Abstract
Objectives
This study's objective was to examine the effectiveness of Sanyinjiao point (SP6) acupressure on women's general health.
Design
This was a randomized, single-blind clinical trial.
Setting
The setting for this trial was at Medical University, Bojnoord University of Medical Science, Bojnoord, Iran.
Materials and methods
Eighty-six (86) university students were recruited for this study. Their demographic characteristics were gathered before the intervention commenced. Participants completed General Health Questionnaires (GHQ) prior to participation. Next, they were randomly assigned to either the acupressure-receiving group or the sham-pressure-receiving group. The study group received acupressure at the Sanyinjiao point, while the control group received sham pressure.
Outcome measures
Both groups completed GHQ after both the first and second months of intervention. Data analysis was carried out using SPSS version 13.5 for Windows.
Results
The mean age of those who completed the study was 20.84±1.64 years. Mean scores of GHQs were similar between groups before intervention (p>0.05). The general health of participants in both groups improved after intervention, and the amelioration in four domains was significant in the groups (p<0.05 within group). It was found that acupressure was more effective than sham pressure. In addition, there was a statistically significant difference between the two groups in the four domains of their general heath after the first month of the intervention (p<0.0001). Furthermore, the general health status of the participants changed much more after the second month in both the acupressure intervention and the sham pressure groups; nevertheless, acupressure was more effective than sham pressure (p<0.05).
Conclusions
Both acupressure and sham pressure were effective in promoting women's general health; nevertheless, the efficacy of acupressure was more than that of sham pressure. SP6 acupressure could be regarded as a self-manageable approach to improve women's general health.
Introduction
Awide range of factors are associated with the mental well-being elements included in the World Health Organization (WHO) definition of health: “A state of complete physical, mental and social well-being, and not merely the absence of disease.”1 Mental health is an essential and integral part of general health as a whole. Individuals who are mentally healthy are in a condition of well-being and capability. In addition, they have stress-coping skills, can be productive at work, and contribute to their community. It can be said that the mental health and general health of human beings affect each other.2
Many diverse conditions can affect psychologic status and general health of both men and women, and in turn disturb their mental health. It has been documented that the rate of mental disorders is higher in women than that of men, which is partly because of fluctuations in sex hormones during the menstrual cycle.3 Several prominent symptoms, including irritability, tension, unhappiness, stress, anxiety, insomnia, headache, fatigue, mood swings, increased emotional sensitivity, and changes in libido have been demonstrated to affect women's mental health status and disturb their quality of life before and during menstrual bleeding.4 Many treatments have been suggested to improve women's mood changes and their quality of life before and during menstrual bleeding, including diet or lifestyle changes, vitamins, minerals, chemical medicines, and other supportive means,5 although there is no unanimity in the literature on the most useful medical treatment. In addition, many women may experience complications through potential serious effects of some of these approaches, in spite of their well-known benefits.6,7 Thereby, some women look for alternative therapies, such as acupressure, to promote their general health status while they experience mood changes during menstrual bleeding.8,9
Acupressure is a complementary medical therapy in which physical pressure is applied manually to specific points on the body with or without various devices in order to balance the internal function of the body.10,11 Acupressure has been used in various clinical trials,12 and has been shown to be free from some of the side-effects of other alternative therapies such as transcutaneous electrical nerve stimulation, spinal manipulation, and aromatherapy effects.13 Additional data also provide support for a biologic relationship between acupressure and the relief of psychologic symptoms such as depression, anxiety, and fatigue.14–16 Therefore, this single blind, randomized, placebo-controlled study was conducted in order to evaluate the effect of acupressure on individuals' general and mental health status.
Materials and Methods
A single-blind, randomized, placebo-controlled clinical trial was conducted at the University of Medical Sciences in Iran during 2008. The protocol received institutional review board approval. Permission to conduct the study and access to the female students were obtained from the director of the Medical University. The Medical Research Ethics Committee of Shiraz University of Medical Sciences approved the study prior to commencement, and permission was obtained from the Dean of Faculty, the Deputy of Educational Affairs, and the Educational Affairs Administration of University of Medical Sciences to conduct the study in the setting.
