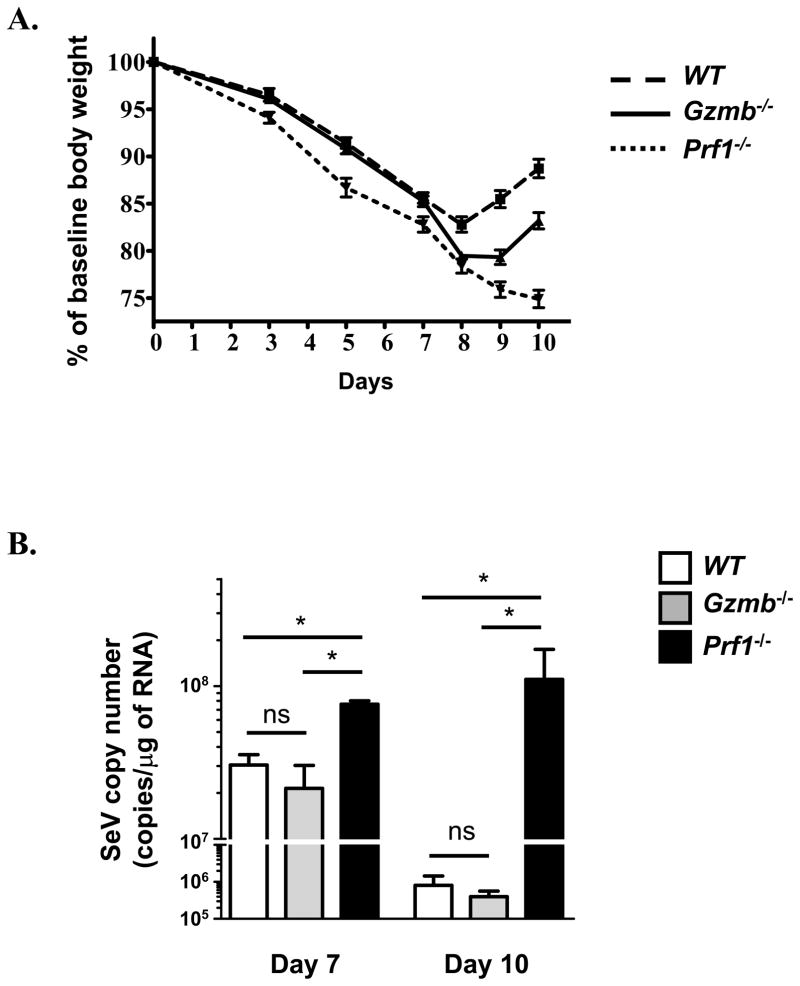
To examine the role of GzmB in SeV infection, we infected WT mice, Gzmb−/− mice, and Prf1−/− mice with SeV. SeV infection in mice induces an acute inflammatory response accompanied by significant weight loss32. Gzmb−/− mice infected with SeV lost more weight and took longer to recover than WT mice (Fig. 1A). In comparison, Prf1−/− mice exhibited the greatest weight loss. H&E-stained lung sections from all mice showed peri-bronchial lymphocyte-rich inflammatory infiltrates, as well as dispersed areas of alveolitis and capillary congestion. Sheets of apoptotic bronchiolar epithelium desquamating into the lumen indicating more severe pathology were observed in Prf1−/− mice and, to a lesser extent, in Gzmb−/− mice, but not WT mice (data not shown).
Figure 1. Response to SeV infection.
A. Weight loss of WT, Gzmb−/−, and Prf1−/− mice infected with 6×104 PFU SeV depicted as percent weight loss from baseline (n=50 for WT, 52 for Gzmb−/− mice, and 28 for Prf1−/− mice). Significant differences in weight loss were detected at day 8 (WT vs. Prf1−/−, p<0.01; WT vs Gzmb−/−, p<0.01), day 9 (WT vs. Prf1−/−, p<0.001; WT vs Gzmb−/−, p<0.001; Prf1−/− vs. Gzmb−/−, p<0.05) and day 10 (WT vs. Prf1−/−, p<0.001; WT vs Gzmb−/−, p<0.001; Prf1−/− vs. Gzmb−/−, p<0.001). Significance was determined by Two-way repeated measures ANOVA. B. Viral RNA copy number in the lungs was determined at days 7 and 10 by real-time RT-PCR for SeV nucleocapsid protein. (n=3–6 mice in each group from 2 separate experiments, *, p<0.05).
We next determined if the absence of GzmB affects viral clearance by measuring viral titers from total lung homogenate by quantitative real-time RT-PCR at day 10 of infection. The results of this assay have been shown to correlate with viral plaque assay and expression of SeV proteins as detected by western blotting32. Prf1−/− mice displayed a significant increase in viral titers compared with WT mice, consistent with the well-established role of Prf in viral clearance. Gzmb−/− mice, on the other hand, exhibited similar viral titers to WT mice at both 7 and 10 days after infection, indicating that GzmB is not essential for clearance of SeV (Fig. 1B).
