Abstract
Background
The best method for managing large bone defects during revision knee arthroplasty is unknown. Metaphyseal fixation using porous tantalum cones has been proposed for severe bone loss. Whether this approach achieves osseointegration with low complication rates is unclear.
Questions/purposes
We therefore asked: (1) What is the risk of infection in revision knee arthroplasty with large bone defects reconstructed with porous tantalum cones? (2) What is the rate of osseointegration with these cones? (3) What is the rate of loosening and reoperation? (4) Is knee function restored?
Methods
We retrospectively reviewed 27 patients who had 33 tantalum cones (nine femoral, 24 tibial) implanted during 27 revision knee arthroplasties. There were 14 women and 13 men with a mean age of 64.6 years. Preoperative diagnosis was reimplantation for infection in 13 knees, aseptic loosening in 10, and wear-osteolysis in four. Patients were evaluated clinically and radiographically using the score systems of the Knee Society and followed for a minimum of 2 years (mean, 3.3 years; range, 2–5.7 years).
Results
One knee with two cones was removed for infection. All but one cone showed osseointegration. One knee was revised for femoral cone and component loosening. There was one reoperation for femoral shaft fracture and one for superficial dehiscence. The mean Knee Society pain score improved from 40 points preoperatively to 79 points postoperatively. The mean function score improved from 19 points to 47 points.
Conclusions
Our observations suggest metaphyseal fixation with tantalum cones can be achieved. Longer-term followup is required to determine whether the fixation is durable.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Severe bone loss and durable component fixation are challenging problems in revision knee arthroplasty. Severe bone deficiency, defined as Anderson Orthopaedic Research Institute [8] Type 2B or 3, has been commonly treated using either morselized [4, 20] or bulk allografts [1, 3, 6, 9, 12, 13] depending on the location and size of the defects. Several studies of revision knee arthroplasty in which femoral head and structural bulk allografts were used report a risk of infection ranging from 4% to 8%, a risk of nonunion ranging from 0% to 4%, and an overall rate of reoperation for failure of 8% to 23% [1, 3, 6, 9].
Porous tantalum metaphyseal cones are now available as an alternative treatment for massive tibial and femoral bone defects [16, 17]. Histologic studies indicate porous tantalum presents a surface for osteoblast expression and, ultimately, the growth of native bone into the metal [5, 11, 23]. Data also suggest that tantalum surfaces increase host white blood cell activation and lower bacterial fixation [21, 22], possibly decreasing the risk of infection. These laboratory studies suggest tantalum cones may provide long-term biologic fixation with a lower risk of infection when used in vivo in complex revision knee arthroplasties. Two studies report on the use of tantalum tibial cones [16, 17] with small numbers of patients and limited followup time. These studies reported infection rates of 12.5% [16] and 13.3% [17] and overall osseointegration rates of 100% in both studies [16, 17]. These preliminary results suggest tantalum cones may indeed be a reasonable alternative to bulk or structural allografts and indicate the need for larger series with longer followup time, however, the high infection rates are concerning.
We asked four questions: (1) What is the risk of infection in revision knee arthroplasty with large bone defects reconstructed with porous tantalum cones and antibiotic bone cement? (2) What is the rate of osseointegration with these cones? (3) What is the rate of loosening and reoperation? (4) Is knee function restored?
