Abstract
Background
Depressive symptomatology is common in older adults and is associated with reduced adherence to recommended preventive care, but little is known as to why. Understanding how depressive symptoms may interfere with adherence can help identify leverage points for interventions to increase preventive service use.
Objective
This study examined perceived access to medical care as a possible mediator linking depressive symptomatology to reduced preventive service use in older adults.
Methods
We analyzed data from 5,465 respondents completing the 1993 and 2003/2004 waves of the Wisconsin Longitudinal Study. Depressive symptomatology was assessed using the Center for Epidemiologic Studies Depression Scale. Perceived access survey items were organized via factor analysis to represent key dimensions of access: availability/accessibility, affordability, acceptability, and accommodation. The primary outcome was the total number of seven recommended preventive services that respondents received. Multivariate path analysis was used to estimate direct and indirect effects between depressive symptomatology, perceived access, and preventive service use.
Results
Older adults with depressive symptomatology received fewer recommended services. Depressive symptomatology reduced preventive service use by adversely affecting two dimensions of perceived access: (1) acceptability, pertaining to poor patient-provider trust and communication, and (2) accommodation, pertaining to inconveniently organized services.
Conclusions
Depressive symptomatology may negatively alter older adults’ perceptions of access and, in turn, negatively impact their preventive service use. In addition to treating depression, interventions designed to mitigate the impact of depression on the patient-provider relationship, and organizational changes to practice that better accommodate the needs of depressed patients, may increase adherence to preventive care guidelines in depressed older adults.
Keywords: preventive care, depression, access, elderly
INTRODUCTION
The health benefits of clinical preventive services in older adults are well-documented. For example, annual influenza vaccination, counseling to encourage health-promoting behaviors (e.g., smoking cessation), and early and continued screening for hypertension, hypercholesterolemia, and many cancers are all known to improve older adults’ health outcomes.1–3 Despite this evidence, as well as recommendations from organizations such as the United States Preventive Service Taskforce, rates of preventive service use in older adults have fallen short of Healthy People 2010 goals.1,4,5 As the U.S. population ages, the underuse of preventive services presents a growing public health problem.
In prior studies of preventive service use in older adults, depressive symptomatology has emerged as both a prevalent and consistent correlate.6–9 However, the underlying mechanisms by which depressive symptomatology reduces preventive service use remain largely unknown. Understanding these mechanisms could help suggest additional ways to intervene with older depressed patients to increase their preventive service use in addition to treating their depression. This is important given that successful resolution of depression can be difficult to achieve in practice, due to the need for long-term, persistent treatment,10 high rates of patient non-adherence,11 and reduced efficacy of medication treatment for less severe depression.12 Thus, research that explicates pathways linking depressive symptoms to poor adherence has potential implications for identifying opportunities for interventions designed to mitigate depression’s negative effect on adherence and achieving Healthy People preventive care goals in older adults with poor mental health.
Prior research suggests that perceived access to care may be one mutable mechanism by which depression impacts preventive care use. Patients with less favorable perceptions of access to medical care have lower overall service use,13 mental health service use,14 routine checkups,15 and emergency care. Further, there is evidence that the U.S. primary care system is not well-structured to meet the complex needs of patients with depressive symptoms, particularly in older patients who may be managing additional chronic conditions.16 Patients with depressive symptomatology also have less favorable perceptions of doctor-patient communications.17 Despite this growing body of evidence linking depression, perceptions of access to care, and use of health services, no research has empirically examined whether depressed patients are less likely to obtain preventive care because they perceive less access to care. Our goal was to address this gap by investigating multiple dimensions of perceived access as potential mediators linking depressive symptoms to reduced preventive service use in older adults. Information about these underlying pathways could inform interventions to improve preventive service use in depressed older adults, particularly in patients whose depressive symptoms are persistent.