Expansion of CD8+ T cell compartment in the lungs of Gzmb−/− mice and Prf1−/− mice in response to SeV infection
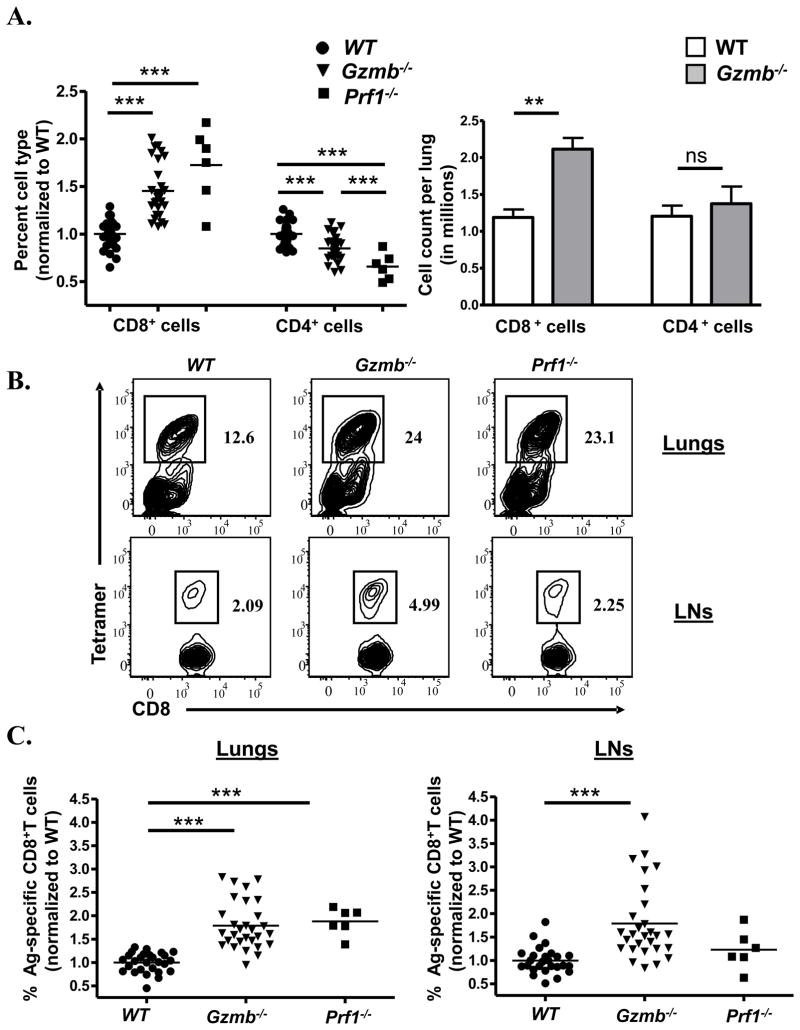
While Gzmb−/− mice did not appear to have a defect in SeV clearance, they clearly exhibited a less favorable outcome to infection, likely due to immune-mediated pathology. To address whether GzmB has a role in regulating anti-viral immune responses, we characterized the magnitude of Ag-specific CD8+ T cell responses in the lungs and draining lymph nodes of these mice. Upon infection with SeV, CD8+ T cells in the lungs of Gzmb−/− and Prf1−/− mice underwent a significant expansion compared to WT mice, with a concomitant decrease in the percentages of CD4+ T cells (Fig. 2A, left panel). This was confirmed by determining absolute numbers of CD4+ and CD8+ T cells in the lungs following infection (Fig. 2A, right panel). Furthermore, Gzmb−/− mice, and to a lesser extent Prf1−/− mice, exhibited a significant increase in the percentages of Ag-specific CD8+ T cells at day 10 of infection (Fig. 2B–C). Similar results were obtained when absolute cell counts were analyzed (data not shown). There was no statistically significant differences in the percentages or absolute numbers of CD19+ cells (B-cells), CD11c+ cells (dendritic cells), or NK1.1+ cells (NK cells) (data not shown).
Figure 2. Expansion of CD8+ T cell compartment in the lungs of Gzmb−/− mice and Prf1−/− mice in response to SeV infection.
WT, Gzmb−/−, and Prf1−/− mice were infected with 6×104 PFU SeV and lungs analyzed by flow cytometry. A. Left: Percent CD4+ and CD8+ T cells from live cell gate in the lungs following SeV infection. Results from each experiment were normalized to WT, and data presented as fold increase over WT samples. Right: Absolute cell count in the lungs following SeV infection. B. Representative FACS plots demonstrating Ag-specific CD8+ T cells in the lungs and draining lymph nodes of infected animals. The plots from the lymph nodes were first gated on CD8+ T cells. C. Percent of CD8+ T cells that are tetramer positive was determined in the lungs and draining lymph node following SeV infection, then normalized to WT mice (n=27 for WT mice, 29 for Gzmb−/− mice, and 6 for Prf1−/− mice, **, p<0.01; and ***, p<0.001).
We also examined the Ag-specific CD8+ T cell response in the para-tracheal draining lymph nodes of infected mice. In contrast to the lungs, there was no relative expansion of CD8+ cells in the draining lymph nodes of Gzmb−/− mice or Prf1−/− mice and total lymphocyte numbers in the draining lymph nodes of these mice were comparable to those of WT mice (data not shown). There was, however, a definite increase in the percentages and absolute numbers of Ag-specific CD8+ T cells in the draining lymph nodes of Gzmb−/− mice but not Prf1−/− mice (Fig. 2B–C and data not shown). The percentages and absolute numbers of other cell types (CD19+ cells, CD11c+ cells, and NK1.1+ cells) were comparable to those of WT mice (data not shown).
In addition to their cytotoxic function, CD8+ T cells are efficient producers of antiviral cytokines such as IFN-γ. Therefore, we investigated the ability of Ag-specific CD8+ T cells from the lungs of WT mice, Gzmb−/− mice, and Prf1−/− mice to produce IFN-γ. Ag-specific CD8+ T cells from all mice produced IFN-γ in response to PMA/ionomycin stimulation to a similar magnitude (Fig 3A). However, Gzmb−/− mice displayed a relative increase in the percent and number of IFN-γ+ CD8+ T cells due to the underlying expansion of Ag-specific CD8+ T cells in these mice.
Figure 3. Expression of IFN-γ and CD25 in Ag-specific CD8+ T cells in response to SeV infection.
A. WT, Gzmb−/−, and Prf1−/− mice were infected with 6×104 PFU SeV, lymphocytes were isolated from the lungs, stimulated with PMA/ionomycin, and IFN-γ was detected by intracellular staining. Representative FACS plots showing IFN-γ expression in Ag specific and non-Ag specific CD8+ T cells. FACS plots were gated on CD8 cells. B. The percent of conventional CD4+ T cells, Treg cells, and Ag-specific and non Ag-specific CD8+ T cells expressing CD25 was determined by flow cytometry (*, p<0.05; **, p<0.01; and ***, p<0.001).
To determine whether GzmB plays a role in regulating the activation state of immune effector cells, we investigated the expression of memory-activation markers CD44, CD62L, and CD25 on CD8+ T cells in SeV-infected mice. Not surprisingly, similar to what has been described in WT mice43, almost all Ag-specific CD8+ T cells in the lungs of Gzmb−/− mice were of the effector memory (CD44hiCD62Llo) phenotype (data not shown). Interestingly, there was a significant increase in the percentage of CD25+Ag-specific CD8+ T cells in the lungs of Gzmb−/− mice compared to WT mice (Fig. 3B). This phenotype was even more pronounced in the draining lymph nodes where up to 60% of Ag-specific CD8+ T cells in Gzmb−/− mice expressed high levels of CD25 (Fig. 3B). On the other hand, CD25 expression in Treg cells and conventional CD4+ T cells was not significantly affected by the lack of GzmB. Taken together, these data argue that GzmB has a role in regulating the magnitude and activation status of Ag-specific CD8+ T cell responses to SeV.