Patients and Methods
Between 2000 and 2007, three surgeons (PFL, MPB, TPV) at two centers performed 33 revision knee arthroplasties in which tantalum metaphyseal cones were used in reconstructing massive bone defects. Five patients were lost to followup and one patient died before minimum 2-year followup. The study group consisted of 27 revision knee arthroplasties (33 tantalum cones) in 27 patients. The data from one surgeon (PFL) were prospectively collected in an Institutional Review Board (IRB)-approved study incorporating clinical and radiographic data collection, whereas the data from the other two surgeons (MPB, TPV) were retrospectively obtained with separate IRB approval. The specific indication for these implants in revision arthroplasty was severe metaphyseal bone loss resulting from reimplantation for infection, aseptic loosening, and osteolysis/polyethylene wear. The contraindications for use were active infection and minimal metaphyseal bone loss as deemed by the surgeon. Using the knee arthroplasty bone loss classification system of the Anderson Orthopaedic Research Institute [8], the preoperative bone deficiency on the side of tantalum cone use was graded Type 3 in 29 knees (20 tibias and nine femurs) and Type 2B for four knees (all tibias). There were 14 female and 13 male patients with a mean age of 64.6 years (range, 49–84 years). The mean patient weight was 103.4 kg (range, 63.5–164.3 kg) and the mean body mass index was 35.9 kg/cm² (range, 23.6–67.4 kg/cm²). For seven patients, this was the first revision surgery, 11 patients had two previous operations on the knee, and five patients had three previous operations. Three patients had five previous operations before this surgery and one patient had 10 prior operations. The preoperative diagnosis was reimplantation for infection in 13 patients (including three with septic loosening and one with massive osteolysis), aseptic loosening in 10 patients (including one with a broken stem), and polyethylene wear-severe osteolysis in four patients. Patients undergoing reimplantation for infection were treated with two-stage revisions with either static or mobile antibiotic cement spacers, and the duration between stages was no less than 5 weeks [15]. The patients were followed for a minimum of 2 years (mean, 3.3 years; range, 2–5.7 years). Patients without recent followup were recalled specifically for this study; all data were obtained from medical records and radiographs.
The techniques used for tantalum cone and prosthesis implantation have been previously described [17, 18]. Intraoperatively, 24 tibial tantalum metaphyseal cones (Trabecular metal; Zimmer, Warsaw, IN) were implanted. There were 18 knees in which only a tibial cone was implanted and six knees in which both tibial and femoral cones were implanted. Seventeen of the tibial cones were full symmetric cones, and seven were asymmetric stepped cones (Fig. 1A–B). There were nine femoral cones implanted (three knees had only a femoral cone), seven full (Fig. 2A–B), and two stepped cones. Five cones implanted in the distal femur were actually inverted tibial cones. The revision knee components used were 22 constrained condylar knees (LCCK®; Zimmer) with constrained articulation in 17 and posterior stabilized in five, two Natural Knee II® components (Zimmer), and three rotating hinge knees (two RHK®; Zimmer; one Biomet, Warsaw, IN). All revision tibial and femoral components had either cemented polished or press-fit grit-blasted modular stems based on surgeon preference and intraoperative judgment. For the tibial stems, 21 were polished and cemented the entire length of the stem. The cemented tibial stem length was 35 mm in nine knees, 50 mm in one, 75 mm in one, 100 mm (one offset) in seven knees, 125 mm in one knee, and 145 mm in two knees. Three grit-blasted tibial stems were not cemented beyond the cone-prosthesis interface. Two uncemented stems were 130 mm and one was 75 mm. Four polished femoral stems were cemented the entire length of the stem. The length of the cemented femoral stem was 90 mm in one knee, 100 mm in two knees, and 145 mm in one knee. Five femoral stems were not cemented beyond the cone-prosthesis interface. The uncemented femoral stem length was 130 mm in four knees and 175 mm in one knee. The choice of stem length and degree of cementing was decided by the surgeon at the time of operation. Fixation of the components into the metaphyseal tantalum cones was with antibiotic bone cement: Simplex P Tobramycin (Howmedica Stryker Osteonics, Mahwah, NJ) in 13 knees and Endurance Gentamicin (DePuy Johnson & Johnson, Warsaw, IN) in 14 knees. During the revision knee arthroplasty, 11 patella were revised (10 cemented polyethylene and one tantalum patellar component).
