Abstract
The last decade saw increased organ donation activity from donors after cardiac death (DCD). This contributed to a significant proportion of transplant activity. Despite certain drawbacks, liver transplantation from DCD donors continues to supplement the donor pool on the backdrop of a severe organ shortage. Understanding the pathophysiology has provided the basis for modulation of DCD organs that has been proven to be effective outside liver transplantation but remains experimental in liver transplantation models. Research continues on how best to further increase the utility of DCD grafts. Most of the work has been carried out exploring the use of organ preservation using machine assisted perfusion. Both ex-situ and in-situ organ perfusion systems are tested in the liver transplantation setting with promising results. Additional techniques involved pharmacological manipulation of the donor, graft and the recipient. Ethical barriers and end-of-life care pathways are obstacles to widespread clinical application of some of the recent advances to practice. It is likely that some of the DCD offers are in fact probably “prematurely” offered without ideal donor management or even prior to brain death being established. The absolute benefits of DCD exist only if this form of donation supplements the existing deceased donor pool; hence, it is worthwhile revisiting organ donation process enabling us to identify counter remedial measures.
Keywords: Non-heart beating donor, Liver graft, Primary non-function, Reperfusion injury, Modulation
INTRODUCTION
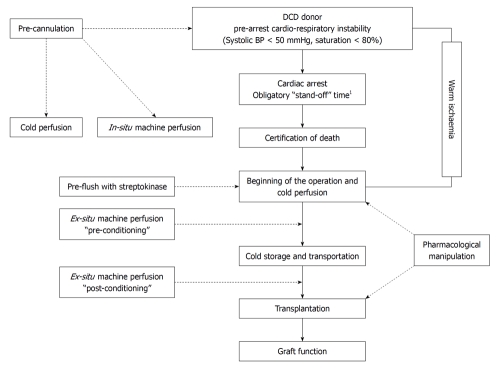
The current literature suggests that outcomes of liver transplantation using organs from donors after cardiac death (DCD) are nearly comparable to that of donors after brain death (DBD) or live donor transplants[1-3]. However, these results are obtained at the expense of significant peri-operative and long term morbidity to the recipient and add substantial cost to the health economics. In countries where transplant programs depend on deceased donors for the supply of organs, there appears to be a recent increase in DCD numbers. In the United Kingdom alone, DCD activity contributed up to 35% of deceased donor transplants in the year 2009-2010. The United Network for Organ Sharing (UNOS) data suggests similar trends, with DCD accounting up to 10% of overall transplant activity. The initial euphoria of DCD as a viable and alternative organ source is diminishing with the realisation that these DCD organs have contributed to an increased number of transplants at the expense of DBD organs (Figure 1).
Figure 1.
Data from the Queen Elizabeth Hospital Birmingham Liver Transplant Unit. (A) Note the average number of patients in the transplant wait list, especially in the years 2001/02, 2004/05 and 2008/09 had not changed; in contrast, the mortality while on transplant wait list has been significantly increased despite an increase in the LT activity from donors after cardiac death donors (B).
There is a lack of universally acceptable objective criteria in identification of an ideal DCD donor and suitable recipient selection. With ever growing transplant waiting lists and death while on the list, clinicians are always on the lookout for means of pushing the boundaries; which donors can be accepted for DCD donation and which organs can be safely transplanted into which potential recipient. The big unanswered question that remains is “which potential DCD donor would become a DBD donor if appropriately managed?” but this is beyond the control of transplant surgeons and lies in the hands of the intensivists who manage most of these donors prior to the referral[4,5].
Translational studies are not readily incorporated in to the practice in the field of DCD liver transplantation. The bulk of the evidence on clinical outcomes consists of retrospective and observational series. On a positive note, there is evidence on manipulation of DCD grafts, potentially rectifying initial warm ischemia induced organ injury[6]. Most of the problems associated with DCD liver transplantation are related to the additional ischemic insult that occurs following cardiac death and until organ perfusion with preservation solution is commenced. The exaggerated ischemia reperfusion injury might be potentially life threatening to the recipient upon reperfusion of the graft[7]. A higher incidence of significant organ dysfunction, delayed graft function with primary non-function is reported with organs from DCD donors[8,9]. Dependency on organ support in the immediate post operative period is an added burden on healthcare systems, in addition to increased risk of long term complications e.g. biliary complications in DCD liver grafts.
In this review we aim to analyze the current literature on outcomes, results and complications of DCD liver transplantation and investigate interventional and experimental strategies to overcome issues related to DCD liver transplantation.
HISTORICAL PERSPECTIVES
For many years, liver transplant programs, based on deceased organ donation programs, have depended on “cadaveric donors” where death has been confirmed by brain stem death testing. These donors are called heart beating donors but more recently have become known as deceased after brain death (DBD) donors. Liver transplantation became an accepted treatment for end stage liver disease following the refinement of immunosuppression therapy that resulted in improved long term graft and patient survival. The increasing success of liver transplantation led to a widening of the indications and in the UK was at a time of a reduction in the number of potential donors offered to the donor coordinator teams to a point where the organ supply did not meet the demand, and so surgeons explored alternative organ sources.
The concept of non-heart beating donation or donation after cardiac death (DCD) was re-visited as a viable source of liver grafts in this setting[10]. DCD donation was in fact not a new phenomenon but could be regarded as a revival of a historical procedure first performed in 1933. Historically, almost all renal transplants were carried out using DCD organs following the first published report in 1955[11]. There was a revival of DCD activity towards the end of the 20th Century[12-14]; this success in the light of a reducing pool of DBD donors prompted liver transplant surgeons to re-explore the possibility of grafts from DCD donors for liver transplantation[15-18]. In the 1990s, there was increased activity of DCD liver transplantation in the United States and Europe, which led to the 1st DCD conference held in 1995[19,20]. During this conference, experts gathered in Maastricht defined the categories of DCD donors, widely known as Maastricht criteria. The following four categories were defined: Category I - Death on arrival; Category II - Failed resuscitation; Category III - Awaiting cardiac arrest, generally comprising planned withdrawal of life support of an in-hospital (ITU) patient; Category IV - Cardiac arrest after brain stem death.
Categories I and II are known as “uncontrolled” donors owing to lack of the time of cardiac arrest; hence the predictability of initial warm ischemia. In contrast, types III/IV donors have a more predictable course before the cardiac death and were termed “controlled” donors. The outcomes of livers from uncontrolled DCD donors were poor; only a few reports have been published on liver transplantation using these donors and some form of cardio-pulmonary support was employed in these donors to maintain recirculation[8,21]. Substantial data on renal transplantation from uncontrolled DCD donors exists; however, most liver transplant programs only use controlled DCD donors at present[22]. Initial results following controlled DCD transplantation were acceptable and similar to that of livers from DBD donors; initially this donor organ source was thought to be a supplement to reducing numbers of organs from DBD donor sources.
CURRENT TREND IN DCD DONATION
In the UK, DCD donation activity has increased by 100% over the last few years. One would expect this to have contributed to a parallel increase in the overall transplant activity, but in reality, the total number of deceased donors (DCD and DBD) and the number transplants has remained static or declined in comparison to the previous years. Therefore, it appears that the DCD activity has increased at the expense of DBD activity. We speculate that this might be explained by some DCD donors being referred prior to the establishment of brain stem death. This is opposite to UNOS data which suggests that DCD activity has increased to supplement the overall transplant activity[16].
