ABSTRACT
Myositis ossificans circumscripta (MOC) is an extra-osseous non- neoplastic growth of a new bone. It occurs most commonly in the second and the third decade of life, while it is rare in children. The etiology of MOC is unknown and the quadriceps and brachials are the most affected. The occurrence of traumatic MOC in tissues of the neck is uncommon. We are presenting below a rare case of traumatic myositis ossificans occurring in sternocleidomastoid and trapezius muscles in a 17-year-old girl.
Keywords: neck muscles, local trauma and children
INTRODUCTION
Myositis ossificans (MO) is a benign condition that appears as a heterotopic, well-defined bone formation in muscles and soft tissues (1). It is of three types: - progressive MO (a rare, inherited disorder, characterized by fibrosing and ossification of muscles, tendons and ligaments of multiple sites); - traumatic MOC (appears after local trauma – cited in 60-75% of all cases); - non-traumatic MOC developed after chronic infections, poliomyelitis, but may occur independently of these conditions) (2). The most common sites affected are the hip, anterior thigh (quadriceps) and anterior arm (brachialis) (2). The etiology is unknown, and major injury (dislocations, fractures), or minor trauma are considered as most frequent causes (1).
We will describe an unusual case of a 17-year-old girl who was hospitalized for a tender soft tissue swelling, rapidly growing on the left side of the neck, caused by a minor local trauma. ❑
CASE REPORT
A 17-year-old girl presented a painful tumefaction on the left side of her neck, accompanied with left hemicrania. Her past history revealed that four weeks before hospitalization she had been pricked by an unknown insect. The incident was followed by a local pain and limitation of movement. She received local massage for approximately two weeks. However a few days later a painful mass was noticed on the laterocervical left region.
Physical examination described a painful mass, in the left laterocervical area of the neck, well delimited, with a diameter of approximately 30 mm, with restriction of neck movements. The local temperature was not increased and there was no erythema. An ENT consultation was made and it described a soft tissue swelling localized on the left side of the neck, which affected the posterior edge of sternocleidomastoidian and trapezius muscles. The explanation of hemicrania was a possible nerve compression.
Laboratory tests revealed normal white blood cell count, a slight increase of Erythrocyte Sedimentation Rate (20 mm/hour) and C-reactive protein (2.2 mg/dl) and normal alkaline phosphatase.
There were suspicions of a possible myositis or cellulitis, therefore the patient received an anti-inflammatory drug (Ibuprofen) and an antibiotic treatment (Ceftriaxone: 1gm q24h), but the local changes persisted.
Musculoskeletal ultrasound showed an inhomogeneous mass (sized 30x25x20 mm), vascularized, localized between left sternocleidomastoidian and trapezius muscles, with multiples hiperechogenic images at the periphery - the aspect looks like the "shell egg" (Figure 1).
Figure 1. Left laterocervical US image showing a hypoechogenic enlargement of soft tissue measuring approximately 30x25x20 mm with lamellar hyperreflectivity at the periphery of the mass.

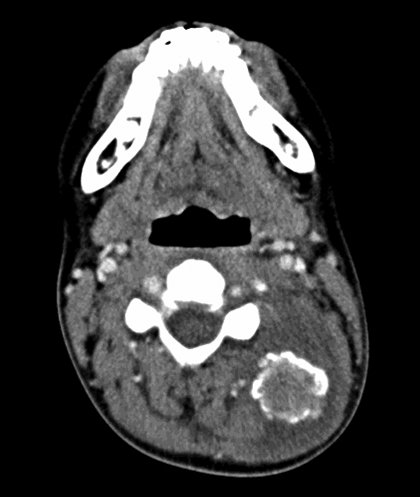
CT scan revealed a peripheric ossification of the lesion with a central inhomogeneous area. There was associated perilesional edema (Figure 2).
Figure 2. CT scan of the neck. Axial image shows a mass with a rim of calcification, with varying thickness at the periphery.
