Abstract
Background
Early studies in the literature reported relatively high early minor reintervention rate for the mobile-bearing unilateral knee arthroplasty (UKA) compared with short- and midterm survivorship after fixed- or mobile-bearing UKA. However, whether the long-term function and survivorship are similar is unclear.
Questions/purposes
We therefore asked whether (1) mobile- or fixed-bearing UKAs have comparable function (as measured by the Knee Society scores); (2) mobile- and fixed-bearing UKA have comparable Knee Society radiographic scores; and (3) the long-term survivorship is comparable.
Methods
We retrospectively reviewed 75 patients (79 knees) with a fixed-bearing UKA and 72 patients (77 knees) with a mobile-bearing UKA operated on between 1989 and 1992. Mean age of the patients was 63 years; gender and body mass index (26 kg/m2) were comparable in the two groups. We obtained Knee Society function and radiographic scores and determined survival. The minimum followup was 15 years (mean, 17.2 ± 4.8 years; range, 15–21.2 years).
Results
The mean Knee Society function and knee scores were comparable in the two groups. Radiographically, the number of overcorrections and the number of radiolucencies were statistically higher in the mobile-bearing group (69% versus 24%). At final followup, considering revision for any reason, 12 of 77 (15%) UKAs were revised (for aseptic loosening, dislocation, and arthritis progression) in the mobile-bearing group and 10 of 79 (12%) in the fixed-bearing group (for wear and arthritis progression).
Conclusions
This long-term study did not demonstrate any difference in survivorship between fixed and mobile-bearing but pointed out specific modes of failure.
Level of Evidence
Level III, comparative study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Unilateral knee arthroplasty (UKA) is a bone and ligament-sparing technique that reliably restores knee kinematics and function for arthritis limited to one compartment of the knee [2, 3, 25, 30]. Function and survivorship after UKA improved since its introduction more than 30 years ago as a result of improvements in designs, indications, materials, and surgical techniques [17, 36]. Reported function and survivorship of UKA are better when the anterior cruciate ligament is intact [3, 6] and kinematic studies suggested that maintaining the anterior cruciate ligament may be advantageous in terms of survivorship, stairclimbing ability, patient satisfaction, and joint kinematics [3, 6, 7, 25, 31]. Historically, the first available UKAs were cemented fixed-bearing all-polyethylene UKA [17]. In 1986, Goodfellow and O’Connor described a mobile-bearing metal-backed UKA designed to improve wear characteristic in UKA [15]. They suggested the potential advantage of the mobile-bearing design allowed a more conformed surface than with a fixed-bearing UKA and therefore larger contact areas and lower contact stresses, which would theoretically improve wear characteristics [15]. One early retrieval studies supported this notion by showing low wear rates with this fully conforming mobile-bearing UKA [4]. Precise alignment and ligament balancing are, however, essential to prevent mobile-bearing dislocation or impingement and to avoid overcorrection, which may lead to rapid progression of arthritis in the opposite compartment [7, 15, 41].
On the other hand, fixed-bearing UKAs often have a flat tibial articular surface, which is less conforming as flexion occurs and might lead to point loading [5]. Earlier studies comparing the reintervention rate [8] and the short- and midterm survivorship [9, 11, 41] after fixed- or mobile-bearing UKA suggested a higher early minor reintervention rate for the mobile-bearing UKA [8]. However, whether the long-term function and survivorship are similar is unclear.
We therefore asked whether (1) mobile- or fixed-bearing UKAs have comparable function (as measured by the Knee Society scores); (2) mobile- and fixed-bearing UKA have comparable Knee Society radiographic scores; and (3) the long-term survivorship is comparable.
