Abstract
Background
The Knee Society Clinical Rating System was developed in 1989 and has been widely adopted. However, with the increased demand for TKA, there is a need for a new, validated scoring system to better characterize the expectations, satisfaction, and physical activities of the younger, more diverse population of TKA patients.
Questions/purposes
We developed and validated a new Knee Society Scoring System.
Methods
We developed the new knee scoring system in two stages. Initially, a comprehensive survey of activities was developed and administered to 101 unilateral TKA patients (53 women, 48 men). A prototype knee scoring instrument was developed from the responses to the survey and administered to 497 patients (204 men, 293 women; 243 postoperatively, 254 preoperatively) at 15 medical institutions within the United States and Canada. Objective and subjective data were analyzed using standard statistical and psychometric procedures and compared to the Knee Injury and Osteoarthritis Score and SF-12 scores for validation. Based on this analysis, minor modifications led to the new Knee Society Scoring System.
Results
We found the new Knee Society Scoring System to be broadly applicable and to accurately characterize patient outcomes after TKA. Statistical analysis confirmed the internal consistency, construct and convergent validity, and reliability of the separate subscale measures.
Conclusions
The new Knee Society Scoring System is a validated instrument based on surgeon- and patient-generated data, adapted to the diverse lifestyles and activities of contemporary patients with TKA. This assessment tool allows surgeons to appreciate differences in the priorities of individual patients and the interplay among function, expectation, symptoms, and satisfaction after TKA.
Introduction
The last 40 years have witnessed the emergence of scoring systems to quantify the results of orthopaedic procedures. In the field of TKA, attempts to quantify outcome were pioneered by Insall et al. [24] with the development of physician-administered scales to assess patients’ pain and function. These efforts led to the publication of the American Knee Society Clinical Rating System [23] in 1989 (later modified in 1993 [52]), which subsequently became widely supported and adopted [3, 9, 13, 28, 29]. Part of the appeal of this scoring system was the empirical use of two scales, both of 100 points, to separately define the clinical and subjective status of the knee. Using this format, the outcome of TKA was expressed in terms of a Knee Society Knee Score, derived from the severity of pain reported by the patient and the alignment, stability, and motion of the knee, and a Knee Society Function Score, based simply on the patient’s ability to walk and climb stairs.
This common-sense approach to measurement of the outcome of TKA represented a major advance in the evaluation of the results of knee surgery. However, with the rapid development of the outcomes movement and the widespread adoption of rigorous psychometric principles to develop assessment instruments, new standards have emerged for evaluating clinical scoring systems. The application of these methodologies to compare different assessment instruments has shown, although the Knee Society scoring system is concise and user-friendly, the Knee Society Knee Score demonstrates poor reliability with acceptable responsiveness, while the Knee Society Function Score demonstrates good reliability with questionable responsiveness [3, 13, 29, 33].
Another important consideration is the dramatic shift that has occurred over the past 20 years in the proportion of younger and more active patients undergoing TKA and the projected growth of this procedure over the next decade [31, 32]. When the original Knee Society scoring system was introduced by Insall et al. [23] in 1989, the many patients receiving TKA were sedentary, and hence, evaluation of knee function on the basis of the patient’s ability to walk and climb stairs may have been appropriate. Today, with many patients expecting to live more than two decades after TKA, it seems essential the outcome of these procedures addresses the ability of each patient to remain actively involved in functional and recreational activities far beyond the rudimentary activities of daily living.
Part of a growing trend in the development of new and more accurate assessment of clinical outcomes is the involvement of each patient in assessing the outcome of medical treatment. Since TKA is an elective procedure, patient-reported subjective outcomes, as opposed to strictly objective or technical measures, are essential to any assessment of how well this intervention serves the goals of the patient [16, 55]. Further, outcomes such as symptoms are, by definition, patients’ perceptions of abnormal states [30] and this definition necessitates patient report of symptom outcomes [2, 14]. The standards for developing and use of patient-reported outcomes for medical product development to support labeling claims have been put forward by the US Food and Drug Administration [53]. Moreover, patient-reported measures offer clear advantages in several different dimensions, all of which have a large subjective component. These include the relief of preoperative symptoms, postoperative function, patient satisfaction, and fulfillment of patient expectations.
Another critical element in the development of improved outcome instruments is a clear definition of the properties of the ideal measurement tool and the methodologies for determining whether those requirements are met in practice. The ideal instrument should not only be validated but also broadly applicable, characterizing the outcomes of every patient no matter whether the result is excellent, good, or poor. The ideal instrument should also detect changes due to treatment (ie, be sensitive) and should be able to provide the measure of patient outcome in a heterogeneous patient population, for example, the population that is diverse with respect to age or sex [6, 8]. Further, it is important to minimize ceiling effects, where one encounters patients with high scores that do not distinguish between differing outcomes. In striving to achieve these goals, we, as a task force appointed by The Knee Society, have developed a new Knee Society Scoring System. This new instrument maintains several of the key features of its predecessor, as well as desired measurement properties, reliability, and validity. Key features of the new scoring system include questions addressing patient satisfaction, patient expectations, and the patient’s symptoms while participating in a broad range of activities encountered in daily living, exercise, recreation, sporting activities, and those activities of greatest personal importance to each patient.
In this paper, we will describe the development and initial testing of the new instrument. These processes of development and testing were organized around the facets of the knee (otherwise termed “domains”), leading to a multidimensional knee score that reflects the health and function of the knee in meeting the unique demands of each patient. We will also describe the formal psychometric process undertaken to test the validity and reliability of this new outcome instrument.
Materials and Methods
Under the Chairmanship of Dr Giles R. Scuderi, The Knee Society appointed a task force of members with an established interest in the development of outcome instruments. The Knee Society Task Force proposed the new Knee Society Scoring System be based on information from two domains: (1) objective measures, which would be surgeon-generated measures based on the objective component of the original Knee Society scoring system and would grade the technical outcome of the procedures on the basis of pain, ROM, alignment, and stability; and (2) subjective measures, which would be other outcome measures determined by the individual patient and would include knee function, satisfaction, and fulfillment of expectations.
The goal of the development effort was set to create psychometrically sound measures assessing each of these domains and providing a set of separate subscores that could be generated within a doctor’s office without the need for specialized software. A further challenge was the development of an instrument that could assess knee function from voluntary activities that varied greatly among respondents [49, 51].
