Abstract
Background
HIV prevention interventions often promote monogamy to reduce sexual risk. However, there is little consensus about how to define monogamy.
Objective
Determine the extent to which recent monogamy and/or being in a committed relationship serve as markers for low sexual risk among men in substance abuse treatment.
Methods
Participants were 360 men enrolled in the NIDA Clinical Trials Network “Real Men Are Safe” protocol who completed all assessments (baseline, 3 months, 6 months). Self- reported behaviors included: number of sexual partners; type of relationships; frequency of vaginal/anal intercourse; percentage of condom use.
Results
The rate of self-reported monogamy in the prior 90 days was stable across assessments (54.2%, 53.1%. 58.3%). However, at each assessment 7.5–10% of monogamous men identified their partner as a casual partner, and only 123 (34.2%) reported being monogamous at every assessment. Of these, 20 (5.6%) reported being monogamous with different partners across assessments. Men with both committed relationship and casual partners reported more condom use with their committed relationship partners than men with only a committed relationship partner.
Conclusion
Clinicians and researchers should consider individual relationship context and behavior, and avoid assuming that recent monogamy or being in a committed relationship denotes low risk.
Scientific Significance
This study provides evidence that, in male drug users, monogamy does not necessarily reflect low sexual risk. Rather, ‘monogamous’ men actually encompass various combinations of partner types and levels of risk behavior, that are unstable, even over brief time periods. Clinicians and researchers must take these variations into account.
Introduction
Educational and behavioral interventions aimed at preventing the sexual transmission of HIV and other sexually transmitted infections often promote some version of the ABC model of prevention (1). Sexual abstinence is the only sure way to prevent sexual transmission. Be faithful to a mutually monogamous sexual partner. Use condoms for all penetrative sex acts if not in a long term mutually monogamous relationship. Although complete sexual abstinence is a totally effective prevention strategy and embraced by some, it is generally not a long term strategy that many are willing to adopt (especially those who are sexually experienced). An overall shortcoming of the “be faithful” of the ABC strategy lies in how confident one can be that their partner is also being monogamous (2–5). Serial monogamy may further complicate the message, especially if the amount of time in and between each monogamous relationship is brief (i.e., sexual concurrency) (3,6).
Sexual risk assessments, especially brief assessments in the context of longer intake evaluations, may unintentionally promote the ABC prevention message without appropriate qualifications. Assessors query about being sexually active, number of sexual partners, nature of the relationship with partners, frequency of various sex acts and whether condoms are used for these acts. If an individual says they are not currently sexually active the assessment may end. Information about past relationships, some of which may have been relatively recent, is typically not obtained, nor is information on the likelihood of sexual activity resuming in the future. Similarly an assessment may end if an individual states they are married or in some type of committed relationship, or that they have only had one sex partner in the recent past. Partnership exclusivity and mutual monogamy is assumed without being assessed. This can be especially true in non-HIV specialty settings (7,8). Most of the brief HIV assessment instruments widely used in the field such as the HIV Risk Behavior Scale (9,10), Risk Behavior Survey (11) and Risk Assessment Battery (12) do not assess for partnership expectations for exclusivity, sexual activity prior to a recent time window, or likelihood of resuming sexual activity if currently inactive. The objective of the current study is to ascertain whether a self-report of current monogamy or being in a committed relationship is in fact a good marker for low sexual risk among men attending substance abuse treatment.
Monogamy is not consistently defined in the HIV prevention literature. We recently conducted a Pub Med search for articles that used the term monogamous in the title or abstract. Of the 40 articles identified, 28 were data driven studies related to sexual risk behavior. Most of these studies defined monogamy as having one sexual partner over some time period ranging from 30 days (2,13–17) to one year (13,16,18,19,20,21) with 3 months (13,22–25) and 6 months (18,26–32) being frequent time frames. Four studies did not define monogamy (33–36) and three defined monogamy as “current” with no time frame parameters (37–39). Only two studies assessed whether the respondents thought their partners were being monogamous (2,23). These findings demonstrate a lack of consensus in definitions across studies and the need to clearly define what is meant by monogamy in order to compare results effectively.
The Real Men Are Safe study conducted within the Clinical Trials Network (CTN) of the National Institute on Drug Abuse (NIDA) (40) provided an excellent opportunity to examine these concepts longitudinally. Men enrolled in the trial provided three detailed sexual risk assessments of the previous 90 days at three time points over a six month period.