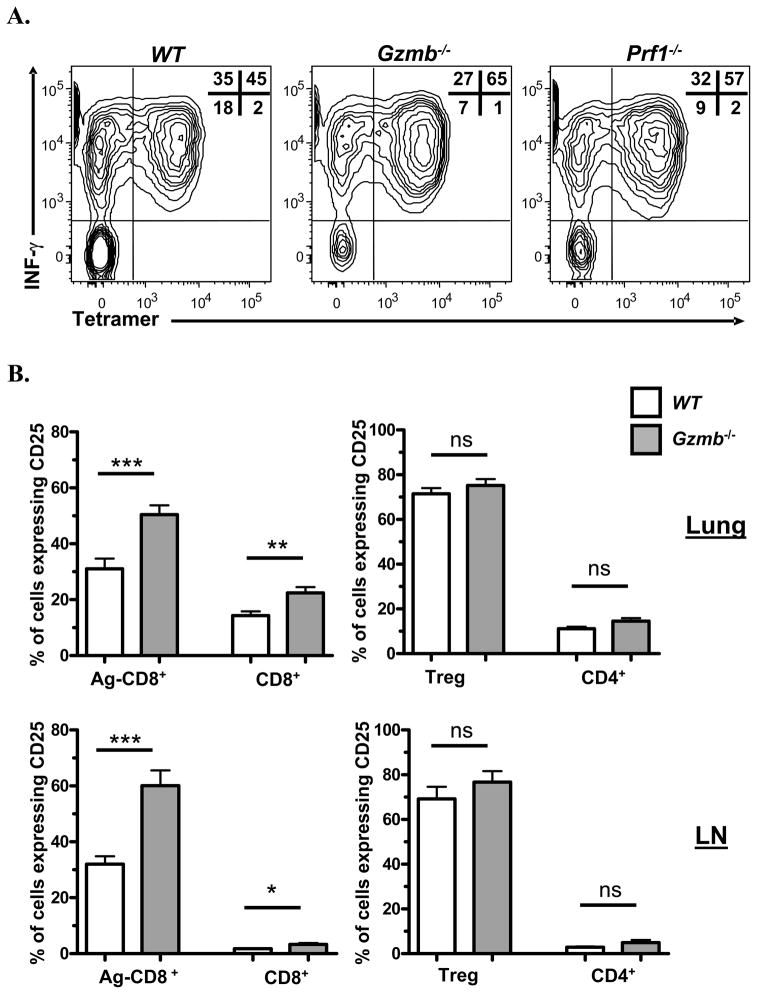
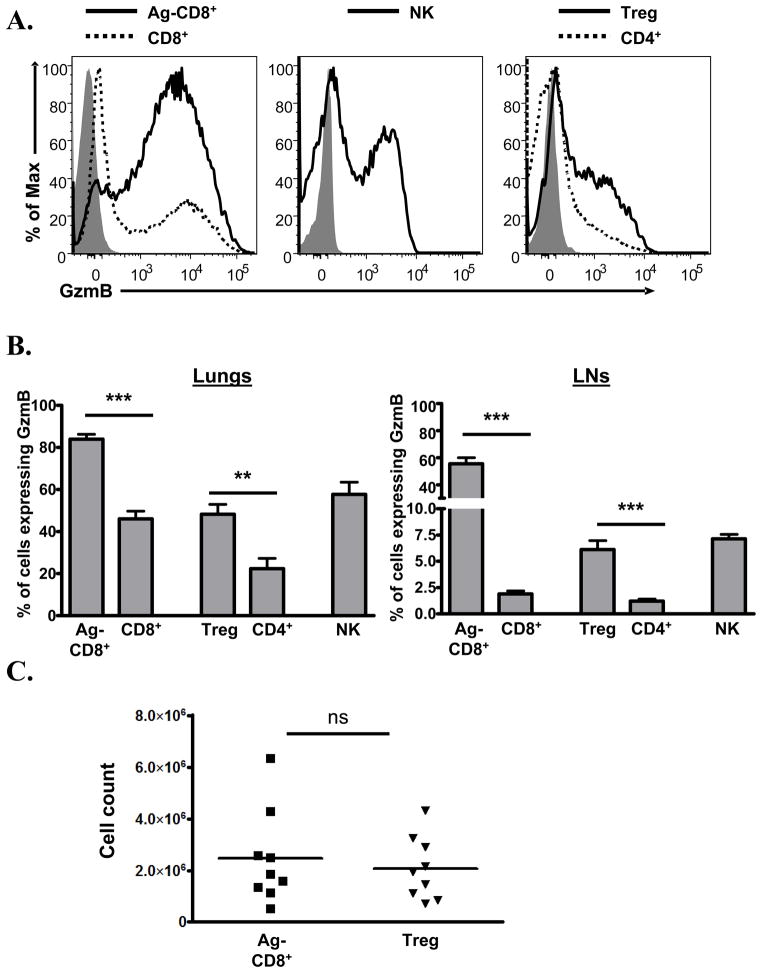
Expression patterns of GzmB in lymphocytes in the lungs and draining lymph nodes of SeV-infected mice
To further investigate the source of GzmB responsible for regulating Ag-specific CD8+ T cell activation/expansion, we examined the expression pattern of GzmB in the lungs and draining lymph nodes of Foxp3EGFP mice during SeV infection. Not surprisingly, at day 10, GzmB was expressed in the majority of NK cells (NK1.1+ cells), Ag-specific CD8+ T cells, and to a lesser extent, non Ag-specific CD8+ T cells isolated from the lungs of WT mice (Fig. 4A–B) and Prf1−/− mice (data not shown). Interestingly, while only a limited percentage of conventional CD4+ T cells expressed GzmB, a significantly larger percentage of Treg cells in the lungs of infected mice upregulated GzmB (Fig. 4A–B). In the draining lymph nodes, around 55% of Ag-specific CD8+ T cells and 5–10% of Treg cells expressed GzmB, with minimal expression in conventional CD4+ T cells (Fig. 4B). Indeed, when absolute counts were analyzed there were roughly equal numbers of GzmB+ Treg cells and GzmB+ Ag-specific CD8+ T cells in the draining lymph nodes of WT mice (Fig. 4C).
