Abstract
Aim
The operative note needs to be an accurate and legible account of events occurring in the surgeon’s theatre. We set out to discover if operative notes within a British District General Oral and Maxillofacial Surgery department adhered to Royal College of Surgeons (England) guidelines.
Method
We audited 100 consecutive Oral and Maxillofacial Surgery operations performed within general theatres. As an intervention we designed and piloted a paper based Operative Note Proforma and re-audit was undertaken.
Results
Initial audit showed results lacking in certain areas. At re-audit all audit criteria showed improvement. The mean percentage of data point inclusion rose from 76.1 to 98.3% (0.001 < P-value < 0.005).
Conclusion
Previous papers have discussed various methods of improving operative note standards. We present statistical evidence for the use of an Operative Note Proforma to improve operative note standards within Oral and Maxillofacial Surgery.
Keywords: Operative note, Operation note, Audit
Introduction
The operative note serves as a record of events occurring within the Surgeons operating theatre. For this reason they are an important part of patients’ case notes, and should be complete and legible for future readers. Increasingly the operative note may feature in medico-legal cases, and it is therefore vital from a legal standpoint, that its documentation is accurate. It is the Surgeons duty and responsibility to ensure that this is the case, and as such represents best practice regarding medical record keeping.
Previous reports have alluded to the poor quality of operative notes [1], and in 2002 and more recently in 2008. The Royal College of Surgeons of England (RCSE) published clear guidelines detailing how to construct the operative note [2]. This audit was undertaken to ascertain whether these guidelines are being adhered to, within an Oral and Maxillofacial Surgery Department, and if standards can be improved.
Method
The RCSE, Good Surgical Practice, 2008 [2] was used as the Gold Standard for this audit.
One hundred consecutive operative notes from elective operations performed within the Royal Derby Hospital (England) Oral and Maxillofacial Surgery Department, during December 2009 and January 2010 were audited (audit 1), by a single observer. To eliminate selection bias all Oral and Maxillofacial Surgery operations performed within general theatres were audited, no discrimination of operation type was made, hence the operative notes varied from smaller dental procedures to larger head and neck oncology cases. A paper based data collection sheet was used, and then data counted using an automated data collection machine. These results were presented at a Local Audit Meeting, and the decision made to design and pilot an Operative Note Proforma Sheet (Appendix 1).
After a period of 2 months to allow integration of the Proforma Sheet into departmental use, a re-audit (audit 2) of 100 operative notes from elective operations performed during April to May 2010 was carried out. An identical method and inclusion criterion as in audit 1 was used. Statistical analysis was performed, applying the Two Sample Parametric (classical) T-test.
Results
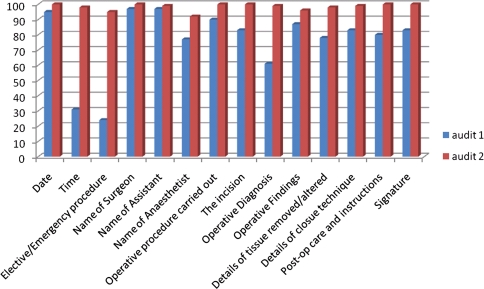
The results of audit 1 and audit 2 are shown in Table 1. Very low scoring data points in audit 1 included: Time (31%) and Elective/Emergency Procedure (24%). With scoring below standards in more vital data points such as: Post-op care and instructions (80%) and Signature (83%). Audit 2 displayed improved scoring in all data points; with all data points scoring >90%, and notably improved scoring in the above data points to 100% (Fig. 1).
Table 1.
Percentage inclusion of specific criteria within operative notes: results of audit round 1 and round 2
| Data entry point | Percentage inclusion | |
|---|---|---|
| Audit 1 | Audit 2 | |
| Date | 95 | 100 |
| Time | 31 | 98 |
| Elective/Emergency procedure | 24 | 95 |
| Name of surgeon | 97 | 100 |
| Name of assistant | 97 | 99 |
| Name of anaesthetist | 77 | 92 |
| Operative procedure carried out | 90 | 100 |
| The incision | 83 | 100 |
| Operative diagnosis | 61 | 99 |
| Operative findings | 87 | 96 |
| Details of tissue removed/altered | 78 | 98 |
| Details of closure technique | 83 | 99 |
| Post-op care and instructions | 80 | 100 |
| Signature | 83 | 100 |
Fig. 1.
Percentage inclusion of specific criteria in audit round 1 and 2: graphical representation
The degree of legibility also improved between audit 1 and audit 2 (Table 2). The number of easily readable operative notes improved from 45 to 63%, while the number of partly illegible operative notes dropped from 53 to 34%, and the number of totally illegible operative notes remaining constant.
Table 2.
Legibility of operative notes, audit round 1 and round 2
| Degree of legibility | Audit 1 | Audit 2 |
|---|---|---|
| Easily readable | 45 | 63 |
| Partly illegible | 53 | 34 |
| Totally illegible | 2 | 3 |
The mean percentage of data point inclusion in audit 1 was 76.1%, which rose to 98.3% in audit 2. Assuming a null hypothesis, the P-value was found to be 0.001 < P < 0.005, demonstrating a statistical significance in the improvement of data point inclusion between audit 1 and audit 2.