Material and Methods
We retrospectively reviewed all 156 knees in 147 patients operated on between 1989 and 1992 with either a fixed-bearing (Miller-Galante; Zimmer, Warsaw, IN) or mobile-bearing design (Oxford meniscal-bearing; Biomet, Warsaw, IN) for medial unicompartmental arthritis of the knee. One of the authors (JMA) began implanting UKAs in 1970 using different types of early UKA designs and another author (JNA) in 1985. Both surgeons had more than 100-case experience using either fixed or mobile-bearing designs prior to the timeframe chosen; during this period, the senior authors were using either fixed- or mobile-bearing cemented UKA. Seventy-five patients (79 knees) received a Miller-Galante fixed-bearing prosthesis and seventy-two patients (77 knees) an Oxford mobile-bearing prosthesis performed by the two senior authors (JMA, JNA). All prostheses were cemented. The indications for the procedure were a confirmed diagnosis of unicompartmental osteoarthritis (Ahlback [1] Grade 2 or greater) with a full-thickness of the articular cartilage in the lateral compartment and a preserved status of the patellofemoral joint (based on clinical evaluation and sky-view radiographs), a preoperative range of knee flexion greater than 100º associated with a full range of knee extension or at least a flexion contracture lower than 10° degrees, and a knee clinically stable in the frontal and sagittal planes. Particular care was given to clinical testing of the ACL. The contraindications included a flexion contracture greater than 10°, chondrocalcinosis (with repeated effusion), and a valgus or varus deformity greater than 10° as measured on long-leg radiographs. Varus and valgus stress radiographs were also performed to evaluate the lateral compartment and the correction of the deformities [13]. A painful narrowing up to 50% of the cartilage on the lateral compartment or a fixed deformity observed on the stress radiograph was considered a contraindication. In both groups, the study inclusion criteria were a primary medial UKA and a minimum clinical followup of 15 years. We excluded five patients who had a medial UKA from 1989 and 1992 with a concurrent high tibial osteotomy, a concurrent or previous ACL reconstruction, or a revision arthroplasty. During the study period, 543 TKAs have been performed, 10 lateral UKAs, and 48 associations of either a medial or a lateral UKA and a patellofemoral arthroplasty.
The decision to use either a fixed- or a mobile-bearing UKA was neither randomized nor chosen because of patient characteristics but rather related to the availability of the implants and equipment. Eleven patients in the fixed-bearing group (at a mean of 12.4 years postoperatively) and 16 in the mobile-bearing group (at a mean of 14.45 years) died before the final review, but data were available from the last followup before their death (1 year before) and we used these data for the final analysis. Six patients were lost to followup in the fixed-bearing group; thus, 73 knees in 69 patients were available for the final analysis in this group. Five patients were lost to followup in the mobile-bearing group; thus, 72 knees in 67 patients were available for the final analysis. The minimum followup was 15 years (mean, 17.2 ± 4.8 years; range, 15–21.2 years). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
The characteristics of the patients were comparable in the two groups (Table 1).
Table 1.
Age at the time of surgery, body mass index, gender of the patients, side of the knees, the etiologies of the osteoarthritis, and the grade of arthritis were comparable in the two groups
| Characteristic of the population | Fixed-bearing group | Mobile-bearing group |
|---|---|---|
| Total number of UKAs | 79 knees | 77 knees |
| Age (mean ± SD) [confidence interval] |
62.8 ± 9.2 [61.8–64.0] |
63.4 ± 11 [61.1–64.7] |
| Gender (male:female) [percentage] |
29:50 [26.1%–47.3%] |
25:52 [22%–43%] |
| Body mass index (mean ± SD) [confidence interval] |
26 kg/m2 ± 4 [24.9–26.2] |
27 kg/m2 ± 3 [26.1–27.6] |
| Side (left:right) | 35:44 | 38:39 |
| Etiology | ||
| OA | 65 | 70 |
| Posttraumatic arthritis | 10 | 6 |
| AVN | 4 | 1 |
| Ahlback [1] grade | ||
| Grade 2 | 4 | 6 |
| Grade 3 | 75 | 71 |
UKAs = unilateral knee arthroplasties; SD = standard deviation; OA = osteoarthritis; AVN = avascular osteonecrosis.
A standard medial parapatellar approach was performed for all knees in both groups [2]. In the fixed-bearing group, a Miller-Galante UKA (Zimmer) was systematically used and performed with modern dedicated instrumentation, including tibial and femoral cutting guides [2]. The only mobile-bearing design used was the Oxford prosthesis with a spherical articular surface. The surgical goal was to perform a resurfacing arthroplasty without any ligament release in both groups. In the fixed-bearing group, a 2-mm laxity during the valgus stress at 20° of flexion at the end of the procedure was the goal. In the mobile-bearing group, the goal was to obtain no laxity during the valgus stress at 20° of flexion at the end of the procedure. Postoperative rehabilitation protocols included immediate weightbearing protected by crutches during the first 2 or 3 weeks according to patient tolerance and exercises were focused on passive flexion immediately and then active recuperation of flexion and extension. All patients in the present study received routine prophylaxis with low-molecular-weight heparin pre- and postoperatively for 21 days.
