Abstract
Background: A Step I diet with lean beef compared with lean white meat both decrease LDL cholesterol. To our knowledge, no studies have evaluated a low–saturated fatty acid (SFA) (<7% calories) diet that contains lean beef.
Objective: We studied the effect on LDL cholesterol of cholesterol-lowering diets with varying amounts of lean beef [ie, Dietary Approaches to Stop Hypertension (DASH): 28 g beef/d; Beef in an Optimal Lean Diet (BOLD): 113 g beef/d; and Beef in an Optimal Lean Diet plus additional protein (BOLD+): 153 g beef/d] compared with that of a healthy American diet (HAD).
Design: Thirty-six hypercholesterolemic participants (with LDL-cholesterol concentrations >2.8 mmol/L) were randomly assigned to consume each of the 4 diets (HAD: 33% total fat, 12% SFA, 17% protein, and 20 g beef/d), DASH (27% total fat, 6% SFA, 18% protein, and 28 g beef/d), BOLD (28% total fat, 6% SFA, 19% protein, and 113 g beef/d), and BOLD+ (28% total fat, 6% SFA, 27% protein, and 153 g beef/d) for 5 wk.
Results: There was a decrease in total cholesterol (TC) and LDL-cholesterol concentrations (P < 0.05) after consumption of the DASH (−0.49 ± 0.11 and −0.37 ± 0.09 mmol/L, respectively), BOLD (−0.48 ± 0.10 and −0.35 ± 0.9 mmol/L, respectively), and BOLD+ (−0.50 ± 0.10 and −0.345 ± 0.09 mmol/L, respectively) diets compared with after consumption of the HAD (−0.22 ± 0.10 and −0.14 ± 0.10 mmol/L, respectively). Apolipoprotein A-I, C-III, and C-III bound to apolipoprotein A1 particles decreased after BOLD and BOLD+ diets compared with after the HAD, and there was a greater decrease in apolipoprotein B after consumption of the BOLD+ diet than after consumption of the HAD (P < 0.05 for both). LDL cholesterol and TC decreased after consumption of the DASH, BOLD, and BOLD+ diets when the baseline C-reactive protein (CRP) concentration was <1 mg/L; LDL cholesterol and TC decreased when baseline CRP concentration was >1 mg/L with the BOLD and BOLD+ diets.
Conclusions: Low-SFA, heart-healthy dietary patterns that contain lean beef elicit favorable effects on cardiovascular disease (CVD) lipid and lipoprotein risk factors that are comparable to those elicited by a DASH dietary pattern. These results, in conjunction with the beneficial effects on apolipoprotein CVD risk factors after consumption of the BOLD and BOLD+ diets, which were greater with the BOLD+ diet, provide support for including lean beef in a heart-healthy dietary pattern. This trial was registered at clinicaltrials.gov as NCT00937898.
INTRODUCTION
The recommended approach for lowering LDL cholesterol, which is a primary target for CVD4 risk reduction, is to reduce dietary SFA (<7% of energy), trans fatty acids (as low as possible), and cholesterol (<200 mg/d) (1). A dietary pattern that emphasizes fruit and vegetables, legumes, whole grains, nuts, and seeds is recommended (2). Skim and reduced-fat dairy products, moderate amounts of lean-protein sources, including meats, poultry, and eggs, and increased seafood (particularly fatty fish), as well as plant-based proteins also are recommended (2). It is not necessary to exclude lean beef, and the Adult Treatment Panel III Guidelines and the Dietary Guidelines for Americans indicate that lean red meat can be included in a heart-healthy dietary pattern that is low in SFA and cholesterol (1, 2). Beef is a popular food and a source of many nutrients, and, consequently, lean beef can be an important lean-protein food source to meet current food-based and nutrient recommendations.
Epidemiologic studies have reported mixed associations between red-meat consumption and CVD mortality (3), acute myocardial infarction, unstable angina, and metabolic syndrome (3–8). A recent report from the Nurses’ Health Study showed that the replacement of one serving of unprocessed red meat with poultry or fish was associated with 19% and 24% reductions in coronary heart disease risk, respectively (5). Some of the discrepancies in the literature may reflect not differentiating higher-fat red meat from lean red meat (specifically beef) or not accounting for different meat processing and cooking methods (6) because some epidemiologic studies have not shown this association (7, 8), especially when SFA was controlled (8) or when only red, and not processed, meat was included in the analysis (7).
Previous free-living and controlled-consumption studies reported comparable LDL cholesterol–lowering effects of a National Cholesterol Education Program Step I diet (total fat <30% and SFA <10% energy) (9) with lean beef or lean white meat (10–12). To our knowledge, no studies have examined the effects of an SFA-restricted (<7% calories), heart-healthy diet with lean beef. Red meat is limited in the DASH diet as a strategy to decrease SFA (13).
The cholesterol-lowering effects of a low-SFA diet with lean beef have not been rigorously evaluated. Thus, we conducted a well-controlled consumption study to evaluate the LDL cholesterol–lowering effects of a DASH-like diet that contained lean beef (BOLD diet: 28% total fat, 6% SFA, 54% carbohydrates, 19% protein, and 113 g beef/d, and a moderate protein diet that contained lean beef (BOLD+: 28% total fat, 6% SFA, 45% carbohydrates, 27% protein, and 153 g beef/d) compared with a healthy American control diet in individuals with elevated LDL-cholesterol concentrations. A DASH diet was included because it is the gold standard for contemporary dietary recommendations. Because Erlinger et al (14) showed that moderate elevations in CRP concentrations attenuated lipid-lowering responses to diet, we also examined this relation.