Figure 4. GzmB expression in immune effector cells in response to SeV infection.
WT Foxp3EGFP locus-tagged mice were infected with 6×104 PFU SeV and analyzed for GzmB expression 10 days later. A. Representative histograms showing GzmB expression in different cell populations in the lungs of an infected animal. Shaded histogram represents background staining using Gzmb−/− mouse. B. Expression of GzmB was determined by flow cytometry and depicted as the percent of each cell population expressing GzmB in the lungs and draining lymph nodes. C. Absolute number of GzmB+ Tregs cells and GzmB+ Ag-specific CD8+ T cells was determined from the draining lymph nodes (**, p<0.01; and ***, p<0.001).
Treg cells are recruited to the lungs of infected mice
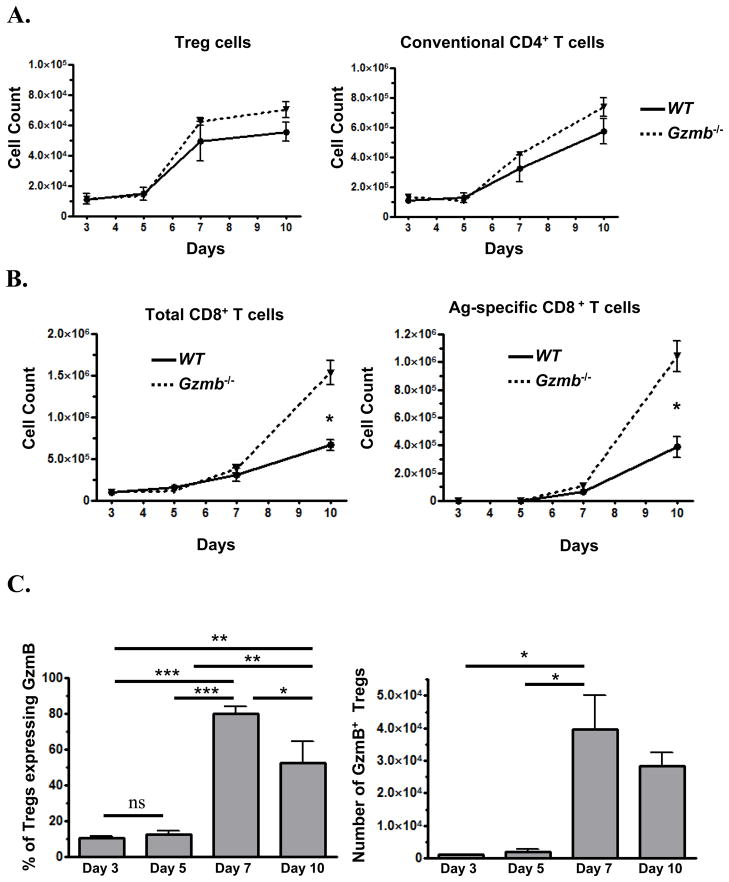
We next examined the kinetics of lymphocyte recruitment to the lungs, and GzmB expression by these cells in response to SeV infection. At day 7, we observed a doubling in the absolute numbers of FoxP3+ Treg cells in the lungs of WT mice in both WT mice and Gzmb−/− mice (Fig. 5A), indicating that these molecules probably do not play a significant role in the expansion or contraction of Treg cells. Expression of GzmB in WT Treg cells also peaked at day 7, with a high percentage of Treg cells in the lung expressing GzmB (Fig. 5C). Increased numbers of CD4+ and Ag-specific CD8+ T cells were first detected in the lungs at day 7 and continued to increase at day 10 (Fig. 5A–B). Significantly more Ag-specific CD8+ T cells were detected in the lungs of Gzmb−/− mice at day 10.
Figure 5. GzmB-expressing Treg cells are recruited to the lungs in response to SeV infection.
WT Foxp3EGFP mice were infected with 6×104 PFU SeV and analyzed for EGFP and GzmB expression at days 3, 5, 7, and 10. A. Quantification of Tregs cell and conventional CD4+ T cell numbers in the lungs. B. Quantification of total CD8+ T cell and Ag-specific CD8+ T cell numbers in the lungs. C. Percent (Left), and absolute count of GzmB+ Tregs cells (Right) in the lungs of infected animals (*, p<0.05; **, p<0.01; and ***, p<0.001).
Treg cells suppress CD8+ T responses in a GzmB-dependent manner
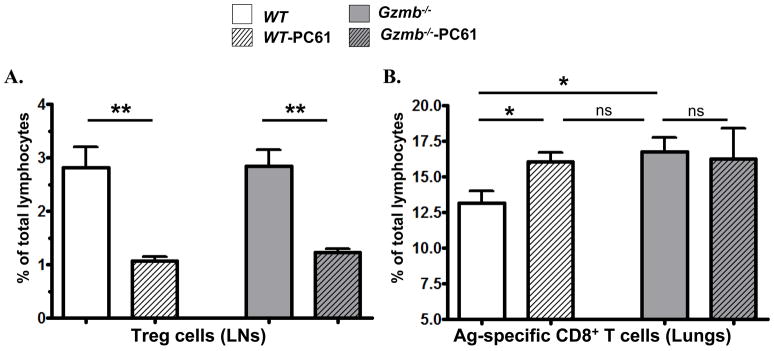
Since Gzmb−/− mice exhibit a defect in regulating Ag-specific CD8+ T cell responses, and since WT Treg cells express GzmB in vivo, we next tested whether depletion of WT Treg cells results in an expansion in Ag-specific CD8+ T cells similar to that observed in Gzmb−/− mice. Pre-treating WT mice with anti-CD25 mAb at days -3 and -1 of SeV infection resulted in a significant decrease in the percentages of FoxP3+ Treg cell in the lungs (data not shown) and the draining lymph nodes (Fig. 6A) of infected animals. This reduction in the number of Treg cells led to a significant increase in the percentages of Ag-specific CD8+ T cells in the lungs of these mice (Fig. 6B). Importantly, the increase in the percentages of Ag-specific CD8+ T cells was more pronounced in Treg cell-depleted WT mice than Treg cell-depleted Gzmb−/− mice, suggesting that the ability of Treg cells to regulate Ag-specific CD8+ T cell responses is mediated in part by GzmB.