Procedures for Data Collection and Instrument Testing
The instrument development and testing consisted of several phases. In Phase I, the pool of generated questions (items) was administered to 101 patients with TKAs. The analysis of these data informed the refinement of items and the development of the prototype instrument in Phase II. Phase II also included the testing of the prototype with approximately 500 patients with TKAs. The analysis of these data led to the modification of the prototype, leading to the final instrument and scoring guidelines. Below we describe each of the phases. All phases of this study were approved by the Institutional Review Boards of the participating institutions in the United States and Canada.
As a preliminary step in the development of the new outcomes instrument (Phase I), the task force created a comprehensive knee function inventory to collect information describing the knee activities of patients with TKAs of all ages and activity levels. The inventory was based on the self-administered Total Knee Function Questionnaire (TKFQ), which was previously developed and validated at the Institute of Orthopedic Research and Education in Houston, TX, USA [42, 55]. The TKFQ was enlarged through the addition of a broad assortment of high-demand activities, primarily those involving gym exercise and recreational sports, as numerous studies have documented frequent involvement of younger and more active patients in these pursuits (Table 1) [20, 39]. The expanded questionnaire included queries within the following domains: knee symptoms (15 questions), ability to walk and run (seven questions), activities of daily living (22 questions), movement and lifestyle (11 questions), exercise, workout, and sports (56 activities). The patient’s ability to perform activities of daily living was assessed through the extent to which the patient’s participation in each activity was limited by his/her knee. Patients’ experiences in activities involving movement and lifestyle and exercise and sports were assessed on the basis of frequency of participation, the personal importance of each activity, and the severity of knee symptoms during each activity.
Table 1.
Inventory of optional activities presented to patients after TKA
| Exercise and sports | Workout/gym activities | Movement and lifestyle | Adventure and water sports | Contact/team sports | Running/biking |
|---|---|---|---|---|---|
| Ballet | Elliptical machine | Carrying bags > 100 m | Canoeing/kayaking | Baseball/softball | Jogging |
| Bowling | Jumping rope | Climbing a ladder | Diving | Baseball/softball: catcher position | Marathons |
| Crosscountry skiing | Kick boxing | Kneeling | Downhill skiing | Basketball | Road cycling |
| Dancing | Leg curls | Lunging | Motor biking/motocross | Boxing | Running |
| Doubles racquet sports | Leg extensions | Moving laterally | Mountain biking | Field hockey | Triathlons |
| Fishing | Leg press | Playing musical instrument | Parachuting | Football: full contact | |
| Golf | Stair climber | Sexual activity | Rock climbing | Ice/roller hockey | |
| Hiking/backpacking | Stationary biking/spinning | Shopping | Rowing | Lacrosse | |
| Horseback riding | Stretching exercises | Squatting | Sailing or yachting | Martial arts | |
| Hunting | Water aerobics | Turning | Skateboarding | Rugby | |
| Inline skating | Weight lifting | Yoga | Snowboarding | Soccer | |
| Singles racquet sports | Surfing | Volleyball | |||
| Swimming | Waterskiing | Wrestling | |||
| Windsurfing |
We performed this phase of the study with 101 patients with TKAs (53 women, 48 men) with an average age of 69.1 years (range, 45–91 years) who had undergone TKA during the period 2004 to 2005. All procedures were performed by members of the Knee Society Task Force using contemporary surgical techniques and prostheses. The inclusion criteria were patients who were 18 years or older and English-speaking (the TKFQ, on which the survey was based, has only been produced and validated in English) and had undergone a primary, unilateral TKA at least 12 months previously. Patients who could not complete or understand the long self-administered survey instrument, who had a previous TKA, or who had pathology, prior injury, or prior surgery involving the contralateral knee were excluded.
In addition to the inventory of knee activities generated by the Knee Society Task Force, the following surveys were administered to each of the 101 participants: (1) the Knee Society Function Score, which is a subscale of the Knee Society Clinical Rating System and has established convergent validity and responsiveness [33]; (2) the Oxford Score [14], which has established construct validity, responsiveness, and internal consistency and reliability [22]; (3) the composite score of the TFKQ; and (4) the average difficulty that patients reported when performing the five activities of most personal importance [42].
We received completed survey instruments from all 101 patients and analyzed them to determine (1) the percentage of patients regularly participating in each activity, (2) of those performing each activity, the percentage of patients who considered it personally important, and (3) the personal importance of each activity, defined as the product of participation and importance. The Knee Society Function Score, Oxford Score, and TKFQ Score were also calculated, in addition to the average TKFQ Score and the average difficulty that patients reported when performing the five activities of most personal importance.
We developed trial versions of a new Knee Society Knee Score for evaluating the status of the knee both before and after TKA (Phase II). The objective component of the instrument was similar to the format of the original Knee Society Score and consisted of six items evaluating knee pain (50 points), alignment (10 points), stability (25 points), and ROM (25 points). The subjective component was developed as a patient-reported outcome measure, based on responses in three domains: satisfaction with outcome (12 items; 100 points), fulfillment of expectations (three items; 15 points), and ability to perform functional activities (21 items; 110 points).
The patient satisfaction questions were derived from the validated, self-administered satisfaction scale (very satisfied, satisfied, neutral, somewhat dissatisfied, very dissatisfied) of Mahomed et al. [7, 17, 35], which assessed overall satisfaction and satisfaction with pain relief and the ability to perform daily and leisure activities. The questions queried the respondent’s satisfaction with the functioning of their knee when performing six different activities and with the level of pain while performing three activities, ranging from sitting to walking up and down stairs. The expectation questions were derived from the work of Mahomed et al. [34] and queried the presence and fulfillment of each patient’s expected outcomes in terms of relief of pain and their ability to perform leisure, recreational, and sports activities and activities of daily living.
Each patient’s assessment of his/her knee function was evaluated through sets of items including standing and walking (four items; 35 points), a graded series of standard activities including activities of daily living (six items; 30 points), an additional six advanced activities (20 points), and three discretionary activities, defined as the three activities most important to each individual patient. Through analysis of the results of the inventory of activities (Phase I), discretionary activities were selected for inclusion in the prototype Knee Society instrument if the following criteria were met: (1) more than 20% of patients with TKA reported frequent participation; or (2) 0% to 20% of patients with TKA reported frequent participation and patients who performed the activity reported the activity was extremely important to them (eg, golf, racquet sports); or (3) though performed by fewer than 10% of respondents, the activity imposed physical demands that would potentially characterize the most active individuals (eg, jogging, running).