A total of 86 full-time female students studying at the University of Medical Sciences participated in the study. An informed consent form was signed by each participant before entering the study and the confidentiality and anonymity of the study were guaranteed.
The inclusive criteria were (1) having regular menstrual cycles (3–8 days of menstruation with intervals of 22–35 days); (2) not taking any medication such as hormonal contraceptives, antipsychotics, antidepressants, vitamins; (3) not suffering from any psychiatric disorder, such as major depressive disorder, panic disorder, or epilepsy; and (4) being a resident at the university's dormitory.
Exclusion criteria were (1) acquiring General Health Questionnaire (GHQ) scores more than 23; (2) suffering from any kind of psychiatric disorders; (3) consumption of any kind of antidepressants, tranquilizers, and psychiatric medicine; (4) students studying physiotherapy. Individuals who did not meet inclusion criteria were excluded from the study at this stage.
From power calculation, a total of 43 participants in each treatment group, with 31 completing the study, were needed for 80% power to detect a 55% difference in general health scores at the statistical significance level of less than 0.05.
Participants were studied for 2 months. Before commencement of the study, the data on demographics were gathered. A GHQ17 was also used to assess the psychologic status of participants prior to the intervention. It has been shown that the general population has been extensively screened for psychiatric problems by means of the short version of GHQ-28.18,19
The GHQ-28 contains 28 items. It has four subscales evaluating somatic symptoms, anxiety, social dysfunction, and depression. Every item has a 4-point scoring system, ranging from a “better/healthier than normal,” “same as usual,” “worse/more than usual” to a “much worse/more than usual.” Previous studies have confirmed the reliability and validity of the questionnaire.18,19
In the current research study, the Likert scoring method (scoring rages: 0-1-2-3) was used. The cutoff point for GHQ-28 scoring was considered to be 23. Higher scores demonstrated a more severe problem.
Distributed questionnaires were collected after the first menstrual cycle. The participants gaining scores higher than 23 were not considered for the study intervention, and were referred to a psychologist for further assessment and possible treatment. Data from those who had the scores of 23 or less were included in the study. Among them, 86 were randomly allocated to one of the 2 groups as follows: A number was assigned to each questionnaire.
Then, two questionnaires were selected randomly and were placed upside down, so that they could not have been recognized. Then, the researcher allocated one of them to the study group and another one to the control group. Therefore, the first person in each of two study groups was identified. After that, the 84 remaining participants were divided into 42 groups. Each group consisted of 2 persons each. The participants of each pair were then randomly allocated to one of the two groups. This resulted finally in two groups of 43 persons each.
In order to specify the accurate point of SP6 on the participant's leg in the acupressure group (study group), the researcher placed a portable battery-powered point-scope Unit on the lower area of the leg, 5 cm above the medial malleous (SEVESA model, Germany). A red lamp was lit, when the acupressure point, SP6, was right under the Unit.
In order to be able to conduct acupressure on the SP6 point, 1 researcher was trained by an expert clinician.
Acupressure at Sanyinjiao point (above the ankles) was then performed during menstrual bleeding of each participant in the acupressure group. The sham point,20 however, was pressed in participants in the control group (n=43). Navidi et al. indicated: “The sham point was chosen on the dorsal side of the leg, away from meridians and is not situated upon the Achilles tendon. According to the acupressure and acupuncture specialists' recommendation and with regard to the text books, this point is not located on a meridian and pressing it is unlikely to cause any changes in the general health of people.”21,22
One (1) month before commencement of the study, the researcher was trained by an expert. A scale (20 g–6 kg) was used to measure the force of finger pressure. The force of finger pressures was measured 30 times every day, and the pressures concerning 1.21 kg and 3.53 kg were practiced by the researcher.