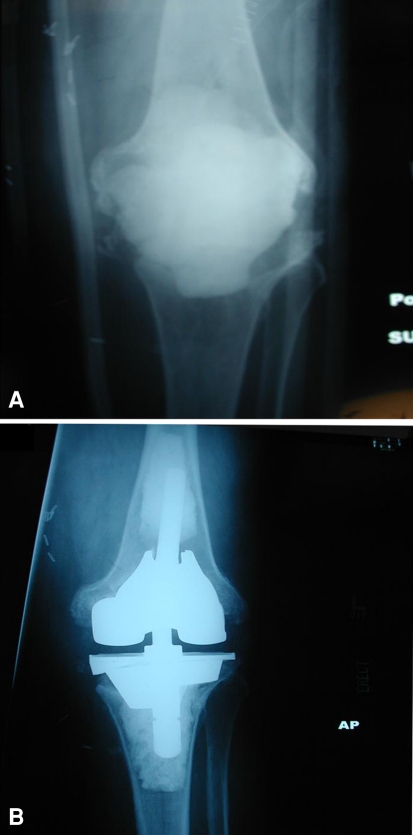
Fig. 1A–B.
(A) Preoperative AP radiograph shows a 75-year-old man who had four prior knee arthroplasties with loosening of the tibial component, a broken stem, and Type 3 tibial defect. (B) Four-year postoperative AP radiograph shows good fixation of a stepped tibial cone and a cemented stem.
Fig. 2A–B.
(A) Preoperative AP radiograph shows a 57-year-old man who had four prior knee procedures, including static antibiotic cement spacer for infection, with Type 3 femoral and tibial defects. (B) Two-year postoperative AP radiograph shows good fixation of a full femoral cone and a stepped tibial cone.
The patients started ambulation, either full or touch-down weightbearing, at the discretion of the surgeon with a walker or crutches on the first postoperative day. All patients received supervised physical therapy twice daily and had a continuous passive motion machine while in the hospital. Supervised physical therapy was continued after discharge at home or at a skilled nursing or rehabilitation facility for 4 to 6 weeks.
The patients were evaluated clinically by the operating surgeon or research nurse (ESS) using the pain and functional score systems of the Knee Society [14]. For the purposes of this study, major complications were defined as deep infection or implant loosening requiring reoperation. Infection was a clinical diagnosis based on a combination of knee aspiration and intraoperative culture in addition to laboratory markers (erythrocyte sedimentation rate, C-reactive protein) [2, 7, 19]. Minor complications included thromboembolism, superficial wound problems, and any other complications that were managed nonoperatively. Radiographic evaluation was performed using the system of the Knee Society [10] using standing AP, lateral, and sunrise radiographs for radiolucent lines and axial alignment (with neutral defined as between 3° and 9° of valgus). Failure was defined as reoperation for implant removal or rerevision.
Results
A deep infection, diagnosed by knee aspiration and intraoperative culture, occurred in one of the 27 patients (3.7%). This patient had a preoperative diagnosis of reimplantation-infection (methicillin-resistant Staphylococcus aureus) and required removal of all components at 28 months as a result of a new infection with Pseudomonas aeruginosa. The tibial cone had good bone ingrowth at the time of resection arthroplasty and was difficult to remove requiring use of a high-speed burr, but the femoral cone and component were grossly loose. At the last clinical followup, the patient had antibiotic spacers in place and no further surgery had been planned.
Osseointegration of the tantalum metaphyseal cones, defined radiographically as absence of radiolucent lines, was noted in 26 patients (31 cones [94%]) at most recent followup. One patient, with five prior operations, had gross loosening of a femoral cone and a hinged knee femoral component and had rerevision with a tumor prosthesis at 25 months. There were 1-mm, nonprogressive, incomplete radiolucent lines seen in 15 of 27 (56 %) knees, usually at the stem extension and unrelated to the tantalum cone. There was no difference in the frequency of radiolucent lines around uncemented or cemented stem extensions. The preoperative anatomic alignment was varus (mean, 8°; range, 3°–14°) in 12 knees, neutral (mean, 5.6°; valgus, range, 3°–8°) in 14 knees, and valgus (11°) in one knee. Although the position of the cones is independent of the prosthesis position, the postoperative anatomic alignment was neutral (mean 5.3° valgus in 24 knees and varus, mean 1°; range, 2° varus to 2° valgus) in three knees.