Methods
Participants
Participants were 360 men enrolled in an HIV risk reduction study that was conducted in 7 methadone maintenance (n = 226) and 7 outpatient, non-medication assisted psychosocial outpatient (n = 134) treatment programs in the United States. These treatment programs were diverse in terms of region, population density, and HIV prevalence rates. Sites were urban (e.g., Philadelphia, PA), suburban (e.g., Norwalk, CT) and rural (e.g., Huntington, WV), and were located in the Northeast, South, Midwest, Southwest, and West. HIV prevalence data at each site were not collected as part of this study, but some sites (e.g., Staten Island, NY; San Francisco, CA) were in cities known to have a higher prevalence of HIV than others (e.g., Santa Fe, NM, High Point, NC). Specific sites are listed elsewhere (40). The study compared a 5-session HIV risk reduction intervention developed specifically for men, Real Men Are Safe (REMAS), to a standard 1-session HIV/AIDS education group intervention (HIV-Ed).
Eligible participants in the parent study (40) were men aged 18 and above who were enrolled in substance abuse treatment, reported engaging in unprotected vaginal or anal intercourse during the prior 6 months, were willing to be randomly assigned to one of two interventions and complete study assessments, and able to speak and understand English. Excluded were men who showed gross mental status impairment defined as severe distractibility, incoherence or retardation as measured by the Mini Mental Status Exam (41,42) or clinician assessment, men who had a primary sexual partner who was intending to become pregnant while the participant was enrolled in the trial, or men who had been in methadone maintenance treatment for less than 30 days. To be included in the current study participants had to complete all three assessments (baseline, 3 months, and 6 months). Participants were recruited between May, 2004 and October, 2005, and were self-referred in response to recruitment posters displayed in clinics, announcements at group therapy meetings and clinic “open houses” designed to introduce the study to clinic patients. Participants were also referred to the study by clinic counselors and/or staff. The HIV status of participants was unknown.
Assessment and Case Identification Procedures
The Sexual Behavior Interview (SBI) was administered as part of the assessment battery at baseline, 3 months post intervention and 6 months post intervention. The SBI items were selected or adapted from the SADAR (Sex and Drug Abuse Relationship Interview (43) and the SERBAS (Sexual Risk Behavior Assessment Schedule (44,45). Behaviors assessed included: 1) number of sexual partners, 2) participant’s relationship with partners, 3) frequency of unprotected vaginal, anal, and oral sex by partner type, and 4) if the main partner was the same main partner identified at earlier assessment time points. SBI items were administered using the audio computer assisted structured interview (ACASI) method often shown to elicit higher levels of risk behaviors than face-to-face interviews (46,47). Participants were identified as being monogamous for the assessment period if they reported only one sexual partner in the prior 90 days. Partnerships were identified as committed if the participant identified their main partner as a “spouse,” “fiancée,” “a lover you've been with for a while,” “a new lover (less than 6 months) with whom you've established a steady relationship.” All other partnerships were characterized as being “casual” relationships. The frequency of engaging in vaginal and anal sex was calculated separately for committed partner and casual partner relationships. Since condom use was known to be infrequent with committed relationship partners (40) condom use with committed relationship partners was dichotomized as “any/none.” For casual partners, condom use for vaginal/anal intercourse was dichotomized at “50% of the time or more.”
Data analysis
To assess representativeness of the sample, t-tests or contingency table analysis utilizing the χ2 statistic were employed to determine if the 360 men for whom full follow-up data were available differed on demographic and monogamy related variables from those men enrolled in the parent study, but for whom follow-up data were not available (n=235). The McNemar test for repeated measurement of dichotomous variables was utilized to assess if the rate of monogamy and involvement in committed or casual relationships changed across the three assessment periods (baseline, 3 and 6 months follow-up). Since 3 pair-wise comparisons were made across time points (baseline/3 months, baseline/6 months, 3 months/6 months) for each variable of interest, a Bonferroni correction was applied and the p-value was set at 0.017 (0.05/3) to minimize the likelihood of type 1 error. At each assessment time point, men in committed relationships who had casual partners were compared to monogamous men in committed relationships on “sexual frequency” utilizing the t-test, and on “any condom use with committed relationship partner” (yes/no) utilizing contingency table analysis and the χ2 statistic. At each assessment time point men in committed relationships who had multiple sexual partners were compared to men who had multiple sexual partners but were not in a committed relationship on “sexual frequency” utilizing the t-test, and on “50% or more condom use with casual partners” utilizing contingency table analysis and the χ2 statistic. To determine if relationship status changed over time during the 90 days preceding each assessment contingency table analysis and the χ2 statistic were utilized. All analyses were conducted using the SPSS Windows software, Version 11.0 (48).
Results
The mean age for participants was 40.4 years (SD = 10.5) and mean years of education completed was 12.2 (SD = 1.8). The sample was 58.9% non-Hispanic white, 26.7% African American, 11.9% Hispanic, and 2.5% reported other racial categories. Being employed full or part time was reported by 43.9% of the sample at baseline assessment. Compared to parent study participants who did not complete all follow-up assessments, participants included in the current study were older (M = 40.3, SD = 12.2 vs. M = 37.1, SD = 12.1 years; t = 3.6, p < .001), less likely to be employed (44.4% vs. 54.9%; χ2 = 6.4, p = .012), and more likely to have been in methadone maintenance (62.8%) than psychosocial outpatient treatment (37.2%, χ2 = 71.2, p < .001). Parent and current study groups did not differ significantly on education or race.