PATHOPHYSIOLOGY OF DCD
Following withdrawal of treatment in DCD donors, organs suffer an ischemic insult resulting from hypotension and desaturation below the levels that are required to maintain adequate tissue perfusion. In our own unit, we consider blood pressure < 50 mmHg and oxygen saturation < 80% as heralding the beginning of warm ischemia. Intracellular energy charge is paramount for cellular viability[23,24]. In the absence of oxygenated perfusion during warm ischemia, anaerobic metabolism heralds intracellular energy depletion, lactic acidosis and paralysis of energy driven Na+/K+ pumps that maintain cell membrane integrity culminating in edema, intracellular vacuolation and cell death. In general, it is accepted that hepatocytes withstand sustained warm ischemic injury for up to 30 min, and grafts transplanted beyond this limit have a higher incidence of primary non function[25]. The degree of intracellular vacuolation has been shown to be predictive of the eventual graft outcome in pig liver transplantation[26], although this is not routinely examined in the clinical setting.
Another factor which is detrimental to DCD grafts is post-mortem clot formation in the hepatic microvasculature. This leads to differential and non-uniform perfusion during both organ retrieval and upon reperfusion and eventually determines subsequent graft function. Additional problems specific to liver transplantation include biliary epithelial damage leading to ischemic type biliary strictures (ITBL)[21]. Bile ducts derive an exclusive arterial blood supply and poor perfusion of the biliary microvasculature is implicated in ITBL. The incidence of biliary strictures is also associated with inadequate bile duct flush at the commencement of cold ischemia. Inspissated bile salts are deposited inside the intrahepatic segmental ducts causing biliary epithelial injury progressing to strictures[27].
The added ischemic insult in DCD grafts compared with DBD donor grafts can provoke severe ischemia reperfusion injury after transplantation. This can lead to cardiovascular, renal and systemic instability and oxygen derived free radicals are implicated[28]. Various bio-markers have been described to quantify the ischemic injury prior to organ retrieval or transplantation, with the objective of assessing suitability of grafts for transplantation; these include xanthine, hypoxanthine, hyaluronic acid and reduced glutathione etc[29-33]. Hypoxanthine is a catabolic by-product of intracellular ATP depletion and upon reperfusion with oxygenated blood becomes oxidised to xanthine. Both molecules possess the potential to generate free radicals which are implicated in ischemia reperfusion injury[28,34]. Proportionate increase in extracellular hypoxanthine was shown to be associated with duration warm ischemia reflecting increased free radical production, poor graft viability and function[31]. Undoubtedly, assessment of these biomarkers in DCD liver grafts prior to implantation would be helpful. Certain technical limitations, namely the failure to identify these biomarkers in the peripheral body fluids, technical demands and time constraints in the actual clinical setting, preclude them from being incorporated in to current practice.
CLINICAL OUTCOMES OF DCD
The incidence of delayed graft function and primary non-function is higher in livers from DCD donors and this leads to patient instability in the early post transplant period. Worsening liver function tests in the presence of acidosis and coagulopathy are poor prognostic markers. The reported incidence of primary non-function is up to 15% following transplantation of a DCD donor liver[21,35]. This is 4-5 fold higher when compared to livers from DBD donors. The risk of PNF further increases with prolongation of the cold ischemia time[36]. Some authors have suggested that cold ischemia is more detrimental to DCD grafts[37].
The early results of graft and patient survival following liver transplantation from DCD donors were comparable to that of transplantation from DBD donors[38]. Refinements of donor procurement, preservation, donor organ selection and peri-operative care has resulted in improved outcomes in the last decade. At present, the long term patient and graft survival stands at 60%-70% at 5 years following liver transplantation from a DCD donor. A recent report even suggested equal survival outcomes[1]. Strict donor selection criteria probably contributed to these results that may not be possible to apply in most of the other centers[39].
ITBL is associated with long term morbidity and risk of further surgical and non-surgical interventions and even re-transplantation[35,40]. Isolated intrahepatic lesions may have an indolent course in the presence of free biliary drainage from the unaffected hepatic parenchyma (Figure 2). Involvement of major bile ducts or the extrahepatic biliary system, however, is not uncommon and warrants aggressive management[41]. The risk of ITBL appears extremely high and is reported in up to 50% of uncontrolled DCD transplantation[21]. Although less frequent, in the controlled DCD setting the highest reported incidence is between 30%-40%[40,42].
Figure 2.
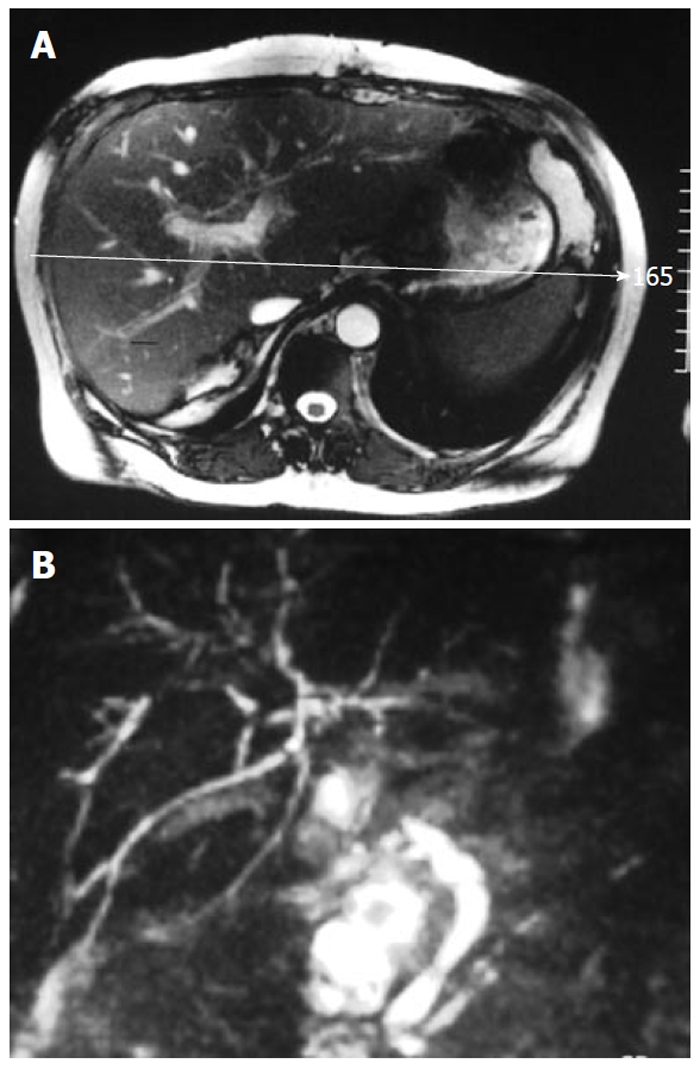
Magnetic resonance cholangiopancreatography images of 60-year-old patient received a donors after cardiac death liver graft received 7 years ago. Patient developed ischemic type intrahepatic biliary strictures 8 mo since transplant, confirmed to be of ischemic origin by liver biopsy. Note: dilated intrahepatic ducts proximal to intrahepatic biliary strictures.