SUBJECTS AND METHODS
Subjects
Healthy men and women (30–65 y of age) with elevated LDL-cholesterol concentrations (2.84–4.55 mmol/L) were recruited. Additional inclusion criteria were as follows: BMI (in kg/m2) of 18.5–37, triglycerides concentration <3.95 mmol/L, and blood pressure <140/90 mm Hg. Participants were allowed to take prescribed blood pressure–lowering medications and were eligible as long as their blood pressure was below the entry criteria. All participants were nonsmokers and free of established CVD, stroke, diabetes, liver, kidney, or autoimmune disease. Exclusion criteria included the use of cholesterol and lipid-lowering medications or supplements (psyllium, fish oil, soy lecithin, and phytoestrogens), pregnancy or lactation, weight loss ≥10% of body weight within the 6 mo before enrollment in the study, and vegetarianism. The Institutional Review Board at the Pennsylvania State University approved the experimental protocol, and all subjects provided written informed consent. This trial was registered at clinicaltrials.gov as NCT00937898.
Study design
The study used a 4-period randomized, crossover, controlled-feeding design. Subjects were randomly assigned to a treatment (diet) order; they consumed 4 diets (HAD and DASH, BOLD, and BOLD+ diets) for 5 wk each. A short compliance break (average of 1 wk) separated the diet periods. At the beginning of the study and at the end of each diet period, on 2 consecutive days, subjects completed a series of clinical and physical assessments (ie, blood draw, height, and weight measurements) at the General Clinical Research Center. The first participants began the study in September 2007; the last participant completed the study in March 2009.
Diets
The nutrient composition of experimental diets is presented in Table 1. Total energy was held constant for each participant throughout the 4-diet periods, and participants were monitored (daily weigh-ins) to ensure they remained weight stable. The 3 experimental diets (DASH, BOLD, and BOLD+ diets) contained similar amounts of total fat, SFA, PUFA, and cholesterol. The HAD was higher in total fat, SFA, MUFA, PUFA, and cholesterol and was lower in total fiber. BOLD and DASH diets were matched for macronutrient composition. The BOLD+ diet was higher in protein (27% of total energy) compared with the HAD (17%), DASH (18%), and BOLD (19%) diets and, thus, lower in carbohydrates (45% compared with 50–55%) (Table 1).
TABLE 1.
BOLD study diets: energy, nutrient composition, and food-group servings1
| Diets |
||||
| HAD | DASH | BOLD | BOLD+ | |
| Nutrient targets | ||||
| Calories | 2097 | 2106 | 2100 | 2104 |
| Protein (g; percentage of kcal) | 17 (91.7) | 18 (98.4) | 19 (99.6) | 27 (145.6) |
| Carbohydrates (g; percentage of kcal) | 50 (268.1) | 55 (298.3) | 54 (287.4) | 45 (243.7) |
| Fat (g; percentage of kcal) | 33 (77.0) | 27 (64.4) | 28 (65.8) | 28 (66.6) |
| Cholesterol (mg) | 287 | 188 | 168 | 193 |
| SFA (g; percentage of kcal) | 12 (27.9) | 6 (15.2) | 6 (15.4) | 6 (14.5) |
| PUFA (g; percentage of kcal) | 7 (15.5) | 8 (18.9) | 7 (16.5) | 7 (16.1) |
| MUFA (g; percentage of kcal) | 11 (25.9) | 9 (21.8) | 11 (25.2) | 12 (29.3) |
| Fiber (g) | 24 | 36 | 32 | 38 |
| Sodium (mg) | 3243 | 2982.8 | 2712 | 3344 |
| Potassium (mg) | 3259 | 4247 | 3998 | 4417 |
| Calcium (mg) | 993 | 1140 | 936 | 1060 |
| Magnesium (mg) | 308 | 403 | 392 | 429 |
| Food groups (servings/d) | ||||
| Fruit and juices (cups) | 3.1 | 4.1 | 4.5 | 3.4 |
| Vegetables (cups) | 3.2 | 4.3 | 3.9 | 4.6 |
| Grains (oz) | 8.3 | 4.5 | 5.6 | 5.3 |
| Low-fat dairy products (cups) | 1.2 | 2.3 | 1.8 | 4.7 |
| High-fat dairy products (cups) | 0.7 | 0.1 | 0.0 | 0.0 |
| Legumes, nuts, seeds, and other vegetable protein (oz) | 0.6 | 2.1 | 1.3 | 4.2 |
| Beef (oz) | 0.7 | 1.0 | 4.0 | 5.4 |
| Poultry, pork, and fish (oz) | 3.7 | 3.7 | 1.0 | 1.0 |
| Egg and egg-product substitutes (oz) | 0.24 | 0.2 | 0.1 | 0.9 |
| Fats and oils (g) | 5.4 | 4.0 | 4.3 | 1.4 |
On the basis of 2100 kcal/d. Average across a 6-d menu cycle. All values were determined by using Nutritionist Pro software (Axxya Systems LLC). BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; SFA, saturated fatty acid.
The HAD provided full-fat cheese and dairy products, more oil and butter, and refined grains. The DASH, BOLD, and BOLD+ diets provided low-fat or nonfat versions of these foods, less oil and butter, and more whole grains. All diets were rich in fruit, vegetables, and lean meats consistent with food-based dietary recommendations. Although matched for protein, the BOLD and DASH diets differed in their primary protein source; the BOLD diet included an average of 113 g lean beef/d. The BOLD+ diet contained 153 g lean beef/d, and the HAD and DASH diet contained 20 and 28 g lean beef/d, respectively.
The lean beef used in the study (primarily select-grade top round, chuck shoulder pot roast, and 95% lean ground beef) was purchased from The Pennsylvania State University Meats Laboratory. The meat was prepared via braising, grilling, or frying (95% lean ground beef only) and never over an open flame to prevent charring.