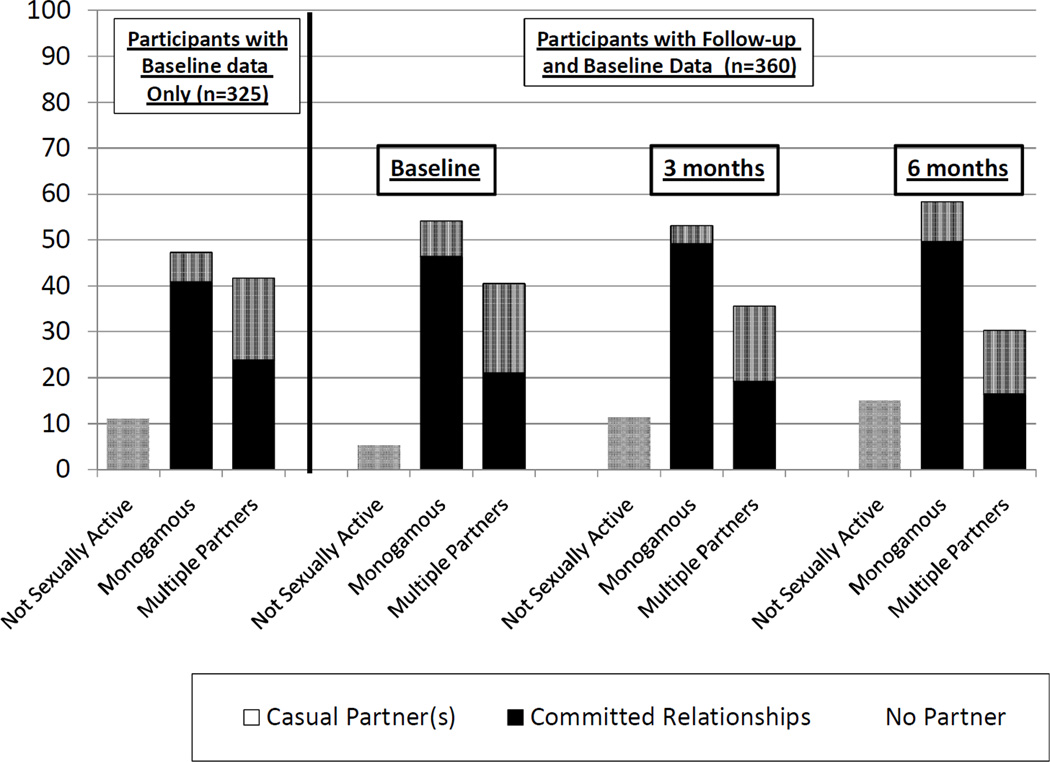
Presented in Table 1 is the number of participants who reported no sex partners, a monogamous sex partner or multiple sex partners for the 90 days prior to each assessment time point for participants with assessments at each time point (n = 360) and the baseline data for men who did not complete all assessments (n = 235). Participants with full follow-up data were more likely to have been sexually active at baseline than participants without full follow-up (χ2= 6.9, p = .009), but did not differ in proportions with multiple partners or in committed relationships. Consistent with participation in an HIV prevention study, the percentage of participants reporting no sexual partner increased from baseline to 3 months (χ2= 10.0, p = .002) and from baseline to 6 months (χ2= 21.0, p < .001), but was not significantly different between 3 and 6 months. The percentage of participants reporting monogamy in the prior 90 days was stable and not statistically different across assessments (53.6 to 58.3). However, at each assessment 13% to 16.7% of the monogamous participants reported their single partner was a casual partner. In addition, only 123 (34.2%) participants reported being monogamous at each assessment. Twenty (5.6%) men, monogamous at each assessment, reported being monogamous with different partners across assessments, Thus, only 103 (28.6%) participants report being monogamous with the same partner in a committed relationship at all three assessment time points. The percent reporting multiple partners significantly decreased from baseline to 6 months (χ2= 21.0, p < .001), and from 3 months to 6 months (χ2= 9.8, p = .002), but was not significantly different between baseline and 3 months. Fewer men with multiple sexual partners at six months reported having a committed relationship partner than men with multiple partners at baseline (χ2= 11.4, p = .001). Changes in monogamy and committed relationship status over the 9 month period assessed, across the three assessment time points, are further illustrated in Figure 1. The proportion not sexually active increases over time and the proportion having multiple sexual partners decrease, while the monogamy rate is fairly constant.
Table 1.