Anecdotal evidence suggests that there is a tendency for an increased use of hospital resources, including intensive care facilities, renal support including dialysis and hemofiltration during the early post transplant period in those recipients receiving a DCD donor liver when compared with those receiving a DBD donor liver. There is no published evidence to support this theory; however, some initial unpublished work that has been carried out in our institution points towards such trend. This means increased financial costs associated with DCD donation and the recipients are at greater operative risk.
Despite all of these shortcomings, DCD donor grafts have been able to save lives of patients with both acute and chronic liver failure and have been used as either full or segmental grafts[43,44]. Despite the substantial risk carried with such procedures, the long term outcomes have been satisfactory. Based on these limited data, it could be speculated that these grafts may even be routinely used in the setting of acute liver failure for emergency transplants or used as split grafts benefiting two recipients[45,46]. The key to success is careful donor selection when DCD donor grafts are considered for such extreme clinical situations.
CURRENT RESEARCH
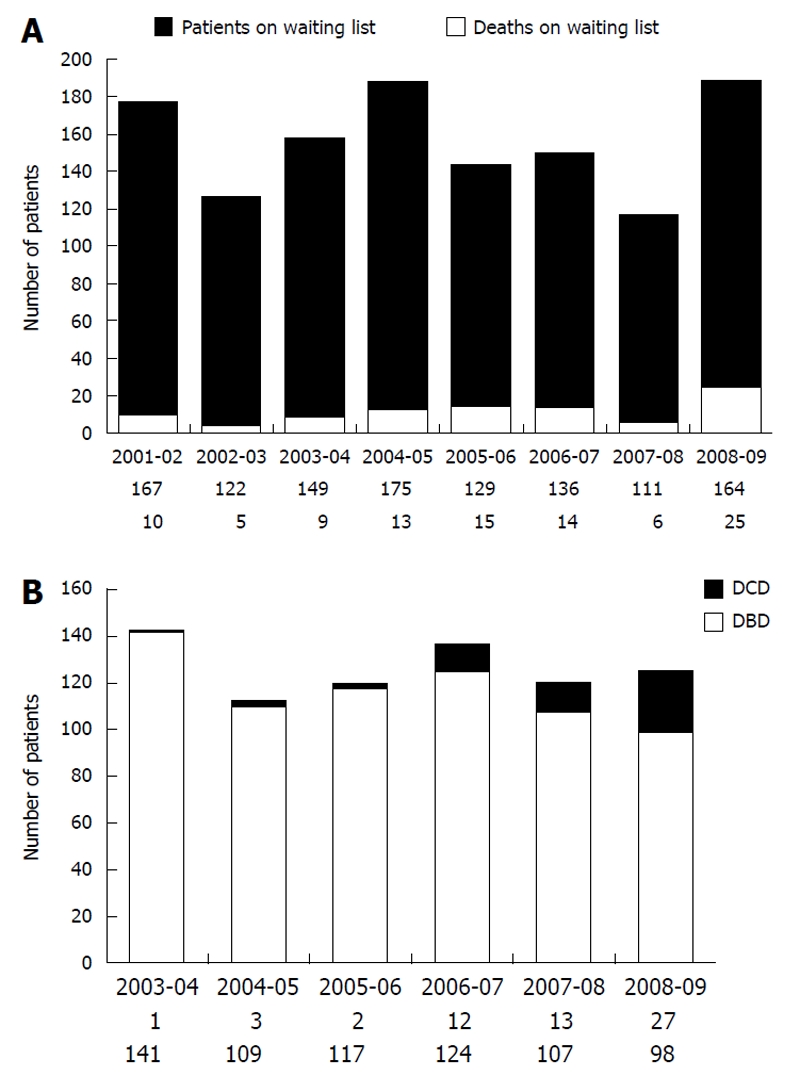
There are a number of levels of intervention that offer potential areas of research on reconditioning of DCD liver grafts (Figure 3). Most of the published studies are in animals and a significant proportion of these included surrogate biomarker analysis in non-transplant models. How these data extrapolate to clinical practice remains unclear. In countries where DCD transplantation (mostly renal transplants) from category II donors is practiced, some of these techniques have been employed in the clinical setting with better long term outcomes for the recipients and grafts[12]. Reconditioning of non heart beating donors offers an opportunity to both improve outcomes and increase the availability of DCD donor organs. Understanding the pathophysiology of DCD donation has enabled many investigators to explore the impact of pharmacological manipulation and both in-situ and ex-situ machine perfusion has begun to become a real clinical possibility. The success of ex-situ machine perfusion of kidney grafts from DCD donors[12,47-49] has been begun to be adapted by other specialties, including cardiac transplantation[50].
Figure 3.
Diagrammatic representation of major steps in donors after cardiac death donation and current research targets. 1Obligatory stand-off time varies according to the setting; in the United Kingdom this is 5 min whilst 2-10 min are being observed by others according to the centre policy. DCD: Donors after cardiac death.
Numerous methods of improving the quality of the DCD grafts have been described and the different terminology adds to confusion. The two principle techniques of machine perfusion described are “hypothermic” and “normothermic”. During hypothermic perfusion, graft energy stores are replenished whilst normothermic reperfusion goes a step further and is aimed at reviving DCD grafts from ischemic injury. Depending on the timing of application, such procedures are further classified as “pre-conditioning” and “post-conditioning”. Apart from machine perfusion, these terms may also encompass other pharmacological modulation/intervention of grafts. Pre-conditioning refers to such applications carried out at the time of retrieval or after the retrieval but prior to cold storage of organs. In contrast, post-conditioning refers to techniques that are employed after cold storage and immediately prior to the reperfusion in the recipient.
Extra-corporeal (ex-vivo) perfusion
The Oxford Group studied the benefits of normothermic machine perfusion extensively. Imber et al[51,52] (2002) reported that normothermic perfusion is superior to the traditional UW solution based cold storage. Total extracorporeal machine perfusion has its disadvantages owing to technical difficulties in vascular connections; expertise and organ transport, etc., and hence may not be practical in most situations. Subsequently Reddy et al[53] (2004) explored the possibility of post-conditioning of liver grafts that have been stored in the cold storage for a limited period. This model has more practical sense as in real practice the organs could be transported (cold stored) to the recipient center and “post-conditioned” with normothermic perfusion for a certain period of time prior to implantation. The authors concluded that sequential cold storage followed by normothermic perfusion is detrimental to the grafts, leading to more hepatocyte injury. Subsequent to this, the same group tested a similar model but with shorter cold ischemia compared to their previous study, and they demonstrated that hepatocytes retained the synthetic function after brief cold ischemia and more prolonged post conditioning[37]. The results from Gong et al[54] (2008) had also drawn similar conclusions following normothermic perfusion of swine liver when compared to cold stored liver in histidine-tryptophan-ketogluterate solution.