In addition to the two patients revised for infection and aseptic loosening, respectively, there were two other patients who had a reoperation. One patient fell and had a periprosthetic distal femur fracture at 48 months treated by locking plate fixation. One patient required reclosure of a superficial wound dehiscence. Other minor complications included one nonfatal perioperative myocardial infarction and atrial fibrillation, one nonfatal pulmonary embolus, and one nontraumatic rupture of the vastus medialis obliquus, all treated nonoperatively.
Preoperatively the patients had mean 5° flexion contracture (range, 0°–25°) and a mean 81° flexion (range, 0°–120°). Postoperatively, the mean flexion contracture was 1° (range, 0°–20°) and the mean flexion was 96° (range, 50°–125°). The mean preoperative Knee Society pain score was 40 points (range, 16–85 points), which improved to a mean 79 points (range, 36–97 points) postoperatively. The mean function score preoperatively was 18.5 points (range, 0–60 points), which improved to a mean 47 points (range, 0–100 points) postoperatively.
Discussion
The best management of large osseous defects in revision TKA is unclear and has included the use of bulk allografts, impaction grafting, and tumor megaprostheses. Both filling the defect and obtaining reliable fixation of the implants are challenging problems in this clinical situation. The recent introduction of tantalum tibial and femoral metaphyseal cones has provided an alternative method for reconstruction of severe bone deficiency with metaphyseal fixation. Reviewing a two-center series of 27 revision knee arthroplasties, we sought to evaluate the following questions: (1) What is the risk of infection in revision knee arthroplasty with large bone defects reconstructed with porous tantalum cones? (2) What is the rate of osseointegration with these cones? (3) What is the rate of loosening and reoperation? (4) Is knee function restored?
This study has several limitations. First, the patient cohort was relatively small but still larger than the two previous reports with 15 [16] and 16 [17] patients in each study. Second, these 27 revision arthroplasties were performed by three surgeons with some differences in technique and philosophy of implant fixation and a variety of prostheses were used. Like with all revision knee arthroplasties, each case is somewhat unique. Data review was retrospective at one center. Third, the mean followup time was short, 3.3 years (range, 2–5.7 years), when compared with studies of revision knee arthroplasties performed with structural or bulk allografts. Fourth, five patients were lost to followup, a notable number considering the size of this study. Fifth, full-length radiographs were not obtained for all patients, and accordingly, we are not able to comment on mechanical alignment. The study’s greatest strength is that it represents the largest series to date on the use of tantalum tibial and femoral cones in revision knee arthroplasty.
The rate of infection in these difficult revision knee arthroplasties, 3.7%, was lower than reported in the two published studies of tantalum cones (Table 1). Long and Scuderi reported recurrent deep infection in two of 16 knees (12.5%) and an overall reoperation rate of 12.5% at a mean followup of 2.6 years [16]. Three of 16 revision arthroplasties (18.8%) in their cohort had a preoperative diagnosis of infection. Meneghini et al. reported infection in two of 15 (13.3%) revisions using tantalum tibial cones and an overall reoperation rate of 26.7% at a mean followup of 2.8 years [17]. Five of 15 revisions in that study (33.3%) had a preoperative diagnosis of infection. The relatively low rate of infection in our study is surprising considering that the preoperative diagnosis was reimplantation for infection in 13 of 27 (48.1%) revisions. Differences in surgical methods or patient characteristics between these reports, which may have resulted in the lower infection rate observed in this study, are not immediately obvious. In all three studies, antibiotic bone cement was used for fixation of the revision component in the tantalum metaphyseal cone. However, cement was used only in the metaphysis in the study of Long and Scuderi [16] and 80% of the tibial stems were cemented in the study of Meneghini et al. [17]. In the case of recurrent infection, a tantalum cone may be difficult to remove and may cause additional bone loss. The rate of deep infection was also low relative to that in studies using structural allografts in revision knee arthroplasty. Four studies of femoral head or structural allografts in revision knee arthroplasty reported a rate of infection between 4% and 8% in series of 46 to 70 knees [1, 3, 6, 9]. It should be noted that these allograft studies had a longer mean followup time than the cohort in this study.