Monogamy and Committed Relationship Status of Participants at Baseline, 3 and 6 Month Follow-up Assessment
| Baseline participants without all follow-up (n=235) |
Baseline participants with all follow-up (n=360) |
3 Month Follow-up (n=360) |
6 Month Follow-up (n=360) |
|
|---|---|---|---|---|
| n (%) | ||||
| No Partners | 26 (11.1)† | 19 (5.3)† | 41 (11.4)# | 54 (15.0)# |
| Monogamous (1 partner) | 111 (47.2) | 195 (54.2) | 191 (53.1) | 210 (58.3) |
| Committed relationship | 96 (40.9) | 167 (46.4) | 177 (49.2) | 179 (49.7) |
| Casual partner | 15 (6.4) | 28 (7.8) | 14 (3.9) | 31 (8.6) |
| Multiple partners | 98 (41.7) | 146 (40.6) | 128 (35.6)# | 96 (26.7)# |
| In a committed relationship | 56 (23.8) | 76 (21.1) | 63 (19.2) | 46 (12.8)# |
| Not in a committed relationship | 42 (17.9) | 70 (19.4) | 65 (16.4) | 50 (13.9) |
Participants without vs with follow-up p = .009
Participants with follow-up, baseline vs. 3 month or 6 month, p ≤.002
Figure 1.
Monogamy and Committed Relationship Status of Participants at Baseline, 3 and 6 month Follow-up Assessment
Presented in Table 2 is the sexual behavior of participants with their committed relationship partners as a function of whether they were monogamous or whether they had casual partners as well. More men with both casual and committed relationship partners reported any condom use with their committed relationship partner than did men who were monogamous with only a committed relationship partner at baseline (Baseline only participants [χ2= 4.4, p < .037]; participants with follow-up [χ2= 6.2, p < .013]) and at the six month follow-up (χ2= 5.3, p = .021). At the 3 month follow-up the trend is similar, but did not attain statistical significance. These differences cannot be explained by the frequency of engaging in vaginal/anal intercourse, as it was not significantly different between the monogamy/non-monogamy groups at any assessment time point.
Table 2.
Sexual Behavior in the Prior 90 Days with Committed Partners for Men Who Were or Were Not Monogamous at Baseline, 3- and 6-Month Follow-up Assessments
| Baseline participants without all follow-up (n=152) |
Baseline participants with all follow-up (n=245) |
3 Month follow-up (n=270) |
6 Month follow-up (n=251) |
|
|---|---|---|---|---|
| n / total (%) | ||||
| Any Condom Usea | ||||
| Had committed partners only | 14 / 83 (16.9) | 28 / 162 (17.3) | 41 / 161 (25.5) | 46 / 168 (27.2) |
| Had committed & casual partners | 16 / 49 (32.7)* | 24 / 76 (31.6)** | 18 / 51 (35.3) | 20 / 44 (45.5) * |
| Vaginal / Anal Sex Occasions | M (SD) / n | |||
| Had committed partners only | 28.7 (30.8) / 96 | 26.3 (35.1) / 169 | 22.4 (26.9) / 184 | 27.2 (31.2) / 193 |
| Had committed & casual partners | 24.3 (29.1) / 56 | 27.9 (36.3) / 76 | 16.8 (25.9) / 86 | 24.5 (28.9) / 58 |
p < .05,
p ≤.01 (committed & casual partners > committed partners only)
Not included in these analyses are partnerships in which no sexual activity or only oral sex occurred during the reporting period.
Presented in Table 3 is the sexual behavior of participants with their casual partners as a function of whether they also had a committed relationship partner. At the 3 month follow-up more men with only casual partners reported using condoms for at least half of casual partner vaginal/anal intercourse occasions than those who also had a committed relationship partner (χ2= 15.6, p < .001). At the 6 month follow-up the trend is similar, but did not attain statistical significance. These differences cannot be explained by the frequency of engaging in vaginal/anal intercourse as it was not significantly different between those with or without a committed relationship partner. The percentage of men having multiple sexual partners during the 90 days prior to each assessment did not vary by HIV intervention prevention assignment condition (Real Men Are Safe versus HIV Education).
Table 3.
Sexual Behavior in the Prior 90 Days with Casual Partners for Men Who Were or Were Not in Committed Relationships at Baseline, 3- and 6-Month Follow-up Assessment
| Baseline participants without all follow-up (n=113) |
Baseline participants with all follow-up (n=172) |
3 Month Follow-up (n=175) |
6 Month Follow-up (n=148) |
|
|---|---|---|---|---|
| n / total (%) | ||||
| Condoms Used for ≥ 50% of Vaginal / Anal Sex Occasionsa | ||||
| Had casual partners only | 27 / 53 (50.9) | 45 / 91 (49.5) | 56 / 77 (72.7) | 48 / 79 (60.8) |
| Had casual & committed partners | 18 / 50 (36.0) | 32 / 71 (45.1) | 23 / 59 (38.0) ** | 19 / 42 (45.2) |
| Vaginal / Anal Sex Occasions | M (SD) / n | |||
| Had casual partners only | 33.5 (48.0) / 57 | 27.8 (39.6) / 96 | 27.7 (45.2) / 99 | 27.9 (53.4) / 90 |
| Had casual & committed partners | 20.1 (29.1) / 56 | 24.5 (40.9) / 76 | 23.1 (34.6) / 76 | 20.4 (23.8) / 58 |
p < .01 (casual partners only > casual & committed partners)
Not included in these analyses are partnerships in which no sexual activity or only oral sex occurred during the reporting period.