The results of hypothermic perfusion appear to be different to that of normothermic models. Several studies have suggested post conditioning in the experimental liver transplant as well as renal transplant setting where hypothermic post conditioning yielded better outcomes[55-57]. Extra-corporeal oxygenated machine perfusion (ECMO) of DCD liver grafts was shown to be superior to the traditionally cold stored liver grafts[58]. The key elements of hypoxia induced cellular injury are shown to be reversible in pre-conditioned grafts perfused with oxygenated buffer using the extracorporeal perfusion system[59]. Short term hypothermic oxygenated machine perfusion restored intracellular ATP and gave better post-transplant biochemical parameters than those transplanted without such intervention[58]. Work carried out by Manekeller et al[60] (2007) reported comparable outcomes in terms of bile acid production, ammonia clearance, vascular resistance and oxygen utilisation of DCD liver grafts treated with a short period of post conditioning prior to viability assessment. The authors concluded that prolonged cold ischemia may potentially augment injury caused by warm ischemia; some of the conclusions drawn in this study may be considered speculative in the presence of drawbacks in their study design[60] (Table 1).
Table 1.
Summary data on normothermic ex-vivo perfusion studies of donors after cardiac death liver
| Author | Yr | Model | Summary | Outcome |
| Gong et al[54] | 2008 | Animal (swine) | Normothermic perfusion with autologous blood (n = 4), compared with cold stored controls in HTK solution (n = 4) | Improved bile production, less hepatocyte damage and favourable haemodynamic parameters |
| Manekeller et al[60] | 2007 | Animal (rat) | Oxygenated hypothermic machine perfusion at the end of cold storage (post perfusion) | Improved performance indicators comparable to controls |
| Reddy et al[37] | 2005 | Animal (swine) | Normothermic perfusion for 24 h (n = 5%) compared with sequential cold storage of 1 h followed by 20 h normothermic perfusion (n = 5) | Greater hepatocyte injury whilst retaining the synthetic function |
| Reddy et al[53] | 2004 | Animal (swine) | Normothermic perfusion for 24 h (n = 4) compared with sequential 4 h cold storage followed by 20 h normothermic reperfusion (post-conditioning, n = 4) | Greater hepatocyte injury in the sequential post conditioning group |
| St Peter et al[55] | 2002 | Animal (swine) | Hypothermic storage (n = 4) compared to normothermic perfusion ex-vivo (n = 4) - reperfusion model not transplant | Recovery of synthetic function, less hepatocyte injury and improved substrate utilisation |
| Imber et al[51] | 2002 | Animal (swine) | Normothermic perfusion (n = 5) compared with standard cold storage (n = 5) | Improved bile production, glucose metabolism and less hepatocyte injury |
HTK: Histidine-tryptophan-ketoglutarate.
Machine perfusion alone, however, may not provide the solutions to the problems associated with DCD livers. Jain et al[61] (2004) extensively studied the hemodynamic perfusion changes occurring during hypothermic perfusion at extremes of cold ischemia time extending to 24 h. Such long cold ischemia is not expected in the routine clinical setting but some of their observations highlight the problems peculiar to DCD livers. It was shown that heterogenous microvascular perfusion occurred with hypothermic perfusion, probably resulting from endothelial cell injury. This has been confirmed by other studies[25]; a similar heterogenous perfusion is commonly observed in the clinical setting that is directly associated with peri-operative instability of recipient and reflected on subsequent graft dysfunction.
In-vivo (in-situ) perfusion
A novel approach is the “in-situ (vivo)” machine perfusion and current interest is centred on in-situ perfusion using autologous blood and an ECMO device. This obviates the need for exhaustive techniques to reconnect the organs to the machine; hence, appears simple when the technical aspects alone are compared with its counterpart “ex-situ (vivo)” machine perfusion. The first results of in-situ perfusion with an ECMO device was published by Ko et al[62] (2000); the authors reported of the use of an ECMO assisted perfusion when legal barriers precluded organ retrieval from DCD donors after certification of cardiac death. The group published data on 8 renal transplants performed after reviving the organs with hypothermic circulation driven by ECMO and reported immediate graft function in 75% cases, whilst delayed graft function was observed in the remainder. This group reproduced similar results in a subsequent publication which created an interest in the in-vivo revival of DCD organs[63].
Quintela et al[64] (2005) reported the earliest clinical results of liver transplantation from a technique that could be simulated to autologous re-perfusion and without a mechanical device; the importance is that this is the only reported clinical series and the donors in this series could be regarded type II DCD donors. They reported 10 liver transplants performed using grafts that were maintained by abdominal compression-decompression to maintain organ perfusion. Successful results reported by this group have not been reproduced by the same or any other groups to date.
There is very limited data on the performance of liver grafts that have been perfused in-situ with normothermic perfusion techniques. Rojas et al[65] (2004) reported their results on swine maintained on ECMO following induced cardiac arrest, and concluded venous oxygen saturation reached the baseline pre-cardiac arrest levels within 15 min of ECMO perfusion, whilst retaining 75% of synthetic function following warm ischemia. These results are exciting, but no other groups have reported similar results. The same group recently published data on a similar model with 30 min of induced warm ischemia followed by ECMO support[66]. Organs were recovered to a transplantable level. The prospects of in-vivo perfusion appear sound as technical aspects are less cumbersome when compared to extracorporeal perfusion techniques. A major obstacle is application of such a technique to human model and overcoming the ethical and legal barriers.
Pharmacological agents and modulation
The initial reports of pre-flush with streptokinase were centered on renal transplantation demonstrating the improved microvascular permeability and graft function[67,68]. The convincing results led to routine incorporation of this to the practice among many centers[69]. In the DCD liver grafts of an ex-vivo transplant model, heterogenous patchy perfusion resulting in loss of cellular integrity had been shown when not treated with anti-fibrinolytic streptokinase solution[70]. Yamauchi et al[71] (2000) reported improved microvascular perfusion in the rat liver transplantation model using DCD grafts pre-flushed with streptokinase.
Multifactorial “modulation” of DCD donors with the use of pharmacological agents was reported in a recent animal study[6]. The investigators used a combined pharmacological modulation “in-situ” as well as during the recipient operation. The agents used mainly were anti-thrombogeneic and vasodilatatory (streptokinase, heparin, epoprostenol) and biological agents (primarily redox agents) aiming to minimise the ischemia reperfusion injury[6,72]. The livers were exposed to 45 min of warm ischemia, followed by a cold storage prior to transplant. The investigators reported a lower incidence of primary non-function, improved hepatic synthetic activity and less parenchymal loss following modulation. They also reported lower bile salt-to-phospholipid ratio in the modulation group. Increased bile salt-to-phospholipid ratio has been previously attributed by the same investigators for the higher incidence of ITBL[27]. The protective effect of L-arginine in relation to attenuation of nitric oxide and plasma endothelin release has also been reported[73]. It appears that scientists have made some headway in addressing key issues related to DCD liver transplantation; however, these are yet to be proven by long term follow up studies and application to clinical practice.
FUTURE OF DCD LIVER TRANSPLANTATION
The lack of a universally accepted and safe criterion for age of the donor and the amount of macro- and micro-vesicular steatosis in the setting of DCD liver grafts remains a problem. Investigators have so far been looking only at the revival of warm ischemic damage, but other surrogate factors should be investigated in the context of initial poor function. Primary non function donor-recipient matching is inevitably carried out at present and tends to be based on clinical and performance indicators in both the donor and recipient; however, models are needed that score the risk of DCD grafts taking other parameters in to account[74]. This would help identify the best recipient for a particular DCD or DBD graft[7]. This would ensure that organ wastage from discard and recipient complications would be minimised.