Menus were created for a 6-d diet cycle across a range of calorie amounts (1800–3600 kcal/d). Sample 1-d menus for each of the diets are shown in Table 2. All meals and snacks were prepared at the Metabolic Diet Study Center, The Pennsylvania State University. Participants ate one meal per day (Monday–Friday) in the Center, and their other meals were prepared and packed for off-site consumption. Adherence with the diets was monitored via daily and weekly compliance questionnaires.
TABLE 2.
One-day DASH, BOLD, and BOLD+ menus1
| HAD | DASH | BOLD | BOLD+ | |
| Breakfast | Oatmeal packet | Whole-grain cereal and milk | Oatmeal packet | Whole-grain cereal and milk |
| Brown sugar Orange juice Milk English muffin Butter |
Yogurt Banana Orange juice |
Blueberries (frozen) Orange juice Milk Plain bagel and margarine |
Orange juice Low-fat cottage cheese |
|
| Lunch | Tuna salad Pita bread Baby carrots Pretzels |
Vegetarian chili Whole-wheat crackers Low-fat cheddar cheese Peaches, canned in juice |
Meatballs and marinara sauce Sandwich roll and lettuce Broccoli, baby carrots, and ranch dressing Pretzels |
Beef chili with shredded cheddar cheese Whole-wheat crackers Peaches, canned in juice |
| Dinner | Southwest fajita with chicken Flour tortillas Cheddar cheese(shredded) Lettuce Red bell pepper Sour cream |
Turkey breast with mashed potatoes and gravy Broccoli Lettuce, cherry tomatoes, and flax tahini dressing Dinner roll with butter |
Southwest fajita with beef Flour tortillas, cheddar cheese (shredded), lettuce, and red bell pepper |
Pot roast with mashed potatoes and gravy Broccoli and edamame beans Lettuce, cherry tomatoes, and flax tahini dressing Dinner roll with margarine |
| Snack | Chocolate-chip cookies | Trail mix Grapes |
Peanut butter Apple Celery sticks |
Hummus Whole-wheat pita and baby carrots for dipping Trail mix |
BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet.
Clinical assessments
Body weight was measured at each laboratory visit (in addition to daily weigh-ins at the diet center). All blood samples were collected after an overnight (10–12 h) fast according to a standardized protocol. Serum and plasma aliquots were stored at −80°C until the time of analysis.
Lipids, lipoproteins, and apolipoproteins
TC and triglycerides were measured by using enzymatic procedures with commercially available kits (cholesterol and triglyceride kits; Alfa Wassermann). HDL cholesterol was quantified according to the modified heparin-manganese precipitation procedure of Warnick and Albers (15). LDL cholesterol was determined by using Friedewald's equation as follows:
These assays were conducted at the core endocrine laboratory at the MS Hershey Medical Center General Clinical Research Center (Hershey, PA). Apolipoprotein A1, B, and C-III were measured by using the immunoturbidimetric procedure of Riopponen et al (16) with corresponding monospecific polyclonal antisera. These assays were conducted at the Oklahoma Research Institute (Oklahoma City, OK) under the supervision of Petar Alaupovic.
Insulin and glucose
Insulin was measured by using a radioimmunoassay with 125I-labeled human insulin and a human insulin antiserum (17). Glucose was determined with an immobilized enzyme biosensor for glucose (YSI 2300 STAT Plus Glucose & Lactate Analyzer; Yellow Springs Instruments) (18). These assays were conducted at the core endocrine laboratory at the MS Hershey Medical Center.
High-sensitivity CRP
CRP was measured with the use of latex-enhanced immunonephelometry (Quest Diagnostics).
Statistical analysis
Power calculations were conducted to estimate the required sample size on the basis of data from the original DASH study (19) in which LDL cholesterol was reduced by 9% after 8 wk consumption of the DASH diet compared with after consumption of the control diet. Analyses used the following assumptions: power was set at 0.8, α was set at 0.05, and 2-tailed tests were used. It was estimated that a sample size of 40 was sufficient to test the primary LDL-cholesterol hypothesis while allowing for a 10% dropout rate.
All statistical analyses were performed with SAS software (version 9.2; SAS Institute Inc). Two-sample t tests were used to determine significant differences between sexes at baseline for each outcome variable. The residuals for each variable were used to assess normality. Logarithmic transformations were used for nonnormally distributed variables (triglycerides). The mixed-models procedure (PROC MIXED) in the SAS software (version 9.2; SAS Institute Inc) was used to test the effects of diet and order on outcome variables. A doubly repeated measures ANCOVA (repeated for diet and day of blood draw) was used with age, weight, and baseline lipid concentrations as covariates for lipid and lipoprotein measurements. Repeated ANCOVA (repeated for diet) was used with age, weight, and baseline amounts for the remaining variables. The primary outcome was the change in LDL cholesterol after consumption of the BOLD and BOLD+ diets compared with after consumption of the HAD; Dunnett's post hoc test was used to determine whether these differences were significant (P < 0.05). Tukey-Kramer–adjusted P values were used to determine whether differences between the diets in secondary outcome variables were significant (P < 0.05). In the secondary analysis of CRP subgroups, P values were Bonferroni-adjusted for multiple comparisons; Tukey-Kramer–adjusted P values were not used to control for overadjustment because of erroneous comparisons.