All patients were evaluated clinically preoperatively, at 3 months postoperatively, at yearly intervals postoperatively, and at last followup by one of two independent observers (MCB, SP) using the Knee Society knee and function score [18]. The arc of knee flexion was recorded preoperatively, during followup, and at the final evaluation. Radiographic evaluation was performed by one observer (SP) on long-leg radiographs and on AP, lateral, and skyline radiographs of the knee at last followup. All the radiographs were aligned with fluoroscopic control to obtain views parallel to the tibial tray to reveal the tibial bone-implant interface. The lower-limb alignment was assessed on long-leg radiographs performed using a standardized protocol in which the patient stood with the patella facing anteriorly pre- and postoperatively. On these long-leg radiographs, pre- and postoperatively, the femoral angle (CH = condylar axis to hip center), the tibial angle (PA = plateau axis to ankle), and the articular deformation (CP = condylar axis and plateau axis) were calculated [10]. At final followup, alignment was classified according to the Kennedy classification, which considers the alignment correct when the mechanical axis is in Zone 2 or C (central) and considered as too much in varus when in Zone 1 and too much in valgus when in Zone 3 [20]. The presence, extent, or progression of femoral, tibial radiolucencies was analyzed on full tangential AP and lateral radiographs and subdivided into two distinct subtypes [16]. First the well-defined 1-mm to 2-mm thick radiolucencies (with parallel running radiodense lines) were described as physiological radiolucencies and defined as a radiolucent line [16]. Second, the progressive, poorly defined is greater than 2-mm thick radiolucencies without any matching radiodense line defined as pathologic radiolucency and considered as indicating aseptic loosening [16]. The Ahlback classification was used to evaluate the osteoarthritis progression in the medial or patellofemoral compartment [1].
A descriptive report of the radiographic outcomes was performed using means and SDs to describe pre- and postoperative alignment and the alignment of the mechanical axis according to the classification of Kennedy and White [20] as well as the number of radiolucencies in each group were compared using Fisher’s exact test [32]. Finally, the 20-year survival analysis was performed using the Kaplan-Meier technique (with 95% confidence intervals) for all patients considering revision for any reason or radiographic loosening as the end point. The impact of nonprogressive radiolucent lines on the survivorship using the Kaplan-Meier technique was also evaluated in the two groups. The survivorship comparison was also performed after exclusion of the overcorrected patients [19]. We also performed Cox model analysis to compare the relative risk of being revised in each group at 5, 10, 15, and 20 years [32]. Analysis was performed using SPSS software (Version 12; SPSS Inc, Chicago, IL). All calculations assumed two-tailed tests.
Results
Function as measured by the Knee Society Function and Knee score was comparable in the two groups at a minimum followup of 15 years (mean, 17.2 ± 4.8 years; range, 15–21.2 years) (Table 2). The mean active knee flexion improved from 120° ± 7º (range, 100°–150º) preoperatively to 129º ± 4º (range, 115º–150º) at final followup in the fixed-bearing group and from 115° ± 8º (range, 105°–145º) to 127º ± 6º (range, 110º–145º) in the mobile-bearing group without any difference (p = 0.85) between the two groups.
Table 2.
The clinical outcomes according to the Knee Society knee and function scores were comparable in the two groups
| Group | Knee Society knee score | Knee Society function score | ||
|---|---|---|---|---|
| Mean preoperative score (SD; range) | Mean score at last followup (SD; range) | Mean preoperative score (SD; range) | Mean score at last followup (SD; range) | |
| Fixed-bearing group | 52 (8; 21–66) | 82 (2; 55–100) (n = 66/73) |
60 (70; 22–74) | 88 (2; 60–100) (n = 66/73) |
| Mobile-bearing group | 49 (4; 22–70) | 81 (2; 66–100) (n = 64/73) |
57 (3; 37–75) | 89 (5; 75–100) (n = 64/73) |
| p | 0.70 | 0.84 | 0.60 | 0.82 |
n represents the number of patient with complete data at final followup for the Knee Society Function and Knee scores; SD = standard deviation.