Conceptual Model
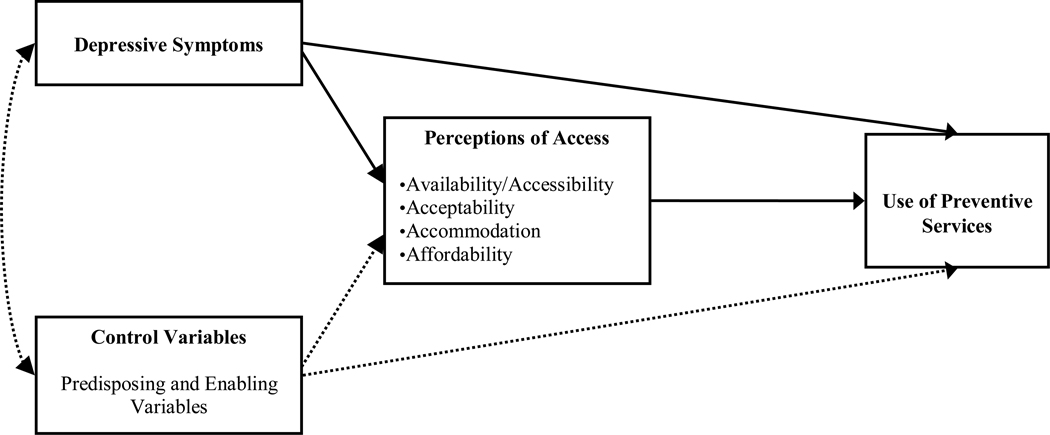
Figure 1 shows our conceptual model of the proposed causal pathway leading from depressive symptoms to receipt of clinical preventive services via perceptions of access to care. We organize perceived access into dimensions described by Penchansky (1981): Availability/Accessibility, Acceptability, Accommodation, and Affordability.18 Availability and Accessibility are related constructs pertaining to the adequacy of supply of healthcare providers and location of providers relative to patients. Acceptability is defined as the interaction between patient and provider attitudes and preferences about what constitutes acceptable personal and treatment practices, with a focus on trust and patient-provider communication in the current study. Accommodation refers to how well the providers’ operations are organized to accommodate patients’ constraints and preferences (e.g., suitable hours of operation). Affordability refers to the relationship of prices of services to patient income, insurance, and overall ability to pay.
Figure 1.
Model of the relationships between depressive symptoms, perceptions of access, and use of preventive services. Solid lines represent pathways of primary interest in the current analysis. Dashed lines represent control pathways.
Depressive symptoms may influence how patients perceive some or all of these dimensions of access to health care, which may in turn influence their preventive service use. In addition to depressive symptoms, the Andersen Socio-Behavioral Model (SBM) of health service use19 suggests that a number of other predisposing, enabling, and medical need factors may shape respondents’ perceptions about access to care and actual preventive service use. In the case of preventive services, where it is recommended that nearly all older adults need the service, illness and impairment do not directly increase medical need for preventive care. Rather, illness, in this context, is conceptualized as a predisposing factor as it acts to increase propensity for using health services.7,8
METHODS
Sample
The sample was drawn from the 2003/2004 wave of the Wisconsin Longitudinal Study (WLS), a longitudinal study of 10,317 randomly sampled graduates from Wisconsin high schools in 1957 that has been described in detail elsewhere.20 In 2003/2004, 8,578 surviving WLS graduates, then aged 63–67, were invited to participate, and 6,279 respondents completed both the phone and mail interviews (73%). To facilitate sensitivity analyses using depressive symptoms measured prior to perceived access and preventive services use, we further excluded 814 respondents who did not complete the prior WLS mail survey fielded in 1993 (final n=5,465).
Measures
Depressive Symptoms
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item self-report scale designed to measure depressive symptomatology in the general population, and subsequently validated in community-dwelling older adults.21,22 Scores range from 0 to 60, with higher scores indicating greater depressive symptoms (Cronbach’s alpha = 0.88). We transformed CES-D scores into a dichotomous variable using the standard cutoff of 16 indicating depressive symptomatology.23
Perceived Access
The 2003/2004 WLS included 18 items pertaining to perceived access to health care. Twelve items originated from the Group Health Association of America (GHAA) Consumer Satisfaction Survey’s23 Access subscale. Each item begins with the stem: “Thinking about your own health care, how would you rate…”. Response options were excellent, very good, good, fair, poor. Specific GHAA items are listed in Table 1, but examples include: access to emergency care, access to specialty care, services for filling prescriptions, convenience of their provider’s location, the amount paid out-of-pocket for co-payments, deductibles or services not covered by insurance, and whether their doctor sufficiently explains the purpose of medical procedures and tests. No significant skew or kurtosis (skew > 2, kurtosis > 7) was noted for any of the 18 items.24
Table 1.
