Abstract
Background
Posttraumatic arthritis secondary to lateral tibial plateau fracture malunion causes pain and limited function for patients. It is sometimes technically challenging to correct malalignment in these patients with advanced arthritis using osteotomies. Lateral unicompartmental knee arthroplasty (UKA) may be an option to treat such patients.
Questions/purposes
We asked whether UKA for lateral posttraumatic osteoarthritis (1) reliably alleviates pain and improve function, (2) restores lower limb alignment, and (3) is as durable as UKA for primary lateral osteoarthritis.
Patients and Methods
We retrospectively reviewed 13 patients with lateral cemented UKA (mean age at surgery, 50.1 years) treated at two institutions between 1985 and 2007. We obtained Knee Society scores and evaluated radiographs for evidence of implant loosening or progression of arthritis in the medial compartment. Minimum followup was 3 years (mean, 10.2 years; range, 3–22.1 years).
Results
Mean Knee Society knee score improved from 51 points (range, 29–75 points) preoperatively to 88 points (range, 65–100 points) at last followup, suggesting the procedure relieved pain. Mean function score improved from 51 points (range, 10–89 points) preoperatively to 87 points (range, 35–100 points) at last followup. The mean hip-knee-ankle angle was 188° preoperatively (range, 184°–193º) and 185° (range, 183°–188°) at last followup. Prosthesis survivorship was 100% at 5 and 10 years and 80% at 15 years.
Conclusions
Despite the limited number of indications and technical considerations, our observations suggest lateral UKA is a reasonable option for treating lateral arthritis secondary to malunited fractures.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Although anatomic fracture reduction and recovery of preoperative function may be achieved after open reduction and internal fixation of tibial plateau fractures [27], relatively rapid development of posttraumatic osteoarthritis may occur. The incidence of secondary posttraumatic arthritis reportedly ranges from 26% to 74%, depending on injury severity, articular surface reduction, and the status of the meniscus [11, 17, 22]. Many of these patients are young with high functional demands yet present with severe degenerative changes, offering a challenge to surgeons. Nonoperative management is the primary treatment option; however, patients are often unable to function adequately through activity modification or bracing.
The surgical options for lateral femorotibial osteoarthritis include varus-producing osteotomies, TKA, or unicompartmental knee arthroplasty (UKA). Various tibial or femoral osteotomies can be utilized to correct valgus deformities and to direct load through the medial compartment [5, 18, 24] when loss of cartilage thickness is partial. These osteotomies result in relief of pain in 77% to 91% of patients [4, 5, 18] and restoration of function in 72% to 88% at 9.4 to 11.2 years [4, 5, 18]. In severe cases, it can be difficult, if not impossible, to correct a large intra-articular defect through an extra-articular procedure [13]. When there is full loss of cartilage in the affected compartment, osteotomy is usually no longer considered. UKA offers an alternative to TKA when the other joint compartments are preserved.
Lateral UKA for primary degenerative disease reportedly provides pain relief in 86% to 100% of patients and restoration of function in 63% to 100% at 5 to 13 years [2, 3, 25], even in relatively young patients (ie, younger than 60 years). However, in these patients, wear is a long-term concern [16]. UKA could also be considered for isolated posttraumatic lateral compartment arthritis if relief of pain, restoration of function, and durability were similar to those for patients with primary degeneration.
We therefore addressed the following questions: (1) Does UKA for lateral posttraumatic osteoarthritis reliably alleviate pain and improve function? (2) Does UKA restore lower limb alignment when performed for lateral posttraumatic osteoarthritis? (3) Is UKA performed for posttraumatic arthritis as durable as UKA performed for primary lateral osteoarthritis?