The mean preoperative hip-knee angle (HKA) was 173° (range, 168°–179°) in the fixed-bearing group and 174° (range, 169°–179°) in the mobile-bearing group with no difference (p = 0.068) between the two groups. At last followup, the mean HKA was similar in the two groups: 177° ± 6º (range, 175°–181°) in the fixed-bearing group and 179° ± 7º (range, 176°–184°) in the mobile-bearing group. We found more knees with a neutral or valgus axis for the patients in the mobile-bearing group (Table 3). The mean AP axis of the tibial component was comparable in the two groups: 88º ± 5º (range, 85°–91º) as well as the mean tibial slope: 4º ± 3º (range, 0°–8º) and as well as the mean AP femoral axis (93º ± 7º; range, 85º–93º). Radiographically, the number of radiolucent lines was higher (p = 0.001) in the mobile-bearing group than in the fixed-bearing group (69% versus 24%) (Fig. 1).
Table 3.
The restoration of the mechanical axis was also analyzed at final followup according to the Kennedy and White [20] classification, which considers the alignment correct when the mechanical axis is in Zone 2 or C (central) and considered as too much in varus when in Zone 1 and too much in valgus when in Zone 3
| Kennedy classification | Fixed-bearing group Number (%) | Mobile-bearing group Number (%) | p |
|---|---|---|---|
| Kennedy 1 | 4 (5.5%) | 1 (1.5%) | 0.0003 |
| Kennedy 2 | 55 (73%) | 33 (44%) | 0.024 |
| Kennedy C | 15 (20%) | 35 (46.5%) | 0.0038 |
| Kennedy 3 | 1 (1.5%) | 6 (8%) | 0.00014 |
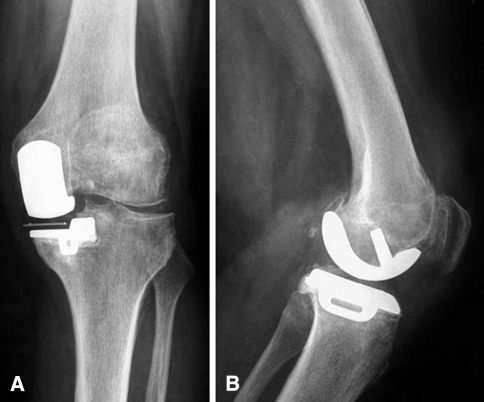
Fig. 1A–B.
This illustrations show an AP view (A) and a mediolateral view (B) of a mobile-bearing unilateral knee arthroplasty (UKA) at final followup with a radiolucent line under the tibial plateau without any sign of clinical or radiologic subsidence.
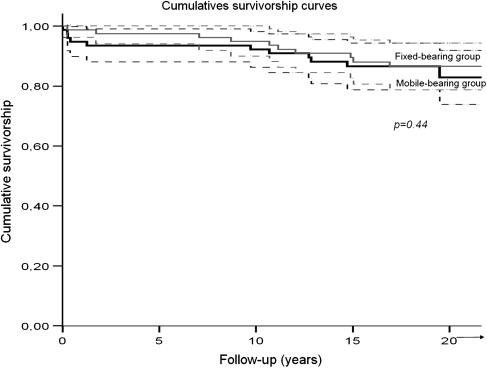
We found no difference in survival (p = 0.44) between the two groups (Fig. 2). Considering revision for any reason as the end point, 20-year survivorship was 0.83 (95% confidence interval, 0.74–0.92) in the fixed-bearing group with 10 patients revised for wear and/or arthritis progression (Table 4). Considering revision for any reason as the end point, the 20-year survivorship was 0.8 (95% confidence interval, 0.81–0.95) in the mobile-bearing group with 12 patients revised for aseptic loosening, dislocation, or arthritis progression (Table 4). The main reason for revision in the fixed-bearing group was polyethylene wear at a mean of 8.9 years treated with direct liner exchange (Fig. 3), whereas the main cause of revision in the mobile-bearing group was progression of osteoarthritis in five cases at a mean of 7.1 years. Within these five cases, three had early progression of osteoarthritis in the lateral compartment at a mean of 3.9 years related to overcorrection of the deformation. We found no difference in survival (p = 0.33) in the two groups for the patients with or without radiolucent lines. No difference of survivorship was found between the two groups after exclusion of the overcorrected patients (p = 0.735).
Fig. 2.
Kaplan-Meier survivorship analysis curves are shown. Considering revision for any reason as the end point, 20-year survivorship was 0.83 (95% confidence interval, 0.74–0.92) in the fixed-bearing group with 10 patients revised for wear and/or arthritis progression. Considering revision for any reason as the end point, the 20-year survivorship was 0.8 (95% confidence interval, 0.81–0.95) in the mobile-bearing group with 12 patients revised for aseptic loosening, dislocation, or arthritis progression. The log-rank test demonstrated no difference (p = 0.44) between the two groups.