Judging by the current popularity, it may be speculated that in the future, DCD liver transplantation will contribute a significant proportion of the liver transplant activity. Whether this increased activity of DCD donation is the end results of the organ donation process through awareness among both public and medical personnel alike, or increased DCD activity at the expense of DBD activity, remains in question. Pressure for ITU beds may prompt intensivists to withdraw life support at the earliest opportunity when it is evident that further treatment of a patient is futile. It is known that the majority of patients with intra-cerebral pathologies are managed with a relatively dry fluid regime in order to prevent intra-cerebral edema; meanwhile, donor optimisation prior to organ retrieval involves fluid, electrolytes, blood sugar and hormonal support and prevention of infection[75,76]. It is likely that if these patients with intra-cerebral pathology were managed using the optimisation guidelines then a proportion would become brain dead within the next few hours[77].
In our experience, there have been many instances where DCD donor offers were converted to DBD offers at the last minute, even just prior to commencement of organ retrieval. As discussed above, experience suggests that, with further management for a few hours, even more DCD offers would almost certainly see the donors become brain dead[78]. Ethical or legal barriers may preclude pharmacological or other manipulation of the donor in some countries. In the United Kingdom, amendments to the Human Tissue Act introduced recently declared that once a suitable recipient has been identified to receive organs from a potential donor, the organs belong to the recipient. This amendment might allow us to challenge critics who suggest donor management/manipulation to optimise organ donation is legally and ethically flawed once it is decided that further treatment is futile[79]. Liver transplantation with DCD organs should also be looked upon as a life saving operation; it is important that every professional involved from donor care to transplantation realises that the price a recipient will have to pay is higher when receiving DCD donor organs than a DBD graft[80].
The revival of donor liver organs is yet to be translated to clinical practice. Unlike in renal transplantation where one can take a calculated risk and if unsuccessful return to dialysis, liver transplantation using these manipulated livers is a very big risk. What has been achieved so far is promising and combined pharmacological manipulation and ECMO support appears the way forward. In-situ revival appears a better option. In the future, we could see a transition from animal to human models at least at the pre-transplant level. In view of the increased demand for donor livers, it is likely that progress made on the issues discussed would increase DCD liver transplantation, contributing to a true and meaningful rise in overall transplant activity.
Footnotes
Peer reviewer: Uwe Klinge, MD, Professor, Institute for Applied Medical Engineering AME, Helmholtz Institute, RWTH Aachen Pauwelsstrabe 30, Aachen 52074, Germany
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
References
- 1.Dubbeld J, Hoekstra H, Farid W, Ringers J, Porte RJ, Metselaar HJ, Baranski AG, Kazemier G, van den Berg AP, van Hoek B. Similar liver transplantation survival with selected cardiac death donors and brain death donors. Br J Surg. 2010;97:744–753. doi: 10.1002/bjs.7043. [DOI] [PubMed] [Google Scholar]
- 2.Fujita S, Mizuno S, Fujikawa T, Reed AI, Kim RD, Howard RJ, Hemming AW. Liver transplantation from donation after cardiac death: a single center experience. Transplantation. 2007;84:46–49. doi: 10.1097/01.tp.0000267424.88023.7b. [DOI] [PubMed] [Google Scholar]
- 3.Manzarbeitia CY, Ortiz JA, Jeon H, Rothstein KD, Martinez O, Araya VR, Munoz SJ, Reich DJ. Long-term outcome of controlled, non-heart-beating donor liver transplantation. Transplantation. 2004;78:211–215. doi: 10.1097/01.tp.0000128327.95311.e3. [DOI] [PubMed] [Google Scholar]
- 4.Gardiner D, Sparrow R. Not dead yet: controlled non-heart-beating organ donation, consent, and the Dead Donor Rule. Camb Q Healthc Ethics. 2010;19:17–26. doi: 10.1017/S0963180109990211. [DOI] [PubMed] [Google Scholar]
- 5.Griffiths J, Verble M, Falvey S, Bell S, Logan L, Morgan K, Wellington F. Culture change initiatives in the procurement of organs in the United kingdom. Transplant Proc. 2009;41:1459–1462. doi: 10.1016/j.transproceed.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 6.Monbaliu D, Vekemans K, Hoekstra H, Vaahtera L, Libbrecht L, Derveaux K, Parkkinen J, Liu Q, Heedfeld V, Wylin T, et al. Multifactorial biological modulation of warm ischemia reperfusion injury in liver transplantation from non-heart-beating donors eliminates primary nonfunction and reduces bile salt toxicity. Ann Surg. 2009;250:808–817. doi: 10.1097/SLA.0b013e3181bdd787. [DOI] [PubMed] [Google Scholar]
- 7.Dezza MC, Berrevoet F, Sainz-Barriga M, Rossetto A, Colenbie L, Haentjens I, Van Vlierberghe H, Colle I, Van Huysse J, Praet M, et al. The choice of recipient does not have a bearing on early outcome in liver transplant patients receiving grafts from non-heart-beating donors: a reappraisal? Transplant Proc. 2007;39:2675–2677. doi: 10.1016/j.transproceed.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Otero A, Gómez-Gutiérrez M, Suárez F, Arnal F, Fernández-García A, Aguirrezabalaga J, García-Buitrón J, Alvarez J, Máñez R. Liver transplantation from maastricht category 2 non-heart-beating donors: a source to increase the donor pool? Transplant Proc. 2004;36:747–750. doi: 10.1016/j.transproceed.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Kubal CA, Harris RM, Inston NG, Graetz KP, Ready AR, Mellor SJ, Hamsho AS, Waring RH, World MJ. Mitochondrial complex activity in donor renal grafts, cold ischemia time, and recovery of graft function. Transplantation. 2009;87:1037–1039. doi: 10.1097/TP.0b013e31819cc463. [DOI] [PubMed] [Google Scholar]
- 10.Reich DJ, Munoz SJ, Rothstein KD, Nathan HM, Edwards JM, Hasz RD, Manzarbeitia CY. Controlled non-heart-beating donor liver transplantation: a successful single center experience, with topic update. Transplantation. 2000;70:1159–1166. doi: 10.1097/00007890-200010270-00006. [DOI] [PubMed] [Google Scholar]
