Abstract
Background
School personnel in contact with students with life-threatening allergies often lack necessary supports, creating a potentially dangerous situation. Sabrina’s Law, the first legislation in the world designed to protect such children, requires all Ontario public schools to have a plan to protect children at risk. Though it has captured international attention, the differences a legislative approach makes have not been identified. Our study compared the approaches to anaphylaxis prevention and management in schools with and without legislation.
Methods
Legislated (Ontario) and non-legislated (Alberta, British Columbia, Newfoundland and Labrador, and Quebec) environments were compared. School board anaphylaxis policies were assessed for consistency with Canadian anaphylaxis guidelines. Parents of at-risk children and school personnel were surveyed to determine their perspectives on school practices. School personnel’s EpiPen technique was assessed.
Results
Consistency of school board policies with anaphylaxis guidelines was significantly better in a legislated environment (p=0.009). Parents in a legislated environment reported more comprehensive anaphylaxis emergency forms (p< 0.001), while school personnel in non-legislated environments reported more comprehensive forms (p=0.004). Despite school personnel in both environments receiving EpiPen training (>80%), suboptimal technique was commonly observed. However, school personnel in the legislated environment had better technique (p < 0.001).
Conclusion
Our results suggest that school boards in legislated environments have made greater efforts to support students at-risk for anaphylaxis compared to non-legislated environments. However, significant gaps exist in both environments, especially with respect to EpiPen administration, content and distribution of anaphylaxis emergency forms, and awareness of school procedures by school personnel and parents.
Keywords: Anaphylaxis, life-threatening allergies, policy, Sabrina’s Law, school
Introduction
Anaphylaxis is a severe, potentially fatal, systemic allergic reaction that can occur suddenly after contact with an allergy-causing substance. Prevention is only achieved through allergen avoidance (1–2). Complete avoidance is difficult as causative anaphylactic agents include common foods and stinging insects (3). Allergen exposure is common in school settings with approximately 18% of food allergic reactions occurring at school (4) in a context of increasing food allergy prevalence (5). Schools have a legal obligation to protect the welfare of students while at school; therefore, they are obliged to support students at risk of anaphylaxis through allergen avoidance and management of reactions (4–8). However, school personnel often lack the knowledge and skills necessary to recognize and treat anaphylactic reactions (9–13).
To address the need for protecting students at risk, anaphylaxis guidelines exist in many countries, including Australia, Canada and the United States (3, 14–16). In response to the death of 13-year-old Sabrina Shannon due to an anaphylactic reaction at school, Sabrina’s Law (“An Act to Protect Anaphylactic Pupils”) was enacted in the province of Ontario, Canada. Effective January 1, 2006, Sabrina’s Law requires Ontario public school boards to establish an anaphylaxis policy that includes reducing allergen exposure, providing regular anaphylaxis management training for school personnel, and establishing individual anaphylaxis emergency management plans (16). In addition, Sabrina’s Law permits the use of epinephrine for anaphylaxis in previously undiagnosed students and grants legal immunity for “good Samaritans” administering epinephrine in good faith. As the first of its kind in the world, Sabrina’s Law captured the attention of parents/guardians of children with life-threatening allergies as well as school boards and government bodies questioning the need for similar legislation. Following the legislative precedent, other jurisdictions in Canada, the United States and Australia have enacted legislation related to anaphylaxis in schools. However, the benefits of a legislative approach are yet to be determined. Therefore, the aim of this study was to examine approaches to anaphylaxis management in schools with legislation and without legislation, comparing school board anaphylaxis policies, perceptions of parents and school personnel regarding school anaphylaxis management practices, and EpiPen technique of school personnel.
Methods
The study involved five Canadian provinces: Ontario (legislated environment) and Alberta, British Columbia, Newfoundland and Labrador, and Quebec (non-legislated environments). To achieve the study aim, a multifaceted approach was used: i) determining the consistency of school board policies with guidelines for preventing and managing anaphylaxis in schools (17), ii) surveying parents/guardians of children at risk for anaphylaxis, iii) surveying school personnel about their school environments, and iv) assessing school personnel’s EpiPen technique. Before initiating the study, ethics approval was obtained from participating universities and school boards. Participants were unaware of the study’s intent to identify the impact of Sabrina’s Law.