For this new prototype questionnaire, we recruited 497 patients (204 men, 293 women) at 15 medical institutions within the United States and Canada, corresponding to an average enrollment of 33.1 patients per location. Two hundred fifty-four of these patients (the preoperative group) were scheduled to undergo TKA within 6 months or less of completing the prototype knee instrument. Ninety-six of these patients (38%) were male (average age, 65.7 years) and 158 (62%) were female (average age, 66.0 years), and none had undergone prior TKA. The remaining 243 patients (the postoperative group) consisted of 108 men (44%; average age, 66.4 years) and 135 women (56%; average age, 67.7 years) who had undergone primary unilateral TKA at least 12 months (average, 25.1 months) before completing the questionnaire. Adjusted for sex, there was no difference between the patients within the two groups in terms of height (men: 178.6 cm; women: 163.1 cm), weight (men: 99 kg; women: 84.1 kg), or BMI (men: 31.1 kg/m2; women: 31.6 kg/m2).
We collected demographic characteristics such as age and sex as part of the patient survey. All research subjects completed the appropriate (pre- or postoperative) prototype instrument in addition to two instruments that had been previously validated, the Knee Injury and Osteoarthritis Score (KOOS) and the SF-12. The SF-12 has established content and construct validity and internal consistency reliability. Physical and mental component summary scores were derived and used [54]. The KOOS has established content and construct validity and internal consistency reliability [46, 47]. Pain, other symptoms, function in activities of daily living, function in sport and recreation, and knee-related quality of life were derived and used.
All completed questionnaires were shipped to the Institute of Orthopedic Research and Education for data entry and analysis. Each completed form was scanned and the encoded responses were stored in a computer database. Normality of distribution of the subscale scores was assessed using the normal plots and Kolmogorov-Smirnov tests for the pre- and postoperative data. All data were normally distributed and comparisons were made between pre- and postoperative scores for all the subscales using independent-samples t-tests with results reported as mean ± SD. Significance level was set a priori at p < 0.05.
Approaches to Validity and Reliability Assessments for Subscale Measures
We performed the assessments of reliability and validity of the prototype using the methods of classical test theory and item response theory (IRT), as described in Appendix 1. The analyses were performed for the objective subscale and for each subscale of subjective measures (satisfaction, expectation, and functional activities subscales: walking and standing, standard activities, advanced activities, discretionary activities).
Results
Phase I: A Comprehensive Survey of Knee Activities Performed by Patients With TKAs
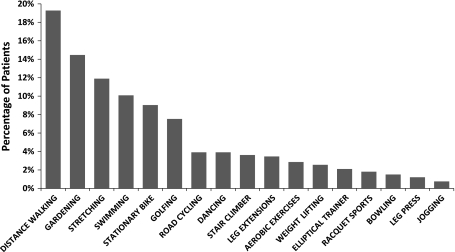
Correlation analysis of the activity-specific outcome scores revealed the scores observed with many activities were highly correlated. Therefore, a stepwise regression analysis was performed to determine the smallest set of activities that would predict the composite function, as expressed by the TKFQ Score. Ten activities were correlated with the TKFQ (p < 0.001), and the inclusion of additional items did not lead to a substantial improvement in prediction of outcome. An additional analysis was performed to determine the number of different activities that must be selected to encompass the most important activities selected by our patient population. In 92% of cases, it was possible to find at least two activities that patients considered important if they were given 14 possible choices; however, this percentage dropped to 83% and 68% when the number of activities per patient increased to three and four, respectively. Most importantly, we found no strong concordance between the activities patients considered most important and those most predictive of outcome. Thus, of the 10 activities selected by statistical analysis, only eight ranked in the 15 most important activities to the patient population, and four of the seven most important activities were not retained in the statistical model. This indicates, because of the diversity of activities performed by patients with TKA, a wider array of activities must be considered for scoring of outcome if virtually all patients with TKA are to find choices applicable to their own lifestyle (Fig. 1).
Fig. 1.
A graph show the most important activities involving the knee, as reported by the patients with TKA enrolled in this study.
Phase II: Evaluation of the Prototype Knee Society Score
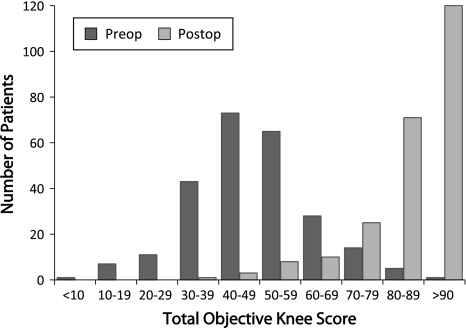
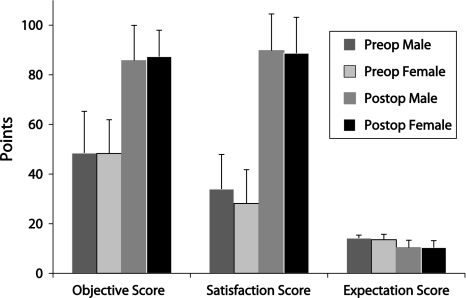
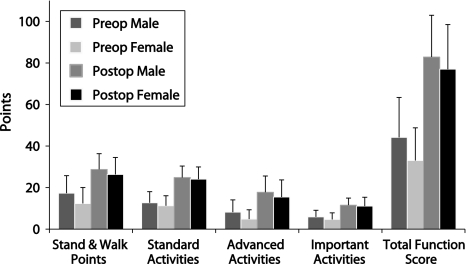
A broad range of values of the Objective Knee Score was observed in the preoperative group, with an average score of 48.3 ± 14.8 points (n = 254) (Fig. 2). In the postoperative group, the average score was 86.6 ± 12.4 points, with ½ of the group scoring in excess of 90 points (n = 243; p < 0.001). Similar differences between the pre- and postoperative groups were seen in the satisfaction score (30.3 ± 14.0 versus 89.2 ± 14.6 points, p < 0.001), and the total function score (37.2 ± 17.9 and 79.6 ± 21.0 [110-point scale]; p < 0.001), corresponding to differences of 194% and 114%, respectively (Fig. 3). The average expectation score (15-point scale) was higher (p < 0.001) in the preoperative group (13.8 ± 1.9 points) than in the postoperative group (10.4 ± 2.9 points). The improvement in function of the postoperative patients varied with the type of activity assessed, ranging from 93% for standing and walking (27.4 ± 8.0 versus 14.2 ± 8.4 points, p < 0.001) to 170% for advanced activities (16.5 ± 8.1 versus 6.1 ± 5.3 points, p < 0.001) (Fig. 4).