Patients and Methods
We retrospectively reviewed all 13 patients (six male, seven female) treated with an isolated lateral UKA (13 knees) for lateral compartmental arthritis secondary to tibial plateau fracture between January 1985 and December 2007 in our two institutions. The seven patients from Hôpital Sainte-Marguerite were included in a previous report of the outcomes after lateral UKA performed for all indications, but the prior study did not separately report outcomes of lateral posttraumatic arthritis [2]. During the study period, 1166 UKAs were performed at our two institutions, 155 of which were lateral UKAs. The general indications for the procedure were isolated lateral compartment arthritis associated with a loss of articular cartilage in the involved compartment of at least Grade 3 according to the Ahlback classification [1] without full-thickness articular cartilage defects in the medial compartment; a preserved patellofemoral joint (based on clinical evaluation and skyline view radiographs); and finally a stable knee in the frontal and sagittal planes. While we consider a coronal plane deformity of greater than 14° of valgus to be a contraindication for lateral UKA in an osteoarthritic population [26], patients with any degree of deformity were considered for posttraumatic UKA as long as a varus stress radiograph demonstrated reducibility of the deformity (Fig. 1). The integrity of the ACL was determined clinically and radiographically with single-leg standing AP and lateral radiographs. Anterior tibial translation of greater than 10 mm, posteromedial flattening, or hooking of the tibial spines (all indicators of ACL insufficiency) were contraindications to UKA, as was clinical evidence of medial collateral ligament deficiency [7]. Any patients undergoing associated procedures were excluded. Five patients had arthroplasty of the right knee and eight the left knee. The mean (± SD) age of the patients at the time of UKA was 50.1 ± 12.6 years (range, 25–67 years). The mean body mass index of the patients was 25 ± 3.7 kg/m2 (range, 21–30 kg/m2). According to the Ahlback classification [1], all knees were Grade 4. The initial tibial plateau injury was treated with open reduction and internal fixation in 10 patients (plate osteosynthesis with bone autograft in two patients, plate osteosynthesis with bone substitute graft in one patient, plate osteosynthesis alone in two patients, and screws alone in five patients) (Table 1). The initial injury was treated nonoperatively in three patients. The mean time from fracture to UKA was 5.1 ± 5.2 years (range, 1–18 years) (Table 1). Five patients engaged in strenuous physical activity (heavy lifting, prolonged standing or walking), while eight did not regularly engage in these activities. None of the patients was lost to followup. Minimum followup was 3 years (mean ± SD, 10.2 ± 5.7 years; range, 3–22.1 years). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Approval of the local ethical committee was obtained.
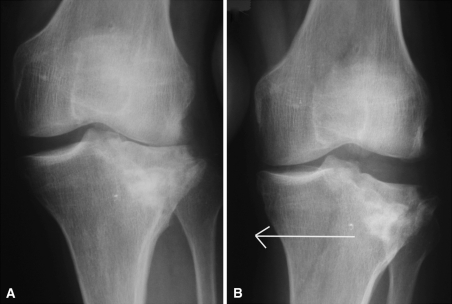
Fig. 1A–B.
(A) An AP plain radiograph of a left knee demonstrates isolated posttraumatic arthritis of the lateral compartment secondary to tibial plateau fracture malunion. A hip-knee-ankle angle of 188° was measured on full-length radiographs. (B) A varus stress view demonstrates complete correction of the valgus deformity. The arrow demonstrates the direction of stress.
Table 1.
Patient demographics
| Patient | Gender | Side | Body mass index (kg/m2) | Age at fracture (years) | Type of fracture (Schatzker) | Fracture management | Age at UKA (years) | Time between fracture and UKA (years) |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | Left | 22 | 50 | 3 | Plate | 53 | 3 |
| 2 | Male | Right | 24 | 37 | 1 | Screws | 42 | 5 |
| 3 | Male | Right | 21 | 55 | 3 | Screws | 67 | 12 |
| 4 | Female | Left | 23 | 61 | 2 | Nonoperative | 66 | 5 |
| 5 | Female | Right | 33 | 61 | 2 | Nonoperative | 63 | 2 |
| 6 | Male | Left | 23 | 41 | 2 | Nonoperative | 52 | 11 |
| 7 | Female | Left | 27 | 37 | 3 | Plate | 55 | 18 |
| 8 | Male | Left | 20 | 30 | 3 | Screws | 32 | 2 |
| 9 | Male | Left | 30 | 23 | 3 | Plate | 25 | 2 |
| 10 | Female | Right | 27 | 55 | 3 | Plate | 56 | 1 |
| 11 | Male | Left | 24 | 46 | 1 | Screws | 49 | 3 |
| 12 | Female | Left | 27 | 37 | 1 | Screws | 39 | 2 |
| 13 | Female | Right | 23 | 51 | 3 | Plate | 52 | 1 |
| Mean | 24.9 | 44.9 | 50.1 | 5.1 |
UKA = unicompartmental knee arthroplasty.