Participants were positioned prone on an intervention table, having a pillow under their head, shoulders, and knees, on the first day of their menstrual bleeding. Acupressure at the Sanyinjiao (SP6) acupoint was performed alternately on each leg of participants of the study group. The initial force of pressure was 1.21 kg per single pressure action, gradually increasing to 3.53 kg at the end of the pressure round for each leg. The researcher used her thumb to press SP6 for 6 seconds and then released the pressure for 2 seconds, and this cycle was repeated for 30 minutes. In the control group, the sham point was pressed in the same manner. This procedure was repeated for the next consecutive menstrual cycle within each group.
The GHQs were completed by participants immediately after each intervention cycle. In addition, individuals were asked to record any adverse events. After two cycles, questionnaires were collected and data were analyzed. Data analysis was carried out using SPSS version 13.5 for Windows. The independent t test was used to compare the mean scores of general health before and after intervention in each group (α=0.05, confidence interval=95%). In addition, analysis of variance was applied to compare differences in mean scores of general health between groups. Tukey's post-hoc for pair comparison was also performed. Demographic data and study side-effects were summarized by means of descriptive statistics. A p-value less than 0.05 was considered statistically significant.
Results
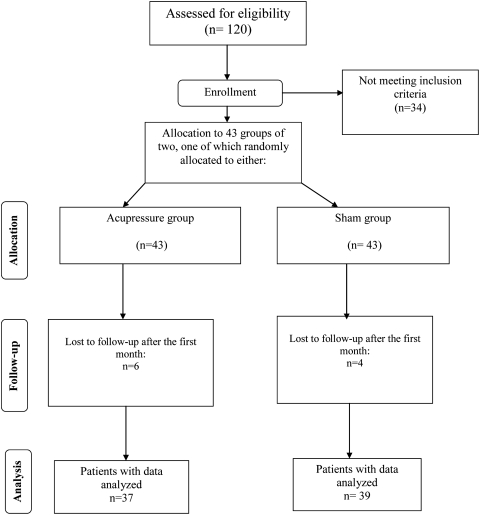
Ten (10) women were considered as dropouts after the first month of intervention (6 on acupressure, 4 on placebo). One (1) of them discontinued intervention, because of a missed period. Five (5) participants were excluded because they used analgesics, and 4 of them were not interested in continuing the participation. Therefore, after the second month of study, the data from 76 participants were available for statistical analysis (Fig. 1). There were no statistically significant differences between those who finished the study and those who did not, in terms of sociodemographic and psychometric status.
FIG. 1.
Flow chart of the participants through each stage of the trial.
The mean age of those who completed the study was 20.84±1.64 years (range 18–28).
The mean scores of the entire GHQ did not differ between groups before intervention (p=0.542) (Table 1). In addition, both groups had similar scores of domains of GHQ prior to the intervention (p>0.05) (Table 2).
Table 1.
Comparison of the Mean Total General Health Scores Among the Two Study Groups Before Interventions, First Month, and Second Month of Interventionsa
| Acupressure | Sham pressure | Significance* | ||
|---|---|---|---|---|
| General health scores | Before intervention | 21.6±3.86 | 21.41±2.45 | F (2177)=2.845 p=0.542 |
| 1st month of intervention | 11.65±3.63 | 15.69±3.14 | F (2163)=38.87 p<0.001 | |
| 2nd month of intervention | 3.99±2.69 | 7.57±2.67 | F (2156)=124.58 p<0.001 |
Values are given as mean±standard deviation.
Tukey's post hoc comparison showed that the difference between acupressure and sham pressure (p<0.001) was statistically significant.
Table 2.
Mean Scores for the Four Domains of General Health Before Intervention in the Two Study Groups
| |
GHQ domains |
|||||||
|---|---|---|---|---|---|---|---|---|
| |
Somatic |
Anxiety |
Social dysfunction |
Depression |
||||
| Group | M | SD | M | SD | M | SD | M | SD |
| Acupressure | 7 | 2.52 | 7.6 | 2.66 | 10.62 | 3.13 | 5.62 | 2.34 |
| Sham pressure | 7.41 | 2.2 | 7.02 | 2.86 | 9.27 | 2.86 | 6.41 | 2.19 |
| Significance | p=0.41 | p=0.33 | p=0.54 | p=0.06 | ||||
| F (2177)=1.78 | F (2177)=1.43 | F (2177)=2.23 | F (2177)=1.94 | |||||
GHQ, General Health Questionnaires; M, mean; SD, standard deviation.