Assessment of School Boards’ Anaphylaxis Policies
A standardized checklist was developed based on the Canadian Society of Allergy and Clinical Immunology’s guidelines for managing anaphylaxis at schools to determine school board policy consistency with guidelines (17). The checklist consisted of 13 items. (Refer to online supplement) For each school board policy, two independent assessors determined whether or not the policy had each of the 13 items, out of a possible maximum score of 13. Assessors were in agreement for 98% of the 13 items. Items characterized by disagreement were handled by consensus and review by a third assessor. Using a random number generator, 150 public school boards were selected for retrieval of school board anaphylaxis-related policies. In the case of Quebec, none of the randomly selected school boards had anaphylaxis-related policies in English or French; therefore, an attempt was made to retrieve written board policies for all school boards. Follow-up with the Quebec school boards suggests that a possible explanation for the lack of policies was that school boards thought this was a responsibility of public health.
Electronic Survey of Parents of Children at Risk for Anaphylaxis
An electronic survey was conducted with members of Anaphylaxis Canada’s Registry. From the five provinces, 4,103 members were sent an electronic message inviting them to complete the survey about their at-risk child and family’s experiences at school (K-12). The electronic survey elicited information about child and school characteristics, the child’s school anaphylaxis policy, the school’s anaphylaxis emergency plan and administration of epinephrine, and parental perceptions of the supportiveness of their child’s school.
Public School Personnel Survey and EpiPen Technique
To determine school personnel’s perceptions of anaphylaxis prevention and management practices at school, a questionnaire comparable to the parental questionnaire was developed and pilot-tested (refer to online supplement). From 12 randomly selected public school boards, 112 randomly selected schools (K-12) participated in the survey. Schools were sent study packages containing a study information sheet, the questionnaire, a postage-paid self-addressed envelope, and a two-dollar beverage/food card. The head school administrative assistant distributed study packages to teachers, school administrators, administrative assistants and school personnel in regular contact with students. Completion of the survey by school personnel was voluntary, confidential and anonymous.
In order to assess school personnel’s EpiPen technique, a four-item assessment and scoring tool was developed. In each province, trained assessors evaluated school personnel’s technique. Prior to data collection, a standard training video was developed demonstrating examples of accurate and inaccurate techniques. Assessors were required to assess and score the video cases. Assessors were in agreement for 96% of the cases.
Statistics
Descriptive statistics were performed for all variables as an aggregate and according to the two study groups - legislated and non-legislated environments. For categorical data, chi-square tests were performed to determine if differences existed between legislated and non-legislated environments. For scores regarding EpiPen technique and comprehensiveness of school emergency management forms, both parametric (unpaired t-test) and non-parametric (Wilcoxon Rank Sum test) tests were used to determine if statistically significant differences existed. Because parametric and non-parametric tests revealed equal p-values, the means and results of the parametric tests are presented. Using two-tailed tests of significance, p-values of less than 0.05 were considered statistically significant.
Results
Assessment of School Boards’ Anaphylaxis Policies
Retrieval and assessment of 76 school board policies, with equal numbers from legislated and non-legislated environments, occurred to determine the consistency of policies with the Canadian Guidelines for Preventing and Managing Anaphylaxis at Schools. Quebec was an outlier in that only three school boards had a policy that could be assessed despite attempting to retrieve policies for all public school boards. Excluding Quebec, school board policies were retrieved for 93% of the randomly selected school boards.
In general, anaphylaxis-related school board policies in the legislated environment demonstrated greater consistency with the Canadian anaphylaxis guidelines (15,17) compared to non-legislated environments. School board policies from the legislated environment had an average score of 8.8 (S.D. 4.4) versus 6.1 (S.D. 4.4; p = 0.009), out of a possible score of 0–13, in non-legislated environments. Policies in a legislated environment were more likely to include clauses related to reducing allergen exposure (78.9% vs. 42.1%), providing regular employee training related to life-threatening allergies (84.2% vs. 63.1%), and requiring completion of individual plans for at-risk students (73.7% vs. 44.7%)(Figure 1). Additionally, they had more specific mandated elements regarding individualized emergency management plans, such as details about the student’s allergen(s), treatment, and epinephrine auto-injector storage.
Figure 1.