All operations were performed by the two senior authors (JNA, PN) via a lateral parapatellar approach. A tourniquet was used in all patients. A tibial tubercle osteotomy was used in two patients in whom the standard lateral parapatellar approach was too limited to obtain adequate visualization of the articular surface [6]. Concomitant hardware removal was performed in seven of the eight patients with retained hardware. In one case, hardware was left in place as it did not interfere with tibial component placement and was believed to provide support to the bone under the tibial implant (see below). Due to fracture malunion and bone loss, the amount of bone resection on the tibial side was minimized. We used autogenous bone graft from the tibial cut to fill contained defects in the proximal tibia below the level of the tibial cut. To improve the mechanical properties of the cancellous bone under the tibial implant (zone of fixation) in cases requiring bone grafting, one or two reinforcing screws in the transverse plane (three patients) (Fig. 2) or a plate and screws (one patient) were placed through the tibial bone below the tibial cut. We recommend the use of screws or a plate to reinforce the subchondral bone in cases of substantial comminution and depression of the lateral tibial plateau. All components were cemented (Fig. 3). Three different UKA prostheses were utilized in this series: the HLS Uni Evolution (Tornier, Inc, Grenoble, France) (six patients), which is a fixed-bearing resurfacing implant with a cemented full-polyethylene tibial plateau; the Marmor II (Richards Orthopaedics, Memphis, TN) (two patients) before 1989; and the Miller-Galante unicompartmental knee system (Zimmer, Inc, Warsaw, IN) (five patients) after 1989 (Table 2). Both were used with metal-backed cemented tibial implant. All patients received perioperative antibiotics (second-generation cephalosporins) and prophylactic anticoagulation treatment (low-molecular-weight heparin).
Fig. 2.
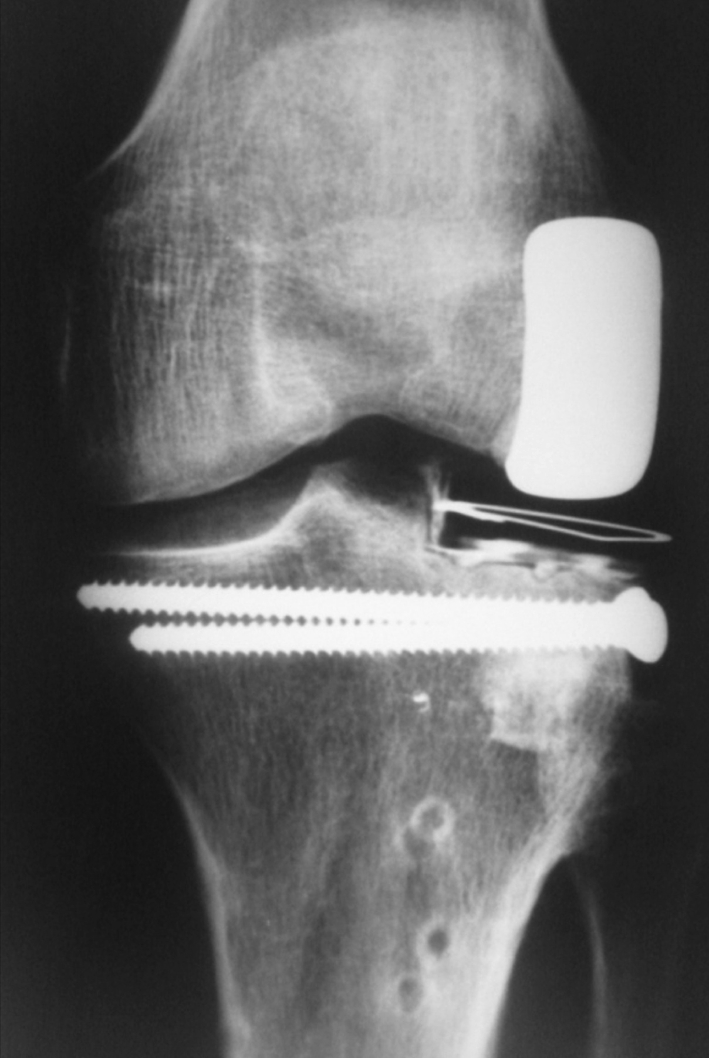