RESULTS
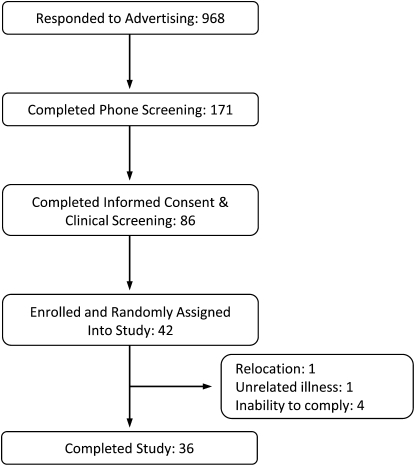
Forty-two individuals were recruited for the study. During the study, one subject dropped out because of a job change and relocation, one subject dropped out because of an unrelated illness, and 4 subjects dropped out because of inability to adhere to the dietary protocol. A total of 36 subjects were included in the final analysis (Figure 1).
FIGURE 1.
Recruitment flow diagram.
Baseline subject characteristics are presented in Table 3. Women had significantly higher serum TC (5.74 compared with 5.02 mmol/L; P = 0.003), LDL cholesterol (3.78 compared with 3.31 mmol/L; P = 0.02), and HDL cholesterol (1.45 compared with 1.16 mmol/L; P = 0.01) concentrations than did men. Men had significantly higher BMI (27.3 compared with 24.8; P = 0.02) and serum glucose (4.82 compared with 4.6 mmol/L; P = 0.03) concentrations compared with women. Despite these differences at baseline, no significant interactions of sex by outcome measure were shown. Subject adherence to the prescribed diets was 93% according to daily self-reporting forms. Body weight was maintained during the diet periods within 2.2 kg.
TABLE 3.
Baseline characteristics of study participants (n = 36)1
| Characteristic | Men (n = 15) | Women (n = 21) | Combined |
| Age (y) | 49 ± 1.8 (39-63) | 50 ± 2.0 (45-97) | 50 ± 1.4 |
| BMI (kg/m2) | 27.3 ± 0.7 (19.4–35.5) | 24.8 ± 0.5 (19.4–35.5)2 | 25.7 ± 0.5 |
| TC (mmol/L) | 5.02 ± 0.14 (3.98–6.16) | 5.74 ± 0.22 (4.58–7.38)2 | 5.46 ± 0.12 |
| LDL cholesterol (mmol/L) | 3.31 ± 0.14 (2.46–2.46) | 3.78 ± 0.12 (3.00–4.84)2 | 3.6 ± 0.1 |
| HDL cholesterol (mmol/L) | 1.16 ± 0.05 (0.91–1.55) | 1.45 ± 0.08 (0.88–2.30)2 | 1.34 ± 0.06 |
| Non–HDL cholesterol | 3.87 ± 0.14 (3.04–5.05) | 4.28 ± 0.13 (3.43–5.33)2 | 4.11 ± 0.19 |
| TG (mmol/L) | 1.18 ± 0.10 (0.55–1.88) | 1.07 ± 0.06 (0.68–1.95) | 1.12 ± 0.05 |
| Glucose (mmol/L) | 4.82 ± 0.10 (3.83–5.55) | 4.60 ± 0.08 (4.05–5.38)2 | 4.7 ± 0.09 |
| Insulin (IU/mL) | 12 ± 1.9 (7-23) | 13 ± 0.961 (9-17) | 12 ± 0.97 |
| CRP (mg/L) | 1.43 ± 0.4 (5.4–0.3) | 1.34 ± 0.3 (4.5–0.3) | 1.4 ± 0.2 |
All values are means ± SEMs; ranges in parentheses. Baseline values were measured before consuming any study food. CRP, C-reactive protein; TC, total cholesterol; TG, triglycerides.
Two-sample t test was used to determine significant (P < 0.05) differences between sexes with SAS (version 9.2; SAS Institute Inc).
Lipids, lipoproteins, and apolipoproteins
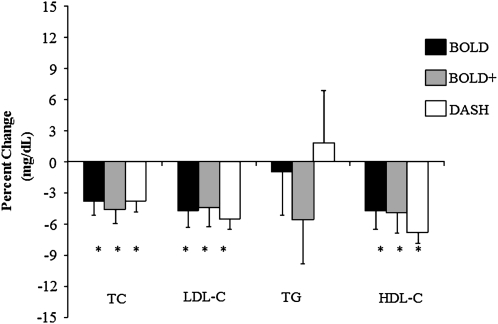
TC, LDL cholesterol, and HDL cholesterol were significantly decreased after consumption of the DASH, BOLD, and BOLD+ diets but not the HAD diet (P < 0.05) (Table 4). Compared with the HAD, LDL cholesterol was significantly decreased by 5.5%, 4.7%, and 4.4% by the DASH, BOLD, and BOLD+ diets, respectively ( < 0.05; Figure 2). TC was decreased after consumption of the DASH, BOLD, and BOLD+ diets by 3.8%, 3.8%, and 4.6%, respectively, compared with after consumption of the HAD. There were no differences in any of the lipid and lipoprotein changes in the test diets (DASH, BOLD, and BOLD+) (P > 0.1).
TABLE 4.
Effect of diet on lipids and lipoproteins1
| HAD (n = 33) | DASH (n = 35) | BOLD (n = 34) | BOLD+ (n = 34) | |
| TC (mmol/L) | 5.25 ± 0.09a | 4.98 ± 0.09b | 4.99 ± 0.09b | 4.96 ± 0.09b |
| TG (mmol/L)2 | 1.06 ± 0.06 | 1.08 ± 0.06 | 1.05 ± 0.07 | 1.00 ± 0.05 |
| LDL cholesterol (mmol/L) | 3.44 ± 0.08a | 3.22 ± 0.07b | 3.23 ± 0.07b | 3.23 ± 0.07b |
| HDL cholesterol (mmol/L) | 1.32 ± 0.05a | 1.22 ± 0.04b | 1.24 ± 0.04b | 1.24 ± 0.04b |
| Non-HDL cholesterol (mmol/L) | 3.89 ± 0.07a | 3.71 ± 0.08b | 3.70 ± 0.08b | 3.66 ± 0.07b |
All values are means ± SEMs. The MIXED procedure (version 9.2; SAS Institute Inc) was used to test the effects of diet. Values in the same row with different superscript letters are significantly different (Dunnett-adjusted P < 0.05). BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; TC, total cholesterol; TG, triglycerides.