Figure 6. Depletion of Treg cells results in expansion of Ag-specific CD8+ T cells in the lungs of WT mice in response to SeV infection.
WT mice and Gzmb−/− mice were pre-treated with anti CD25 mAb (PC61) or isotype at days -3 and -1, followed by infection with 6×104 PFU SeV. Lungs were analyzed for EGFP+CD4+ Treg cells and Ag-specific CD8+ T cells 10 days later. A. Percent of Treg cells in the draining lymph nodes of infected animals. B. Percent of Ag-specific CD8 cells in the lungs of infected animals (n=6 mice per group) (*, p<0.05; and **, p<0.01).
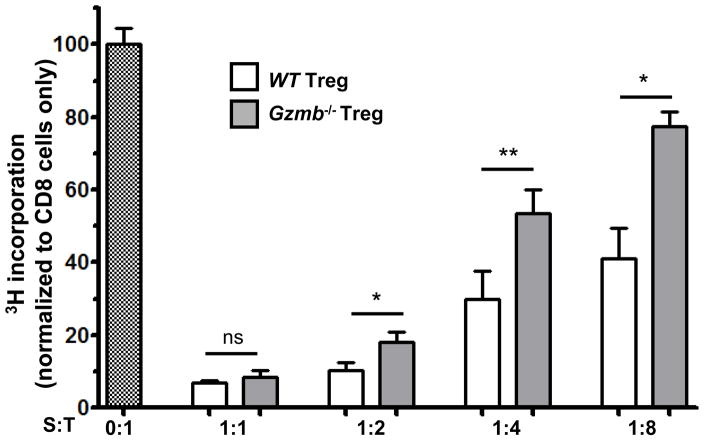
The above studies demonstrate a role for GzmB in regulating Ag-specific CD8+ T cell responses in vivo, and suggest that this effect may be mediated by Treg cells. We next directly tested whether GzmB is required for Treg cells to suppress CD8+ T cell proliferation in vitro. WT Treg cells were able to efficiently suppress CD8+ T proliferation in a dosedependent manner, while Gzmb−/− Treg cells displayed less suppression of CD8+ T cell proliferation (Fig. 7). This supports our findings in the SeV model that Treg cells regulate the immune responses to viral challenges in a GzmB-dependent manner.
Figure 7. Tregs cells suppress CD8+ T cell proliferation in a GzmB-dependent manner.
WT CD8+ T cells were cultured with WT or Gzmb−/− Treg cells in the indicated suppressor:target ratios (S:T) and stimulated with soluble anti-CD3 mAb. Proliferation of CD8+ T cells was assessed by [3H]thymidine incorporation at day 4. Data are the average of 9 replicates from 3 independent experiments normalized to CD8+ T cells proliferation without added Treg cells (*, p<0.05; and **, p<0.01).
Discussion
In this study we characterized the role of GzmB in immune regulation in a model of viral infection. Using the SeV model of acute respiratory bronchiolitis we demonstrated that Gzmb−/− mice, despite having intact viral clearance, exhibited greater weight loss than WT mice. This correlated with an expansion of Ag-specific CD8+ T cells in the lungs and draining lymph nodes of these mice. We further characterized the expression of GzmB in WT mice in this model and demonstrated that, in addition to CD8+ T cells and NK cells, Treg cells are efficient producers of GzmB, suggesting that GzmB expression in Treg cells may be required to inhibit the expansion of Ag-specific CD8+ T cells. In support of this, depletion of Treg cells in WT mice produced an expansion in Ag-specific CD8+ T cells similar to that observed in Gzmb−/− mice. Furthermore, Gzmb−/− Treg cells were deficient in their ability to suppress CD8+ T cell proliferation in vitro.
Infection of Prf1−/− mice with LCMV, MCMV, and Respiratory syncytial virus (RSV) is known to result in severe inflammatory responses with features of HLH along with failure to clear viral challenges9;13;44;45. Depletion of CD8+ T cells, IFN-γ13, or TNF-α9 ameliorates the increased mortality in these mice, arguing that CD8+ T cell-driven immune pathology is responsible for the observed morbidity and mortality. One possible explanation for these observations is that persistence of viral Ags, due to failure in viral clearance, results in prolonged and excessive CD8+ T cell activation, cytokine production, and immune pathology. However, in our model Gzmb−/− mice infected with SeV displayed viral titers comparable to WT mice indicating that GzmB is not essential for SeV clearance. While this is not surprising, due to redundancy in the antiviral roles of Gzms8;9;46, the expansion of Ag-specific CD8+ T cells and the corresponding enhanced weight loss in Gzmb−/− mice demonstrate a regulatory role for GzmB independent of its role in viral clearance.
These studies suggest that GzmB-expressing Treg cells contribute to the control of Ag-specific CD8+ T cells. In our model, we observed a significant increase in the number of Treg cells in the lungs of SeV infected mice. The majority of these cells expressed GzmB at day 7, indicating that viral infection is a potent inducer of GzmB expression in Treg cells. In addition, Treg cell depletion of WT mice with monoclonal antibodies to CD25 resulted in an increase in the percentages of Ag-specific CD8+ T cells similar to that seen in untreated Gzmb−/− mice. Finally, Gzmb−/− Treg cells demonstrated a reduced capacity to suppress CD8+ T cell proliferation in vitro. Although a role for GzmB expressed by cells other than Treg cells, such as Ag-specific CD8+ T cells and NK cells, cannot be ruled out, our data suggests a specific immune-regulatory role for GzmB in the Treg cell compartment in response to viral infection. Supporting these observations is the enhanced survival of Gzmb−/− mice to syngeneic tumor challenges due to inability of Treg cells in these mice to suppress effective CD8+ T and NK cell anti-tumor responses15. Similarly, FoxP3+ Treg cells were shown to induce dendritic cell death in a Prf-dependent manner in tumor draining lymph nodes, thereby limiting the onset of CD8+ T cell anti-tumor responses47. Additionally, different groups have demonstrated that Treg cells are recruited to sites of infection, and that immune responses specific to viruses are enhanced when CD4+CD25+ Treg cells are depleted in vivo4;48–50.