In this postoperative AP plain radiograph of a patient treated with a UKA for posttraumatic lateral compartment arthritis, two screws have been placed through the cancellous bone graft used to fill a defect under the tibial component. These screws improve the mechanical strength of the proximal tibia and allow it to support the implant without subsidence.
Fig. 3A–D.
(A) AP and (B) lateral plain radiographs of a left knee demonstrate isolated posttraumatic arthritis of the lateral compartment secondary to tibial plateau fracture malunion. (C) AP and (D) lateral plain radiographs show the knee postoperatively. The hip-knee-ankle angle is 182° and the weightbearing axis passes through the lateral tibial spine.
Table 2.
Preoperative and postoperative data
| Patient | Type of UKA | Preoperative | Followup (months) | Final followup | Reoperation | ||||
|---|---|---|---|---|---|---|---|---|---|
| HKA angle (°) | IKS knee score (points) | IKS function score (points) | HKA angle (°) | IKS knee score (points) | IKS function score (points) | ||||
| 1 | Miller-Galante | 186 | 65 | 38 | 129 | 181 | 0 | 28 | Patellar fracture (119 months after UKA) |
| 2 | Miller-Galante | 185 | 75 | 89 | 36 | 186 | 100 | 100 | |
| 3 | Miller-Galante | 186 | 55 | 54 | 184 | 183 | 90 | 90 | |
| 4 | Miller-Galante | 186 | 50 | 65 | 184 | 183 | 85 | 80 | |
| 5 | Miller-Galante | 188 | 58 | 45 | 165 | 183 | 75 | 100 | TKA for progression of osteoarthritis (160 months after UKA) |
| 6 | Marmor II | 186 | 55 | 48 | 183 | 184 | 65 | 35 | |
| 7 | Marmor II | 193 | 68 | 30 | 265 | 188 | 95 | 100 | |
| 8 | HLS Uni Evolution | 191 | 35 | 10 | 82 | 184 | 70 | 40 | |
| 9 | HLS Uni Evolution | 192 | 60 | 70 | 84 | 183 | 95 | 100 | Hardware removal (66 months after UKA) |
| 10 | HLS Uni Evolution | 187 | 27 | 40 | 57 | 188 | 95 | 100 | |
| 11 | HLS Uni Evolution | 184 | 29 | 80 | 76 | 186 | 95 | 100 | |
| 12 | HLS Uni Evolution | 193 | 60 | 60 | 38 | 188 | 95 | 100 | |
| 13 | HLS Uni Evolution | 191 | 30 | 40 | 120 | 186 | 95 | 100 | |
HKA = hip-knee-ankle; UKA = unicompartmental knee arthroplasty; IKS = International Knee Society.