Raw values reported. Data were log transformed to achieve normality when testing for significant differences.
FIGURE 2.
Change in lipids and lipoproteins. Mean percentage change (±SEM) from the HAD (HAD: n = 33; DASH: n = 35; BOLD: n = 34; and BOLD+: n = 34). The MIXED procedure in SAS software (version 9.2; SAS Institute Inc) was used to test the effects of diet. *Significantly different from the HAD, P < 0.05. BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; TC, total cholesterol; TG, triglycerides.
Apolipoprotein A-I was significantly decreased after consumption of the BOLD and BOLD+ diets compared with after consumption of the HAD (130.6 and 130.1 compared with 135.9 mg/dL, respectively), with no significant differences after consumption of the DASH diet (133.7 mg/dL). Apolipoprotein B was significantly decreased after consumption of the BOLD+ diet than after consumption of the HAD (88.6 compared with 92.8 mg/dL). There were no significant differences in the A1:apolipoprotein B ratio for the DASH, BOLD, or BOLD+ diets compared with that for the HAD. Apolipoprotein C-III concentrations were significantly decreased after consumption of the BOLD+ diet (7.7 mg/dL) compared with after consumption of the HAD (8.5 mg/dL) and DASH (8.2 mg/dL) diets. Apolipoprotein C-III concentrations were also significantly decreased after consumption of the BOLD diet (7.9 mg/dL) but not after consumption of the DASH diet compared with after consumption of the HAD (Table 5). Apolipoprotein C-III HS concentrations were decreased after consumption of the BOLD (5.4 mg/dL) and BOLD+ (5.3 mg/dL) diets compared with after consumption of the HAD (5.8 mg/dL, P < 0.05). No significant differences were observed with heparin-precipitated apolipoprotein C-III concentrations or apolipoprotein C-III ratio (apolipoprotein C-III HS to heparin-precipitated apolipoprotein C-III) during this intervention.
TABLE 5.
Effect of diet on apolipoproteins1
| Apolipoprotein | HAD | DASH | BOLD | BOLD+ |
| A-I (mg/dL) | 135.9 ± 2.1a | 133.73 ± 2.1a,b | 130.6 ± 1.2b | 130.11 ± 2.1b |
| B (mg/dL) | 92.8 ± 1.5a | 91.0 ± 1.5a,b | 91.1 ± 1.5a,b | 88.6 ± 1.5b |
| C-III (mg/dL) | 8.5 ± 0.2a | 8.21 ± 0.2a,b | 7.94 ± 0.2b,c | 7.71 ± 0.2c |
| C-III HP (mg/dL) | 2.62 ± 0.1 | 2.6 ± 0.1 | 2.5 ± 0.1 | 2.43 ± 0.1 |
| C-III HS (mg/dL) | 5.83 ± 0.2a | 5.59 ± 0.2a,b | 5.4 ± 0.1b | 5.30 ± 0.2b |
All values are means ± SEMs. The MIXED procedure (version 9.2; SAS Institute Inc) was used to test the effects of diet. Values in the same row with different superscript letters are significantly different (Tukey-adjusted P < 0.05). BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; HP, heparin precipitated; HS, heparin supernatant fluid.
CRP
There were no differences in CRP after consumption of any of the dietary treatments (Table 6). Secondary analysis revealed that baseline CRP concentrations affected TC and the LDL-cholesterol responses of subjects to the dietary treatments (diet × baseline CRP; P < 0.05). Subjects with baseline CRP concentrations ≥1 mg/L experienced significant decreases in TC from baseline after consumption of the BOLD and BOLD+ diets. These changes were greater than after consumption of the HAD diet. In addition, the changes were greater after consumption of the BOLD diet than after consumption of the DASH diet. Similar effects of CRP were observed for LDL cholesterol; individuals with baseline CRP concentrations ≥1 mg/L had significant decreases in LDL cholesterol after consumption of the BOLD and BOLD+ diets, although these were not different from after consumption of the HAD (P = 0.052 and P = 0.087, respectively) or DASH (P = 0.098 and P = 0.999, respectively) diets (Table 6).
TABLE 6.
Effect of diet on CRP, TC, and LDL-cholesterol change1
| HAD | DASH | BOLD | BOLD+ | |
| CRP (mg/L) | 1.14 ± 0.19 | 1.07 ± 0.15 | 1.0 ± 0.18 | 0.92 ± 0.09 |
| TC-change (mmol/L) | ||||
| Baseline CRP | ||||
| <1 mg/L (n = 21) | −0.35 ± 0.13a,2 | −0.73 ± 0.13b,2 | −0.47 ± 0.13a,b,2 | −0.49 ± 0.13a,b,2 |
| ≥1 mg/L (n = 15) | −0.08 ± 0.14a | −0.20 ± 0.14a,b | −0.53 ± 0.13b,c,2 | −0.54 ± 0.14b,2 |
| LDL-cholesterol change (mmol/L) | ||||
| Baseline CRP | ||||
| <1 mg/L (n = 21) | −0.19 ± 0.08a | −0.47 ± 0.10b,2 | −0.29 ± 0.08a,2 | −0.31 ± 0.10a,2 |
| ≥1 mg/L (n = 15) | −0.07 ± 0.13a | −0.21 ± 0.13a | −0.38 ± 0.13a,2 | −0.39 ± 0.16a,2 |
All values are means ± SEMs. CRP stratification was based on American Heart Association CRP cutoffs (29). Changes are from baseline. There was no significant effect of diet (P < 0.05) on CRP concentrations. Diet × baseline CRP, P = 0.0008 (LDL-cholesterol change) and P = 0.0009 (TC change). CRP was log transformed to achieve normality. Actual values of CRP are presented. Values in the same row with different superscript letters are significantly different, adjusted P < 0.05 (MIXED procedure, version 9.2; SAS Institute Inc). BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; CRP, C-reactive protein; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; TC, total cholesterol.