Table 4.
Unicompartmental arthroplasty revision details, followup, and outcomes
| Reason for revision | Number of knees | Mean time to revision (years) | Type of revision | Followup (years) | Mean Knee Society score (knee/function) |
|---|---|---|---|---|---|
| Fixed-bearing group | |||||
| Progression of arthritis | 3 | 10 | Add PFA: 2 Add lateral UKA: 1 | Mean 9.7 | (84/82) |
| Aseptic loosening | 2 | 14.6 | Conversion to TKA: 2 | Mean 6.3 | (80/75) |
| Polyethylene wear | 4 | 8.9 | PE exchange: 4 | Mean 12.4 | (85/86) |
| Bearing dislocation | 0 | – | – | – | – |
| Septic loosening | 1 | 0.25 | Conversion to TKA after spacer | Mean 17 | (72/70) |
| Total | 10 | 8.43 | – | 11.35 | (80/78) |
| Mobile-bearing group | |||||
| Progression of arthritis | 5 | 7.1 | Conversion to TKA: 5 | Latest 12.8 | (84/75) |
| Aseptic loosening | 3 | 17.7 | Conversion to TKA: 3 | Latest 3.8 | (85/78) |
| Polyethylene wear | 0 | – | – | – | – |
| Bearing dislocation | 3 | 0.44 | Conversion to TKA: 3 | Latest 18.7 | (77/70) |
| Septic loosening | 1 | 12.9 | Conversion to TKA after spacer | Latest 5.8 | (60/50) |
| Total | 12 | 8.5 | – | 10.3 | (77/68) |
PFA = patellofemoral arthroplasty; UKA = unilateral knee arthroplasty; PE = polyethylene.
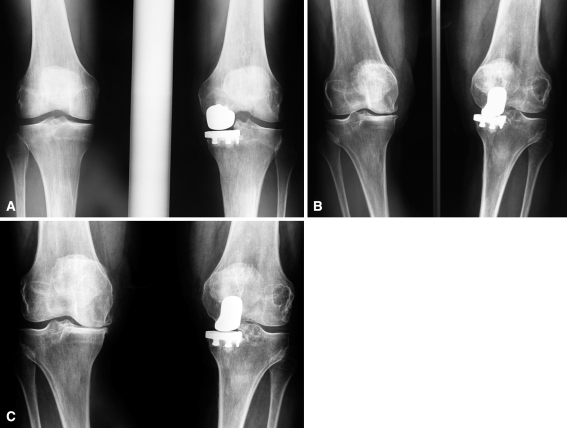
Fig. 3A–C.
This figure shows an AP view of a well-functioning left unilateral knee arthroplasty (UKA) 7 years after implantation (A). The patient presented with a painful knee at the 12-year followup with signs of complete polyethylene wear (B). The patient underwent an isolated liner exchange in 2002. In 2010, the AP radiographs (C) show stable evolution on the left knee and she is now requesting surgery on her right knee.
At 5 years, the relative risk for being revised was similar (relative risk, 0.382; 95% confidence interval, 0.0074–1.967; p = 0.25) compared with the mobile-bearing group as well as at 10 years: 0.639 (95% confidence interval, 0.180–2.26; p = 0.488), at 15 years: 0.763 (0.301–1.934; p = 0.569), and at 20 years: 0.837 (0.360–1.945; p = 0.679).
Discussion
Arthroplasty registries [22–24, 34, 35] comparing fixed- and mobile-bearing designs of UKA suggested no conclusive advantage of one bearing design over another with some authors citing differing reasons for the failure of each design [22–24, 34, 35, 37, 41]. Higher early minor reintervention rates for the mobile-bearing UKA were reported [7, 8, 11, 41]. Comparative studies did not find any differences in terms of survivorship; however, the followup was limited [7, 8, 11, 25, 41]. Our goal was therefore to compare the long-term function and survivorship of fixed- and mobile-bearing UKA. We therefore asked whether (1) mobile- or fixed-bearing UKAs have comparable function (as measured by the Knee Society scores); (2) mobile- and fixed-bearing UKA have comparable Knee Society radiographic scores; and (3) the long-term survivorship is comparable.