- 11.HUME DM, MERRILL JP, MILLER BF, THORN GW. Experiences with renal homotransplantation in the human: report of nine cases. J Clin Invest. 1955;34:327–382. doi: 10.1172/JCI103085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daemen JH, de Wit RJ, Bronkhorst MW, Marcar ML, Yin M, Heineman E, Kootstra G. Short-term outcome of kidney transplants from non-heart-beating donors after preservation by machine perfusion. Transpl Int. 1996;9 Suppl 1:S76–S80. doi: 10.1007/978-3-662-00818-8_20. [DOI] [PubMed] [Google Scholar]
- 13.Pacholczyk MJ, Lagiewska B, Szostek M, Chmura A, Morzycka-Michalik M, Rowińska-Stryjecka D, Wałaszewski J, Rowiński W. Transplantation of kidneys harvested from non-heart-beating donors: early and long-term results. Transpl Int. 1996;9 Suppl 1:S81–S83. doi: 10.1007/978-3-662-00818-8_21. [DOI] [PubMed] [Google Scholar]
- 14.Gerstenkorn C. Non-heart-beating donors: renewed source of organs for renal transplantation during the twenty-first century. World J Surg. 2003;27:489–493. doi: 10.1007/s00268-002-6488-0. [DOI] [PubMed] [Google Scholar]
- 15.García-Valdecasas Salgado JC. Non beating heart donors as a possible source for liver transplantation. Acta Chir Belg. 2000;100:268–271. [PubMed] [Google Scholar]
- 16.Merion RM, Pelletier SJ, Goodrich N, Englesbe MJ, Delmonico FL. Donation after cardiac death as a strategy to increase deceased donor liver availability. Ann Surg. 2006;244:555–562. doi: 10.1097/01.sla.0000239006.33633.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D'Alessandro AM, Hoffmann RM, Knechtle SJ, Eckhoff DE, Love RB, Kalayoglu M, Sollinger HW, Belzer FO. Successful extrarenal transplantation from non-heart-beating donors. Transplantation. 1995;59:977–982. doi: 10.1097/00007890-199504150-00009. [DOI] [PubMed] [Google Scholar]
- 18.D'Alessandro AM, Hoffmann RM, Knechtle SJ, Eckhoff DE, Love RB, Kalayoglu M, Sollinger HW, Belzer FO. Controlled non-heart-beating donors: a potential source of extrarenal organs. Transplant Proc. 1995;27:707–709. [PubMed] [Google Scholar]
- 19.Kootstra G, Daemen JH, Oomen AP. Categories of non-heart-beating donors. Transplant Proc. 1995;27:2893–2894. [PubMed] [Google Scholar]
- 20.Kootstra G. Statement on non-heart-beating donor programs. Transplant Proc. 1995;27:2965. [PubMed] [Google Scholar]
- 21.Suárez F, Otero A, Solla M, Arnal F, Lorenzo MJ, Marini M, Vázquez-Iglesias JL, Gómez M. Biliary complications after liver transplantation from maastricht category-2 non-heart-beating donors. Transplantation. 2008;85:9–14. doi: 10.1097/01.tp.0000297945.83430.ce. [DOI] [PubMed] [Google Scholar]
- 22.Gok MA, Asher JF, Shenton BK, Rix D, Soomro NA, Jaques BC, Manas DM, Talbot D. Graft function after kidney transplantation from non-heartbeating donors according to maastricht category. J Urol. 2004;172:2331–2334. doi: 10.1097/01.ju.0000145128.00771.14. [DOI] [PubMed] [Google Scholar]
- 23.Lanir A, Jenkins RL, Caldwell C, Lee RG, Khettry U, Clouse ME. Hepatic transplantation survival: correlation with adenine nucleotide level in donor liver. Hepatology. 1988;8:471–475. doi: 10.1002/hep.1840080306. [DOI] [PubMed] [Google Scholar]
- 24.Hickman R, Rose-Innes C, Tyler M, Bracher M, Lotz Z, Fourie J. Energy charge as an indication of liver viability. A comparison of changes in livers that remained intact with those subjected to autografting. Transplantation. 1992;53:540–545. doi: 10.1097/00007890-199203000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Ma Y, Wang GD, Wu LW, Hu RD. Dynamical changing patterns of histological structure and ultrastructure of liver graft undergoing warm ischemia injury from non-heart-beating donor in rats. World J Gastroenterol. 2006;12:4902–4905. doi: 10.3748/wjg.v12.i30.4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Monbaliu D, Libbrecht L, De Vos R, Vekemans K, Walter H, Liu Q, Heedfeld V, Goossens V, Pirenne J, Roskams T. The extent of vacuolation in non-heart-beating porcine donor liver grafts prior to transplantation predicts their viability. Liver Transpl. 2008;14:1256–1265. doi: 10.1002/lt.21513. [DOI] [PubMed] [Google Scholar]
- 27.Yska MJ, Buis CI, Monbaliu D, Schuurs TA, Gouw AS, Kahmann ON, Visser DS, Pirenne J, Porte RJ. The role of bile salt toxicity in the pathogenesis of bile duct injury after non-heart-beating porcine liver transplantation. Transplantation. 2008;85:1625–1631. doi: 10.1097/TP.0b013e318170f5f7. [DOI] [PubMed] [Google Scholar]
- 28.McCord JM. Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med. 1985;312:159–163. doi: 10.1056/NEJM198501173120305. [DOI] [PubMed] [Google Scholar]
- 29.Net M, Valero R, Almenara R, Rull R, Gonzalez FJ, Taurá P, Lopez-Boado MA, Deulofeu R, Elena M, Capdevila L, et al. Hepatic xanthine levels as viability predictor of livers procured from non-heart-beating donor pigs. Transplantation. 2001;71:1232–1237. doi: 10.1097/00007890-200105150-00009. [DOI] [PubMed] [Google Scholar]
- 30.Soejima Y, Yanaga K, Wakiyama S, Nishizaki T, Yoshizumi T, Sugimachi K. Serum hyaluronic acid as a reliable parameter of allograft viability in porcine liver transplantation. Hepatogastroenterology. 2002;43:590–595. [PubMed] [Google Scholar]
- 31.Nagayama M, Katsuramaki T, Kimura H, Isobe M, Meguro M, Matsuno T, Nui A, Hirata K. Prediction of graft viability from non-heart-beating donor pigs using hepatic microdialysate hypoxanthine levels. J Surg Res. 2002;107:210–218. doi: 10.1006/jsre.2002.6514. [DOI] [PubMed] [Google Scholar]
- 32.Golling M, Kellner H, Fonouni H, Rad MT, Urbaschek R, Breitkreutz R, Gebhard MM, Mehrabi A. Reduced glutathione in the liver as a potential viability marker in non-heart-beating donors. Liver Transpl. 2008;14:1637–1647. doi: 10.1002/lt.21585. [DOI] [PubMed] [Google Scholar]
- 33.Zapletal C, Heyne S, Breitkreutz R, Gebhard MM, Golling M. The influence of selenium substitution on microcirculation and glutathione metabolism after warm liver ischemia/reperfusion in a rat model. Microvasc Res. 2008;76:104–109. doi: 10.1016/j.mvr.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 34.Nishino T, Nakanishi S, Okamoto K, Mizushima J, Hori H, Iwasaki T, Nishino T, Ichimori K, Nakazawa H. Conversion of xanthine dehydrogenase into oxidase and its role in reperfusion injury. Biochem Soc Trans. 1997;25:783–786. doi: 10.1042/bst0250783. [DOI] [PubMed] [Google Scholar]