Fig. 2.
A graph shows the distribution of values of the Objective Knee Score for patients in the preoperative and postoperative study groups. Preop = preoperative; postop = postoperative.
Fig. 3.
A graph shows the average values of the Objective Knee Score (maximum: 100 points), Satisfaction Score (maximum: 100 points), and Expectation Score (maximum: 15 points), recorded using the prototype Knee Society instrument, for both male and female patients in the preoperative and postoperative groups. Error bars = SD. Preop = preoperative; postop = postoperative.
Fig. 4.
A graph shows the average values of the Function Score (maximum: 110 points) and its subscales, recorded using the prototype Knee Society instrument, for both male and female patients in the preoperative and postoperative groups. Error bars = SD. Preop = preoperative; postop = postoperative.
Internal Consistency, Construct and Convergent Validity, and Reliability Assessments for Subscale Measures
The values of Chronbach’s alpha for the satisfaction construct were 0.90 for preoperative data and 0.95 for postoperative data (Table 2). Slightly lower values were observed for the expectation construct (preoperative: 0.79; postoperative: 0.92). Values for the individual subscales of the functional activities subscale ranged from 0.68 to 0.95, which suggests an acceptable level of internal consistency. Conversely, values for the objective subscale were only 0.41 preoperatively and 0.42 postoperatively, indicating a lack of acceptable internal consistency.
Table 2.
The values of Chronbach’s alpha for each of the subscales of the prototype instrument and the components of the functional subscale
| Time | Objective Knee Score | Satisfaction Score (5 items) | Expectation Score (3 items) | Functional Activity Score | |||
|---|---|---|---|---|---|---|---|
| Walking and standing (4 items) | Standard activities (6 items) | Advanced activities (5 items) | Discretionary activities (3 times) | ||||
| Preoperative | 0.41 | 0.90 | 0.79 | 0.68 | 0.87 | 0.88 | 0.72 |
| Postoperative | 0.42 | 0.95 | 0.92 | 0.71 | 0.88 | 0.84 | 0.82 |
Exploratory factor analysis was performed to assess whether all of the items (questions) within each domain elicited internally consistent responses (construct validity) [26, 27]. The results showed the underlying constructs of the expectation and function instruments (both pre- and postoperative) responded unidimensionality and thus gave internally consistent responses. Moreover, each subscale of the function instrument (ie, walking and standing, standard activities, advanced activities, and discretionary activities) had construct validity, both pre- and postoperatively. Thus, the use of a separate summed score for each subscale was supported by the analysis. However, in the case of the satisfaction questionnaire, while unidimensionality was supported, two items were inconsistent with the other 10 items and were eliminated. For the objective subscale, the results show the underlying constructs of the pre- and postoperative questionnaires did not respond unidimensionally. The stability items were consistently aligned and thus represented a single dimension. Two pain items loaded onto another separate dimension; however, the rest of the items did not have high correlations with other items or common dimensions. Thus, the use of a summed objective score was not supported by the analysis.
Concerning convergent validity, correlations for pre- and postoperative satisfaction score data were found with all related constructs (p < 0.001) (Table 3). Correlations were also found with the objective scores, both pre- and postoperatively (p < 0.05). Conversely, preoperative expectation scores were not related to pain, symptoms, activities of daily living, or quality of life (p > 0.05). Although the mental component score of the SF-12 showed a correlation with preoperative expectations scores, the correlation was small (r = 0.140) and likely not clinically relevant. Given the number of repeated tests, chance is a likely explanation for its statistical significance. In contrast, we found correlations with the expectation scores for postoperative data on all related constructs (p < 0.001) except the SF-12 mental component score (p = 0.107) (Table 3).
Table 3.
Correlation (Pearson product-moment) between the satisfaction, expectation, and objective subscales of the prototype instrument and the individual subscales of the SF-12 and KOOS for preoperative and postoperative data
| Scoring system | Subscale | r value | |||||
|---|---|---|---|---|---|---|---|
| Satisfaction subscale | Expectation subscale | Objective subscale | |||||
| Preop | Postop | Preop | Postop | Preop | Postop | ||
| SF-12 | PCS | 0.420* | 0.513* | 0.121 | 0.396* | 0.164* | 0.334* |
| MCS | 0.283* | 0.267* | 0.140* | 0.107 | 0.155† | 0.209* | |
| KOOS | Pain | 0.650* | 0.736* | 0.062 | 0.421* | 0.0391* | 0.605* |
| Symptoms | 0.408* | 0.500* | 0.044 | 0.286* | 0.198* | 0.317* | |
| ADL | 0.641* | 0.782* | 0.117 | 0.458* | 0.325* | 0.581* | |
| Sport/recreation | 0.317* | 0.597* | −0.012 | 0.391* | 0.156* | 0.461* | |
| Quality of life | 0.524* | 0.702* | 0.014 | 0.425* | 0.223* | 0.483* | |
* p < 0.0001; †p < 0.03; KOOS = Knee Injury and Osteoarthritis Outcome Score; preop = preoperative data; postop = postoperative data; PCS = physical component summary score; MCS = mental component summary score; ADL = activities of daily living.
The pre- and postoperative functional activities subscale scores correlated with all related constructs (p < 0.001) (Table 4), although the postoperative standing and walking (p = 0.187), advanced activities (p = 0.197), and discretionary activities (p = 0.097) subscale scores did not correlate with the mental component score of the SF-12. The correlations among the four subscales of the functional activities construct were also substantial. In view of the magnitude of these correlations, the use of a single aggregate function score derived from the sum of all four subscale scores is justified.
Table 4.