Significantly different from zero (P < 0.05) (MIXED procedure, version 9.2; SAS Institute Inc).
In comparison, in individuals with baseline CRP concentrations <1 mg/L, TC was significantly decreased after consumption of all 4 diets; the TC reduction was greatest for the DASH diet, and this was significantly different from that for the HAD but not different from that for the BOLD or BOLD+ diets. In the low-CRP subgroup (<1 mg/L), the experimental diets (not the HAD) significantly decreased LDL cholesterol; only differences between the HAD and DASH diet were significant (Table 6).
Glucose and insulin
Serum glucose and insulin concentrations were not different after consumption of the DASH (4.76 ± 0.05 mmol/L and 12.0 ± 0.06 μU/mL, respectively), BOLD (4.82 ± 0.05 mmol/L and 13.6 ± 0.5 μU/mL, respectively), or BOLD+ (4.92 ± 0.05 mmol/L and 13.6 ± 0.6 μU/mL, respectively) diets compared with after consumption of the HAD (4.82 ± 0.05 mmol/L and 12.6 ± 0.6 μU/mL, respectively).
DISCUSSION
Lipids, lipoproteins, and apolipoproteins
To our knowledge, this was the first controlled-consumption study that showed an increase in lean-beef consumption while controlling SFA (6% calories) in the context of a heart-healthy diet was associated with significant decreases in LDL cholesterol. In the current study, the BOLD and DASH diets decreased the LDL-cholesterol concentration by −0.41 mmol/L compared with similar decreases, compared with baseline, of −0.34 mg/dL and −0.30 mmol/L in the DASH (19) and OmniHeart (carbohydrate diet) (20) trials, respectively. In addition, the decrease in the LDL-cholesterol concentration for the BOLD+ and OmniHeart protein diets was similar at −0.42 mg/dL and −0.36 mmol/L, respectively. Decreases in LDL-cholesterol concentrations observed for the BOLD and BOLD+ diets were achieved with protein sources that differed from those used in the DASH (0.5 servings of beef, pork, or ham/d, and OmniHeart (0.9 servings of beef, pork, or ham/d studies. However, SFA concentrations were similar in the DASH, OmniHeart, and BOLD study diets (7%, 6%, and 6% of total calories, respectively). HDL cholesterol decreased during the DASH (1.2 mmol/L), BOLD (1.2 mmol/L), and BOLD+ (1.2 mmol/L) diets compared with during the HAD (1.3 mmol/L); these decreases were due to differences in total and saturated fat between diets (total fat: 33% compared with 28%; SFA: 12% compared with 6%). Thus, the protein source [with the exception of soy protein (21)] does not appear to modify the TC or LDL cholesterol response to a cholesterol-lowering diet.
The LDL-cholesterol decreases we observed extend the findings of studies conducted by Davidson et al (11) and Hunninghake et al (10) with free-living subjects who were instructed to substitute lean beef for chicken, fish, or pork in a National Cholesterol Education Program Step I diet (<30% total fat, <10% SFA, and <300 mg cholesterol/d). Subjects who consumed the BOLD diet experienced a greater decrease in TC (−9.3%) and LDL cholesterol (−10.1%) (compared with consumption of the HAD) from baseline than reported by Davidson et al (−1.0% and −1.7% respectively) and Hunninghake et al (−0.9% and −1.9%, respectively). These differences most likely were due to the lower SFA intake after consumption of the BOLD diet (6% SFA). In a controlled-consumption study conducted by Beauchesen-Rondeau et al (12) to evaluate the substitution of lean beef compared with chicken or white fish, the decrease in LDL cholesterol (−7.0%) was not as great as that (−10.1%) with the BOLD diet. Again, this result may reflect differences in the SFA content of the experimental diets (10% compared with 6%) compared with the control diets between studies [BOLD study: 6% compared with 12%; Beauchesen-Rondeau et al (12): 10% compared with 12%]. Despite the greater magnitude of the LDL-cholesterol decrease in our study than in some previous studies (10, 11), a key consistent finding (from our study and in the literature) is the equivalent decreases in LDL cholesterol with lean beef than with white meat when macronutrient profiles of diets are similar.
Compared with the HAD, the BOLD+ diet was the only treatment diet that significantly decreased apolipoprotein B. Compared with the HAD, both lean-beef diets significantly decreased apolipoprotein A1 and total apolipoprotein C-III. Smit et al (22), by using NHANES (phase 1) data, reported that the highest quartile of apolipoprotein B was associated with the highest intakes of beef. However, SFA was highly correlated with the protein source, which, thus, prevented conclusions from being drawn on the basis of individual predictors (ie, beef or SFA). Our results concurred with the apolipoprotein B findings from the OmniHeart trial in which the moderate protein diet yielded the greatest decrease in apolipoprotein B. Mensink et al (23) reported that an isocaloric substitution (1% of energy) of carbohydrates for MUFA and PUFA but not SFA decreased apolipoprotein B; however, isocaloric substitution of protein for carbohydrate also decreases apolipoprotein B; the extent of this effect has yet to be fully quantified.