The increase in the number of Ag-specific CD8+ T cells in the lungs of Gzmb−/− mice indicates that GzmB in Treg cells regulates either the initiation of Ag-specific CD8+ T cell responses or the down modulation of terminal effector cells, or a combination of both. In addition, preliminary data from our lab show a trend toward increased antigen specific CD8 cells and total CD8 cells in the lungs of Gzmb−/− 55 days after infection, suggesting that control of the primary CD8+ T response may affect the magnitude of a memory response(data not shown). So far, in vivo studies have been inconclusive about the exact nature of the targets of GzmB-Treg cell-mediated immune suppression. Tumor infiltrating CD8+ T cells and NK cells in one model15, dendritic cells in another model47, and CD4+ T cells (but not CD8+ T cells) in yet another model29 have all been implicated. In our SeV model, Treg cells did not exhibit significant upregulation of GzmB until day 7. Additionally, there were no significant differences in the numbers or percentages of dendritic cells or B cells in either the lungs or the draining lymph nodes of Gzmb−/− mice. While this does not preclude a regulatory role for GzmB in the priming of the immune response by means other than inducing apoptosis of APCs or CD4 cells, we propose that GzmB has a direct down-modulating effect on Ag-specific effector CD8+ T cells. Whether this effect occurs in the lungs and/or the draining lymph remains to be seen. In support of this, the enhanced survival of Gzmb−/− mice in the tumor challenge model15 was attributed to the direct decrease in killing of CD8+ T cells and NK cells by tumor-infiltrating Treg cells deficient in GzmB. A direct down-modulating effect on Ag-specific CD8+ T cells as they are expanding would limit immune regulation to cells that are responsible for the observed immune-pathology after allowing for initiation of effective anti-viral immune responses.
One interesting finding in these studies was that Gzmb−/− mice exhibited a significant increase in the percentages of CD25+Ag-specific CD8+ T cells, which could result in enhanced responsiveness to IL-2 and increased proliferation of these cells. This raises the possibility that GzmB in Treg cells is responsible for down regulation of CD25 expression in target CD8+ T cells, thereby allowing for selective down modulation of their responsiveness to IL-2, which in turn is critical for their ability to produce IFN-γ and for their cytotoxic function51–52. Indeed, WT CD4+CD25+ Treg cells were shown to suppress CD25 expression and IFN-γ production in responding CD8+ T cells in co-culture studies53. How Treg cells inhibit CD25 expression is unclear. Inhibition of APC function or induction of apoptosis in APCs could limit the extent of CD8+ T cell activation and CD25 expression. Alternatively, GzmB delivered directly to CD8+ T cells could affect expression of CD25 independently from its proapoptotic function. This may explain the observation that Treg cells are able to inhibit lymphocyte responses in a Prf independent manner24. Further investigations are required to address these possibilities.
In summary, our findings identify a unique role for GzmB in regulating Ag-specific CD8+ T responses in the context of viral infection. They also suggest that this role is mediated, in part, by the Treg cell compartment.
Acknowledgments
We thank Drs. Michael Holtzman and Eugene Agapov for the kind gift of the SeV qPCR primers and probe.
This work was supported by the Children’s Hospital of Wisconsin Foundation and the NIH (N01A150032, K08AI072023) (to J.W.V.) and (R01HL087778) (to M.H.G.)
Footnotes
Disclosures
The authors have no financial conflict of interest.
Reference List
- 1.Lieberman J. The ABCs of granule-mediated cytotoxicity: new weapons in the arsenal. Nat Rev Immunol. 2003;3:361–370. doi: 10.1038/nri1083. [DOI] [PubMed] [Google Scholar]
- 2.Trapani JA, Smyth MJ. Functional significance of the perforin/granzyme cell death pathway. Nat Rev Immunol. 2002;2:735–747. doi: 10.1038/nri911. [DOI] [PubMed] [Google Scholar]
- 3.Kagi D, Ledermann B, Burki K, Seiler P, Odermatt B, Olsen KJ, Podack ER, Zinkernagel RM, Hengartner H. Cytotoxicity mediated by T cells and natural killer cells is greatly impaired in perforin-deficient mice. Nature. 1994;369:31–37. doi: 10.1038/369031a0. [DOI] [PubMed] [Google Scholar]
- 4.Zelinskyy G, Balkow S, Schimmer S, Schepers K, Simon MM, Dittmer U. Independent roles of perforin, granzymes, and Fas in the control of Friend retrovirus infection. Virology. 2004;330:365–374. doi: 10.1016/j.virol.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 5.Simon MM, Hausmann M, Tran T, Ebnet K, Tschopp J, ThaHla R, Mullbacher A. In vitro- and ex vivo-derived cytolytic leukocytes from granzyme A x B double knockout mice are defective in granule-mediated apoptosis but not lysis of target cells. J Exp Med. 1997;186:1781–1786. doi: 10.1084/jem.186.10.1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebnet K, Hausmann M, Lehmann-Grube F, Mullbacher A, Kopf M, Lamers M, Simon MM. Granzyme A-deficient mice retain potent cell-mediated cytotoxicity. EMBO J. 1995;14:4230–4239. doi: 10.1002/j.1460-2075.1995.tb00097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zajac AJ, Dye JM, Quinn DG. Control of lymphocytic choriomeningitis virus infection in granzyme B deficient mice. Virology. 2003;305:1–9. doi: 10.1006/viro.2002.1754. [DOI] [PubMed] [Google Scholar]