Both SP6 pressure and sham point pressure improved the general health of participants and there was remarkable amendment in the four domains of GHQ in both groups. There were statistically significant changes within groups from before intervention to after the first month of intervention (p<0.05) (Table 3).
Table 3.
Mean Scores of the Four Domains of General Health After the First Month of Intervention in the Two Study Groups
| |
GHQ domains |
|||||||
|---|---|---|---|---|---|---|---|---|
| |
Somatic |
Anxiety |
Social dysfunction |
Depression |
||||
| Group | M | SD | M | SD | M | SD | M | SD |
| Acupressure | 4.81 | 0.09 | 3.83 | 1.31 | 5.63 | 1.04 | 3.12 | 1.41 |
| Sham pressure | 6.09 | 0.73 | 5.3 | 2.47 | 8.7 | 1.98 | 5.58 | 2.67 |
| Significance* | p<0.0001 | p=0.02 | p=0.04 | p=0.02 | ||||
| F (2163)=15.12 | F (2163)=7.76 | F (2163)=8.39 | F (2163)=4.21 | |||||
GHQ, General Health Questionnaires; M, mean; SD, standard deviation.
Tukey's post hoc comparison showed that the difference between acupressure and sham pressure groups (p<0.001) was statistically significant in the four domains.
Although both acupressure and sham pressure had positive effects on participants' general health and its improvement, acupressure was more effective than sham pressure and there were statistically significant differences between the two groups regarding the scores of four domains of general health after the first month of the intervention (p<0.05) (Table 3).
Furthermore, the general health status of the participants changed a lot more after the second month for those who completed the acupressure treatment, and it differed significantly between the first and second months of the intervention (p<0.001). In addition, there was a significant difference between the second month after intervention and before intervention (p<0.05, within group) (Table 4).
Table 4.
Mean Scores of the Four Domains of General Health After Second Month of Intervention in the Two Study Groups
| |
GHQ domains |
|||||||
|---|---|---|---|---|---|---|---|---|
| |
Somatic |
Anxiety |
Social dysfunction |
Depression |
||||
| Group | M | SD | M | SD | M | SD | M | SD |
| Acupressure | 2.07 | 0.99 | 1.13 | 0.24 | 2.41 | 0.85 | 1.71 | 1.06 |
| Sham pressure | 4.52 | 1.45 | 3.21 | 1.76 | 5.07 | 2.95 | 4. 11 | 2.01 |
| Significance* | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| F (2158)=59.99 | F (2158)=47.87 | F (2158)=44.38 | F (2158)=61.12 | |||||
GHQ, General Health Questionnaires; M, mean; SD, standard deviation.
Tukey's post hoc comparison showed that the difference between acupressure and sham pressure (p<0.001) was statistically significant in the four domains.
Likewise, the scores of GHQ decreased after the second month of intervention in participants who completed sham pressure (p<0.05 within group). In addition, there was a significant difference between the second month after intervention and before intervention among participants receiving sham pressure (p<0.05, within group) (Table 4). A treatment comparison between the two groups showed that acupressure was significantly more effective than sham pressure in alleviating the participants' general health scores (p<0.0001) (Tables 1 and 4).
None of the participants reported intervention-related adverse events.
Discussion
To the authors' knowledge, this was the first study in which the effects of acupressure on women's general health before and during their menstrual bleeding were evaluated. The health problems studied for each category included physical illness, tiredness, and headache (somatic domain); sleep difficulties, being under pressure, nervousness, mood changes, and being bad-tempered (anxiety domain); having difficulty coping with different situations, unable to do tasks properly, decision-making problems, and joyless life (social dysfunction domain); feeling worthless, hopeless, and having suicidal thoughts (depression domain). It has already been shown that many women experience psychiatric problems before and during their menstrual bleeding; however, different women demonstrate various patterns of complications 23. Physical or mood changes have been reported by many women during the days when they have menstrual bleeding,4 and “irritability,” “fatigue,” “anxiety,” “nervous tension,” “mood swings,” “depression,” and “feeling overwhelmed or out of control” are among the most frequent and prevalent symptoms.