Changes in total apolipoprotein C-III on lean-beef diets reflected decreases in apolipoprotein C-III HS, which represents the number of apolipoprotein C-III molecules bound to apolipoprotein A1–containing particles (Table 5). Kawakami and Yoshida (24) have suggested that apolipoprotein C-III bound to HDL inhibits the antiinflammatory properties of HDL. Although total apolipoprotein A1 was decreased in the BOLD and BOLD+ diets, the decrease in apolipoprotein C-III bound to apolipoprotein A1–containing particles suggested that the antiinflammatory capacity of the apolipoprotein A1–containing particles was improved.
Baseline CRP concentrations appeared to influence TC and LDL cholesterol responses of subjects to the experimental diets. The link between inflammation and lipid and lipoprotein changes has been known for several decades (25, 26); however, the mechanism by which CRP modulates these responses is unknown. Previous studies have reported a blunted TC- and LDL cholesterol–lowering response to DASH (14) and Step I (27, 28) diets in individuals with increased baseline CRP. However, we observed a different effect in the high-CRP group for diets that contained lean beef. We observed a greater decrease in TC (compared with in the DASH diet) and LDL cholesterol (compared with zero) with consumption of BOLD and BOLD+ diets in subjects with high CRP concentrations. In subjects with high CRP, the BOLD and BOLD+ diets significantly decreased concentrations of TC (−0.53 and −0.54 mmol/L, respectively) and LDL cholesterol (−0.38 and −0.39 mmol/L respectively) similarly. The mechanisms that account for these different diet responses in subjects with high compared with low CRP are not clear. Additional studies are needed to determine whether diets that contain lean beef benefit individuals with high CRP to achieve a substantial cholesterol-lowering diet response.
The BOLD study has several strengths. We conducted a tightly controlled clinical study and achieved high levels of dietary adherence as verified by the daily monitoring forms. To our knowledge, the BOLD study is first study to examine the effects of increased lean-beef consumption in the context of current dietary recommendations. Finally, our study population was representative of a large portion of the US population [LDL-cholesterol concentrations in approximately the 35th percentile (1)], and thus, the findings have broad applicability. A limitation of our study was that we had only self-reported compliance measures and no biological measures of adherence to the lean beef and other test diets. In addition, we used a controlled-consumption study design and lean beef was preselected for, prepared for, and consumed by participants. In a free-living setting, individuals would be required to select lean cuts of beef from a wide variety of options in the marketplace and be mindful of preparation techniques and portion control. Although there are 29 cuts of beef that meet lean beef criteria, many grocery stores would feature the following cuts: top loin and top round steaks, top sirloin bottom round roast, and 95% lean ground beef. Adhering to the BOLD and BOLD+ diets that we prepared might be challenging for consumers, at least initially, and therefore, decreases in LDL-cholesterol concentrations would be less than expected. It is important for consumers to be mindful of the types of cut, preparation techniques, and portion control. For many individuals, this can be challenging, which would lessen the expected LDL cholesterol–lowering response.
In conclusion, the inclusion of lean beef (113 g/d) or the partial replacement of carbohydrates with protein (including lean beef) in a low-SFA, DASH-like diet significantly decreased TC and LDL cholesterol compared with in a HAD. These reductions were similar in magnitude to those observed for the DASH diet. The specific effects of the moderate protein, BOLD+ diet on apolipoprotein B and C-III merit additional study. These effects could reflect the increased lean-beef, total protein, or reduced carbohydrate content of the BOLD+ diet; additional research is needed to determine the role of each of these components in the BOLD+ diet on CVD risk. The results of the BOLD study provide convincing evidence that lean beef can be included in a heart-healthy diet that meets current dietary recommendations and reduces CVD risk.
Acknowledgments
We thank our research participant for their participation and commitment to the study. Many members of the Kris-Etherton Laboratory participated in this study, including Deborah Bagshaw, Jennifer Fleming, Amy Cifelli, Melissa Hendricks, and Marcella Smith. We also are grateful to the nursing and clinician staff of the General Clinical Research Center, The Pennsylvania State University.
The authors’ responsibilities were as follows—PMK-E, JPVH, SGW, and PJG: designed the research; MAR and AMH: conducted the research; PA: performed apolipoprotein analysis; MAR and TLG: performed the statistical analyses; MAR, AMH, SGW, JPVH, PJG, PA, and PMK-E: wrote the manuscript, and all authors: took responsibility for the final content of the manuscript. PMK-E and MAR received travel funds and honoraria from the Beef Checkoff Program for giving presentations on this research. MAR received travel funds from the Beef Checkoff Program for giving a presentation on this research. PMK-E, SGW and JPVH received funding from the Beef Checkoff Program for the research reported in this article. AMH, PA, PJG, and TLG had no conflicts of interest to declare. Financial supporters had no role in the design and conduct of the study, collection, analysis, and interpretation of data, or preparation, review, or approval of the manuscript.
Footnotes
Abbreviations used: BOLD, Beef in an Optimal Lean Diet; BOLD+, Beef in an Optimal Lean Diet plus additional protein; CRP, C-reactive protein; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; HAD, healthy American diet; HS, heparin supernatant fluid; SFA, saturated fatty acid; TC, total cholesterol.