Correlation (Pearson product-moment) between the functional activities subscale of the prototype instrument and the individual subscales of the SF-12 and KOOS for preoperative and postoperative data
| Scoring system | Subscale | r value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Functional activities subscale | |||||||||
| Walking and standing | Standard activities | Advanced activities | Discretionary activities | ||||||
| Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | ||
| SF-12 | PCS | 0.600* | 0.587* | 0.366* | 0.539* | 0.352* | 0.433* | 0.338* | 0.530* |
| MCS | 0.267* | 0.086 | 0.308* | 0.215† | 0.273* | 0.086 | 0.171† | 0.115 | |
| KOOS | Pain | 0.466* | 0.585* | 0.689* | 0.725* | 0.567* | 0.460* | 0.582* | 0.658* |
| Symptoms | 0.208† | 0.245* | 0.411* | 0.446* | 0.284* | 0.313* | 0.287* | 0.364* | |
| ADL | 0.483* | 0.662* | 0.753* | 0.793* | 0.596* | 0.529* | 0.593* | 0.717* | |
| Sport/recreation | 0.292* | 0.482* | 0.383* | 0.596* | 0.461* | 0.527* | 0.471* | 0.568* | |
| Quality of life | 0.407* | 0.543* | 0.552* | 0.693* | 0.485* | 0.509* | 0.486* | 0.654* | |
| New Knee Society Scoring System | Functional activities subscale | ||||||||
| Walking and standing | 1.000 | 1.000 | 0.493* | 0.691* | 0.556* | 0.604* | 0.370* | 0.566* | |
| Standard activities | 0.493* | 0.691* | 1.000 | 1.000 | 0.660* | 0.651* | 0.601* | 0.711* | |
| Advanced activities | 0.556* | 0.064* | 0.660* | 0.651* | 1.000 | 1.000 | 0.557* | 0.455* | |
| Discretionary activities | 0.370* | 0.566* | 0.601* | 0.711* | 0.557* | 0.455* | 1.000 | 1.000 | |
* p < 0.0001; †p < 0.009; KOOS = Knee Injury and Osteoarthritis Outcome Score; preop = preoperative data; postop = postoperative data; PCS = Physical component summary score; MCS = mental component summary score; ADL = activities of daily living.
The results of IRT analyses for the satisfaction construct revealed adequate coverage overall, with a potential redundancy among three of the items for both pre- and postoperative data. As the item discrimination parameters were close, two items were removed based on subject matter expertise. The results of IRT analyses for the expectations construct revealed adequate coverage overall, with a slight redundancy between two items for both pre- and postoperative data; however, given the short length of the subscale, a decision was made to retain all three items. The results of IRT analyses for the walking and standing and standard activities subscales of the functional activities construct revealed good coverage overall in the lower range of functional activities for both pre- and postoperative data, with redundancy between two items of the standard activities subset. Given that one of these items also exhibited differential item functioning (DIF) by sex (see Appendix 1), a decision was made to remove it. Good coverage of difficult activities was observed for the advanced acitivities subscale for pre- and postoperative data, with redundancy between among questions. However, since the advanced activities subscale is the only section of the functional activities construct that covers the range of more difficult functional activities, a decision was made to retain all items. The results of the IRT analyses for the discretionary activities subscale of the functional activities construct revealed good coverage with no redundancies for both pre- and postoperative data. The results of the IRT analyses for the objective construct revealed adequate coverage overall for both pre- and postoperative data; however, the alignment item was not consistent with the rest for preoperative data and had very low item location parameter for postoperative data. Thus, the separation of this item from the other items is supported.
There was no DIF for the items of the objective, satisfaction, or expectations constructs (pre- and postoperative) after adjustment for multiple testing. One item of each of the walking and standing, standard activities, and advanced activities subscales of the functional activities construct exhibited uniform DIF by sex. These items were removed from the walking, and the standing and standard activities subscales; however, given the need for more difficult functional activities in the advanced activities subscale, a decision was made to keep this item. Some DIF was detected for items on all subscales as a function of age; however, the magnitudes of these effects in terms of final scores were too small to be of practical importance.
The Final Design of the New Knee Society Scoring System
The statistical and psychometric analysis led to shortening of the prototype instrument with consolidation of items, primarily within the satisfaction subscale. The final design of the new Knee Society Scoring System consists of four subscales: (1) Objective Knee Score (seven items; 100 points), (2) Satisfaction Score (five items; 40 points), (3) Expectation Score (three items; 15 points), and (4) Functional Activity Score (19 items; 100 points). Further details appear in Appendix 2, and the scoring instrument is presented with an editorial in this issue of Clinical Orthopedics and Related Research [50].
Discussion
We have successfully developed and completed initial testing of a new multidimensional Knee Society Score that quantifies the health and function of the knee from the perspectives of both the surgeon (the objective score) and the patient (the subjective score). Moreover, we have developed subscores that further define the outcome of TKA in terms of symptoms, deformity, stability, and ROM (components of the objective score), in addition to patient satisfaction, fulfillment of expectations, and function in performing the activities of daily living and advanced and discretionary activities (components of the subjective score).
The new Knee Society Score offers substantial benefits in capturing the outcome of TKA from a contemporary frame of reference. In keeping with the movement toward patient-reported outcome measures that have become widely adopted in many fields of medicine, many of the items present in the subscales of the new scores are based on patient self-report [53, 55, 56]. Moreover, the internal priorities and responses of each patient to the outcome of TKA are captured in every domain of the subjective score, including function, expectation, and satisfaction. This is a major philosophical departure from the previous Knee Society Score and is driven by the belief that the outcome of all musculoskeletal interventions involves trade-offs and that only the patient can truly assess the extent to which his/her outcome is optimal [4, 57, 58].
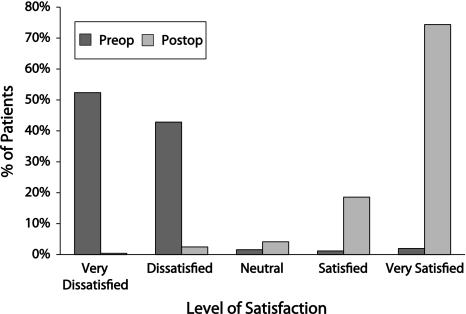
The addition of patient satisfaction to the traits measured by the new Knee Society Score recognizes discrepancies exist between clinician- and patient-derived health-related quality-of-life tools [25, 38]. Despite substantial advances in patient selection, surgical technique, and implant design for primary TKA, numerous reports indicate only 82% to 89% of patients report they are satisfied or very satisfied with their primary TKA, with the prevalence of frank dissatisfaction with knee function ranging from 8% to 15% after these procedures (Fig. 5) [1, 11, 15, 18, 21, 41, 45].
Fig. 5.
A graph shows the distribution of levels of patient satisfaction, as recorded by the prototype Knee Society instrument, for the preoperative and postoperative patient groups. Preop = preoperative; postop = postoperative.