These changes affect a woman's normal life, her general health, and could induce psychologic instability.24 It was assumed that acupressure might have had a positive influence on the women's psychologic status during their menstrual days. The results of this study showed that both kinds of interventions improved the general health of women; however, acupressure was more effective than sham pressure. Participants were selected among students living in the dormitory (i.e., all residing in the same place), omitted students studying physiotherapy, and conducted a randomized, placebo-controlled, single-blind trial; however, this study faced some limitation.
Limitations of this study were that the authors had to rely on participants' remarks about basic information, and any previous psychologic disorders. In addition, the diet of each participant may affect her mood status, as some nutrients can affect mental health of women25, 26; however, it was not possible to assimilate participants' diet during the study.
Comparing the mean scores of each domains, before and at the end of the intervention, showed that the diminution in “within group scores” of anxiety and social dysfunction (differences of means: −6.47, −8.21, respectively) were more remarkable than those of somatic symptoms and depression in the study group. Equally among four domains of general health, in the group receiving sham pressure, anxiety and social dysfunction were improved the most (differences of means: −3.81, −4.20, respectively). Hence, it can generally be derived that social dysfunction was the symptom that improved the most.
The efficacy of acupressure has been evaluated in various studies. It has been demonstrated that the psychosomatic health of climacteric women can be ameliorated by performing acupressure.27 Furthermore, research studies have reported that the level of anxiety in laboring women,28 the duration and severity of pain during the active phase of labor, the need for cesarean section, and the necessity and amount oxytocin29 are reduced while conducting acupressure in each occasion. Acupressure is also able to reduce the length of delivery time.30 Moreover, it has been demonstrated that the severity of dysmenorrhea can decrease instantly by conducting SP6 acupressure. In addition, SP6 acupressure could palliate the level of menstrual distress due to dysmenorrhea.31
It has also been shown that cognition and controlling of mood in the central nervous system can be modulated by acupressure.32 In addition, the results of another study have revealed that using acupressure bands can diminish the severity of chemotherapy-induced nausea and vomiting in women with cancer.33 Several kinds of acupressure are currently practiced as an alternative therapy, although all of them stimulate the same sensitive spots. Some of the main techniques include “pressing,” “kneading,” “rubbing,” “pushing,” “scrubbing,” “grasping,” “patting,” “rub rolling,” and “wiping.”34 The method used in this study was “pressing”; nevertheless, the authors acknowledge the fact that alternative acupressure techniques may have different effects and may play an important role in certain pathological conditions such as major depression, anxiety disorders, and schizophrenia.35,36
In the current study, the general health status of participants in both groups improved and both acupressure and sham pressure had positive effects on general health scores; however, the scores of the participants receiving acupressure showed more improvement than those of the sham pressure group (p<0.0001).
In addition, promotion of the health status of participants was more remarkable after the second month of intervention than after the first month of intervention. Therefore, it could be supposed that if the treatment period is longer, the acupressure could be more efficient and effective. Nevertheless, further population-based studies with larger sample size and longer follow-up periods are recommended to support the results of this study.
Because both complementary and alternative medicine and depression are highly prevalent among women suffering mood changes,37 it is recommended that this inexpensive and safe approach be taken into consideration while evaluating various treatment strategies for women who suffer from mood swings, or those whose general health status is at risk.
Conclusions
In the present study, acupressure and sham pressure were able to promote women's general health; nevertheless, the positive effect of acupressure was more noticeable than that of sham pressure, and it also was much more remarkable after the second month of intervention.
Acknowledgments
We would like to express our sincere gratitude to the Deputy for Research of Shiraz University of Medical Sciences for financial supports we received (grant 86-3652). The authors would also like to thank the students studying at the University of Medical Science for their cooperation. We would also like to thank Ms. Natasha Trpcevski for contributing to the editing process of the article.
Disclosure Statement
No competing financial interests exist.