Discussion
The quality of the operative note is paramount as an accurate record of in-theatre events. A legible, well structured operative note is a part of best practice medical record keeping, and may prove important in medico-legal cases. Several previous studies have assessed the quality of operative notes [3–8], with all of these finding operative notes lacking in compliance to RCSE guidelines, or respective sub-speciality association guidelines. This represents the same conclusion this author found after our initial audit and the reason for our change in practice.
Evidence exists, and it is acknowledged that the gold standard for operative note keeping is an electronic operative note, either printed and placed in the patients’ case notes, and/or stored in an operative note database [9–12]; thus providing a valuable resource for audit and future research. But even within this area is the option for many further alterations to data input practice. For example, the use of free text entry versus a template based system, or the use of digital dictation. Studies have compared the above methods, and point towards a template based system as being more cost and time effective [13]. It is logical to assume that a template based system, be it electronic or paper based, will increase compliance with set operative note guidelines. By instructing and prompting users to enter data points, you attempt to eliminate operator error. With this is mind, we developed a paper based operative profoma, using a template of data points derived from RCSE guidelines, in an effort to improve operative note quality. One limitation we discovered with this method is the finite space available for documenting operative details; however, one side of A4 was adequate for the majority of our operations. For the small number of larger operations, we used a supplementary sheet, similar in design to the proforma, to provide further writing space.
For many hospitals, the option of a computer based operative note system is unfeasible. Considerations such as cost, staff training, and ongoing maintenance can limit its use to larger hospitals. Several previous papers have described methods aimed at improving the quality of paper based operative notes. Among these are: an aide-memoire sheet placed on the operation sheet [3, 4], a poster in theatre, surgeon education and an operative checklist [14], or an operative note proforma sheet [5, 6]; all have been shown to be effective.
In this paper we put forward further evidence of the effectiveness of a paper based operative note proforma; showing a statistically significant improvement in operative note standards after the introduction our proforma. For those hospitals unable to implement electronic systems, likely to be smaller hospitals, this method represents a cheap and easy method to improve operative note standards, and adhere to RCSE guidelines. In those surgical departments not already using a proforma; we recommend an audit of operative note quality, and the implementation of an operative note proforma.
Further research could look at expanding our proforma into a larger care pathway, including pre and post-operative histology and radiograph reports. The development of language independent universal computer software, allowing operative data input specific to Oral and Maxillofacial Surgery operations would be of great value.
Acknowledgments
Conflicts of Interests The author declares there are no conflicts of interest concerning this article.
Appendix 1
Operative Proforma Sheet

References
- 1.National Confidential Enquiry into Perioperative Deaths. Who Operates When? II, 2003
- 2.Royal College of Surgeons of England. Good Surgical Practice, 2008
- 3.Batemen ND, et al. An audit of the quality of operation notes in an otolaryngology unit. J R Coll Surg Edinb. 1999;44:94–95. [PubMed] [Google Scholar]
- 4.Din R, et al. The use of an aide-memoire to improve the quality of operation notes in an orthopaedic unit. Ann R Coll Surg Engl. 2001;83(5):319–320. [PMC free article] [PubMed] [Google Scholar]
- 5.Al Hussainy H, et al. Improving the standard of operation notes in orthopaedic, trauma surgery: the value of a proforma. Injury. 2004;35(11):1102–1106. doi: 10.1016/j.injury.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Scherer R, et al. Comparison of information obtained by operative note abstraction with that recorded on a standardized data collection form. Surgery. 2003;133(3):324–330. doi: 10.1067/msy.2003.74. [DOI] [PubMed] [Google Scholar]
- 7.Rogers A, et al. The quality of operative notes at a general surgery unit. S Afr Med J. 2008;98(9):726–728. [PubMed] [Google Scholar]
- 8.Mathew J, et al. Quality of operative notes in a district general hospital: a time for change? Internet J Surg. 2003;5(1):1–5. [Google Scholar]
- 9.Brown ML, et al. A pilot study of electronic cardiovascular operative notes: qualitative assessment, challenges in implementation. J Am Coll Surg. 2010;210(2):178–184. doi: 10.1016/j.jamcollsurg.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Atrey A, et al. Interactive computer operative notes for arthroscopy of joints: a free, accurate tool for surgeons. Arthroscopy. 2010;26(6):853–860. doi: 10.1016/j.arthro.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Curral VA, et al. Computer generated operation notes. Stud Health Technol Inform. 2008;137:51–55. [PubMed] [Google Scholar]
- 12.O’Bichere A, et al. The quality of operation notes: can simple word processors help? Ann R Coll Surg Engl. 1997;7(5):204–208. [PubMed] [Google Scholar]
- 13.Laflamme MR et al. (2005) Efficiency, comprehensiveness and cost-effectiveness when comparing dictation and electronic templates for operative reports. AMIA Annu Symp Proc, pp 425–429 [PMC free article] [PubMed]
- 14.Morgan D, et al. Improving operation notes to meet British Orthopaedic Association guidelines. Ann R Coll Surg Engl. 2009;91(3):217–219. doi: 10.1308/003588409X359367. [DOI] [PMC free article] [PubMed] [Google Scholar]