REFERENCES
- 1.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421 [PubMed] [Google Scholar]
- 2.2010 Dietary Guidelines Advisory Committee Report of the Dietary Guidelines Advisory Committee on the dietary guidelines for Americans. : United States Department of Agriculture, ed Washington, DC: US Government Printing Office, 2010 [Google Scholar]
- 3.Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med 2009;169:562–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azadbakht L, Esmaillzadeh A. Red meat intake is associated with metabolic syndrome and the plasma C-reactive protein concentration in women. J Nutr 2009;139:335–9 [DOI] [PubMed] [Google Scholar]
- 5.Bernstein AM, Sun Q, Hu FB, Stampfer MJ, Manson JE, Willett WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation 2010;122:876–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tasevska N, Sinha R, Kipnis V, Subar AF, Leitzmann MF, Hollenbeck AR, Caporaso NE, Schatzkin A, Cross AJ. A prospective study of meat, cooking methods, meat mutagens, heme iron, and lung cancer risks. Am J Clin Nutr 2009;89:1884–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010;121:2271–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Damião R, Castro TG, Cardoso MA, Gimeno SGA, Ferreira SRG. Dietary intakes associated with metabolic syndrome in a cohort of Japanese ancestry. Br J Nutr 2006;96:532–8 [PubMed] [Google Scholar]
- 9.National Cholesterol Education Program Second Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults ((Adult Treatment Panel II). Circulation 1994;89:1333–445 [DOI] [PubMed] [Google Scholar]
- 10.Hunninghake DB, Maki KC, Kwiterovich PO, Jr, Davidson MH, Dicklin MR, Kafonek SD. Incorporation of lean red meat into a national cholesterol education program Step I diet: a long-term, randomized clinical trial in free-living persons with hypercholesterolemia. J Am Coll Nutr 2000;19:351–60 [DOI] [PubMed] [Google Scholar]
- 11.Davidson MH, Hunninghake D, Maki KC, Kwiterovich PO, Jr, Kafonek S. Comparison of the effects of lean red meat vs lean white meat on serum lipid levels among free-living persons with hypercholesterolemia: a long-term, randomized clinical trial. Arch Intern Med 1999;159:1331–8 [DOI] [PubMed] [Google Scholar]
- 12.Beauchesne-Rondeau E, Gascon A, Bergeron J, Jacques H. Plasma lipids and lipoproteins in hypercholesterolemic men fed a lipid-lowering diet containing lean beef, lean fish, or poultry. Am J Clin Nutr 2003;77:587–93 [DOI] [PubMed] [Google Scholar]
- 13.Vogt TM, Appel LJ, Obarzanek EVA, Moore TJ, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Cutler JA, Windhauser MM, et al. Dietary approaches to stop hypertension: rationale, design, and methods. J Am Diet Assoc 1999;99:S12–8 [DOI] [PubMed] [Google Scholar]
- 14.Erlinger TP, Miller ER, III, Charleston J, Appel LJ. Inflammation modifies the effects of a reduced-fat low-cholesterol diet on lipids: results from the DASH-sodium trial. Circulation 2003;108:150–4 [DOI] [PubMed] [Google Scholar]
- 15.Warnick GR, Albers JJ. A comprehensive evaluation of the heparin-manganese precipitation procedure for estimating high density lipoprotein cholesterol. J Lipid Res 1978;19:65–76 [PubMed] [Google Scholar]
- 16.Riepponen P, Marniemi J, Rautaoja T. Immunoturbidimetric determination of apolipoproteins A-1 and B in serum. Scand J Clin Lab Invest 1987;47:739–44 [PubMed] [Google Scholar]
- 17.Morgan C, Lazarow A. Immunoassay of insulin using a two-antibody system. Proc Soc Exp Biol Med 1962;110:29–32 [DOI] [PubMed] [Google Scholar]
- 18.Kraus RM, Stallings H, Yeager R, Gavin T. Circulating plasma VEGF response to exercise in sedentary and endurance-trained men. J Appl Physiol 2004;96:1445–50 [DOI] [PubMed] [Google Scholar]
- 19.Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER 3rd, Lin PH, Karanja NM, Most-Windhauser MM, Moore TJ, Swain JF, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr 2001;74:80–9 [DOI] [PubMed] [Google Scholar]
- 20.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 2005;294:2455–64 [DOI] [PubMed] [Google Scholar]
- 21.Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S. Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr 2007;85:1148–56 [DOI] [PubMed] [Google Scholar]
- 22.Smit E, Nieto FJ, Crespo CJ. Blood cholesterol and apolipoprotein B levels in relation to intakes of animal and plant proteins in US adults. Br J Nutr 1999;82:193–201 [PubMed] [Google Scholar]
- 23.Mensink RP, Zock PL, Kester ADM, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–55 [DOI] [PubMed] [Google Scholar]
- 24.Kawakami A, Yoshida M. Apolipoprotein C-III links dyslipidemia with atherosclerosis. J Atheroscler Thromb 2009;16:6–11 [DOI] [PubMed] [Google Scholar]
- 25.Cabana VG, Siegel J, Sabesin S. Effects of the acute phase response on the concentration and density distribution of plasma lipids and apolipoproteins. J Lipid Res 1989;30:39–49 [PubMed] [Google Scholar]
- 26.Khovidhunkit W, Memon RA, Feingold KR, Grunfeld C. Infection and Inflammation-induced proatherogenic changes of lipoproteins. J Infect Dis 2000;181:S462–72 [DOI] [PubMed] [Google Scholar]
- 27.Hilpert KF, Kris-Etherton PM, West SG. Lipid response to a low-fat diet with or without soy is modified by C-reactive protein status in moderately hypercholesterolemic adults. J Nutr 2005;135:1075–9 [DOI] [PubMed] [Google Scholar]
- 28.St-Onge M-P, Zhang S, Darnell B, Allison DB. Baseline serum C-reactive protein is associated with lipid responses to low-fat and high-polyunsaturated fat diets. J Nutr 2009;139:680–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pearson TA, Mensah G, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003;107:499–511 [DOI] [PubMed] [Google Scholar]