- 8.Loh J, Thomas DA, Revell PA, Ley TJ, Virgin HW. Granzymes and caspase 3 play important roles in control of gammaherpesvirus latency. J Virol. 2004;78:12519–12528. doi: 10.1128/JVI.78.22.12519-12528.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Dommelen SL, Sumaria N, Schreiber RD, Scalzo AA, Smyth MJ, Degli-Esposti MA. Perforin and granzymes have distinct roles in defensive immunity and immunopathology. Immunity. 2006;25:835–848. doi: 10.1016/j.immuni.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Filipovich AH. Hemophagocytic lymphohistiocytosis and related disorders. Curr Opin Allergy Clin Immunol. 2006;6:410–415. doi: 10.1097/01.all.0000246626.57118.d9. [DOI] [PubMed] [Google Scholar]
- 11.Stepp SE, Dufourcq-Lagelouse R, Le Deist F, Bhawan S, Certain S, Mathew PA, Henter JI, Bennett M, Fischer A, Saint Basile G, Kumar V. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science. 1999;286:1957–1959. doi: 10.1126/science.286.5446.1957. [DOI] [PubMed] [Google Scholar]
- 12.Verbsky JW, Grossman WJ. Hemophagocytic lymphohistiocytosis: diagnosis, pathophysiology, treatment, and future perspectives. Ann Med. 2006;38:20–31. doi: 10.1080/07853890500465189. [DOI] [PubMed] [Google Scholar]
- 13.Badovinac VP, Hamilton SE, Harty JT. Viral infection results in massive CD8+ T cell expansion and mortality in vaccinated perforin-deficient mice. Immunity. 2003;18:463–474. doi: 10.1016/s1074-7613(03)00079-7. [DOI] [PubMed] [Google Scholar]
- 14.Belkaid Y, Piccirillo CA, Mendez S, Shevach EM, Sacks DL. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature. 2002;420:502–507. doi: 10.1038/nature01152. [DOI] [PubMed] [Google Scholar]
- 15.Cao X, Cai SF, Fehniger TA, Song J, Collins LI, Piwnica-Worms DR, Ley TJ. Granzyme B and perforin are important for regulatory T cell-mediated suppression of tumor clearance. Immunity. 2007;27:635–646. doi: 10.1016/j.immuni.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Haribhai D, Lin W, Relland LM, Truong N, Williams CB, Chatila TA. Regulatory T cells dynamically control the primary immune response to foreign antigen. J Immunol. 2007;178:2961–2972. doi: 10.4049/jimmunol.178.5.2961. [DOI] [PubMed] [Google Scholar]
- 17.Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 18.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 19.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. doi: 10.1126/science.1079490. [DOI] [PubMed] [Google Scholar]
- 20.Thornton AM, Shevach EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grossman WJ, Verbsky JW, Barchet W, Colonna M, Atkinson JP, Ley TJ. Human T regulatory cells can use the perforin pathway to cause autologous target cell death. Immunity. 2004;21:589–601. doi: 10.1016/j.immuni.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Shevach EM. Mechanisms of foxp3+ T regulatory cell-mediated suppression. Immunity. 2009;30:636–645. doi: 10.1016/j.immuni.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 23.von Boehmer H. Mechanisms of suppression by suppressor T cells. Nat Immunol. 2005;6:338–344. doi: 10.1038/ni1180. [DOI] [PubMed] [Google Scholar]
- 24.Gondek DC, Lu LF, Quezada SA, Sakaguchi S, Noelle RJ. Cutting edge: contact-mediated suppression by CD4+CD25+ regulatory cells involves a granzyme B-dependent, perforin-independent mechanism. J Immunol. 2005;174:1783–1786. doi: 10.4049/jimmunol.174.4.1783. [DOI] [PubMed] [Google Scholar]
- 25.Zhao DM, Thornton AM, DiPaolo RJ, Shevach EM. Activated CD4+CD25+ T cells selectively kill B lymphocytes. Blood. 2006;107:3925–3932. doi: 10.1182/blood-2005-11-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips T, Opferman JT, Shah R, Liu N, Froelich CJ, Ashton-Rickardt PG. A role for the granzyme B inhibitor serine protease inhibitor 6 in CD8+ memory cell homeostasis. J Immunol. 2004;173:3801–3809. doi: 10.4049/jimmunol.173.6.3801. [DOI] [PubMed] [Google Scholar]
- 27.Sun J, Ooms L, Bird CH, Sutton VR, Trapani JA, Bird PI. A new family of 10 murine ovalbumin serpins includes two homologs of proteinase inhibitor 8 and two homologs of the granzyme B inhibitor (proteinase inhibitor 9) J Biol Chem. 1997;272:15434–15441. doi: 10.1074/jbc.272.24.15434. [DOI] [PubMed] [Google Scholar]
- 28.Zhang M, Park SM, Wang Y, Shah R, Liu N, Murmann AE, Wang CR, Peter ME, Ashton-Rickardt PG. Serine protease inhibitor 6 protects cytotoxic T cells from self-inflicted injury by ensuring the integrity of cytotoxic granules. Immunity. 2006;24:451–461. doi: 10.1016/j.immuni.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Gondek DC, Devries V, Nowak EC, Lu LF, Bennett KA, Scott ZA, Noelle RJ. Transplantation survival is maintained by granzyme B+ regulatory cells and adaptive regulatory T cells. J Immunol. 2008;181:4752–4760. doi: 10.4049/jimmunol.181.7.4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faisca P, Desmecht D. Sendai virus, the mouse parainfluenza type 1: a longstanding pathogen that remains up-to-date. Res Vet Sci. 2007;82:115–125. doi: 10.1016/j.rvsc.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 31.Tashiro M, Yokogoshi Y, Tobita K, Seto JT, Rott R, Kido H. Tryptase Clara, an activating protease for Sendai virus in rat lungs, is involved in pneumopathogenicity. J Virol. 1992;66:7211–7216. doi: 10.1128/jvi.66.12.7211-7216.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walter MJ, Morton JD, Kajiwara N, Agapov E, Holtzman MJ. Viral induction of a chronic asthma phenotype and genetic segregation from the acute response. J Clin Invest. 2002;110:165–175. doi: 10.1172/JCI14345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iwai H, Machii K, Otsuka Y, Ueda K. T cells subsets responsible for clearance of Sendai virus from infected mouse lungs. Microbiol Immunol. 1988;32:305–315. doi: 10.1111/j.1348-0421.1988.tb01390.x. [DOI] [PubMed] [Google Scholar]