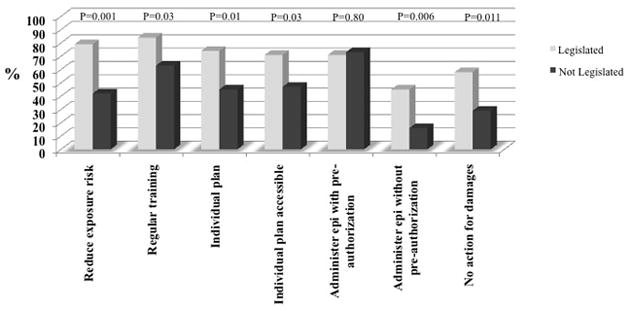
School Board Policy Consistency with Canadian Guidelines for Preventing and Managing Anaphylaxis at Schools
Over 70% of all school board policies in both environments contained a clause stating that employees may be preauthorized to administer medication or supervise a student taking medication in response to an anaphylactic reaction, if the school has both up-to-date treatment information and the consent of the parent/guardian and pupil (if age appropriate). However, two important areas addressed in the Canadian guidelines (15, 17) and Sabrina’s Law were commonly missing from school board policies in both environments: 1) A clause that would allow an employee to administer medication to a student if the employee believes the student is experiencing an anaphylactic reaction, even if there is no preauthorization from the parent. This would allow for treatment of a first life-threatening allergic reaction; and 2) A statement that no action for damages would occur for any action done in good faith in response to an anaphylactic reaction (Figure 1).
Survey of Parents of Children at Risk for Anaphylaxis
Online survey participants numbered 1,365 (33% response rate): 801 (58%) represented the legislated environment and 564 (42%) represented non-legislated environments. Most participants had children attending elementary schools (>70%) of 200–500 students. About 95% of parents reported that their children (average age 8–9 years) had life-threatening food allergies, most commonly peanut and tree nut allergies. See Figure 2.
Figure 2.
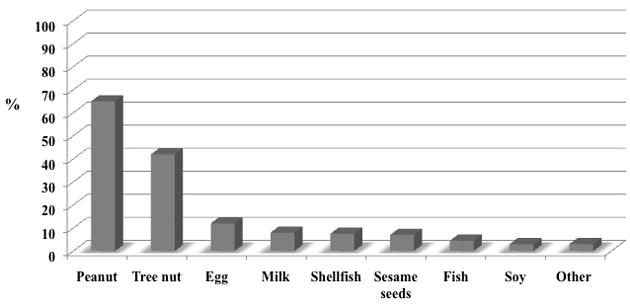
Parental Reports of Student Food Allergy
In general, more parents living in a legislated environment reported that their children’s schools had practices demonstrating support towards their allergic children. Parents in a legislated environment reported that their schools were more likely to have written policies for preventing and managing anaphylaxis (62% vs. 44%; p = 0.002). Although most parents in both legislated (88.3%) and non-legislated (73.3%) environments reported a school requirement to complete anaphylaxis emergency forms, parents in the legislated environment reported completing more comprehensive forms. Parents in a legislated environment reported, on average, that their emergency forms had 3.0 (SD ± 1.3) versus 2.4 (SD ± 1.5; p < 0.001) of the four key elements. Parents in a legislated environment were also more likely to report that their children’s school personnel received epinephrine autoinjector training. Parents in both environments were more likely to report that a lack of awareness and training in schools had put their child at risk, than to report that training and awareness in school helped their child. However, parents in a non-legislated environment were more likely to report that a lack of awareness and training in the schools had placed their child at risk compared to parents in the legislated environment (42.6% vs 35.5%; P=0.02). See Table 1.
Table 1.