References
- 1.Larson J. The World Health Organization's Definition of Health: Social versus spiritual health. Soc Indicators Res. 1996;38:181–192. [Google Scholar]
- 2.Taylor S. Stanton A. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- 3.Rapkin A. A review of treatment of premenstrual syndrome & premenstrual dysphoric disorder. Psychoneuroendocrinology. 2003;28(suppl 3):39–53. doi: 10.1016/s0306-4530(03)00096-9. [DOI] [PubMed] [Google Scholar]
- 4.Freeman EW. Premenstrual syndrome and premenstrual dysphoric disorder: Definitions and diagnosis. Psychoneuroendocrinology. 2003;28(suppl 3):25–37. doi: 10.1016/s0306-4530(03)00099-4. [DOI] [PubMed] [Google Scholar]
- 5.Keye WR. Premenstrual Syndrome (PMS) In: Luciano M, editor. Encyclopedia of Endocrine Diseases. New York: Elsevier; 2004. pp. 73–75. [Google Scholar]
- 6.Wyatt K. Dimmock P. Jones P, et al. Efficacy of progesterone and progestogens in management of premenstrual syndrome: Systematic review. BMJ. 2001;323:776–780. doi: 10.1136/bmj.323.7316.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessel B. Premenstrual syndrome: Advances in diagnosis and treatment. Obstet Gynecol Clin North Am. 2000;27:625–639. doi: 10.1016/s0889-8545(05)70160-1. [DOI] [PubMed] [Google Scholar]
- 8.Bair YA. Gold EB. Zhang G, et al. Use of complementary and alternative medicine during the menopause transition: Longitudinal results from the Study of Women's Health Across the Nation. Menopause. 2008;15:32–43. doi: 10.1097/gme.0b013e31813429d6. [DOI] [PubMed] [Google Scholar]
- 9.Chandra K. Magee L. Einarson A. Koren G. Nausea and vomiting in pregnancy: Results of a survey that identified interventions used by women to alleviate their symptoms. J Psychosom Obstet Gynecol. 2003;24:71–75. doi: 10.3109/01674820309042804. [DOI] [PubMed] [Google Scholar]
- 10.Lee MK. Chang SB. Kang D-H. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10:959–965. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 11.Ezzo J. Vickers A. Richardson MA, et al. Acupuncture-point stimulation for chemotherapy-induced nausea and vomiting. J Clin Oncol. 2005;23:7188–7198. doi: 10.1200/JCO.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal A. Ranjan R. Dhiraaj S, et al. Acupressure for prevention of pre-operative anxiety: A prospective, randomised, placebo controlled study. Anaesthesia. 2005;60:978–981. doi: 10.1111/j.1365-2044.2005.04332.x. [DOI] [PubMed] [Google Scholar]
- 13.Cherkin D. Sherman K. Deyo R. Shekelle P. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 14.Cho Y. Tsay S. The effect of acupressure with massage on fatigue and depression in patients with end-stage renal disease. J Nurs Res. 2004;12:51–54. doi: 10.1097/01.jnr.0000387488.63438.9a. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh L. Kuo C. Lee L, et al. Treatment of low back pain by acupressure and physical therapy: Randomised controlled trial. BMJ. 2006;332:696–700. doi: 10.1136/bmj.38744.672616.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kober A. Scheck T. Schubert B, et al. Auricular acupressure as a treatment for anxiety in prehospital transport settings. Anesthesiology. 2003;98:1328–1332. doi: 10.1097/00000542-200306000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg D. London: Oxford University Press; 1972. The Detection of Psychiatric Illness by Questionnaire: A Technique for the Identification and Assessment of Non-psychotic Psychiatric Illness (Maudsley Monographs No. 21) [Google Scholar]
- 18.Goldberg D. William P. A User Guide to General Health Questionnaire. Windsor: NFER-Nelson; 1988. [Google Scholar]