A knee immobilizer was placed immediately postoperative and removed when quadriceps function returned. Weightbearing as tolerated without a brace was initiated on Postoperative Day 1. Full ROM was allowed immediately with the exception of the two patients who underwent tibial tubercle osteotomy. In these patients, ROM was limited to 95° of flexion for the first 45 days postoperatively and then advanced to full ROM. The knee immobilizer was utilized during weightbearing for 45 days in these patients. For all patients, physical therapy was supervised daily in the immediate postoperative period and then with two to three times weekly outpatient therapy visits after hospital discharge. Crutches or walkers were utilized in the immediate postoperative period and discontinued at the discretion of the therapist.
Postoperative clinical and radiographic followup was performed prospectively at 2 months, 6 months, 1 year, and every 2 years thereafter in all patients. The clinical and radiographic evaluation was performed according to the same protocol at both institutions and included International Knee Society (IKS) knee and function scores [12]. Data from the last followup were reviewed and confirmed by two independent observers (SL, SP).
Two of us (SL, SP) evaluated all radiographs using a standardized protocol at followup, including standing AP, lateral, and full leg length views and an axial view in 30° of knee flexion. We recorded overall mechanical axis, radiolucent lines, and progression of degenerative disease in the medial or patellofemoral compartments. Mechanical axis was measured as the angle between the femoral mechanical axis (a line drawn from the center of the femoral head to the center of the knee) and the tibial mechanical axis (a line drawn from the center of the knee to the center of the ankle) [19]. Intraclass coefficients (ICCs) for interrater reliability of this method is reportedly 0.88 to 0.94 [19]. The presence of radiolucent lines was noted on standard AP and lateral radiographs of the knee. The ICC for interrater reliability of assessment of the presence of radiolucent lines after UKA is greater than 0.98 [8]. Progression of medial compartment degenerative disease was defined as progression of the medial compartment to a more severe stage of degeneration according to the International Knee Documentation Committee (IKDC) system [10]. The ICC for interrater reliability of assessment of the medial compartment with this system is reportedly between 0.35 and 0.56 [20]. Any subsequent operations on the index knee were recorded.
We report patient demographics using means and SDs or medians and ranges for continuous variables and counts (percent) for categorical variables. We report radiographic outcomes using means and SDs to describe preoperative and postoperative alignment. Finally, we performed 5-, 10-, and 15-year survival analyses for all patients, considering implant revision for any reason as the end point.
Results
At last followup, mean IKS knee and function scores improved from 51 points (range, 29–75 points) preoperatively to 88 points (range, 65–100 points) postoperatively and from 51 points (range, 10–89 points) preoperatively to 87 points (range, 35–100 points) postoperatively, respectively (Table 2). ROM at last followup was generally similar to that before surgery. One patient had a decreased arc of motion, from 110° preoperatively to 80° postoperatively. One patient had an extensor lag preoperatively (20°) that improved to 10° postoperatively.
The mean mechanical axis was 188° (range, 184°–193º) preoperatively and 185° (range, 183°–188°) at last followup. Two knees had a radiolucency of less than 1 mm at the tibial bone-cement interface without any sign of progression after 5 years of followup. No femoral radiolucency was observed.
Considering revision for any reason as the end point, the 5-year and 10-year implant survivorship rates were 100% and the 15-year implant survivorship was 80%. We performed no revisions for infection or loosening. One patient had revision to a TKA for progressive medial compartment degenerative changes at 13.7 years postoperatively. His IKS scores reflect his condition before this revision. The mechanical axis of this knee was not included in the alignment data reported above. One patient suffered a traumatic patella fracture 10 years postoperatively. Before this injury, he was satisfied with the procedure; however, after the injury, he continued to experience anterior knee pain and never regained acceptable knee function. His knee scores were not included in the functional results above as they reflect primarily his disability secondary to the patella fracture. No loosening or substantial polyethylene wear occurred in any knees.