Parental Reports of their Children’s School Environments Regarding Prevention and Management of Anaphylaxis
| Legislated (n=801) | Non- Legislated (n=564) | P-value | |
|---|---|---|---|
| School board has written policy for managing and limiting life-threatening allergies | 61.6% | 44.0% | 0.001 |
|
| |||
| Asked to complete an emergency management plan | 88.3% | 73.3% | < 0.001 |
|
| |||
| Emergency Management Form Comprehensiveness | (n=707) | (n=436) | |
| Mean score (theoretical score range: 0 – 4) | |||
| Frequency of elements on emergency form: | 3.0 ± 1.3 | 2.3 ± 1.5 | < 0.001 |
| • List of child’s allergies | 75.9% | 65.3% | |
| • Location of auto-injector | 51.8% | 38.6% | |
| • Emergency protocol | 62.3% | 52.4% | |
| • Photo of child | 66.0% | 44.7% | |
|
| |||
| Staff trained to administer epinephrine auto-injector | 71.7% | 62.7% | 0.003 |
|
| |||
| A lack of school awareness and training related to allergies placed my child at risk | 35.5% | 42.6% | 0.02 |
|
| |||
| School awareness and training related to allergies helped my child | 27.3% | 27.3% | NS |
Public School Personnel Survey and EpiPen Technique
From the 112 randomly selected schools, 1,563 (70% response rate) school personnel completed questionnaires. For the EpiPen technique assessment, 857 (61% response rate) school personnel participated. Most participants (96%) were teachers with the remainder being principals, vice principals, and administrative assistants.
Although fairly low percentages of school personnel in both environments reported that their schools had written anaphylaxis-related policies, the difference between legislated (54.6%) and non-legislated (47.1%) environments reached statistical significance (p=0.003). Comparable rates of school personnel in both environments reported that parents were required to submit an emergency management form. However, unlike the parental survey, more school personnel in non-legislated environments reported that their schools’ emergency forms were more comprehensive. School personnel in the legislated environment reported that their schools’ plans had, on average, 1.9 compared to 2.2 of the four key elements in non-legislated environments (p=0.04). The majority of personnel from both environments (60%) reported that their schools’ forms were missing one or more elements and most frequently cited the location of the epinephrine auto-injector and the necessary steps for treating a reaction as the missing elements. Over 80% of school personnel in both environments reported receiving previous epinephrine auto-injector training. However, out of a possible score of 0 to 4, those in the legislated environment were more likely to demonstrate accurate EpiPen technique, with 39% scoring a 4, compared to 26% (p<0.002) of school personnel in non-legislated environments. Overall school personnel, regardless of environment, did not report that a lack of awareness or training placed a student at-risk or that training and awareness helped a student with allergies during the last year. See Table 2.
Table 2.
School Personnel Reports of School Environments Regarding Prevention and Management of Anaphylaxis
| Legislated (n = 710) | Non-Legislated (n = 853) | P-value | |
|---|---|---|---|
| School has written policy for prevention and management of anaphylaxis | 54.6% | 47.1% | 0.003 |
|
| |||
| Parents required to complete emergency management form for child | 57.3% | 57.1% | 0.967 |
|
| |||
| Emergency Management Form Comprehensiveness | (n=407) | (n=487) | |
| Mean score (theoretical score range: 0 – 4) | 1.9 ± 1.8 | 2.2 ± 1.8 | 0.04 |
| Frequency of elements on emergency form: | |||
| • List of child’s allergies | 53.6% | 61.2% | |
| • Location of auto-injector | 43.7% | 49.3% | |
| • Emergency protocol | 45.0% | 52.0% | |
| • Photo of child | 47.3% | 55.6% | |
|
| |||
| Provided with personal copy of emergency form | 38.2% | 43.4% | 0.05 |
|
| |||
| Trained to administer EpiPen | 95.1% | 81.1% | < 0.001 |
|
| |||
| EpiPen Technique | (n = 418) | (n = 439) | |
| Mean score (theoretical score range: 0 – 4) | 3.0 ± 1.2 | 2.5 ± 1.2 | < 0.001 |
|
| |||
| A lack of school awareness and training related to allergies placed a student at risk | 0.70% | 1.1% | 0.28 |
|
| |||
| School awareness and training related to allergies helped a student during a reaction | 10.9% | 9.6% | 0.07 |
Discussion
Australia, Canada and the United States all have legislation in an attempt to protect students at-risk of life threatening allergies while at school. Our study is the first to explore the impact and experiences of legislated environments compared to non-legislated environments. Results of the school board policy assessments, parental and school personnel surveys, and school personnel EpiPen technique assessments suggest that, in general, a legislated environment is characterized by a greater number of supportive indicators than a non-legislated environment. These indicators include the existence of school board policies consistent with practice guidelines (17), higher proportions of school personnel provided with EpiPen training and school personnel with better EpiPen technique. However, numerous indicators fail to appear in a legislated environment despite Sabrina’s Law being in effect. School board policies in a legislated environment were equally deficient in two areas mandated by Sabrina’s Law; namely, permitting emergency epinephrine administration to those without prior consent and granting immunity from legal action for damages resulting from actions taken in good faith in response to an anaphylactic reaction.