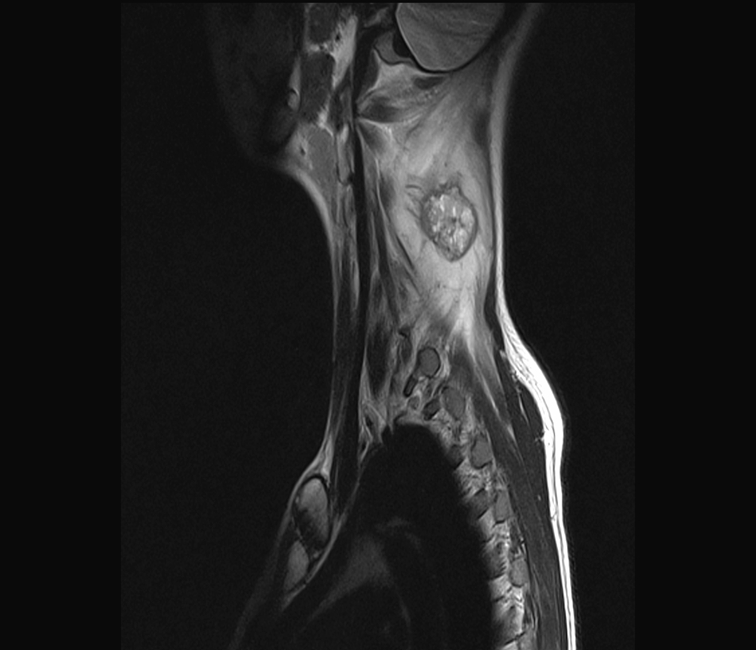
The MRI with and without intravenous contrast described an inhomogeneous soft tissue lesion, well defined, in the left posterior-lateral cervical triangle and the inflammation of the lateral and posterior neck muscles (Figure 3).
Figure 3. Parasagittal image shows an inhomogeneous mass well defined, surrounded by a frame of lower signal intensity, signifying cortical calcification, with perilesional edema along the muscle fibres.
Because of the persistent local modifications, the intractable local pain, the left hemicrania and the restriction of movements, a surgery excision was performed. The mass was excised totally and the histopathologic examination found myositis ossificans, characterized by many large vascular spaces separated by septums consisting of fibroblasts and myofibroblasts cells. At the periphery, the lesion presented lamellar bone delimited by osteoblasts.
After the surgical excision, the patient's clinical course was favorable, the pain disappeared and there was no more limitation of movement, so, she left home in good condition.
Three months after surgery, the patient was reassessed. She attained substantial improvement in neck joint mobility as a result of bone excision and the pain was gone. Local physical examination revealed the post surgery scar but there were no other pathological changes. Musculoskeletal ultrasound also showed no pathological modifications.
One year later, the patient was in good condition and the laterocervical ultrasound showed no specific changes, fact that excluded the post-operative recurrences.
We must draw attention to the fact that after contusion, swelling, muscles injuries, the local massage is not recommended. Therefore, in our case also the massage performed was an error and it should have been avoided. ❑
DISCUSSIONS
Myositis ossificans traumatica (MOT) is a benign disorder of heterotopic bone formation occurring in response to soft tissue trauma. Often, it can be caused by minor or major trauma (60-75% of cases), being a result of muscle injury (3). In our case, the patient had suffered a minor trauma: an unknown insect pricked her and after that she received intensive local massage. MO is rare in childhood (57 cases have been reported in the literature) (1) and more frequently in teenage athletes and over 50% of cases are diagnosed in the third decade of life (3). The most affected muscles are those of the extremities (4). A correct diagnostic of MO must be three-dimensional, based on clinical examination, radio-imaging and histological examination. In approximately 1-2 weeks after the injury, MOT developpes as a rapid significant pain and soon after that, the patient presents a local tumefaction. Laboratory tests usually are normal, as in our case, but sometimes an increase of Erythrocyte Sedimentation Rate and serum alkaline phosphatase can be observed (5). Radio-imaging reveals that in 1-2 weeks after local trauma, a not well defined zone of peripheral calcification may appear. At 2-4 weeks after injury, it appears like a round mass with margin of mature peripheral calcification, well defined from surrounding tissues. The center of the mass is more radiolucent, consisting of immature osteoid and primitive mesenchymal tissues. Mature calcification will progress towards the center of the mass (6). On MRI imaging MOC appears as a well-defined, inhomogeneous soft-tissue mass, surrounded by a frame of lower signal intensity, signifying cortical calcification (4). CT scan helps delineate a central radiolucency, surrounded by a dense periphery (5).
The differential diagnosis that should be taken into discussion can be non-neoplastic disorders (calcified fibromatosis, local infections) and malignant tumors (lymphoma, osteosarcoma, rhabdomyosarcoma). The most frequently clinical misdiagnoses are tumor, especially osteosarcoma (1). In our case, the radio imaging (musculoskeletal ultrasound, CT scan and MRI) made us think about the possibility of a myositis ossificans or an osteosarcoma. Between these two entities, there are several differences: if in MO the pain tends to decrease in time, in osteosarcoma the pain tends to increase and another difference is that in MO the calcification begins at the periphery and progresses towards the center, while in osteosarcoma it begins at the center and continues to the periphery (5).