One patient suffered a postoperative pulmonary embolism, which required anticoagulant treatment at therapeutic levels. This patient developed persistent stiffness postoperatively and had manipulation under anesthesia 1 month postoperatively. After manipulation and physical therapy, the patient’s ROM improved to within 10° of the contralateral side. No late complications related to the UKA were encountered. One patient underwent hardware removal at 5.5 years postoperatively to remove the plate used in the initial fracture fixation and left in place as a buttress at the time of UKA. At the time of removal, the proximal two screws were left in place to reinforce the bone under the tibial baseplate as discussed above.
Discussion
The surgical options for posttraumatic lateral femorotibial arthritis include osteotomy, TKA, and UKA [9]. Long-term pain control and functional improvement after lateral UKA for degenerative disease has been reported in the literature [2, 3, 25], even in relatively young patients in whom wear is a concern [16]. UKA can thus be discussed for isolated lateral posttraumatic arthritis. We asked whether UKA for lateral posttraumatic osteoarthritis (1) reliably alleviated pain and improved function, (2) restored lower limb alignment, and (3) was as durable as UKA for primary lateral osteoarthritis.
Some limitations to this study can be outlined. First, the number of patients is relatively small. This limitation is a reflection of the relative rarity of this surgical indication. However, the large improvements in outcome scores and longevity of the implants are effectively demonstrated even in this small series. Second, three different implants were used during the study period. Although we lack numbers for a formal comparison between implant types, we do not believe implant choice to drive outcome. Third, we did not match our patients with patients undergoing lateral UKA implanted for primary arthritis. We have compared these patients to literature controls, but one must be aware of inherent differences in the patient populations when making such comparisons.
Our observations suggest lateral UKA relieves pain and improves function in patients with posttraumatic arthritis. Sah and Scott [25] reported on 10 patients with posttraumatic arthritis in a series of 49 lateral UKAs and an average followup of 5 years. They found lower IKS scores in the patients with posttraumatic arthritis (knee = 74; function = 65) than in patients having UKA for primary degenerative disease (knee = 95, function = 86) in their series. Our results are more similar to those achieved by other authors performing lateral UKA for all indications. Argenson et al. [2] and Sah and Scott [25] reported IKS knee scores ranging from 88 to 89 and function scores ranging from 78 to 80 with 5 to 12 years of followup. Using the Hospital for Special Surgery (HSS) knee score, Ohdera et al. [21] demonstrated good or excellent results in 89% or patients at 5 years and Pennington et al. [23] noted all good or excellent results at 12.4 years with a mean HSS score of 90. Using the Bristol Knee Score, Ashraf et al. [3] noted good or excellent outcomes in 86% of patients at 9 years (Table 3).
Table 3.
Comparison with series of lateral UKA performed for all indications
| Study | Number of UKAs | Followup (years) | IKS knee score (points) | IKS function score (points) | Preoperative alignment (°) | Postoperative alignment (°) | Survival rate |
|---|---|---|---|---|---|---|---|
| Sah and Scott [25] | 49 | 5.2 | 89 | 80 | 190 | 186 | 100% at 5 years |
| Argenson et al. [2] | 40 | 12.6 | 88 | 78 | 188 | 183 | 92% at 10 years |
| 84% at 16 years | |||||||
| Ashraf et al. [3] | 88 | 9.0 | NR | NR | NR | NR | 83% at 10 years |
| 74% at 15 years | |||||||
| Pennington et al. [23] | 29 | 12.4 | NR | NR | 190 | 186 | 100% at 12.6 years |
| Ohdera et al. [21] | 18 | 5 | NR | NR | 190 | 186 | 89% at 5 years |
| Lustig et al. | 13 | 10.2 | 88 | 87 | 188 | 185 | 100% at 5 and 10 years |
| 80% at 15 years |
UKA = unicompartmental knee arthroplasty; IKS = International Knee Society; NR = not reported.
The mechanical axis in our series improved from a mean of 188° preoperatively to 185° postoperatively. This change parallels that noted in previous series of lateral UKA performed for all indications, with preoperative alignment ranging from 188° to 190° and postoperative alignment ranging from 183° to 186° [2, 21, 23, 25] (Table 3).