Discussion
Although over half the sample reports being monogamous during the 90 days prior to each assessment, only 28.6% were monogamous with the same partner in a committed relationship throughout the 9 month assessment period. Thus, a quarter of the sample was serially monogamous during the study time period; i.e., monogamous with one partner at one 90 day assessment, and monogamous with a different partner at a future 90 day assessment.
Although we do not know about the behavior of the respondents’ partners in the current study, there were likely some partners who considered their male study participant partner to be monogamous when in fact he was not. Consistent with other work (3), the current study found that at each assessment time point slightly over half of the men who reported having multiple sex partners in the prior 90 days also reported having a regular partner in a committed relationship. We did not ask these men if there was an expectation of exclusivity in their committed partner relationship, nor did we ask about temporal relationship between multiple partners. Thus, we do not know if the multiple partners were a form of serial monogamy or of concurrent (simultaneous) relationships with a steady and a non-steady partner. From a clinical standpoint, these data point to the potentially erroneous assumption that a currently monogamous person is at low risk, or that being in a committed relationship denotes low risk. Previous studies show that it is common to have a main sexual partner and a non-steady partner concurrently within relatively short periods of time (e.g., 3 months (3), 12 months (2)). Therefore, the clinician assessing sexual risk needs to go beyond asking about number of recent partners or about a current main partner. Questions assessing for type of partnership, exclusivity expectations and evidence of a pattern of serial monogamy should be included in all conversations assessing sexual risk. Condom use questions should be asked even for monogamous and committed relationship partners. As this study and others (2) have shown, men in committed relationships who had multiple partners are often not using condoms with either their committed relationship partner or their casual partners. In addition, there is a need to repeat assessments on a regular basis, as clearly relationship patterns and partners can change quickly over a short period of time.
The findings from this study highlight a potential shortcoming in the ABC model of HIV prevention. Like the research literature on monogamy, the “be faithful/monogamous” message is not clearly defined, nor is it sufficient to reduce sexual risk due to its unrealistic simplicity. For example, serial monogamy (consistent with “be faithful/monogamous”) was actively practiced among the current study sample, but the risk of this relationship pattern is unknown. Possible risks of serial monogamy include believing your partner to be monogamous when in fact he/she is not, and the length of the relationship being insufficient (i.e., < 6 months) for the recommended window for HIV testing accuracy. The condom use findings from this study further highlight the risks. Although men with both casual and committed relationship partners were more likely to have used condoms with their committed relationship partner than men without casual partners, any use of condoms with a committed relationship partner by these men was very low. Furthermore, the majority of men with both committed relationship and casual partners did not use condoms frequently with their casual partners either, thus putting themselves and their partners at increased sexual risk.
A difficult tight rope for HIV prevention interventionists to walk is encouraging people to protect themselves and their partners by using condoms without sowing seeds of distrust in relationships that may be very important to clients. For clinicians, making a distinction between short-term and long-term monogamy, and clearly defining what is meant by those terms, may facilitate assessment of risk exposure in their patients. For patients, this study and others (2, 40) provide converging evidence that a focus on condom use alone is an insufficient HIV/STD prevention strategy. Given the complexities of sexual relationship partner status, interventions are needed that teach other risk-reduction skills for use in committed and casual relationships. For example, teaching communication skills that facilitate topics such as sexual/personal safety negotiation, expectations about sexual exclusivity and conflict resolution; actively using HIV testing as a risk reduction method; and increasing awareness of partner risk, could be very relevant to a variety of relationship types.
For some purposes it would be useful to have well-articulated and universally accepted definitions for monogamy in both research and clinical practice. The following are a set of possible questions that may provide a start to this conversation. Should monogamy be defined by the respondent or by the reported number of partners for a standardized time period? If the latter, what should that time period be (e.g., 90 days, 6 months, 1 year)? Is there benefit to distinguishing between long term and short term monogamy? If so, what do “long term” and “short term” mean? Should the nature of the relationship (committed vs. non-committed, main vs. casual partner) be considered when defining monogamy? Should partnership expectations for exclusivity be required for a relationship to be considered monogamous? Formative qualitative research could be conducted with both researchers in the field, as well as substance abusing individuals in and out of substance abuse treatment, to assist in arriving at a consensus for terms and definitions. It is beyond the scope of this paper to make these determinations for the field. However, we would support efforts to build a consensus among researchers and clinicians for defining monogamy and incorporating the definition into measures used in future studies and assessments developed for use in practice.