- 34.Iwai H, Yamamoto S, Otsuka Y, Ueda K. Cooperation between humoral factor(s) and Lyt-2+ T cells in effective clearance of Sendai virus from infected mouse lungs. Microbiol Immunol. 1989;33:915–927. doi: 10.1111/j.1348-0421.1989.tb00979.x. [DOI] [PubMed] [Google Scholar]
- 35.Cole GA, Hogg TL, Woodland DL. The MHC class I-restricted T cell response to Sendai virus infection in C57BL/6 mice: a single immunodominant epitope elicits an extremely diverse repertoire of T cells. Int Immunol. 1994;6:1767–1775. doi: 10.1093/intimm/6.11.1767. [DOI] [PubMed] [Google Scholar]
- 36.Cole GA, Hogg TL, Coppola MA, Woodland DL. Efficient priming of CD8+ memory T cells specific for a subdominant epitope following Sendai virus infection. J Immunol. 1997;158:4301–4309. [PubMed] [Google Scholar]
- 37.Hou S, Doherty PC, Zijlstra M, Jaenisch R, Katz JM. Delayed clearance of Sendai virus in mice lacking class I MHC-restricted CD8+ T cells. J Immunol. 1992;149:1319–1325. [PubMed] [Google Scholar]
- 38.Kast WM, Roux L, Curren J, Blom HJ, Voordouw AC, Meloen RH, Kolakofsky D, Melief CJ. Protection against lethal Sendai virus infection by in vivo priming of virus-specific cytotoxic T lymphocytes with a free synthetic peptide. Proc Natl Acad Sci U S A. 1991;88:2283–2287. doi: 10.1073/pnas.88.6.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Revell PA, Grossman WJ, Thomas DA, Cao X, Behl R, Ratner JA, Lu ZH, Ley TJ. Granzyme B and the downstream granzymes C and/or F are important for cytotoxic lymphocyte functions. J Immunol. 2005;174:2124–2131. doi: 10.4049/jimmunol.174.4.2124. [DOI] [PubMed] [Google Scholar]
- 40.Kim EY, Battaile JT, Patel AC, You Y, Agapov E, Grayson MH, Benoit LA, Byers DE, Alevy Y, Tucker J, Swanson S, Tidwell R, Tyner JW, Morton JD, Castro M, Polineni D, Patterson GA, Schwendener RA, Allard JD, Peltz G, Holtzman MJ. Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat Med. 2008;14:633–640. doi: 10.1038/nm1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kohm AP, McMahon JS, Podojil JR, Begolka WS, DeGutes M, Kasprowicz DJ, Ziegler SF, Miller SD. Cutting Edge: Anti-CD25 monoclonal antibody injection results in the functional inactivation, not depletion, of CD4+CD25+ T regulatory cells. J Immunol. 2006;176:3301–3305. doi: 10.4049/jimmunol.176.6.3301. [DOI] [PubMed] [Google Scholar]
- 42.Onizuka S, Tawara I, Shimizu J, Sakaguchi S, Fujita T, Nakayama E. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor alpha) monoclonal antibody. Cancer Res. 1999;59:3128–3133. [PubMed] [Google Scholar]
- 43.Usherwood EJ, Hogan RJ, Crowther G, Surman SL, Hogg TL, Altman JD, Woodland DL. Functionally heterogeneous CD8(+) T-cell memory is induced by Sendai virus infection of mice. J Virol. 1999;73:7278–7286. doi: 10.1128/jvi.73.9.7278-7286.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aung S, Rutigliano JA, Graham BS. Alternative mechanisms of respiratory syncytial virus clearance in perforin knockout mice lead to enhanced disease. J Virol. 2001;75:9918–9924. doi: 10.1128/JVI.75.20.9918-9924.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matloubian M, Suresh M, Glass A, Galvan M, Chow K, Whitmire JK, Walsh CM, Clark WR, Ahmed R. A role for perforin in downregulating T-cell responses during chronic viral infection. J Virol. 1999;73:2527–2536. doi: 10.1128/jvi.73.3.2527-2536.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bem RA, van Woensel JB, Lutter R, Domachowske JB, Medema JP, Rosenberg HF, Bos AP. Granzyme A- and B-cluster deficiency delays acute lung injury in pneumovirus-infected mice. J Immunol. 184:931–938. doi: 10.4049/jimmunol.0903029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boissonnas A, Scholer-Dahirel A, Simon-Blancal V, Pace L, Valet F, Kissenpfennig A, Sparwasser T, Malissen B, Fetler L, Amigorena S. Foxp3+ T cells induce perforin-dependent dendritic cell death in tumor-draining lymph nodes. Immunity. 32:266–278. doi: 10.1016/j.immuni.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 48.Dittmer U, He H, Messer RJ, Schimmer S, Olbrich AR, Ohlen C, Greenberg PD, Stromnes IM, Iwashiro M, Sakaguchi S, Evans LH, Peterson KE, Yang G, Hasenkrug KJ. Functional impairment of CD8(+) T cells by regulatory T cells during persistent retroviral infection. Immunity. 2004;20:293–303. doi: 10.1016/s1074-7613(04)00054-8. [DOI] [PubMed] [Google Scholar]
- 49.Rouse BT, Sarangi PP, Suvas S. Regulatory T cells in virus infections. Immunol Rev. 2006;212:272–286. doi: 10.1111/j.0105-2896.2006.00412.x. [DOI] [PubMed] [Google Scholar]
- 50.Suvas S, Kumaraguru U, Pack CD, Lee S, Rouse BT. CD4+CD25+ T cells regulate virus-specific primary and memory CD8+ T cell responses. J Exp Med. 2003;198:889–901. doi: 10.1084/jem.20030171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mosmann TR, Sad S, Krishnan L, Wegmann TG, Guilbert LJ, Belosevic M. Differentiation of subsets of CD4+ and CD8+ T cells. Ciba Found Symp. 1995;195:42–50. doi: 10.1002/9780470514849.ch4. [DOI] [PubMed] [Google Scholar]
- 52.Sad S, Krishnan L. Cytokine deprivation of naive CD8+ T cells promotes minimal cell cycling but maximal cytokine synthesis and autonomous proliferation subsequently: a mechanism of self-regulation. J Immunol. 1999;163:2443–2451. [PubMed] [Google Scholar]
- 53.Piccirillo CA, Shevach EM. Cutting edge: control of CD8+ T cell activation by CD4+CD25+ immunoregulatory cells. J Immunol. 2001;167:1137–1140. doi: 10.4049/jimmunol.167.3.1137. [DOI] [PubMed] [Google Scholar]