Abstract
Aims
To describe some of the variability across the world in levels of quit smoking attempts and use of various forms of cessation support.
Design
Use of the International Tobacco Control Policy Evaluation Project surveys of smokers, using the 2007 survey wave (or later, where necessary).
Settings
Australia, Canada, China, France, Germany, Ireland, Malaysia, Mexico, Netherlands, New Zealand, South Korea, Thailand, UK, Uruguay and USA.
Measures
Self-report on use of cessation aids and on visits to health professionals and provision of cessation advice during the visits.
Findings
Prevalence of quit attempts in the last year varied from under 20% to over 50% across countries. Similarly, smokers varied greatly in reporting of visiting health professionals in the last year (< 20% to over 70%), and among those who did, provision of advice to quit also varied greatly. There was also marked variability in the levels and types of help reported. Use of medication was generally more common than use of behavioural support, except where medications are not readily available.
Conclusions
There is wide variation across countries in rates of attempts to stop smoking and use of assistance with higher overall use of medication than behavioural support. There is also wide variation in the provision of brief advice to stop by health professionals.
Introduction
The global community, through the World Health Organization's Framework Convention on Tobacco Control (FCTC), has agreed Guidelines for the implementation of Article 14 of the Convention, which deals with support for smoking cessation. Recent studies have shown that few countries have developed comprehensive support systems to help people to stop smoking (1, 2). Case studies of treatment systems indicate a variety of models in place, with the greatest challenges being faced by large, lower income countries (3). However, very little is known about quitting activity within countries, how this varies as a result of the availability of different treatment systems and how this might inform the development of treatment systems across different countries.
Before smokers consider using cessation aids, they need to be interested in quitting smoking. Health care services can only directly contribute to this interest when smokers use them, e.g., in consultations with health professionals. Advice from health care professionals can increase successful quitting (4), medications such as nicotine replacement therapy (NRT) and varenicline are effective (5, 6) and a range of support, ranging from automated personalized advice, through quitlines to face-to face programs, have also been shown to be effective (7, 8).
This paper reports comparative data on the prevalence of recent quitting activity and the extent to which health professionals are advising their clients/patients to quit smoking in 15 countries participating in the International Tobacco Control (ITC) policy evaluation surveys. We also examined those who have made recent quit attempts and report on levels of reported use of a variety of forms of help, both medication and non-medication. We expected levels of quitting activity to be a function of extent of public education and other tobacco control efforts in the country, and use of support to be a function both of these and of the availability and accessibility of support within a country.
The data are provided not to make fine-grained comparisons between countries, but to assess large-scale differences and to analyse their implications.
Methods
The data came from 15 countries, ranging from high to middle-income, that are surveying smokers as part of ITC policy evaluation project. The ITC surveys are longitudinal studies, (usually with replenishment), and in those countries a majority of those surveyed were existing members of the cohorts. We have chosen the survey wave closest to 2007 in each country that has the bulk of the relevant measures. Details of the individual studies can be found at www.itcproject.org
Sample size by country and other details are in Table 1. The survey data are weighted to the age and sex distribution of smokers in the relevant populations. As can be seen from Table 1, survey methods differed across countries. The sample sizes for the different surveys yield 95% CIs of approximately 4% for prevalence estimates around 20%, and 5% for prevalence estimates of approximately 50%. This data is not presented alongside the actual data so that the focus remains on the overall range of estimates across countries and not on detailed comparisons between countries. Methods were adopted to make the surveys as representative as possible for the populations sampled, and we have used weighting by survey weights to increase further the representativeness of the results. Face to face surveys used multi-level stratified sampling. Telephone surveys usually used random digit dialing, and the internet sample came from a large, broadly representative, panel.