Several limitations of the current study should be considered to place the results in context. Although the study was conducted in a variety of settings and had few exclusion criteria, the limits on generalizability of the findings in terms of client factors such as self-referral to the study, age, type of substance of abuse, psychiatric and substance abuse diagnosis, and sexual history, have not been explored. Findings are based on self-report of sexual behavior with no attempt to verify data by other means. Findings are limited to adult men in outpatient substance abuse treatment.
Acknowledgments
Support and Acknowledgements
The authors wish to thank the research staff and participants at each of the 14 participating treatment programs. This study was supported by the National Institute on Drug Abuse (NIDA) Clinical Trials Network grants: U10 DA13714, U10 DA13035. The trial is registered with ClinicalTrials.gov, a Service of the US National Institutes of Health, Number NCT00084175, http://www.clinicaltrials.gov/
This study was supported by the National Institute on Drug Abuse (NIDA) Clinical Trials Network grants: U10 DA13714, U10 DA13035
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1. [Accessed July 6, 2010];The ABC Approach: Preventing the Sexual Transmission of HIV. Available at http://www.usaid.gov/our_work/global_health/aids/TechAreas/prevention/abcfactsheet.html#approach.
- 2.Riehman KS, Wechsberg WM, Francis SA, Moore M, Morgan-Lopez A. Discordance in monogamy beliefs, sexual concurrency, and condom use among young adult substance-involved couples: implications for risk of sexually transmitted infections. Sex Transm Dis. 2006;33:677–682. doi: 10.1097/01.olq.0000218882.05426.ef. [DOI] [PubMed] [Google Scholar]
- 3.Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban M. Sexual partner concurrency among STI clinic patients with a steady partner: Correlates and associations with condom use. Sex Transm Infect. 2009;85:343–347. doi: 10.1136/sti.2009.035758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thorburn S, Harvey SM, Ryan EA. HIV prevention heuristics and condom use among African-Americans at risk for HIV. AIDS Care. 2005;17:335–344. doi: 10.1080/09540120412331299762. [DOI] [PubMed] [Google Scholar]
- 5.Drumright LN, Gorbach PM, Holmes KK. Do people really know their sex partners? Concurrency, knowledge of partner behavior, and sexually transmitted infections within partnerships. Sex Transm Dis. 2004;31:437–442. doi: 10.1097/01.olq.0000129949.30114.37. [DOI] [PubMed] [Google Scholar]
- 6.Adimora AA, Schoenbach VJ, Doherty IA. Concurrent sexual partnerships among men in the United States. Am J Public Health. 2007;97(12):2230–2237. doi: 10.2105/AJPH.2006.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khan A, Plummer D, Hussain R, Minichiello V. Sexual risk assessment in general practice: evidence from a New South Wales survey. Sexual Health. 2007;4:1–8. doi: 10.1071/sh06012. [DOI] [PubMed] [Google Scholar]
- 8.Kahle E, Zhang Q, Golden M, Goldbaum G, Buskin S. Trends in evaluation for sexually transmitted infections among HIV-infected people, King County, Washington. Sex Transm Dis. 2007;34:940–946. doi: 10.1097/olq.0b013e31813e0a48. [DOI] [PubMed] [Google Scholar]
- 9.Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5:181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Petry NM. Reliability of drug users' self-reported HIV risk behaviors using a brief, 11-item scale. Subst Use Misuse. 2001;36:1731–1747. doi: 10.1081/ja-100107576. [DOI] [PubMed] [Google Scholar]
- 11.NIDA: Risk Behavior Survey. 3ed. Rockville, MD: National Institute on Drug Abuse, Community Research Branch; 1993. [Google Scholar]
- 12.Metzger DS, Woody G, De Philippis D, McLellan AT, O’Brien CP, Platt JJ. Risk factors for needle sharing among methadone-treated patients. Am J Psychiatry. 1991;148:636–640. doi: 10.1176/ajp.148.5.636. [DOI] [PubMed] [Google Scholar]
- 13.Fierros-Gonzalez R, Brown JM. High risk behaviors in a sample of Mexican-American college students. Psychol Rep. 2002;90:117–130. doi: 10.2466/pr0.2002.90.1.117. [DOI] [PubMed] [Google Scholar]