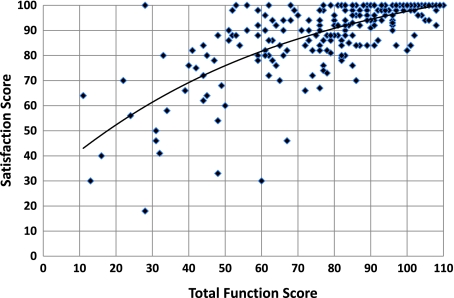
The role of expectations in determining satisfaction with TKA is also well-documented [36, 37, 40]. As this procedure is performed for both pain relief and restoration of joint function, each patient’s individual goals with respect to postoperative function and activity will fundamentally determine the extent to which his/her outcome is successful, the degree of any residual disability, and whether, at some point in the future, symptoms related to knee function will cause the patient to seek additional treatment. In a landmark study, Bourne et al. [7] prospectively followed a large cohort of patients with primary TKA enrolled in the Ontario Joint Replacement Registry who were representative of academic and community high- and low-volume centers. They found 81% were very satisfied or satisfied with their primary TKA at 1-year followup. Only 72% of patients were satisfied with their pain relief and their ability to go up and down stairs, compared to 85% of patients who were satisfied with their pain relief and ability to walk on level surfaces. Consistent with the findings of Mahomed and others [7, 17, 35, 41], our results in developing the new Knee Society Scoring System have reiterated the conclusion that the greatest predictor of patient dissatisfaction is failure of a procedure to meet patient expectations (Fig. 6).
Fig. 6.
A scatterplot shows the values of the Satisfaction Score and the Function Score, as recorded by the prototype Knee Society instrument. Low Knee Society Function Scores are typically associated with low levels of patient satisfaction with the outcome of TKA.
Much of the effort committed to the development and testing of the new Knee Society Score has been devoted to the measurement of function within the context of essential activities (eg, activities of daily living), higher-level activities (eg, carrying loads, squatting, kneeling), and discretionary/recreational activities (eg, exercise, sport, gym). This is associated with a number of challenges in creating a consistent outcome score that is amenable to conventional statistical analysis. At the outset, the diversity of patients who undergo TKA, in terms of age, sex, and lifestyle make it particularly difficult for any given set of activities to adequately capture those activities that are of importance to any one patient or, in many cases, activities that may even be performed by a major proportion of the target population. The new Knee Society Score has addressed this issue through use of a statistical process for selecting activities to gauge patient function. This process balanced the validity and sensitivity of each activity considered for inclusion in the instrument with the frequency of participation in that activity of patients with TKA of different ages and both sexes.
An additional challenge arises from the inclusion of recreational or discretionary activities. The task force was convinced an essential feature of the new Knee Score should be accommodation of activities that the individual patient frequently performs and perceives as being important. However, by definition, activities that patients perform voluntarily (ie, by choice) will typically not be undertaken by the majority of patients. Moreover, previous studies have shown the younger and more active the patient is, the less common are the activities that a subgroup of patients considers of major importance (eg, golf, road cycling, bowling, ballet, yoga, rowing). To meet this challenge, the new Knee Society Score allows patients to select three activities of personal importance from a battery of 17 activities that field testing showed captured the favorite activities of almost all patients.
The work required to develop the ideal instrument for assessment of musculoskeletal outcomes will never be complete. The instrument we have developed to date has been tested in 15 participating medical institutions across the United States and Canada, resulting in a sample of patients. Although the patients enrolled in this study were geographically diverse, they were culturally homogeneous, which is a limitation of the work completed to date. While the findings obtained in this study are not generalizable beyond the population of patients treated at these institutions, the samples were large and included both men and women, as well as patients from different age groups. Future work should also explore the applicability of this instrument to the measurement of outcomes in the face of comorbid conditions, including a contralateral joint arthroplasty and concomitant pathology of the hip or spine. Adaptations of the new score are also needed in countries outside the United States and Canada, with appropriate substitution of culturally appropriate items capturing the activities and expectations of local patient populations. Further research is also needed to determine the responsiveness of the new score in measuring changes in response to TKA. Such evaluation involves longitudinal followup of the same cohort of patents and is currently underway.
Acknowledgments
The authors warmly acknowledge the contributions of Richard S. Laskin MD (deceased) to the work of The Knee Society Task Force. They also acknowledge the technical assistance of Dr Michael Conditt, Mr Uche Osadebe, Dr Maureen Dwyer, Mr Sabir Ismaily, Mr Prem Ramkumar, Mr Paul Newhouse, Mr Eugene Stone, and Ms Denise Leon in preparing the manuscript and in performing background studies in support of this work and Dianne Bryant, PhD, and Bert Chesworth, PhD, for their contributions relating to epidemiologic aspects of the study. The authors acknowledge the work of the following members of The Knee Society in contributing patients to the field evaluation of the new Knee Society Score: Keith Berend, MD; Dan Berry, MD; Kim Bertin, MD; Kevin Bozic, MD; David Dalury, MD; Terence Gioe, MD; Arlen Hanssen, MD; Steve Incavo, MD; Carlos Lavernia, MD; David Lewallen, MD; Adolph Lombardi, MD; Bassam Masri, MD; Michael Mont, MD; Mark Pagnano, MD; Michael Reis, MD; Jay Rodrigo, MD; Tad Vail, MD; and Ray Wasielewski, MD. The authors are also indebted to Dr Gerald Engh, who, as President of The Knee Society, appointed the task force to develop a new Knee Society Score, and Ms Olga Foley for organizing its meetings and activities.
Appendix 1
Methodologies for Assessment of the Validity and Reliability of the Subscale Measures
The reliability and validity of the prototype instrument were assessed using classical test theory and item response theory (IRT) methods described below. These analyses were performed for the objective subscale and for each subscale of subjective measures (satisfaction, expectation, and functional activities subscales: walking and standing, standard activities, advanced activities, and discretionary activities).
Classical Test Theory Methods
Validity
The validity assessment aims at the evaluation of the systematic component of the error of measurement, which is the difference between the unobserved true score of an individual and the computed score from the instrument. Content validity reflects the adequacy of the instrument with respect to the trait being measured and is achieved by the involvement of subject matter expert in the generation and refinement of items. Factor analyses establish dimensionality of the underlying trait, that is, determine whether a single subscale score is an adequate summary of the trait. In this study, we employed exploratory factor analysis for categorical indicators since the item responses were categorical and not treated as continuous. The exploratory factor analysis assessed the dimensions into which the prototype items tap and was implemented in Mplus software (Muthen and Muthen, Los Angeles, CA, USA). Convergent validity was established by evaluating the associations between the measure under investigation and other measures of the same or related constructs. In this study, the new Knee Society Score was correlated to the individual subscales of the SF-12 (physical and mental component scores) and the Knee Injury and Osteoarthritis Score (pain, symptoms, activities of daily living, sport/recreation, quality of life).