Table 1. Characteristics of the samples of current smokers in the ITC Project countries.
| Country | Year of Survey | N | Mode | Sample | Survey wave |
|---|---|---|---|---|---|
| High Incomeˆ | |||||
| New Zealand | 2007 –2008 | 1376 | Phone | National | 1 |
| Australia | 2007–2008 | 1775 | Phone | National | 6 |
| Canada | 2007–2008 | 1697 | Phone | National | 6 |
| USA | 2007–2008 | 1723 | Phone | National | 6 |
| UK | 2007–2008 | 1657 | Phone | National | 6 |
| Ireland | 2006 | 582 | Phone | National | 3 |
| Netherlands | 2009 | 1637 | Phone & internet | National | 3 |
| Germany | 2009 | 912 | Phone | National | 2 |
| France | 2008 | 1540 | Phone | National | 2 |
| South Korea | 2008 | 1737 | Phone | National | 2 |
| Middle income | |||||
| Uruguay | 2006 | 885 | Face to face | Capital city | 1 |
| Mexico | 2007 | 941 | Face to face | 4 cities | 2 |
| China | 2007–2008 | 4623 | Face to face | 6 cities | 2 |
| Thailand | 2006 | 1874 | Face to face | National | 2 |
| Malaysia | 2006–2007 | 1564 | Face to face & phone | National | 2 |
Note: More details on the individual surveys are available from the ITC website: www.itcproject.org
Income status of countries is based on the latest World Bank classification. See http://data.worldbank.org/about/country-classifications/country-and-lending-groups
Because recruitment into the ITC surveys is only of current smokers, we have restricted the analyses to those who were currently smoking at the time of the target survey, for countries where the wave used was not the first wave. This mode of sampling underestimates quitting activity by the proportion of quit attempts that occurred in the period asked about, but were ongoing at the time of the survey. One implication is that the quit attempts under discussion have been unsuccessful and somewhat shorter on average.
Measures
Quit attempts in last year and ever
At the initial survey smokers were asked if they had ever tried to quit smoking and how recently their last attempt ended. For subsequent waves smokers were asked: “Have you made any attempts to quit smoking since we last talked to you in (with date inserted)?”, and if so, when. Only those reporting attempts in the last year were included as having made recent attempts.
Visits to health professionals and advice about quitting
Respondents were asked: “Have you visited a doctor or other health professional since last survey date?” (for recontacted smokers, or “in the last year” for newly recruited smokers). Those that had visited were further asked: “During any visit to the doctor or other health professional, since last survey date (or in the last year), did you receive advice to quit smoking?”
Use of medications
Smokers were asked “In the last year (Since <insert last survey date> have you used any stop-smoking medication?” And if so what, with nicotine replacement therapy (NRT) and prescription medications distinguished from other remedies. In countries where we had reason to believe that knowledge of stop smoking medications would be low the questioning was different. We first asked: “Have you heard about medications to help people stop smoking, including nicotine gum or patches, stop smoking pills, such as bupropion or herbal medications?” Only those who knew of such products were asked about use, the remainder were assumed not to have used.
Use of quitlines, internet and dedicated clinics
Respondents were asked: “In the last year (last survey date, or 6 months in some cases), have you received advice or information about quitting smoking from any of the following?” “Telephone or quitline services”; “The internet”; and “Local stop smoking services (such as clinics and specialists)”? Where the questions refer to different time intervals across countries, these are clearly indicated in the Results.
Use of specific aids among those reporting making quit attempts
Interest in quitting is one major factor determining demand for services and/or aids. To control in part for varying levels of interest in quitting across countries, we explore use of specific aids among those reporting having made a quit attempt in the relevant period. This excludes a small proportion of those who reported using a quit aid but failed to report a quit attempt.
Results
Quitting Activity
Recent quitting activity varied considerably by country (Figure 1). Reports of ever having tried to quit varied from around 60% in New Zealand, Mexico and China, to over 80% in most of the other countries. Less than 20% of smokers in China and Malaysia reported recent attempts to quit compared with around 50% among smokers in Thailand. There was no clear relationship between the two measures; for example, New Zealand had low ever-quit rates but high recent quitting; Germany, had high ever-quit rates, but low levels of recent activity.
Figure 1.
Reported history of quit attempts by country. Note: The total height of the bars refers to ever quit and the bottom part to those where there was an attempt in the last year. 95% confidence intervals (of the total height) are presented on the top of the bars.
Health Professional Advice
To ascertain the potential for health care consultations to be an important locus for providing advice and motivation to quit smoking, we asked about visits to doctors or other health professionals for any reason. The level of such visits varied enormously from 50-70% in most of the developed countries, to less than 20% in Malaysia (Figure 2). The likelihood of reporting getting advice to quit when they visited also varied markedly (Figure 2). In some countries, including the USA, Thailand and Malaysia, over two thirds of those visiting a health professional reported getting advice, while in others, most notably The Netherlands, it was a clear minority, around 20%. This translates into overall advice to quit from health professionals ranging from less than 10% in The Netherlands to over 50% in the USA.