Implant survivorship in our series was 100% at 5 and 10 years and 80% at 15 years. This finding is similar to the 100% survival at 5 years noted by Sah and Scott [25] in UKAs performed for posttraumatic arthritis, as well as previously published reports of UKA for all indications in which survival rates of 74% to100% have been reported at 10 to 16 years of followup [2, 3, 21, 23] (Table 3).
An important characteristic of the posttraumatic population in our series is that the prior tibial plateau fracture led to the development of arthritis and subsequent UKA at a younger age (mean, 50 years) than the mean age reported in series utilizing UKA for lateral compartment degenerative disease (61–72 years) [2, 3, 16, 21, 23]. The functional demands of these younger patients theoretically increases their failure risk in the medium and long term, as has been noted in medial UKA [14, 15]. In spite of this concern, we noted no evidence of substantial polyethylene wear or implant loosening and implant survival was comparable to that in published series. An alternative to prosthesis use in these young patients is the performance of a lateral opening wedge osteotomy to unload the lateral compartment. It is indicated to treat a valgus malunion of the metaphysis [5, 18, 24] but may not adequately compensate for severe depression of the lateral tibial plateau. Kerkoffs et al. [13] recently published a technique combining osteotomies of the tibial metaphysis and articular surface to correct and unload malunions of the lateral compartment. This technique may be useful in preventing the development of posttraumatic arthritis or preventing its progressing in mild cases but is contraindicated in cases of severe osteoarthritis [13] such as those in our series.
TKA is another surgical option for the treatment of posttraumatic lateral compartment arthritis. Results of TKA after tibial plateau fracture were reported by Weiss et al. [28] in 2003 in a series of 62 patients with a mean followup of 4.2 years (average patient age, 46 years). They found a mean IKS knee score of 82.9 and a functional score of 84. However, a number of perioperative (10%) and postoperative (26%) complications were reported, with a total reoperation rate of 21% in the first 5 years postoperatively.
Our data suggest lateral UKA can relieve pain and restore function for relatively young patients with posttraumatic arthritis of the lateral compartment. Postoperative mechanical axis of the lower limb and implant survival rates were comparable to those obtained for lateral UKA implanted for primary osteoarthritis [2, 16, 23]. We believe lateral UKA is a reasonable option for treating patients with isolated posttraumatic arthritis of the lateral compartment.
Footnotes
PN receives research funding and royalties from Tornier, Inc (Grenoble, France). JNA is a paid consultant for Zimmer, Inc (Warsaw, IN). One or more of the authors (RAM, SL) have received funding from Tornier, Inc. Each remaining author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Hôpital de la Croix Rousse and Hôpital Sainte-Marguerite.
References
- 1.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh) 1968;Suppl 277:7–72. [PubMed] [Google Scholar]
- 2.Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008;466:2686–2693. doi: 10.1007/s11999-008-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashraf T, Newman JH, Evans RL, Ackroyd CE. Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Joint Surg Br. 2002;84:1126–1130. doi: 10.1302/0301-620X.84B8.13447. [DOI] [PubMed] [Google Scholar]
- 4.Chambat P, Ait Si Selmi T, Dejour D. Varus tibial osteotomy. Oper Tech Sports Med. 2000;8:44–47. doi: 10.1016/S1060-1872(00)80024-6. [DOI] [Google Scholar]
- 5.Coventry MB. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69:32–38. [PubMed] [Google Scholar]
- 6.Dejour H, Neyret P, Donell ST. Tibial tubercle osteotomy for access in lateral unicompartmental knee replacement. Knee. 1998;5:33–36. doi: 10.1016/S0968-0160(97)00019-7. [DOI] [Google Scholar]