Analysis of responses from the three targets - school board policies, school personnel, and parents of children with life-threatening allergies - reveals several noteworthy trends and inconsistencies. Data from all three sources consistently indicated that a legislated environment was more likely to have written school board policies for the prevention and management of anaphylaxis. However, parents and school personnel were often unaware of existing school board policies in both environments. Over 90% of Ontario school boards had written policies that could be easily retrieved from their websites, yet only slightly more than half of parents and school personnel knew of their existence. Strategies for improving the awareness of and familiarity with the content of existing school board policies are needed for school personnel and families.
The availability of completed comprehensive individualized emergency management plans is an important element in creating supportive and safe school environments for children at risk for anaphylaxis and was more frequently required in a legislated environment. A noteworthy observation was that most parents (>78%), regardless of study environment, reported completing emergency management plans for school yet only about 40% of school personnel reported having personal copies. Previous research also highlights the observed gap in school personnel possession of individualized emergency management plans (9–11). Omissions commonly reported in the emergency management form by parents and school personnel were the location of the epinephrine auto-injector and treatment steps. The lack of key information on emergency management forms is consistent with an earlier study noting emergency plans often lack a description of treatment steps and location of emergency medicine (18).
In both environments, an interesting but somewhat expected discrepancy was noted between school personnel’s reported receipt of EpiPen training and the accuracy of their technique. According to the policy assessment and parental and school personnel survey study elements, over 80% of school personnel receive regular epinephrine autoinjector training. However, assessment of their EpiPen technique revealed suboptimal performance (> 35% had perfect technique), supporting the results of previous studies (9, 11–13, 19). In an earlier study (19), comparable accuracy rates were reported for school personnel that had not received training. This suggests that even with training, some school personnel are unable to correctly administer epinephrine.
Some limitations to this study should be noted. Participation rates from parents, schools and school personnel while not ideal, were comparable to or better than participation rates observed in similar studies (20–23). For the EpiPen technique assessment, it is possible that those most knowledgeable volunteered to participate, thus generating falsely high scores. However, our results still indicate suboptimal technique; therefore, it is likely that a higher response rate would reveal even poorer EpiPen technique. A second limitation is that participating parents may not have been from schools that were randomly selected to participate. The sampling framework for the parental survey did not include geographical information that would permit sampling according to participating schools. However, the majority of participating school personnel and parents were from the same participating school boards. A third limitation inherent to cross-sectional studies is the potential for recall bias, which may have occurred for parents and school personnel.
This study has important implications for policy development and implementation. A gap identified by our study indicates that school personnel and parents are likely not aware of or knowledgeable about their own school boards’ written policies for the prevention and management of anaphylaxis. This highlights deficiencies in training, communication and ineffective policy implementation for schools. It also has important implications for legislators and policy-makers to implement measures for enforcing policy. Our observations suggest that despite a legal mandate, laws without proper resources for implementation and/or “legal teeth” fail to produce the desired improvements. The province of Ontario does not have a body responsible for monitoring consistency with or enforcing Sabrina’s Law.
Our study is novel and innovative as it is the first to examine, and compare and contrast legislated and non-legislated environments for the prevention and management of anaphylaxis in school settings from the perspectives of written school board policies, school personnel, and parents of children at-risk for anaphylaxis. While legislated environments have made efforts to create a supportive school environment for students with life-threatening allergies, they fall short on the actual implementation of their policies. School personnel do not have many of the necessary supports to respond effectively in the case of an allergic reaction, for instance a personal copy of the student’s emergency management form. Allergists and other health care providers can play an important role by informing families of students at-risk of an anaphylactic reaction to review their school board policies. Our study suggests that the implementation of policies for students at-risk for anaphylaxis whether legislated or not, requires involvement from all parties involved to ensure the safety of these children when at school.