Table 1.
Tantalum components of TKA revisions
| Study | Number of knees | Tibia/femur (implants) | Preoperative AORI class | Preoperative diagnosis of infection (knees, %) | Mean followup (years) | Antibiotic bone cement? | Results | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Tibia | Femur | 2a/b | 3 | Infection (knees, %) | Loosening (knees, %) | |||||
| Meneghini et al. [17] | 15 | 15 | 0 | 7 | 8 | 5 (33.3) | 2.8 | Yes | 2 (13.3) | 0 (0) |
| Long and Scuderi [16] | 16 | 16 | 0 | 5 | 11 | 3 (18.8) | 2.6 | Yes | 2 (12.5) | 0 (0) |
| Current study | 27 | 24 | 9 | 4 | 29 | 13 (48.1) | 3.3 | Yes | 1 (3.7) | 1 (3.4) |
AORI = Anderson Orthopaedic Research Institute classification of metaphyseal defects [6]. Class 1 defects are minor femoral or tibial defects with intact metaphyseal bone, not compromising stability of a revision component. Class 2 defects are damaged metaphyseal bone requiring reconstruction to provide stability of the component (Subtype A = one femoral or tibial condyle; Subtype B = both femoral or tibial condyles). Class 3 defects are those with deficient metaphyseal segments compromising major portion(s) of either femoral condyle or tibial plateau, occasionally associated with collateral or patellar ligament detachment.
The rate of reoperation for component loosening in this study was 3.4% with loosening of one femoral cone but no loosening of a tibial cone. Both previous studies of tibial tantalum cones reported no loosening of a cone or revision component, whether or not the stem was fully cemented [16, 17]. These studies, together with our report, suggest these tantalum cones do achieve osseointegration with native host bone at 2 to 5 years followup. These results may be compared with the rate of reoperation for nonunion or component loosening in knee revisions with structural allografts. Backstein et al. reported that 13 of 61 knees (21.3%) failed as a result of graft related complications (including four for infection) at a mean followup time of 5.4 years [1]. Engh and Ammeen reported two cases (4.4%) of aseptic loosening requiring rerevision in 46 knees at a mean followup time of 97 months [9]. These authors used femoral head bulk allografts. Bauman et al. reported 16 allograft-related failures and one nonunion requiring rerevision in 70 knees (22.8%) [3]. Eight of these rerevisions were the result of allograft failure, three resulted from failure of a component not supported by allograft, and five were attributable to infection. Clatworthy et al. reported 12 of 52 knees (23%) had a repeat revision at a mean followup time of 71 months. Of these, five had progressive allograft resorption. However, only 25 patients (29 knees) who were alive who had not had a revision were assessed radiographically [6].
In conclusion, our study suggests the use of tantalum cones for large structural defects in revision TKA is a promising technique with a low rate of infection and component loosening. However, the number of revision arthroplasties using this technique is still smaller than the number or revision knee arthroplasties performed with bulk or structural allografts and the length of followup is still relatively short. Longer-term followup will be necessary to determine if the osseointegration of the tantalum metaphyseal cones and metaphyseal component fixation will be durable.
Acknowledgment
We thank Dr. Tyler Steven Watters for his extensive contribution in data collection and interpretation for this study.
Footnotes
One of the institutions of the authors (Chapel Hill Orthopedics Surgery and Sports Medicine) receives research support from Zimmer, Inc. Two of the authors (PFL, MPB) are also on the Speakers’ Bureau of Zimmer, Inc.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This project was performed at the Durham VA Medical Center, Duke University Medical Center, Durham, NC, USA, and Chapel Hill Orthopedic Surgery and Sports Medicine, Chapel Hill, NC, USA.