Figure 2.
Reported visits to doctors or other healthcare professionals and of advice to quit on any such visit by country. Interval is last year (or between waves), except where indicated with an asterisk *, where it is 6 months. 95% confidence intervals (of the total height) are presented on the top of the bars.
Use of Cessation Supports
Reported use of cessation support was restricted to those who reported making quit attempts, as this is the main factor determining use. Figure 3 shows much higher use of quit smoking medications among those who made quit attempts in the previous year in western countries (over 40% in Australia, Canada, UK & USA) than in the low- and middle-income countries, with negligible levels of recent use reported from Malaysia. Germany had notably low levels of use among the high-income countries. Korea had a moderate level of medication use, consistent with programs supporting cessation there and Korea's relatively advanced economic conditions.
Figure 3.
Reported use of quit smoking medications in the last year, or between survey waves. Reported only among those reporting making quit attempts in the previous year. Notes: France did not ask for recent use. 95% confidence intervals are presented on the top of the bars. #The bar indicated is based on very small numbers of “yes” answers (<5 cases).
Use of advice-based behavioural supports was typically considerably lower than use of medications. Use of the quitlines (Figure 4) ranged from a high of 12% in New Zealand, to very low levels in some countries where the question was asked, but where facilities are known to be very limited. Surveys did not assess quitline use in countries where no service was offered.
Figure 4.
Reported use of quitlines (or related services) for assistance in smoking cessation (in the last year (previous survey), except where indicated by an asterisk, where it was for the last 6 months) by country, among those reporting making quit attempts in the previous year.
Notes: Question not asked in Uruguay or Mexico because quitline did not exist at survey administration. 95% confidence intervals are presented on the top of the bars. #The bar indicated is based on very small numbers of “yes” answers (<5 cases).
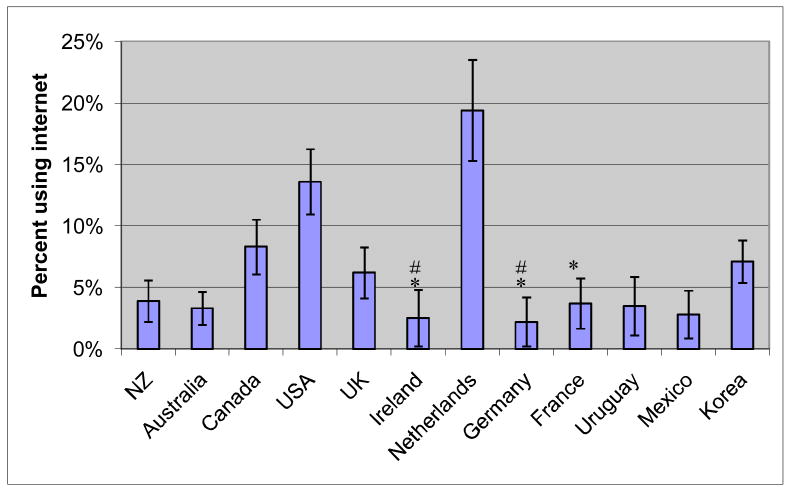
Use of the internet for cessation support varied considerably (Figure 5). Smokers in The Netherlands reported the highest use of the internet for quitting (nearly 20% of those making attempts), followed by the USA (around 13%), with lower levels in other countries where we asked. The high level of use in The Netherlands is likely to be partly due to most of that sample being surveyed on the internet, although the rate for this sub-sample was non-significantly higher in internet use than that for the telephone surveyed sub-sample.
Figure 5.
Reported use of the internet as a source of smoking cessation advice (in the previous year except where indicated by an asterisk, where it is 6 months) by country among those reporting making quit attempts in the previous year.
Notes: Countries not listed here were not asked.95% confidence intervals are presented on the top of the bars. #The bars indicated are based on very small numbers of “yes” answers.