Reliability
Methods for assessment of reliability deal with random error and include evaluation of the internal consistency reliability (Cronbach’s alpha) [12]. Values above 0.7 or 0.8 are preferred for group level measurement [44].
IRT Model
IRT analyses were used to assess the properties of items and their coverage of the underlying trait. IRT models evaluate whether a set of items can be used to measure, indirectly, a trait of interest, such as expectation, satisfaction, or activities performed by an individual. Each item in the instrument has a set of numerical values called item parameters. Ideally, the items should be chosen so that their range of difficulty covers the potential range of the trait but with small-enough increments to be able to discriminate between different levels of the trait. In other words, if the instrument is designed to measure satisfaction in the population of patients that include those who are highly satisfied and highly unsatisfied, items should be present that capture both ends of the range and the levels in between. Further, when two or more items have approximately the same location parameters, they are redundant. In this case, the item providing the highest discrimination could be kept to minimize the burden placed on respondents while preserving the measurement properties of the instrument itself. For each of the one-dimensional subscales established using factor analyses, the location and discrimination parameters of each item were evaluated using Samejima’s graded response model [10, 19, 48].
Differential Item Functioning (DIF)
In terms of IRT modeling, DIF testing stems from the requirement that item parameters are properties of items and not properties of patients who respond to these items. DIF is also known as item bias, and it occurs when there are no differences in the underlying trait between groups of patients, for example, males and females, but responses to a particular item differ between the two sexes. When this happens, the validity of measurement is jeopardized since the item measures sex and not the underlying trait. The logistic regression method of DIF testing was implemented in this study. Nonuniform DIF (ie, DIF with varying direction across levels of the trait) is present if the interaction term is significant. Comparison of models with summed score only and summed score and group yields a test for uniform DIF. The DIF analyses were carried out in two stages: initially with all items and then after censoring any items exhibiting DIF on the initial run [43]. Logistic regression analyses were performed using SAS® Version 9.2 (SAS Institute Inc, Cary, NC, USA). Since DIF analyses involved running multiple logistic regression models and multiple tests, the Benjamini-Hochberg procedure was used to control the false discovery rate [5].
Appendix 2
The New Knee Society Score: Domains and Point Allocations
Objective Knee Score (seven items; 100 points):
AP alignment (25 points)
Stability (25 points)
Medial/lateral (15 points)
Anterior/posterior (10 points)
ROM (25 points)
Symptoms (25 points)
Deductions
Malalignment (−10 points)
Flexion contracture (−2/−5/−10/−15 points)
Extensor lag (−5/−10/−15 points)
Satisfaction Score (five items; 40 points):
Pain level while sitting (8 points)
Pain level while lying in bed (8 points)
Knee function while getting out of bed (8 points)
Knee function while performing light household duties (8 points)
Knee function while performing leisure recreational activities (8 points)
Expectation Score (three items; 15 points):
Pain relief (5 points)
Ability to carry out activities of daily living (5 points)
Ability to perform leisure, recreational, or sport activities (5 points)
Functional Activity Score (19 items; 100 points):
Walking and standing (five items; 30 points)
Standard activities (six items; 30 points)
Advanced activities (five items; 25 points)
Discretionary activities (three items; 15 points)
Footnotes
The institution of one or more of the authors (RBB, PCN) has received, in any 1 year, funding from The Knee Society. P. C. Noble certifies that he has consultancies in Zimmer Inc (Warsaw, IN, USA). G. R. Scuderi certifies that he has consultancies in Zimmer Inc and Salient Surgical Technologies (Portsmouth, NH, USA). J. H. Lonner certifies that he has consultancies in Zimmer Inc. W. N. Scott certifies he received royalties from Zimmer Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work reflects the efforts of a task force of The Knee Society.
References
- 1.Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty. 1996;11:831–840. doi: 10.1016/S0883-5403(96)80183-5. [DOI] [PubMed] [Google Scholar]
- 2.Ayers DC, Franklin PD, Ploutz-Snyder R, Boisvert CB. Total knee replacement outcome and coexisting physical and emotional illness. Clin Orthop Relat Res. 2005;440:157–161. doi: 10.1097/01.blo.0000185447.43622.93. [DOI] [PubMed] [Google Scholar]
- 3.Bach CM, Nogler M, Steingruber IE, Ogon M, Wimmer C, Göbel G, Krismer M. Scoring systems in total knee arthroplasty. Clin Orthop Relat Res. 2002;399:184–196. doi: 10.1097/00003086-200206000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Bayley KB, London MR, Grunkemeier GL, Lansky DJ. Measuring the success of treatment in patient terms. Med Care. 1995;33:AS226–AS235. [PubMed] [Google Scholar]
- 5.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 6.Bourne RB. Measuring tools for functional outcomes in total knee arthroplasty. Clin Orthop Relat Res. 2008;466:2634–2638. doi: 10.1007/s11999-008-0468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourne RB, Maloney WJ, Wright JG. An AOA critical issue: the outcome of the outcomes movement. J Bone Joint Surg Am. 2004;86:633–640. doi: 10.2106/00004623-200403000-00026. [DOI] [PubMed] [Google Scholar]
- 9.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271:1349–1357. doi: 10.1001/jama.1994.03510410061034. [DOI] [PubMed] [Google Scholar]
- 10.Chang CH, Reeve BB. Item response theory and its applications to patient-reported outcomes measurement. Eval Health Prof. 2005;28:264–282. doi: 10.1177/0163278705278275. [DOI] [PubMed] [Google Scholar]
- 11.Chesworth BM, Mahomed NN, Bourne RB, Davis AM. Willingness to go through surgery again validated WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol. 2008;61:907–918. doi: 10.1016/j.jclinepi.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrica. 1951;16:297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- 13.Davies AP. Rating systems for total knee replacement. Knee. 2002;9:261–266. doi: 10.1016/S0968-0160(02)00095-9. [DOI] [PubMed] [Google Scholar]
- 14.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 15.Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty: results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83:339–344. doi: 10.1302/0301-620X.83B3.11134. [DOI] [PubMed] [Google Scholar]