- 35.de Vera ME, Lopez-Solis R, Dvorchik I, Campos S, Morris W, Demetris AJ, Fontes P, Marsh JW. Liver transplantation using donation after cardiac death donors: long-term follow-up from a single center. Am J Transplant. 2009;9:773–781. doi: 10.1111/j.1600-6143.2009.02560.x. [DOI] [PubMed] [Google Scholar]
- 36.Qing DK. Prolonging warm ischemia reduces the cold preservation limits of liver grafts in swine. Hepatobiliary Pancreat Dis Int. 2006;5:515–520. [PubMed] [Google Scholar]
- 37.Reddy S, Greenwood J, Maniakin N, Bhattacharjya S, Zilvetti M, Brockmann J, James T, Pigott D, Friend P. Non-heart-beating donor porcine livers: the adverse effect of cooling. Liver Transpl. 2005;11:35–38. doi: 10.1002/lt.20287. [DOI] [PubMed] [Google Scholar]
- 38.Barlow AD, Metcalfe MS, Johari Y, Elwell R, Veitch PS, Nicholson ML. Case-matched comparison of long-term results of non-heart beating and heart-beating donor renal transplants. Br J Surg. 2009;96:685–691. doi: 10.1002/bjs.6607. [DOI] [PubMed] [Google Scholar]
- 39.Bhogal RH, Sutaria R, Gunson BK, Bramhall SR. Similar liver transplantation survival with selected cardiac death donors and brain death donors (Br J Surg 2010; 97: 744-753) Br J Surg. 2010;97:1310; author reply 1310–1311. doi: 10.1002/bjs.7207. [DOI] [PubMed] [Google Scholar]
- 40.Abt P, Crawford M, Desai N, Markmann J, Olthoff K, Shaked A. Liver transplantation from controlled non-heart-beating donors: an increased incidence of biliary complications. Transplantation. 2003;75:1659–1663. doi: 10.1097/01.TP.0000062574.18648.7C. [DOI] [PubMed] [Google Scholar]
- 41.Maheshwari A, Maley W, Li Z, Thuluvath PJ. Biliary complications and outcomes of liver transplantation from donors after cardiac death. Liver Transpl. 2007;13:1645–1653. doi: 10.1002/lt.21212. [DOI] [PubMed] [Google Scholar]
- 42.Lee HW, Suh KS, Shin WY, Cho EH, Yi NJ, Lee JM, Han JK, Lee KU. Classification and prognosis of intrahepatic biliary stricture after liver transplantation. Liver Transpl. 2007;13:1736–1742. doi: 10.1002/lt.21201. [DOI] [PubMed] [Google Scholar]
- 43.Muiesan P, Girlanda R, Baker A, Rela M, Heaton N. Successful segmental auxiliary liver transplantation from a non-heart-beating donor: implications for split-liver transplantation. Transplantation. 2003;75:1443–1445. doi: 10.1097/01.TP.0000069024.86527.0B. [DOI] [PubMed] [Google Scholar]
- 44.Muiesan P, Jassem W, Girlanda R, Steinberg R, Vilca-Melendez H, Mieli-Vergani G, Dhawan A, Rela M, Heaton N. Segmental liver transplantation from non-heart beating donors--an early experience with implications for the future. Am J Transplant. 2006;6:1012–1016. doi: 10.1111/j.1600-6143.2006.01293.x. [DOI] [PubMed] [Google Scholar]
- 45.Gozzini S, Perera MT, Mayer DA, Mirza DF, Kelly DA, Muiesan P, Sharif K. Liver transplantation in children using non-heart-beating donors (NHBD) Pediatr Transplant. 2010;14:554–557. doi: 10.1111/j.1399-3046.2009.01280.x. [DOI] [PubMed] [Google Scholar]
- 46.Perera MT, Gozzini S, Mayer D, Sharif K, Bennett J, Muiesan P, Mirza DF. Safe use of segmental liver grafts from donors after cardiac death (DCD) in children with acute liver failure. Transpl Int. 2009;22:757–760. doi: 10.1111/j.1432-2277.2009.00886.x. [DOI] [PubMed] [Google Scholar]
- 47.Brook NR, Waller JR, Nicholson ML. Nonheart-beating kidney donation: current practice and future developments. Kidney Int. 2003;63:1516–1529. doi: 10.1046/j.1523-1755.2003.00854.x. [DOI] [PubMed] [Google Scholar]
- 48.Balupuri S, Buckley P, Mohamed M, Cornell C, Mantle D, Kirby J, Manas DM, Talbot D. Assessment of non-heart-beating donor (NHBD) kidneys for viability on machine perfusion. Clin Chem Lab Med. 2000;38:1103–1106. doi: 10.1515/CCLM.2000.164. [DOI] [PubMed] [Google Scholar]
- 49.Balupuri S, Buckley P, Mohamad M, Chidambaram V, Gerstenkorn C, Sen B, Kirby J, Manas DM, Talbot D. Early results of a non-heartbeating donor (NHBD) programme with machine perfusion. Transpl Int. 2000;13 Suppl 1:S255–S258. doi: 10.1007/s001470050336. [DOI] [PubMed] [Google Scholar]
- 50.Ali A, White P, Dhital K, Ryan M, Tsui S, Large S. Cardiac recovery in a human non-heart-beating donor after extracorporeal perfusion: source for human heart donation? J Heart Lung Transplant. 2009;28:290–293. doi: 10.1016/j.healun.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 51.Imber CJ, St Peter SD, Lopez de Cenarruzabeitia I, Pigott D, James T, Taylor R, McGuire J, Hughes D, Butler A, Rees M, et al. Advantages of normothermic perfusion over cold storage in liver preservation. Transplantation. 2002;73:701–709. doi: 10.1097/00007890-200203150-00008. [DOI] [PubMed] [Google Scholar]
- 52.Imber CJ, St Peter SD, de Cenarruzabeitia IL, Lemonde H, Rees M, Butler A, Clayton PT, Friend PJ. Optimisation of bile production during normothermic preservation of porcine livers. Am J Transplant. 2002;2:593–599. doi: 10.1034/j.1600-6143.2002.20703.x. [DOI] [PubMed] [Google Scholar]
- 53.Reddy SP, Bhattacharjya S, Maniakin N, Greenwood J, Guerreiro D, Hughes D, Imber CJ, Pigott DW, Fuggle S, Taylor R, et al. Preservation of porcine non-heart-beating donor livers by sequential cold storage and warm perfusion. Transplantation. 2004;77:1328–1332. doi: 10.1097/01.tp.0000119206.63326.56. [DOI] [PubMed] [Google Scholar]
- 54.Gong J, Lao XJ, Wang XM, Long G, Jiang T, Chen S. Preservation of non-heart-beating donor livers in extracorporeal liver perfusion and histidine-trytophan-ketoglutarate solution. World J Gastroenterol. 2008;14:2338–2342. doi: 10.3748/wjg.14.2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.St Peter SD, Imber CJ, Lopez I, Hughes D, Friend PJ. Extended preservation of non-heart-beating donor livers with normothermic machine perfusion. Br J Surg. 2002;89:609–616. doi: 10.1046/j.1365-2168.2002.02052.x. [DOI] [PubMed] [Google Scholar]
- 56.Balupuri S, Strong A, Hoernich N, Snowden C, Mohamed M, Manas D, Kirby J, Talbot D. Machine perfusion for kidneys: how to do it at minimal cost. Transpl Int. 2001;14:103–107. doi: 10.1007/s001470050855. [DOI] [PubMed] [Google Scholar]
- 57.Lindell SL, Compagnon P, Mangino MJ, Southard JH. UW solution for hypothermic machine perfusion of warm ischemic kidneys. Transplantation. 2005;79:1358–1361. doi: 10.1097/01.tp.0000159143.45022.f6. [DOI] [PubMed] [Google Scholar]