Supplementary Material
Acknowledgments
Funding : AllerGen NCE Inc., the Allergy, Genes and Environment Network, a member of the Networks for Centres of Excellence Canada Program. Support for students provided by: the Universities of Toronto (Julien) and McMaster University, the Canadian Institutes of Health Research National Training Program in Allergy and Asthma Research, the Ross Fellowship from the Montreal Children’s Hospital (Nguyen-Luu), and the GEMS Program funded by the National Heart, Lung and Blood Institute Training Grant #1R25HL103286-01 (Li). Dr. Clarke is a National Research Scholar of the Fonds de la recherché en santé de Quebec.
The project team would like to thank all of the school boards, school personnel, and parents and guardians that participated in the project and assisted the team in understanding this very important area.
Abbreviations
- S.D
Standard Deviation
- SPSS
Statistical Package for Social Sciences
Footnotes
Author’s Contributions and Conflicts
Lisa Cicutto: Led the design, development of data collection tools, attained Research Ethics Board approvals, led data analysis and interpretation, and first and subsequent manuscript drafts.
No conflicts of interest to declare.
Brianna Julien: Coordinated the acquisition of data, assisted with data collection for Ontario, assisted with attaining Research Ethics Board approvals, participated in data entry, analysis and interpretation and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Nancy Y. Li: Assisted with data analysis and interpretation and assisted L. Cicutto in the first draft and subsequent manuscript drafts.
No conflicts of interest to declare.
Nha Uyen Nguyen-Luu: Provided feedback on study design and instruments, coordinated and participated in data collection, entry, analysis for Quebec and data interpretation, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Janice Butler: Provided feedback on study design and instruments, attained Research Ethics Board approvals, coordinated and participated in data collection for Newfoundland and Labrador, participated in data interpretation, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Ann Clarke: Provided feedback on study design, instruments, and data analysis plan, supervised the Quebec site, attained Research Ethics Board approvals, participated in data interpretation, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Susan J. Elliott: Provided feedback on study design, instruments, and data analysis plan, and participated in the interpretation of data and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Laurie Harada: Provided feedback on study design and instruments, coordinated the parental electronic survey, participated in the interpretation of data, and reviewed and provided feedback on manuscript drafts.
No personal conflicts of interest to declare. Her employer, Anaphylaxis Canada, has received unrestricted educational grants from King Pharmaceuticals and Paladin Labs.
Shawna McGhan: Provided feedback on study design and instruments, attained Research Ethics Board approvals, coordinated and participated in data collection for Alberta, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Donald Stark: Provided feedback on study design and instruments, attained Research Ethics Board approvals, coordinated and participated in data collection for British Columbia, participated in the interpretation of data, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Timothy K Vander Leek: Provided feedback on study design and instruments, supported the work at the Alberta site, participated in the interpretation of data, and reviewed and provided feedback on manuscript drafts.
No conflicts of interest to declare.
Susan Waserman: Provided feedback on study design, instruments, and data analysis plan, attained Research Ethics Board approval, coordinated and participated in data collection for Ontario, participated in the interpretation of data, and reviewed and provided feedback on manuscript drafts.
Susan has served on the Advisory Board of King Pharmaceuticals.