Some limitations should be noted. First, our study was retrospective with the attendant risk of selection bias. Second, we were unable to compare the functional improvement as measured using contemporary evaluation tools such as a specific quality-of life questionnaire (such as the WOMAC score or the Knee Osteoarthritis Outcomes Score) [29, 41]. These scores were not available in our institution at the time of the preoperative screening of the patients [29, 41]. Third, the radiographs were not subjected to review by multiple blinded observers, which can lead to an analysis bias related to potential inter- and intraobserver error [32]. Despite these limitations, we report a comparative study of two comparable groups of patients with a long-term followup operated on in the same department by the two senior authors.
The Knee Society scores [18] were comparable in the two groups and comparable with the function scores reported in the literature with excellent pain relief in the treatment of the medial compartment arthritis (Table 5) [7, 9, 11, 25, 38, 41]. In vivo kinematic studies suggest patients implanted with fixed-bearing UKA have kinematics close to the normal knee despite some cases of paradoxical anterior translation seen over time [3]. In vivo kinematic studies failed to demonstrate kinematic advantages of mobile-bearing over fixed-bearing in UKA [25], probably related to the fact that both cruciates are present in UKA [21, 25, 38].
Table 5.
Results of the different series comparing fixed- and mobile-bearing unicompartmental arthroplasty in the literature
| Authors | Date of publication | Number of implants (fixed/mobile) | Methods of evaluation | Clinical results Fixed/mobile | Followup mean years (minimum to maximum) | Survivorship (number of revisions) |
|---|---|---|---|---|---|---|
| Emerson et al. [11] | 2002 | 51 | Clinic and radiographic | KSKS = 89/92 pts | 6.1 | FB: 92% at 11 years |
| 50 | KSFS = 74/82 pts | (6 months to 13 years) | MB: 92% at 11 years | |||
| Confalonieri et al. [9] | 2004 | 20 | Clinic and radiographic | KSKS = 87/88 pts | 5.7 years | O revision |
| 19 | KSFS = 76/77 pts | NA | ||||
| Li et al. [25] | 2006 | 28 | Clinic | KSKS = 91/89 pts | FB: 0 revision | |
| Kinematics | KSFS = 84/85 pts | |||||
| 28 | radiographic | 31.9 months | MB: 2 revisions | |||
| 7–70 months | ||||||
| Whittaker et al. [41] | 2010 | 150 | Clinic and radiographic | KSS = 169/173 pts | FB: 8.1 (1–17.8) | FB: 96% at 5 years |
| 79 | MB: 3.6 (1–11.3) | MB: 89% at 5 years | ||||
| Parratte et al. (current study) | 2011 | 79 | Clinic and radiographic | KSKS = 82/81 pts | 17.2 years | FB: 83% at 20 years |
| 77 | KSFS = 88/89 pts | 15–21.2 years | MB: 80% at 20 years |
UKA = unicompartmental arthroplasty; KSS = Knee Society score; KSKS = Knee Society Knee score; KSFS = Knee Society Function score; pts = points; NA = not applicable; FB = fixed-bearing; MB = mobile-bearing.
The number of radiolucent lines reported in our study was higher in the mobile-bearing group (69% versus 24%). All but one of the previous comparative studies between fixed and mobile studies in the literature did not compare the rate of radiolucencies [7, 9, 11, 25, 38, 41]. Li et al. [25] in a prospective comparative randomized study did find a higher rate of radiolucencies in the fixed-bearing group at 2 years with comparable clinical scores and survivorship and no longer followup [25]. The nonprogressive radiolucent lines have been described as usual in the mobile-bearing implant by the Oxford group [16] and their etiology remains unclear. One explanation might be a link between overtension of the resurfaced compartment and radiolucent lines but we are unaware of any data in the biomechanical or clinical literature to support this hypothesis. In our study, these lines were not associated with a higher revision rate. Price et al. [33] using the same mobile-bearing implant reported a 15-year survivorship rate of up to 92% with complete radiolucent lines in 96% of the cases around the tibial component and no relation between radiolucent lines and the failures [33].
We found comparable 20-year survivorship rates in the two groups and these results are consistent with the results reported in the literature (Table 5) [2, 6, 7, 11, 14, 23, 24, 26–28, 30, 33, 37, 39–41]. Discrepancies have been observed between the survivorship reported in the United Kingdom by the Oxford Group and the survivorship reported in North American patients by independent teams [12, 26, 39, 40], possibly related to the potential differences between the patients in the United Kingdom and in North America [7]. The survivorship reported in the Swedish and the Finnish Joint registry failed to demonstrate any difference between fixed- and mobile-bearing UKA [22–24, 34, 35].