- 58.Dutkowski P, Furrer K, Tian Y, Graf R, Clavien PA. Novel short-term hypothermic oxygenated perfusion (HOPE) system prevents injury in rat liver graft from non-heart beating donor. Ann Surg. 2006;244:968–76; discussion 976-7. doi: 10.1097/01.sla.0000247056.85590.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Miyagi S, Iwane T, Akamatsu Y, Nakamura A, Sato A, Satomi S. The significance of preserving the energy status and microcirculation in liver grafts from non-heart-beating donor. Cell Transplant. 2008;17:173–178. doi: 10.3727/000000008783906874. [DOI] [PubMed] [Google Scholar]
- 60.Manekeller S, Dobberahn V, Hirner A, Minor T. Liver integrity after warm ischemia in situ and brief preservation ex vivo: the value of aerobic post-conditioning. Cryobiology. 2007;55:249–254. doi: 10.1016/j.cryobiol.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 61.Jain S, Xu H, Duncan H, Jones JW, Zhang JX, Clemens MG, Lee CY. Ex-vivo study of flow dynamics and endothelial cell structure during extended hypothermic machine perfusion preservation of livers. Cryobiology. 2004;48:322–332. doi: 10.1016/j.cryobiol.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 62.Ko WJ, Chen YS, Tsai PR, Lee PH. Extracorporeal membrane oxygenation support of donor abdominal organs in non-heart-beating donors. Clin Transplant. 2000;14:152–156. doi: 10.1034/j.1399-0012.2000.140209.x. [DOI] [PubMed] [Google Scholar]
- 63.Ko WJ, Chen YS, Chen RJ, Lai MK, Lee PH. Non-heart-beating donors under extracorporeal membrane oxygenation support. Transplant Proc. 2002;34:2600–2601. doi: 10.1016/s0041-1345(02)03440-1. [DOI] [PubMed] [Google Scholar]
- 64.Quintela J, Gala B, Baamonde I, Fernández C, Aguirrezabalaga J, Otero A, Suárez F, Fernández A, Gomez M. Long-term results for liver transplantation from non-heart-beating donors maintained with chest and abdominal compression-decompression. Transplant Proc. 2005;37:3857–3858. doi: 10.1016/j.transproceed.2005.10.039. [DOI] [PubMed] [Google Scholar]
- 65.Rojas A, Chen L, Bartlett RH, Arenas JD. Assessment of liver function during extracorporeal membrane oxygenation in the non-heart beating donor swine. Transplant Proc. 2004;36:1268–1270. doi: 10.1016/j.transproceed.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 66.Rojas-Pena A, Reoma JL, Krause E, Boothman EL, Padiyar NP, Cook KE, Bartlett RH, Punch JD. Extracorporeal support: improves donor renal graft function after cardiac death. Am J Transplant. 2010;10:1365–1374. doi: 10.1111/j.1600-6143.2010.03063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gok MA, Shenton BK, Peaston R, Cornell C, Robertson H, Mathers M, Aitchison JD, Dark JH, Mantle D, Talbot D. Improving the quality of kidneys from non-heart-beating donors, using streptokinase: an animal model. Transplantation. 2002;73:1869–1874. doi: 10.1097/00007890-200206270-00003. [DOI] [PubMed] [Google Scholar]
- 68.Yamauchi J, Schramm R, Richter S, Vollmar B, Menger MD, Minor T. Improvement of microvascular graft equilibration and preservation in non-heart-beating donors by warm preflush with streptokinase. Transplantation. 2003;75:449–453. doi: 10.1097/01.TP.0000053404.67581.F4. [DOI] [PubMed] [Google Scholar]
- 69.Gok MA, Shenton BK, Buckley PE, Peaston R, Cornell C, Soomro N, Jaques BC, Manas DM, Talbot D. How to improve the quality of kidneys from non-heart-beating donors: a randomised controlled trial of thrombolysis in non-heart-beating donors. Transplantation. 2003;76:1714–1719. doi: 10.1097/01.TP.0000093834.05766.FD. [DOI] [PubMed] [Google Scholar]
- 70.Minor T, Hachenberg A, Tolba R, Pauleit D, Akbar S. Fibrinolytic preflush upon liver retrieval from non-heart beating donors to enhance postpreservation viability and energetic recovery upon reperfusion. Transplantation. 2001;71:1792–1796. doi: 10.1097/00007890-200106270-00015. [DOI] [PubMed] [Google Scholar]
- 71.Yamauchi JI, Richter S, Vollmar B, Menger MD, Minor T. Warm preflush with streptokinase improves microvascular procurement and tissue integrity in liver graft retrieval from non-heart-beating donors. Transplantation. 2000;69:1780–1784. doi: 10.1097/00007890-200005150-00009. [DOI] [PubMed] [Google Scholar]
- 72.Pirenne J, Monbaliu D, Aerts R, Desschans B, Liu Q, Cassiman D, Laleman W, Verslype C, Magdy M, Van Steenbergen W, et al. Biliary strictures after liver transplantation: risk factors and prevention by donor treatment with epoprostenol. Transplant Proc. 2009;41:3399–3402. doi: 10.1016/j.transproceed.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 73.Gong J, Lao XJ, Zhang SJ, Chen S. Protective effects of L-arginine against ischemia-reperfusion injury in non-heart beating rat liver graft. Hepatobiliary Pancreat Dis Int. 2008;7:481–484. [PubMed] [Google Scholar]
- 74.Asher J, Oliver A, Wilson C, Gupta A, Gok M, Balupuri S, Shenton B, Del Rio Martin J, Rix D, Soomro N, et al. A simple cardiovascular risk score can predict poor outcome in NHBD renal transplantation. Transplant Proc. 2005;37:3292–3293. doi: 10.1016/j.transproceed.2005.09.136. [DOI] [PubMed] [Google Scholar]
- 75.Gheorghita E, Rata O, Trifu M. [Intensive care issues in the management of potential organ donors] Chirurgia (Bucur) 2010;105:225–228. [PubMed] [Google Scholar]
- 76.Dictus C, Vienenkoetter B, Esmaeilzadeh M, Unterberg A, Ahmadi R. Critical care management of potential organ donors: our current standard. Clin Transplant. 2009;23 Suppl 21:2–9. doi: 10.1111/j.1399-0012.2009.01102.x. [DOI] [PubMed] [Google Scholar]
- 77.Varelas PN, Abdelhak T, Hacein-Bey L. Withdrawal of life-sustaining therapies and brain death in the intensive care unit. Semin Neurol. 2008;28:726–735. doi: 10.1055/s-0028-1105969. [DOI] [PubMed] [Google Scholar]
- 78.Mascia L, Mastromauro I, Viberti S, Vincenzi M, Zanello M. Management to optimize organ procurement in brain dead donors. Minerva Anestesiol. 2009;75:125–133. [PubMed] [Google Scholar]
- 79.Rady MY, Verheijde JL, McGregor J. Organ procurement after cardiocirculatory death: a critical analysis. J Intensive Care Med. 2008;23:303–312. doi: 10.1177/0885066608320928. [DOI] [PubMed] [Google Scholar]
- 80.Collins TJ. Organ and tissue donation: a survey of nurse's knowledge and educational needs in an adult ITU. Intensive Crit Care Nurs. 2005;21:226–233. doi: 10.1016/j.iccn.2004.10.006. [DOI] [PubMed] [Google Scholar]