- 7.Dejour H, Walch G, Deschamps G, Chambat P. Arthrosis of the knee in chronic anterior laxity] [in French. Rev Chir Orthop Reparatrice Appar Mot. 1987;73:157–170. [PubMed] [Google Scholar]
- 8.Gulati A, Chau R, Pandit HG, Gray H, Price AJ, Dodd CA, Murray DW. The incidence of physiological radiolucency following Oxford unicompartmental knee replacement and its relationship to outcome. J Bone Joint Surg Br. 2009;91:896–902. doi: 10.1302/0301-620X.91B7.21914. [DOI] [PubMed] [Google Scholar]
- 9.Gunther TV, Murray DW, Miller R, Wallace DA, Carr AJ, O’Connor JJ, MacLardy Smith P, Goodfellow JW. Lateral unicompartmental arthroplasty with Oxford meniscal knee. Knee. 1996;3:33–39. doi: 10.1016/0968-0160(96)00208-6. [DOI] [Google Scholar]
- 10.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 11.Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma. 1995;9:273–277. doi: 10.1097/00005131-199509040-00001. [DOI] [PubMed] [Google Scholar]
- 12.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 13.Kerkhoffs GM, Rademakers MV, Altena M, Marti RK. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia. J Bone Joint Surg Am. 2008;90:1252–1257. doi: 10.2106/JBJS.D.01816. [DOI] [PubMed] [Google Scholar]
- 14.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1, 819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–135. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 15.Kuipers BM, Kollen BJ, Bots PC, Burger BJ, Raay JJ, Tulp NJ, Verheyen CC. Factors associated with reduced early survival in the Oxford Phase III medial unicompartment knee replacement. Knee. 2010;17:48–52. doi: 10.1016/j.knee.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Lustig S, Paillot JL, Servien E, Henry J, Ait Si Selmi T, Neyret P. Cemented all polyethylene tibial insert unicompartmental knee arthroplasty: a long term follow-up study. Orthop Traumatol Surg Res. 2009;95:12–21. doi: 10.1016/j.otsr.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010;34:565–570. doi: 10.1007/s00264-009-0790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marti RK, Verhagen RA, Kerkhoffs GM, Moojen TM. Proximal tibial varus osteotomy: indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am. 2001;83:164–170. [PubMed] [Google Scholar]
- 19.Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA, Pavlov H. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011 March 23 [Epub ahead of print]. [DOI] [PubMed]
- 20.Mehta VM, Paxton LW, Fornalski SX, Csintalan RP, Fithian DC. Reliability of the International Knee Documentation Committee radiographic grading system. Am J Sports Med. 2007;35:933–935. doi: 10.1177/0363546507299742. [DOI] [PubMed] [Google Scholar]
- 21.Ohdera T, Tokunaga J, Kobayashi A. Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty. 2001;16:196–200. doi: 10.1054/arth.2001.2090. [DOI] [PubMed] [Google Scholar]
- 22.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006;37:475–484. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 23.Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty. 2006;21:13–17. doi: 10.1016/j.arth.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 24.Puddu G, Cipolla M, Cerullo G, Franco V, Gianni E. Which osteotomy for a valgus knee? Int Orthop. 2010;34:239–247. doi: 10.1007/s00264-009-0820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sah AP, Scott RD. Lateral unicompartmental knee arthroplasty through a medial approach: study with an average five-year follow-up. J Bone Joint Surg Am. 2007;89:1948–1954. doi: 10.2106/JBJS.F.01457. [DOI] [PubMed] [Google Scholar]
- 26.Servien E, Ait Si Selmi T, Neyret P, Verdonk P. How to select candidates for lateral unicompartmental prosthesis. Tech Knee Surg. 2007;6:51–59. doi: 10.1097/btk.0b013e3180326ee9. [DOI] [Google Scholar]
- 27.Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop Relat Res. 1993;292:87–100. [PubMed] [Google Scholar]
- 28.Weiss NG, Parvizi J, Trousdale RT, Bryce RD, Lewallen DG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. J Bone Joint Surg Am. 2003;85:218–221. doi: 10.1302/0301-620X.85B2.13559. [DOI] [PubMed] [Google Scholar]