- 14.Mertz KJ, Finelli L, Levine WC, Mognoni RC, Berman SM, Fishbein M, Garnett G, St Louis ME. Gonorrhea in male adolescents and young adults in Newark, New Jersey: implications of risk factors and patient preferences for prevention strategies. Sex Transm Dis. 2000;27:201–207. doi: 10.1097/00007435-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Kwiatkowski CF, Stober DR, Booth RE, Zhang Y. Predictors of increased condom use following HIV intervention with heterosexually active drug users. Drug Alcohol Depend. 1999;54:57–62. doi: 10.1016/s0376-8716(98)00145-8. [DOI] [PubMed] [Google Scholar]
- 16.Carey MP, Carey KB, Weinhardt LS, Gordon CM. Behavioral risk for HIV infection among adults with a severe and persistent mental illness: patterns and psychological antecedents. Community Ment Health J. 1997;33:133–142. doi: 10.1023/a:1022423417304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacGowan RJ, Brackbill RM, Rugg DL, Swanson NM, Weinstein B, Couchon A, Scibak J, Molde S, McLaughlin P, Barker T, Voigt R. Sex, drugs and HIV counseling and testing: a prospective study of behavior-change among methadone-maintenance clients in New England. AIDS. 1997;11:229–235. doi: 10.1097/00002030-199702000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Toltzis P, Stephens RC, Adkins I, Lombardi E, Swami S, Snell A, Cargill V. Human immunodeficiency virus (HIV)-related risk-taking behaviors in women attending inner-city prenatal clinics in the mid-west. J Perinatol. 1999;19:483–487. doi: 10.1038/sj.jp.7200253. [DOI] [PubMed] [Google Scholar]
- 19.Ward J, Sanson-Fisher R. Prevalence and detection of HIV risk behavior in primary care: implications for clinical preventive services. Am J Prev Med. 1995;11:224–230. [PubMed] [Google Scholar]
- 20.King VL, Jr, Brooner RK, Bigelow GE, Schmidt CW, Felch LJ, Gazaway PM. Condom use rates for specific sexual behaviors among opioid abusers entering treatment. Drug Alcohol Depend. 1994;35:231–238. doi: 10.1016/0376-8716(94)90079-5. [DOI] [PubMed] [Google Scholar]
- 21.Saxon AJ, Calsyn DA, Whittaker S, Freeman G., Jr. Sexual behaviors of intravenous drug users in treatment. J Acquir Immune Defic Syndr. 1991;4(10):938–944. [PubMed] [Google Scholar]
- 22.Connell CM, Gilreath TD, Hansen NB. A multiprocess latent class analysis of the co-occurrence of substance use and sexual risk behavior among adolescents. J Stud Alcohol Drugs. 2009;70:943–951. doi: 10.15288/jsad.2009.70.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban M. Sexual partner concurrency among STI clinic patients with a steady partner: correlates and associations with condom use. Sex Transm Infect. 2009;85:343–347. doi: 10.1136/sti.2009.035758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malow RM, Dévieux JG, Jennings T, Lucenko BA, Kalichman SC. Substance-abusing adolescents at varying levels of HIV risk: psychosocial characteristics, drug use sexual behavior. J Subst Abuse. 2001;13:103–117. doi: 10.1016/s0899-3289(01)00069-4. [DOI] [PubMed] [Google Scholar]
- 25.El-Bassel N, Schilling RF. Drug use and sexual behavior of indigent African American men. Public Health Rep. 1991;106:586–590. [PMC free article] [PubMed] [Google Scholar]
- 26.Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007;45:85–92. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soskolne V, Maayan S. HIV knowledge, beliefs and sexual behavior of male heterosexual drug users and non-drug users attending an HIV testing clinic in Israel. Isr J Psychiatry Relat Sci. 1998;35:307–317. [PubMed] [Google Scholar]
- 28.Wells EA, Clark LL, Calsyn DA, Saxon AJ, Jackson TR, Wrede AF. Reporting of HIV risk behaviors by injection drug using heterosexual couples in methadone maintenance. Drug Alcohol Depend. 1994;36:33–38. doi: 10.1016/0376-8716(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 29.McDonald C, Loxley W, Marsh A. A bridge too near? Injecting drug users' sexual behaviour. AIDS Care. 1994;6:317–326. doi: 10.1080/09540129408258643. [DOI] [PubMed] [Google Scholar]
- 30.Hingson R, Strunin L, Craven DE, Mofenson L, Mangione T, Berlin B, Amaro H, Lamb GA. Survey of AIDS knowledge and behavior changes among Massachusetts adults. Prev Med. 1989;18:806–816. doi: 10.1016/0091-7435(89)90016-9. [DOI] [PubMed] [Google Scholar]