References
- 1.Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:104–112. doi: 10.1097/01.blo.0000214426.52206.2c. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Jennings RW, Wolfe MW, Bertot AJ. The Coventry award: the value of preoperative aspiration before total knee revision. Clin Orthop Relat Res. 1997;345:8–16. doi: 10.1097/00003086-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Bauman RD, Lewallen DG, Hanssen AD. Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res. 2009;467:818–824. doi: 10.1007/s11999-008-0679-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamin J, Engh G, Parsley B, Donaldson T, Coon T. Morselized bone grafting of defects in revision total knee arthroplasty. Clin Orthop Relat Res. 2001;392:62–67. doi: 10.1097/00003086-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914. doi: 10.1302/0301-620X.81B5.9283. [DOI] [PubMed] [Google Scholar]
- 6.Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am. 2001;83:404–411. doi: 10.2106/00004623-200103000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Duff GP, Lachiewicz PF, Kelley SS. Aspiration of the knee joint before revision arthroplasty. Clin Orthop Relat Res. 1996;331:132–139. doi: 10.1097/00003086-199610000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175. [PubMed] [Google Scholar]
- 9.Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89:2640–2647. doi: 10.2106/JBJS.F.00865. [DOI] [PubMed] [Google Scholar]
- 10.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 11.Findlay DM, Welldon K, Atkins GJ, Howie DW, Zannettino AC, Bobyn D. The proliferation and phenotypic expression of human osteoblasts on tantalum metal. Biomaterials. 2004;25:2215–2227. doi: 10.1016/j.biomaterials.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE. Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Joint Surg Am. 1997;79:17–25. doi: 10.1302/0301-620X.79B6.7534. [DOI] [PubMed] [Google Scholar]
- 13.Hockman DE, Ammeen D, Engh GA. Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. 2005;20:35–41. doi: 10.1016/j.arth.2004.09.059. [DOI] [PubMed] [Google Scholar]
- 14.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 15.Jacobs C, Christensen CP, Berend ME. Static and mobile antibiotic-impregnated cement spacers for the management of prosthetic joint infection. J Am Acad Orthop Surg. 2009;17:356–368. doi: 10.5435/00124635-200906000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009;24:1086–1092. doi: 10.1016/j.arth.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90:78–84. doi: 10.2106/JBJS.F.01495. [DOI] [PubMed] [Google Scholar]
- 18.Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):131–138. doi: 10.2106/JBJS.H.01061. [DOI] [PubMed] [Google Scholar]
- 19.Parvizi J, Ghanem E, Sharkey P, Aggarwal A, Burnett RSJ, Barrack RL. Diagnosis of infected total knee: findings of a multicenter database. Clinical Orthop Relat Res. 2008;466:2628–2633. doi: 10.1007/s11999-008-0471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ries MD. Impacted cancellous autograft for contained bone defects in total knee arthroplasty. Am J Knee Surg. 1996;9:51–54. [PubMed] [Google Scholar]
- 21.Schildhauer TA, Peter E, Muhr G, Koller M. Activation of human leukocytes on tantalum trabecular metal in comparison to commonly used orthopedic metal implant materials. J Biomed Mater Res A. 2009;88:332–341. doi: 10.1002/jbm.a.31850. [DOI] [PubMed] [Google Scholar]
- 22.Schildhauer TA, Robie B, Muhr G, Koller M. Bacterial adherence to tantalum versus commonly used orthopedic metallic implant materials. J Orthop Trauma. 2006;20:476–484. doi: 10.1097/00005131-200608000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Welldon KJ, Atkins GJ, Howie DW, Findlay DM. Primary human osteoblasts grow into porous tantalum and maintain an osteoblastic phenotype. J Biomed Mater Res A. 2008;84:691–701. doi: 10.1002/jbm.a.31336. [DOI] [PubMed] [Google Scholar]