- 16.Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award. Functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–2604. doi: 10.1007/s11999-008-0428-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandhi R, Davey JR, Mahomed NN. Predicting patient dissatisfaction following joint replacement surgery. J Rheumatol. 2008;35:2415–2418. doi: 10.3899/jrheum.080295. [DOI] [PubMed] [Google Scholar]
- 18.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Hays RD, Morales LS, Reise SP. Item response theory and health outcomes measurement in the 21st century. Med Care. 2000;38:II28–II42. doi: 10.1097/00005650-200009002-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:2245–2252. doi: 10.2106/JBJS.H.00274. [DOI] [PubMed] [Google Scholar]
- 21.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998;356:93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Impellizzeri FM, Mannion AF, Leunig M, Bizzini M, Naal FD. Comparison of the reliability, responsiveness, and construct validity of 4 different questionnaires for evaluating outcomes after total knee arthroplasty. J Arthroplasty. 2011;26:861–869. doi: 10.1016/j.arth.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 23.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society Clinical Rating System. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 24.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 25.Janse AJ, Gemke RJBJ, Uiterwaal CSPM, Tweel I, Kimpen JL, Sinnema G. Quality of life: patients and doctors don’t always agree: a meta-analysis. J Clin Epidemiol. 2004;57:653–661. doi: 10.1016/j.jclinepi.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Kline P, Auld F, Cooper C. Five new personality scales: their location in the factor space of personality measures. J Clin Psychol. 1987;43:328–336. doi: 10.1002/1097-4679(198705)43:3<328::AID-JCLP2270430305>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 27.Kline P, Cooper C. A factorial analysis of the authoritarian personality. Br J Psychol. 1984;75:171–176. doi: 10.1111/j.2044-8295.1984.tb01888.x. [DOI] [Google Scholar]
- 28.Konig A, Scheidler M, Rader C, Eulert J. The need for a dual rating system in total knee arthroplasty. Clin Orthop Relat Res. 1997;345:161–167. [PubMed] [Google Scholar]
- 29.Kreibich DN, Vaz M, Bourne RB, Rorabeck CH, Kim P, Hardie R, Kramer J, Kirkley A. What is the best way of assessing outcome after total knee replacement? Clin Orthop Relat Res. 1996;331:221–225. doi: 10.1097/00003086-199610000-00031. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K. Studying symptoms: sampling and measurement issues. Ann Intern Med. 2001;134:844–853. doi: 10.7326/0003-4819-134-9_part_2-200105011-00008. [DOI] [PubMed] [Google Scholar]
- 31.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 32.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB. Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83:1856–1864. doi: 10.2106/00004623-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 35.Mahomed NN, Sledge CB, Daltroy LH, Fossel AH, Katz JN. Self-administered satisfaction scale for joint replacement arthroplasty. J Bone Joint Surg Br. 1998;80:9. [Google Scholar]
- 36.Mancuso CA, Graziano S, Briskie LM, Peterson MG, Pellicci PM, Salvati EA, Sculco TP. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466:424–431. doi: 10.1007/s11999-007-0052-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RF, Williams-Russo P. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83:1005–1012. doi: 10.1302/0301-620X.83B7.12105. [DOI] [PubMed] [Google Scholar]
- 38.Mäntyselkä P, Kumpusalo E, Ahonen R, Takala J. Patients’ versus general practitioners’ assessments of pain intensity in primary care patients with non-cancer pain. Br J Gen Pract. 2001;51:995–997. [PMC free article] [PubMed] [Google Scholar]
- 39.Mont MA, Marker DR, Seyler TM, Jones LC, Kolisek FR, Hungerford DS. High-impact sports after total knee arthroplasty. J Arthroplasty. 2008;23:80–84. doi: 10.1016/j.arth.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 40.Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80:55–61. doi: 10.1080/17453670902805007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award. Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 42.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 43.Orlando M, Thissen D. Likelihood-based item-fit indices for dichotomous item response theory models. Appl Psychol Meas. 2002;24:50–64. doi: 10.1177/01466216000241003. [DOI] [Google Scholar]
- 44.Reeve BB, Hays RD, Bjorner J. Psychometric evaluation and calibration of health-related quality of life item banks. Med Care. 2007;45:S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 45.Robertsson O, Dunbar MJ. Patient satisfaction compared with general health and disease-specific questionnaires in knee arthroplasty patients. J Arthroplasty. 2001;16:476–482. doi: 10.1054/arth.2001.22395a. [DOI] [PubMed] [Google Scholar]
- 46.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 47.Roos EM, Toksvig-Larsen S. Knee Injury and Osteoarthritis Outcome Score (KOOS)— validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Samejima F. Handbook of Modern Item Response Theory. New York, NY: Springer; 1997. p. 49. [Google Scholar]
- 49.Schmalzried TP, Szuszczewicz ES, Northfield MR, Akizuki KH, Frankel RE, Belcher G, Amstutz HC. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–59. doi: 10.1302/0301-620X.80B1.7739. [DOI] [PubMed] [Google Scholar]
- 50.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The New Knee Society Knee Scoring System. Clin Orthop Relat Res. 2011. DOI:10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed]
- 51.Swanson EA, Schmalzried TP, Dorey FJ. Activity recommendations after total hip and knee arthroplasty: a survey of the American Association for Hip and Knee Surgeons. J Arthroplasty. 2009;24:120–126. doi: 10.1016/j.arth.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 52.The Knee Society. Outcomes assessment. Available at: https:\\www.kneesociety.org/web/outcomes.html. Accessed October 4, 2011.
- 53.US Food and Drug Administration. Patient-reported outcome measures: use in medical product development to support labeling claims. 2009. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071975.pdf. Accessed October 4, 2011.
- 54.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 55.Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;404:172–188. doi: 10.1097/00003086-200211000-00030. [DOI] [PubMed] [Google Scholar]
- 56.Wright JG. Evaluating the outcome of treatment: shouldn’t we be asking patients if they are better? J Clin Epidemiol. 2000;53:549–553. doi: 10.1016/S0895-4356(99)00225-5. [DOI] [PubMed] [Google Scholar]
- 57.Wright JG, Young NL. The patient-specific index: asking patients what they want. J Bone Joint Surg Am. 1997;79:974–983. doi: 10.2106/00004623-199707000-00003. [DOI] [PubMed] [Google Scholar]
- 58.Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br. 2008;90:1172–1179. doi: 10.1302/0301-620X.90B9.21031. [DOI] [PubMed] [Google Scholar]