Similarly, the use of dedicated smoking cessation clinics was low (Figure 6), with use of such services highest in the UK which has a dedicated network of clinics. In several countries we have no comparable data, but in some of these at least we can be fairly sure that use of such services is minimal, as few if any are known to exist, and those that do are small and very localized.
Figure 6.
Reported use of specialist cessation services (eg, clinics) in the past year (or where *, 6 months) among those reporting quit attempts in the previous year. Notes: this question was not asked in the other countries or a non-comparable question was used. 95% confidence intervals are presented on the top of the bars. #The bar indicated is based on very small numbers of “yes” answers.
Discussion
There are considerable differences between countries in the level of quitting activity and the level and type of support used. This variation reflects some combination of differences in the history of tobacco control efforts, the capacity of the country or its smokers to afford different quit methods, and the priority given to specific tobacco control policies (e.g., the relative emphasis given to public education, regulatory measures, and provision of cessation assistance); and doubtlessly, more general cultural factors.
Generally speaking, less wealthy countries have fewer resources available to invest in smoking cessation relative to higher income countries, both from governments and individuals. Our data showed that compared to smokers in those high income countries, smokers in middle income countries generally reported lower level use of quitting smoking medications and health professional services, but not always less interest in quitting. Thailand for example reported the highest level of recent quit attempts, probably due to this survey following its first major mass media campaign, backed by several years of legislative reforms and a revered king who speaks strongly against tobacco use. Having a population educated about the harms of smoking and where smoking is institutionally discouraged may be a necessary condition for high levels of smoking cessation activity, but other factors are also clearly important in determining the extent to which this translates into use of help and or provision of advice by health professionals.
Published evidence shows that mass media campaigns to encourage quitting make a large difference to quitting activity (9), and we see this in our, as yet unpublished data. For example, earlier waves of the ITC surveys in Korea and Malaysia, taken just after or during large campaigns, found rates of recent quitting much higher than those reported here, while the reverse was the case in Thailand where the data reported here followed its first large-scale mass media campaign. Published evidence also shows that other population level activities like the introduction of stronger health warnings on cigarette packages (10) and increases in the price of tobacco products can increase quitting activity in a population (11, 12).
One of the most striking findings is the diversity across countries in use of health professionals and in the encouragement they provide for quitting. Overall the lower income countries reported fewer visits to health professionals, for example Mexico and Malaysia were particularly low. But a note of caution, the low level of reporting visits in Malaysia, coupled with the high level of reporting getting advice, raises the possibility that some smokers, at least in Malaysia, answered about visiting health professionals in relation to their smoking, not visits in general. The Malay translation of this question is less clear than elsewhere that any visit is meant. That said, there is little doubt that some of the differences we report are real. We suspect that in many, if not most, of the world's poorer countries, levels of visiting health professionals will be even lower than those reported here for the middle-income countries.
The potential role of health professionals in encouraging cessation is likely to be more limited in countries where smokers consult them less frequently. Further, when visits are rarer, the presenting problems may be more serious, and time constraints may be more likely to squeeze out mention of smoking cessation, especially where it is not relevant to the reason for the consultation.
The highest levels of advice to quit were found in the USA, where there has been a lot of effort to encourage doctors to apply evidence-based guidelines, including those for smoking cessation (13) based on evidence that such advice can motivate quitting (4). However, our data suggest that in some countries doctors are not providing advice as often as they might. For example, we found low rates of providing advice in The Netherlands. We understand that many Dutch physicians are reluctant to intervene with what many consider the right of patients to “choose” the lifestyle they want. As a result, most restrict their advice on this matter to patients with smoking-related complaints. However, reporting that doctors do not seem to take smoking cessation seriously (14), is a commonly voiced rationalization for continuing to smoke, at least in those western countries where it has been studied. Tobacco control advocates should try to convince doctors who are reluctant to provide advice that free choice necessarily involves having adequate knowledge relevant to that choice, and thus they, as health experts, have a responsibility for ensuring that their patients have a realistic understanding of how continuing to smoke risks compromising their long term health. Doctors should raise the issue, encourage cessation to reduce risks, discuss options, and offer whatever help they can (e.g. referring or otherwise pointing their patients/clients in the direction of evidence-based forms of assistance where they are available).