- 19.Maruyama S. Sato H. Morimoto K. Relationship between work-life satisfaction, health practice and primary symptoms/problems. Nippon Eiseigaku Zasshi. 1991;45:1082–1094. doi: 10.1265/jjh.45.1082. [DOI] [PubMed] [Google Scholar]
- 20.Paul S. Purdy R. Neuroactive steroids. FASEB J. 1992;6:231–232. [PubMed] [Google Scholar]
- 21.Chen H. Chen C. Effects of acupressure at the Sanyinjiao point on primary dysmenorrhea. J Adv Nurs. 2004;48:380–387. doi: 10.1111/j.1365-2648.2004.03236.x. [DOI] [PubMed] [Google Scholar]
- 22.Navidi A. Khedmat H. HeliSaz M. Base of Acupuncture. Tehran: Teymoorzadeh; 2000. [Google Scholar]
- 23.Freeman E. Sondheimer S. Premenstrual dysphoric disorder: Recognition and treatment. Prim Care Companion J Clin Psychiatry. 2003;5:30–39. doi: 10.4088/pcc.v05n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halbreich U. The etiology, biology and evolving pathology of premenstrual syndrome. Psychoneuroendocrinology. 2003;28:55–99. doi: 10.1016/s0306-4530(03)00097-0. [DOI] [PubMed] [Google Scholar]
- 25.Soh N. Walter G. Baur L. Collins C. Nutrition, mood and behaviour: A review. Acta Neuropsychiatr. 2009;21:214–227. doi: 10.1111/j.1601-5215.2009.00413.x. [DOI] [PubMed] [Google Scholar]
- 26.Markus C. Dietary amino acids and brain serotonin function: Implications for stress-related affective changes. NeuroMol Med. 2008;10:247–258. doi: 10.1007/s12017-008-8039-9. [DOI] [PubMed] [Google Scholar]
- 27.Clark C. Complementary Health for Women. New York: Springer Publishing Company; 2009. [Google Scholar]
- 28.Lee M. Effects of San-Yin-Jiao (SP6) acupressure on anxiety, pulse and neonatal status in women during labor. Korean J Women Health Nurs. 2003;9:138–151. [Google Scholar]
- 29.Kashanian M. Shahali S. Effects of acupressure at the Sanyinjiao point (SP6) on the process of active phase of labor in nulliparas women. J Matern Fetal Neonatal Med. 2009;15:1–4. doi: 10.1080/14767050903277662. [DOI] [PubMed] [Google Scholar]
- 30.Lee M. Chang S. Kang D. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10:959–965. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 31.Wong CL. Lai KY. Tse HM. Effects of SP6 acupressure on pain and menstrual distress in young women with dysmenorrhea. Complement Ther Clin Pract. 2010;16:64–69. doi: 10.1016/j.ctcp.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Payne JK. A neuroendocrine-based regulatory fatigue model. Biol Res Nurs. 2004;6:141–150. doi: 10.1177/1099800404268280. [DOI] [PubMed] [Google Scholar]
- 33.Rapkin A. Morgan MM. Goldman M. Progesterone metabolite allopregnanolone in women with premenstrual syndrome. Obstet Gynecol. 1997;90:709–714. doi: 10.1016/S0029-7844(97)00417-1. [DOI] [PubMed] [Google Scholar]
- 34.Ya Li F. Chinese Self-Massage Therapy. 3rd. Boulder, CO: Blue Poppy Press; 2002. [Google Scholar]
- 35.Kim K. Cohen S. Oh H. Sok S. The effects of meridian exercise on anxiety, depression, and self-esteem of female college students in Korea. Holistic Nurs Pract. 2004;18:230–234. doi: 10.1097/00004650-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Samuels N. Gropp C. Singer SR. Oberbaum M. Acupuncture for psychiatric illness: A literature review. Behav Med. 2008;34:55–64. doi: 10.3200/BMED.34.2.55-64. [DOI] [PubMed] [Google Scholar]
- 37.Wu P. Fuller C. Liu X, et al. Use of complementary and alternative medicine among women with depression: Results of a national survey. Psychiatr Serv. 2007;58:349–356. doi: 10.1176/ps.2007.58.3.349. [DOI] [PubMed] [Google Scholar]