- 31.Dolezal C, Meyer-Bahlburg HF, Liu X, Ehrhardt AA, Exner TM, Rabkin JG, Gorman JM, Marder K, Stern Y. Longitudinal changes in sexual risk behavior among HIV+ and HIV- male injecting drug users. Am J Drug Alcohol Abuse. 1999;25:281–303. doi: 10.1081/ada-100101861. [DOI] [PubMed] [Google Scholar]
- 32.Dolezal C, Ehrhardt AA, Meyer-Bahlburg HF, Liu X, Exner TM, Rabkin JG, Gorman JM, Marder K, Stern Y. Sexual risk behavior changes among HIV+ and HIV-female injecting drug users over 4 years. Women Health. 1998;27:1–17. doi: 10.1300/J013v27n04_01. [DOI] [PubMed] [Google Scholar]
- 33.Reingle J, Thombs DL, Weiler RM, Dodd VJ, O'Mara R, Pokorny SB. An exploratory study of bar and nightclub expectancies. J Am Coll Health. 2009;57:629–637. doi: 10.3200/JACH.57.6.629-638. [DOI] [PubMed] [Google Scholar]
- 34.Newman PA, Zimmerman MA. Gender differences in HIV-related sexual risk behavior among urban African American youth: a multivariate approach. AIDS Educ Prev. 2000;12:308–325. [PubMed] [Google Scholar]
- 35.Boyer CB, Shafer M, Wibbelsman CJ, Seeberg D, Teitle E, Lovell N. Associations of sociodemographic, psychosocial, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. J Adolesc Health. 2000;27:102–111. doi: 10.1016/s1054-139x(99)00113-5. [DOI] [PubMed] [Google Scholar]
- 36.Kramer TH, Mosely JA, Rivera A, Ottomanelli G, Li PW, Bihari B. Condom knowledge, history of use, attitudes among chemically addicted populations. J Subst Abuse Treat. 1991;8:241–246. doi: 10.1016/0740-5472(91)90045-c. [DOI] [PubMed] [Google Scholar]
- 37.Bousman CA, Cherner M, Ake C, Letendre S, Atkinson JH, Patterson TL, Grant I, Everall IP HNRC Group. J Negative mood and sexual behavior among non-monogamous men who have sex with men in the context of methamphetamine and HIV. Affect Disord. 2009;118:84–91. doi: 10.1016/j.jad.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson EH, Jackson LA, Hinkle Y, Gilbert D, Hoopwood T, Lollis CM, Willis C, Gant L. What is the significance of black-white differences in risky sexual behavior? J Natl Med Assoc. 1994;86(10):745–759. [PMC free article] [PubMed] [Google Scholar]
- 39.Chetwynd J, Chambers A, Hughes A. Sexual practices, sexually transmitted diseases and other risk factors for HIV among injecting drug users. Aust J Public Health. 1993;17:32–35. doi: 10.1111/j.1753-6405.1993.tb00101.x. [DOI] [PubMed] [Google Scholar]
- 40.Calsyn DA, Hatch-Maillette M, Tross S, Doyle SR, Crits-Christoph P, Song YS, Harrer JM, Lalos G, Berns SB. Motivational and Skills Training HIV/STI Sexual Risk Reduction Groups for Men. J Subst Abuse Treat. 2009;37:138–150. doi: 10.1016/j.jsat.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading cognitive state of patients for the clinician. J Psychiat Res. 1975;12:196–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 42.Cockrell JR, Folstein MF. Mini-Mental State Examination. Psychopharmacol Bull. 1988;24:689–692. [PubMed] [Google Scholar]
- 43.Calsyn DA, Wells EA, Saxon AJ, Jackson R, Heiman JR. Sexual activity under the influence of drugs is common among methadone clients. In: Harris LS, editor. Problems of Drug Dependence 1999, NIH Pub. No. 00-4773. Rockville, MD: National Institute on Drug Abuse; 2000. p. 315. [Google Scholar]
- 44.Meyer-Bahlburg H, Ehrhardt A, Exner TM, Gruen RS. Sexual Risk Behavior Assessment Schedule--Adult Armory Interview (SERBAS-A-ARM) New York: New York State Psychiatric Institute and Columbia University; 1991. [Google Scholar]
- 45.Sohler N, Colson PW, Meyer-Bahlberg HFL, Susser E. Reliability of self reports about sexual risk behaviors for HIV among homeless men with severe mental illness. Psychiatr Serv. 2000;51:814–816. doi: 10.1176/appi.ps.51.6.814. [DOI] [PubMed] [Google Scholar]
- 46.Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S. Randomized controlled trial of audio computer-assisted self-interviewing: Utility and acceptability in longitudinal studies. Am J Epidemiol. 2000;152:99–106. doi: 10.1093/aje/152.2.99. [DOI] [PubMed] [Google Scholar]
- 47.Gross M, Holte SE, Marmor M, Mwatha A, Koblin BA, Mayer KM. Anal sex among HIV-seronegative women at high risk of HIV exposure. J Acquir Immune Defic Syndr. 2000;24:393–398. doi: 10.1097/00126334-200008010-00015. [DOI] [PubMed] [Google Scholar]
- 48.SPSS for Windows, Release 11.0. Chicago, IL: SPSS Inc.; 2001. [Google Scholar]