Even in the country where smokers are most likely to receive quit advice from health professionals (the USA), our data suggests that only half of all smokers receive any such advice each year. This highlights the importance of reaching many smokers through interventions outside of the formal health system, such as mass media campaigns or pictorial pack warnings that promote quitting. Population-level interventions are a critically important part of encouraging smokers to use whatever help is available if they feel unable to quit without assistance. Further, promoting services to assist cessation may help make public information campaigns more effective because they signal the importance of taking action.
As would be expected, use of smoking cessation medications also varied greatly by country, much undoubtedly due to limits on affordability and availability in some countries. In some countries, typically richer ones, cessation medications are paid for or subsidized by the government (eg UK, New Zealand) or health insurance schemes (for many in the US) and this is likely to increase use. Germany, which is rich and where medications are widely available and promoted, but which has no subsidies, had low levels of use of medication. However, the role of subsidies is not always a major factor. For example, Australia had much high levels of medication use, most being NRT which is not subsidized (15), and New Zealand with a sophisticated and widely available subsidy scheme has relative low levels of medication use.
Before smokers will begin to use aids, they must want to or at least be convinced of the need to quit smoking, believe that this is something that they need help to do, and then they need to believe that some form of available help is likely to assist them. They also need to have the idea of using aids top of mind, and as there may be less promotion of aids when they are subsidised, this might act to counter the use promoting function of reduced price. To the extent that the low use in some places reflects low demand, then it will be important to create more interest in quitting smoking and a greater realization of the benefits of assistance before rates of use are likely to approach those achieved in countries where reported use levels are nearing half of those making quit attempts.
Use of other forms of assistance was generally lower than use of cessation medications. The forms of support, as well as the overall amount, vary by country. For example, New Zealand and Australia provide most assistance through quitlines, while the UK focuses on face to face services, and the internet is the preferred delivery mode in The Netherlands. The relatively high quitline use in New Zealand probably reflects its provision of heavily-subsidized NRT (16), and in both Australia and New Zealand heavy promotion of the services, including having the telephone number on cigarette packs as part of the health warning material clearly contributes to the higher levels of use (17). In The Netherlands, high level of internet use is related to very high high-speed internet access (>90% of population) and the wide promotion of internet-based cessation support by STIVORO, including tailored advice on a self-help smoking cessation website, all integrated with the national telephone quitline (18). All mass media cessation campaigns refer to the website and not the quitline number, so the website is seen as the first place to go.
The generally low level of use of help, even in countries where smoking prevalence has reduced markedly and such help is widely available, shows that availability of help is not sought by many, and is not necessary to make progress in reducing prevalence. However, help can play an important role because smokers can increase their chances of quitting by using it, and there is some evidence that the provision of services can also encourage self-quitting (19).
It is important to be clear about the limitations of these multi-country comparisons and how they limit the conclusions that can sensibly be drawn. This paper is designed to provide an overview of some large-scale differences between countries to stimulate thinking as to why and what the implications of these large differences might be for policies that relate to the provision of supports for smoking cessation. Small differences (say less than 5%) should be interpreted with extreme caution, and then only as a suggestion of the need to seek corroborating data from other sources to see if they do reflect an underlying reality. The ITC Project interviews were completed in several languages, and although we took care with translations to equate concepts, inevitably the nuances of words differ and these differences may have had some effects on the results. We only surveyed smokers, so we miss quitting activity from recent quitters, thus underestimating quitting activity marginally, but this is common for all countries. Similarly, different data collection modes (eg, face to face interviews vs telephone interviews) might have had some effects, as may differences in response rates. In analyses not reported here we have looked at both kinds of differences. In countries where we used mixed modes of responding, we do not find large survey mode differences. We have also looked for differences in responding between new recruits into our survey and those retained from previous waves (an increasingly less- representative group), and have only found no or small effects (in the order of 2-3% differences in estimates), so sampling effects likely only contribute a small amount to the variance. Further inter-wave intervals varied and even where we asked about a set period, having a reference of a previous survey close to the reference time may have affected responding. We do not know the size of such effects, but believe they are typically small, are most likely to affect reports of events occurring (e.g., of quit attempts and the use of health professionals) rather than what was done on such occasions (use of aids). Further, any biases due to different levels of familiarity with the form of assistance would most likely have acted to reduce the observed differences: over-reporting the rare and underreporting the more commonplace (e.g., any use of medication, even trying, might be reported where use of medication is rare, but in a context of widespread use, more extensive use might be expected before the person would report ‘really’ using it on a quit attempt). Finally, in a couple of countries (China, Mexico, Uruguay) we only surveyed in some cities, so these results should not be generalized to the entire countries, particularly not to rural areas where conditions are much different. We believe that the differences we highlighted are likely to be real between-country differences, but reiterate that readers should not interpret differences between countries of less than around 5% without corroborating evidence.