We observed three bearing dislocations within the first year, consistent with those reported in the literature [38, 40, 41]. The surgeon’s fear of dislocation may lead to increase the polyethylene high and this may lead to an overcorrection of the deformation and consecutively to early arthritis progression in the lateral compartment as described in previous studies [11, 38, 40, 41]. We also observed five cases of progression of arthritis in the lateral compartment and within these five cases, three had early progression of osteoarthritis in the lateral compartment at a mean of 3.9 years related to overcorrection of the deformation. As a result of these early complications, and despite a very low wear rate in the mobile-bearing group, we found no difference in survivorship between fixed- and mobile-bearing inserts. In fact, in the fixed-bearing group, no early complication was observed and the main complication remains polyethylene wear at a mean of 8.9 years. This complication was successfully treated with direct polyethylene exchange thanks to the use of metal-backed tibial implants [5].
In conclusion, we compared the long-term function and survivorship of mobile- and fixed-bearing medial UKAs to analyze the potential benefits of each type of bearing design. We observed comparable long-term pain relief and function restoration. We found a higher rate of lucencies in the mobile-bearing group without any influence on the survivorship. In the mobile-bearing group, more early complications, potentially related to the surgical technique and the fear of dislocation, were observed such as overcorrection of the deformation leading to early arthritis progression in the lateral compartment when wear was observed in the fixed-bearing group. We found no difference in survivorship between fixed- and mobile-bearing but noted implant-specific specific modes of failure.
Acknowledgments
We thank Mina Chevrol-Benkeddache for her participation in the clinical review of the patients.
Footnotes
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
One of the authors (JNA) is a consultant for Zimmer (Warsaw, IL).
References
- 1.Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:7–72. [PubMed]
- 2.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed] [Google Scholar]
- 3.Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S. In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty. 2002;17:1049–1054. doi: 10.1054/arth.2002.34527. [DOI] [PubMed] [Google Scholar]
- 4.Argenson JN, O’Connor JJ. Polyethylene wear in meniscal knee replacement. A one to nine-year retrieval analysis of the Oxford knee. J Bone Joint Surg Br. 1992;74:228–232. doi: 10.1302/0301-620X.74B2.1544958. [DOI] [PubMed] [Google Scholar]
- 5.Argenson JN, Parratte S. The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res. 2006;452:137–142. doi: 10.1097/01.blo.0000229358.19867.60. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006. doi: 10.2106/JBJS.C.00568. [DOI] [PubMed] [Google Scholar]
- 7.Bonutti PM, Dethmers DA. Contemporary unicompartmental knee arthroplasty: fixed vs mobile bearing. J Arthroplasty. 2008;23:24–27. doi: 10.1016/j.arth.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 8.Clark M, Campbell DG, Kiss G, Dobson PJ, Lewis PL. Reintervention after mobile-bearing Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2010;468:576–580. doi: 10.1007/s11999-009-1089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Confalonieri N, Manzotti A, Pullen C. Comparison of a mobile with a fixed tibial bearing unicompartmental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee. 2004;11:357–362. doi: 10.1016/j.knee.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. doi: 10.1016/S1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 11.Emerson RH, Jr, Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res. 2002;404:62–70. doi: 10.1097/00003086-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Emerson RH, Jr, Higgins LL. Unicompartmental knee arthroplasty with the Oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am. 2008;90:118–122. doi: 10.2106/JBJS.F.00739. [DOI] [PubMed] [Google Scholar]
- 13.Gibson PH, Goodfellow JW. Stress radiography in degenerative arthritis of the knee. J Bone Joint Surg Br. 1986;68:608–609. doi: 10.1302/0301-620X.68B4.3733839. [DOI] [PubMed] [Google Scholar]
- 14.Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH. Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee. 2004;11:379–384. doi: 10.1016/j.knee.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Goodfellow JW, O’Connor J. Clinical results of the Oxford knee: surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res. 1986;205:21–42. [PubMed] [Google Scholar]