References
- 1.Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF, Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: Summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117:391–7. doi: 10.1016/j.jaci.2005.12.1303. [DOI] [PubMed] [Google Scholar]
- 2.Simons FER. Anaphylaxis. J Allergy Clin Immunol. 2010;125:S161–S181. doi: 10.1016/j.jaci.2009.12.981. [DOI] [PubMed] [Google Scholar]
- 3.AAAAI Board of Directors. Anaphylaxis in schools and other child-care settings. J Allergy Clin Immunol. 1998;102:173–6. [PubMed] [Google Scholar]
- 4.Young MC, Muñoz-Furlong A, Sicherer SH. Management of food allergies in schools: a perspective for allergists. J Allergy Clin Immunol. 2009;124:175–182. doi: 10.1016/j.jaci.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Branum AM, Lukacs SL. Food allergy among U.S. children: trends in prevalence and hospitalizations. NCHS Data Brief, No. 10. 2008 October; Available at: http://www.cdc.gov/nchs/data/databriefs/db10.pdf. [PubMed]
- 6.Behrmann J. Ethical principles as a guide in implementing policies for the management of food allergies in schools. J Sch Nurs. 2010;26:183–193. doi: 10.1177/1059840510364844. [DOI] [PubMed] [Google Scholar]
- 7.Houle CR, Leo HL, Clark NM. A developmental, community, and psychosocial approach to food allergies in children. Curr Allergy Asthma Rep. 2010 May 13; doi: 10.1007/s11882-010-0123-1. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 8.Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155:790–5. doi: 10.1001/archpedi.155.7.790. [DOI] [PubMed] [Google Scholar]
- 9.Kastner M, Harada L, Waserman S. Gaps in anaphylaxis management at the level of physicians, patients, and the community: a systematic review of the literature. Allergy. 2010;65:435–444. doi: 10.1111/j.1398-9995.2009.02294.x. [DOI] [PubMed] [Google Scholar]
- 10.Bansal PJ, Marsh R, Patel B, Tobin MC. Recognition, evaluation, and treatment of anaphylaxis in the child care setting. Ann Allergy Asthma Immunol. 2005;94:55–9. doi: 10.1016/S1081-1206(10)61286-0. [DOI] [PubMed] [Google Scholar]
- 11.Rhim GS, McMorris MS. School readiness for children with food allergies. Ann Allergy Asthma Immunol. 2001;86:172–6. doi: 10.1016/S1081-1206(10)62687-7. [DOI] [PubMed] [Google Scholar]
- 12.Clegg SK, Ritchie JM. “Epipen” training: a survey of the provision for parents and teachers in West Lothian. Ambul Child Health. 2001;7:169–175. [Google Scholar]
- 13.Frost DW, Chalin CG. The effect of income on anaphylaxis preparation and management plans in Toronto primary schools. Can J Public Health. 2005;96:250–3. doi: 10.1007/BF03405156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baumgart K, Brown S, Gold M, Kemp A, Loblay R, Loh R, et al. ASCIA guidelines for prevention of food anaphylactic reactions in schools, preschools and child-care centres. J Paediatr Child Health. 2004;40:669–671. doi: 10.1111/j.1440-1754.2004.00509.x. [DOI] [PubMed] [Google Scholar]
- 15.Allen M, Binkley K, Chad Z, Dufresne C, Fischer D, Gold M, et al. for Canadian Society of Allergy and Clinical Immunology. Anaphylaxis in Schools & Other Settings. Canadian Society of Allergy and Clinical Immunology. 2009 [Google Scholar]
- 16.Sabrina’s Law, 2005, S.O. 2005, c.7.
- 17.Allen M, Binkley K, Chad Z, Dufresne C, Fischer D, Gold M, et al. for Canadian Society of Allergy and Clinical Immunology. Anaphylaxis in Schools & Other Settings. Canadian Society of Allergy and Clinical Immunology. 2005 [Google Scholar]
- 18.Powers J, Bergren MD, Finnegan L. Comparison of school food allergy emergency plans to the Food Allergy and Anaphylaxis Network’s standard plan. J Sch Nurs. 2007;23:252–8. doi: 10.1177/10598405070230050301. [DOI] [PubMed] [Google Scholar]
- 19.Patel BM, Bansal PJ, Tobin MC. Management of anaphylaxis in child care centers: evaluation 6 and 12 months after an intervention program. Ann Allergy Asthma Immunol. 2006;97:813–5. doi: 10.1016/S1081-1206(10)60974-X. [DOI] [PubMed] [Google Scholar]
- 20.Rankin KE, Sheikh A. Serious shortcomings in the management of children with anaphylaxis in Scottish schools. PLoS Med. 2006;3:e326. doi: 10.1371/journal.pmed.0030326. Published online 2006 August 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watson W, Woodrow AM, Bruce A, Power A. Are teachers knowledgeable and confident about dealing with allergy emergencies? Allergy Asthma Clin Immunol. 2010;6(Suppl 1):10. [Google Scholar]
- 22.Wong I, Awolow T, Gordon K, Mo Y. Survey of administration of medicines to pupils in primary schools in the London area. Arch Dis Child. 2004;89:998–1001. doi: 10.1136/adc.2003.047258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pulcini JM, Sease KK, Marshall GD. Disparity between the presence and absence of food allergy action plans in one school district. Allergy Asthma Proc. 2010;31:141–146. doi: 10.2500/aap.2010.31.3315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