This study included ten high-income and five middle-income countries, but no data were available from the low income countries more recently included in the ITC study (eg Bangladesh). Future studies of this kind will be able to include such countries, both using ITC data and data from other sources such as the Global Adult Tobacco Survey (GATS).
This study shows that tobacco control strategies that focus on service delivery, or advice giving, within the health-care system are likely to have limited impacts in low- and middle-income countries because contacts with such services are less common. Population-based strategies will be even more important in these countries to encourage smokers to consider quitting, and where necessary, to seek out help. These strategies include mass media campaigns, pictorial health warnings on tobacco packaging, and higher taxes on tobacco products (1), and can produce rapid variations in interest in quitting and quit-related activity. Cessation services can and do provide useful functions. Countries need to consider how to provide such services (including both pharmaceuticals and advice-based help) in ways that best fit into their existing health care system, and to ensure they are accessible, affordable, and widely promoted. Even where an extensive range of services and aids are available and promoted, many smokers do not use them, suggesting that demand for such services is something that only grows gradually with prolonged public education and denormalization of smoking. Allowing services to grow organically with demand is one way to maximize benefits and to minimize initial costs.
Acknowledgments
Declaration of interest: Major funders of multiple surveys were: National Cancer Institute, US (P50 CA111326): (RO1 CA 100362) (R01 CA125116); Canadian Institutes for Health Research (79551);Ontario Institute for Cancer Research (Senior Investigator Award). In addition, major support for individual countries came from: National Health and Medical Research Council of Australia (450110);Cancer Research UK (C312/A3726), Chinese Center for Disease Control and Prevention; Bloomberg Global Initiative - Union Against Tuberculosis and Lung Disease (Mexico 1-06) and the Mexican National Council on Science and Technology (CONACyT Salud-2007-C01-70032); French Institute for Health Promotion and Health Education (INPES), French National Cancer Institute (INCa); German Cancer Research Center, German Ministry of Health; Dieter Mennekes-Umweltstiftung; The Netherlands Organisation for Health Research and Development (ZonMw); New Zealand Health Research Council; The National Cancer Center of Korea (from Ministry of Health and Welfare). The funding sources had no role in the study design, in collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Footnotes
Additional contributions: Other leaders of ITC projects who checked the paper for appropriateness of any claims made about their countries were: Romain Guignard (French Institute for Health Promotion and Health Education, INPES, France), Martina Poetschke-Langer (German Cancer Research Center, Germany), Yuan Jiang (Chinese Center for Disease Control and Prevention, China), Hong-Gwan Seo (National Cancer Institute, South Korea), Edna Arillo-Santillán (Mexico), Marcelo Boado (Uruguay), Buppha Sirirassamee (Mahidol University, Thailand), Maizurah Omar (Universiti Sains Malaysia, Malaysia), and Gerard Hastings (Stirling and Open Universities, UK).
What this research adds: This paper is designed to focus policy-makers attention on the inappropriateness of a “one size fits all” approach to encouraging cessation and providing services to facilitate it. It shows that even in the countries with the best established cessation infrastructure, many smokers do not avail themselves of the available help. It also clearly shows limitations of relying on health professionals as the primary means of educating smokers especially in countries where they are visited less frequently, although they clearly have an important role to play.
Contributorship statement:
RB led the project, co-ordinated drafts and contributed large sections of the text as well as being involved in survey development and the form of some of the questions.
LL and PD conducted most of the analyses and checked the surveys for consistency of questions and ensured maximal comparability and commented on drafts. LL also drafted sections of the Methods.
NW helped in the conceptualisation of the paper, supervised analysis of the New Zealand data and commented extensively on drafts.