- 16.Goodfellow JW, Tibrewal SB, Sherman KP, O’Connor JJ. Unicompartmental Oxford meniscal knee arthroplasty. J Arthroplasty. 1987;2:1–9. doi: 10.1016/S0883-5403(87)80025-6. [DOI] [PubMed] [Google Scholar]
- 17.Insall J, Walker P. Unicondylar knee replacement. Clin Orthop Relat Res. 1976;120:83–85. [PubMed] [Google Scholar]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 19.Kaplan E, Meier P. Nonparametric observation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 20.Kennedy WR, White RP. Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin Orthop Relat Res. 1987;221:278–285. [PubMed] [Google Scholar]
- 21.Komistek RD, Allain J, Anderson DT, Dennis DA, Goutallier D. In vivo kinematics for subjects with and without an anterior cruciate ligament. Clin Orthop Relat Res. 2002;404:315–325. doi: 10.1097/00003086-200211000-00047. [DOI] [PubMed] [Google Scholar]
- 22.Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50, 493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79:499–507. doi: 10.1080/17453670710015490. [DOI] [PubMed] [Google Scholar]
- 23.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1, 819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–135. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 24.Lewold S, Goodman S, Knutson K, Robertsson O, Lidgren L. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis. A Swedish multicenter survival study. J Arthroplasty. 1995;10:722–731. doi: 10.1016/S0883-5403(05)80066-X. [DOI] [PubMed] [Google Scholar]
- 25.Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D. Mobile vs fixed-bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee. 2006;13:365–370. doi: 10.1016/j.knee.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80:983–989. doi: 10.1302/0301-620X.80B6.8177. [DOI] [PubMed] [Google Scholar]
- 27.Naudie D, Guerin J, Parker DA, Bourne RB, Rorabeck CH. Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Joint Surg Am. 2004;86:1931–1935. doi: 10.2106/00004623-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 28.O’Rourke MR, Gardner JJ, Callaghan JJ, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. doi: 10.1097/01.blo.0000185451.96987.aa. [DOI] [PubMed] [Google Scholar]
- 29.Ornetti P, Parratte S, Gossec L, Tavernier C, Argenson JN, Roos EM, Guillemin F, Maillefert JF. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage. 2007;16:423–428. doi: 10.1016/j.joca.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 30.Parratte S, Argenson JN, Pearce O, Pauly V, Auquier P, Aubaniac JM. Medial unicompartmental knee replacement in the under-50s. J Bone Joint Surg Br. 2009;91:351–356. doi: 10.1302/0301-620X.91B3.21588. [DOI] [PubMed] [Google Scholar]
- 31.Patil S, Colwell CW, Jr, Ezzet KA, D’Lima DD. Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Joint Surg Am. 2005;87:332–338. doi: 10.2106/JBJS.C.01467. [DOI] [PubMed] [Google Scholar]
- 32.Petrie A. Statistics in orthopaedic papers. J Bone Joint Surg Br. 2006;88:1121–1136. doi: 10.1302/0301-620X.88B9.17896. [DOI] [PubMed] [Google Scholar]
- 33.Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171–180. doi: 10.1097/00003086-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 34.Robertsson O, Knutson K, Lewold S, Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001;83:45–49. doi: 10.1302/0301-620X.83B1.10871. [DOI] [PubMed] [Google Scholar]
- 35.Robertsson O, Lidgren L. The short-term results of 3 common UKA implants during different periods in Sweden. J Arthroplasty. 2008;23:801–807. doi: 10.1016/j.arth.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Scott RD. Three decades of experience with unicompartmental knee arthroplasty: mistakes made and lessons learned. Orthopedics. 2006;29:829–831. doi: 10.3928/01477447-20060901-36. [DOI] [PubMed] [Google Scholar]
- 37.Scott RD. Mobile- versus fixed-bearing unicompartmental knee arthroplasty. Instr Course Lect. 2010;59:57–60. [PubMed] [Google Scholar]
- 38.Smith TO, Hing CB, Davies L, Donell ST. Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res. 2009;95:599–605. doi: 10.1016/j.otsr.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 39.Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br. 2001;83:191–194. doi: 10.1302/0301-620X.83B2.10966. [DOI] [PubMed] [Google Scholar]
- 40.Vorlat P, Putzeys G, Cottenie D, Isacker T, Pouliart N, Handelberg F, Casteleyn PP, Gheysen F, Verdonk R. The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:40–45. doi: 10.1007/s00167-005-0621-1. [DOI] [PubMed] [Google Scholar]
- 41.Whittaker JP, Naudie DD, McAuley JP, McCalden RW, MacDonald SJ, Bourne RB. Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin Orthop Relat Res. 2010;468:73–81. doi: 10.1007/s11999-009-0975-7. [DOI] [PMC free article] [PubMed] [Google Scholar]