Other misdiagnoses that might be taken into consideration is lymphoma. In the first stage of the disease the lymph nodes are soft, but in the course of illness, they become firm and elastic. These lymph nodes are not painful, yet they are generally accompanied by fever, night sweats, and weight loss (7). Our patient did not have the symptoms described above: she presented a soft tissue swelling in the left laterocervical area of the neck, there was no fever and she did not lose weight.
Microscopically, the developing lesion presents three zones. Ackerman named it the "zone phenomena" and it is an important criterion for the diagnosis of MO. The central zone contains extreme variation of cells and atypical mitotic figures; the middle zone contains orientated osteoid, and the outer zone (periphery) has well formed bone (8).
Myositis ossificans is a benign, self-limiting disease. The treatment in most cases is conservative; it consists of rest, ice and anti-inflammatory drugs to relieve pain. Physiotherapy can also help improve movements by performing passive and active motion. Typically, a regression of the symptoms is seen in the course of disease (30%) (9). A spontaneous resorption or an incomplete regression can occur (10). Surgical intervention is recommended when the heterotopic bone has matured. The optimum time for a surgery excision is between 9 and 12 month after the trauma (11).
It is also recommended if it interferes with joint motion, functional limitation or if it generates a significant pain, due to the compression of nerve trunk (12), or in cases of dubious etiology (4). In conclusion, the mark of this case is the unusual localization for a MO, followed by a local minor trauma and the fact that a surgery excision was performed earlier because of the persistent local modifications, the intractable local pain, the left hemicrania and the limitation of function. Ultrasonography, CT scan and MRI show approximately the same aspects that suggest a possible MO, but the histological examination confirms the diagnosis. ❑
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
All authors were inlvolved in the clinical care of the patient and drafting of the manuscript. All authors have read and approved the final manuscript.
References
- 1.Micheli A, Trapani S, Brizzi I, et al. Myositis ossificans circumscripta: a pediatric case and review of the literature. Eur J Pediatr. 2009;168(5):523–529. doi: 10.1007/s00431-008-0906-8. [DOI] [PubMed] [Google Scholar]
- 2.Patel S, Richards A, Trehan R, et al. Post-traumatic myositis ossificans of the sternocleidomastoid following fracture of the clavicle: a case report. Cases J. 2008;1:413–413. doi: 10.1186/1757-1626-1-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Messina M, Volterrani L, Molinaro F, et al. Myositis ossificans in children: description of a clinical case with a rare localization. Minerva Pediatr. 2006;58(1):69–72. [PubMed] [Google Scholar]
- 4.Kokkosis A, Balsam D, Lee TK, et al. Pediatric nontraumatic myositis ossificans of the neck. Pediatr. Radiol. 2009;39(4):409–412. doi: 10.1007/s00247-009-1165-1. [DOI] [PubMed] [Google Scholar]
- 5.Cushner FD, Morwessel RM. Myositis ossificans traumatica. Orthopaedic Review, 1992:1319–1326. [PubMed] [Google Scholar]
- 6.Tyler W. Myositis ossificans. Orthopaedia. Colaborative Orthopaedic Knowledgebase. 2008:15–16. [Google Scholar]
- 7.Hoppe RT, Mauch PM, Armitage JO, et al. Hodgkin lymphoma. 2007;(2) [Google Scholar]
- 8.Ackermann LV. Extra-osseous localized non neoplastic bone and cartilage formation (so called myositis ossificans). J. Bone Joint Surg. Am. 1958;40(2):279–298. [PubMed] [Google Scholar]
- 9.Wang XL, Malghem J, Parizel PM, et al. Myositis ossificans circumscripta. JBR - BTR. 2003;86:278–285. [PubMed] [Google Scholar]
- 10.Rossler H. Myositis ossificans circumscripta. Ped. Rad. (serial online) 4(6). [Google Scholar]
- 11.Oh KS, Moissinac K, Chong Se To B. Childhood myositis ossificans: early surgery can help. Sicot Case-Reports: 2002 May [Google Scholar]
- 12.Chadha M, Agarwal A. Myositis ossificans traumatica of the hand. Can. J. Surg. 2007;50(6):E21–E21. [PMC free article] [PubMed] [Google Scholar]