DH, GTF, AM, KMC all contributed to the development of the surveys and the specific questions used here, and provided input into the drafts, both overall and specific to their country.
MET contributed to the development of the surveys, provided advice about how to best match up the data and, provided input into drafts and checked to ensure comparability.
UM, MW and JFT provided input into drafts and provided significant sections of text especially related to countries they are from or are associated with.
The Acknowledged others all checked the analyses and interpretations relevant to their country, and in some cases gave permission for their country data to be included.
Ethics Clearance: Ethical clearance for the various components of this study were gained from the appropriate institutions in all participating countries.
Conflict of Interest: No author has any conflict of interest, although some have associations with organisations that deliver smoking cessation services.
References
- 1.World Health Organization. WHO report on the global tobacco epidemic, 2008. The MPOWER package. Geneva: World Health Organization; 2008. pp. 36–38. [Google Scholar]
- 2.Raw M, Regan S, Rigotti N, McNeill A. A survey of tobacco dependence treatment services in 36 countries. Addiction. 2009;104:279–287. doi: 10.1111/j.1360-0443.2008.02443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raw M, McNeill A, Murray R. Case studies of tobacco dependence treatment in Brazil, England, India, South Africa and Uruguay. Addiction. 2010;105:1721–8. doi: 10.1111/j.1360-0443.2010.03043.x. [DOI] [PubMed] [Google Scholar]
- 4.Stead L, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2008. 2008;(2) doi: 10.1002/14651858.CD000165.pub3. Art. No.: CD000165. [DOI] [PubMed] [Google Scholar]
- 5.Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev. 2008;(3) doi: 10.1002/14651858.CD006103.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Databse Syst Rev. 2008;(1) doi: 10.1002/14651858.CD000146.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Lancaster T, Stead LF. Self-help interventions for smoking cessation. Cochrane Database Syst Rev. 2005;(3) doi: 10.1002/14651858.CD001118.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;(3) doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Wakefield M, Durkin S, Spittal M. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98:1–8. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borland R, Yong HH, Wilson N, et al. How reactions to cigarette pack health warnings influence quitting: findings from the ITC Four Country survey. Addiction. 2009;104:669–675. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jha P, Chaloupka FJ. Curbing the epidemic: governments and the economics of tobacco control. Washington, DC: The World Bank; 1999. [Google Scholar]
- 12.Reed M, Anderson CM, Vaughn JW, et al. The effect of cigarette price increases on smoking cessation in California. Prev Sci. 2008;9:47–54. doi: 10.1007/s11121-008-0081-1. [DOI] [PubMed] [Google Scholar]
- 13.Fiore MC, Bailey MD, Cohen DJ, et al. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services; 2000. Treating tobacco use and dependence. Public Health Service. [Google Scholar]
- 14.Mullins R, Borland R. Doctors' advice to their patients about smoking. Aust Fam Physician. 1993;22:1146–1155. [PubMed] [Google Scholar]
- 15.Cooper J, Borland R, Yong H. Australian smokers increasingly use help to quit, but number of attempts remain stable: findings from the International Tobacco Control Study 2002-09. Australian and New Zealand Journal of Public Health. 2011;35:368–76. doi: 10.1111/j.1753-6405.2011.00733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson N, Weerasekera D, Borland R, et al. Use of a national quitline and variation in use by smoker characteristics: ITC Project New Zealand. Nicotine Tob Res. 2010;12 Suppl:S78–84. doi: 10.1093/ntr/ntq111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilson N, Weerasekera D, Hoek J, et al. Increased smoker recognition of a national quitline number following introduction of improved pack warnings: ITC Project New Zealand. Nicotine Tob Res. 2010;12 Suppl:S72–7. doi: 10.1093/ntr/ntq092. [DOI] [PubMed] [Google Scholar]
- 18.TNS Opinion & Social. Special Eurobarometer 335: E-communications Household Survey. Survey requested by the European Commission (EC); Brussels: 2010. [Google Scholar]
- 19.Ossip-Klein DJ, Giovino GA, Megahed N, et al. Effects of a smoker's hotline: Results of a 10-country self-help trial. J Consult Clin Psychol. 1991;59:325–332. doi: 10.1037//0022-006x.59.2.325. [DOI] [PubMed] [Google Scholar]