Items and Dimensionality of the Perceived Access to Care Measure* (n=5,465)
| Perceived Access Items | Primary factor loading |
|---|---|
| Availability/Accessibility (Cronbach’s α reliability = .90) | |
| Emergency care | .90 |
| Specialists | .84 |
| Hospital care | .96 |
| Mental health care | .72 |
| Services for filling prescription medications | .55 |
| Convenience of provider’s location | .48 |
| Accommodation (Cronbach’s α = .84) | |
| How soon can get in to be seen for routine care | .82 |
| Time spent waiting in office for provider | .77 |
| Availability of medical information/advice by phone | .67 |
| Amount of time with doctor and staff during visit | .49 |
| Acceptability (Cronbach’s α = .84) | |
| Doctor sufficiently explains procedures/tests | .78 |
| Doctor is honest in telling you about treatment options | .79 |
| Doctor pays attention | .79 |
| Doctor sufficiently involves in treatment decisions | .67 |
| Doctor discusses treatment options as long as wanted | .58 |
| Affordability (Cronbach’s α = N/A) | |
| Amount paid out-of-pocket for medical services | N/A** |
Perceived access items were selected primarily from the Group Health Association of America’s Consumer Satisfaction Survey.
Reliability and factor loadings cannot be calculated from single item.
We performed a principal factor analysis (PFA) to examine item dimensionality using parallel analysis to determine the optimal number of factors for extraction.25,26 Details of the complete factor analysis can be found in Appendix II. PFA revealed a 3-factor solution, and we followed with an oblique factor rotation to allow for possible correlation among factors. Item factor loadings corresponded to three of the access dimensions described by Penchansky: availability, accommodation, and acceptability.18 Two items, hours the doctor’s office is open, arrangements for making appointments by phone, were ultimately deleted due to low primary loadings or high cross-loadings.27 Amount paid out-of-pocket, while not included in the final PFA because of a failure to load highly on any of the 3 dimensions, was retained as its own separate access dimension because it was the only item representing Penchansky’s affordability dimension. Internal consistency reliabilities (Cronbach’s alpha) were calculated for each identified dimension (see Table 1). We constructed scores for each access dimension by summing items within identified dimensions. Higher scores on each subscale indicate greater perceived access.
Preventive Care
The WLS used self-report to capture the respondent’s receipt of 7 guideline- or expert-recommended preventive services appropriate for both men and women of the ages represented in the WLS sample.28,29 These included receipt in the past year of an (1) influenza vaccination, (2) cholesterol test, (3) blood pressure check, (4) routine dental check-up, (5) routine physical examination or check-up, (6) eye examination; and (7) whether they ever received a colon cancer screening such as colonoscopy, sigmoidoscopy, or endoscopy. Our primary outcome variable was a count of the total number of recommended services received.
Covariates (SBM variables)
Predisposing variables are intrapersonal factors that affect one’s propensity for using health services (e.g., demographics), and in this study included age (years), sex (0=female, 1=male), marital status (0=unmarried, 1=married), years of formal education, and several indicators of illnesses or impairments. In the WLS, diagnoses of 21 common conditions were assessed via self-report. We created one variable representing the total number of diagnosed conditions, and also included indicators for 6 of the most common conditions in older adults: diabetes, hypertension, heart problems, cancer in the past 5 years, arthritis or rheumatism, and stroke. The WLS also administers the Health Utilities Index Mark III (HUI-III).30 We created dichotomous variables representing the presence of any reported limitation with regard to five of the eight attributes from the HUI-III: cognition, vision, hearing, speech, and dexterity; we excluded items related to emotion, ambulation, and pain attributes due to potential overlap with other independent variables (e.g., somatic complaints in CES-D). HUI item response options 2–6 indicate at least some level of perceived limitation and were coded as a limitation in this study (any limitation=yes).
Enabling variables are factors that either facilitate or impede access to health services. Individual-level enabling variables included perceived financial inadequacy, measured as the sum of two items probing respondents’ dissatisfaction with their present financial situation (1=not at all, 2=not very, 3=somewhat, 4=very, 5=completely) and difficulty with meeting monthly payments for bills (1=not at all, 2=slightly, 3=somewhat, 4= very, 5= extremely); health insurance coverage (0=any private insurance, 1=public insurance only [eg, Medicaid, Medicare, VA], 2=no insurance); current employment status (0=not employed, 1=currently employed); perceived environmental mastery, calculated as the sum of 5 items from Ryff’s Psychological Well-Being Inventory (Cronbach’s alpha=0.67); and social involvement, measured as frequency of social visits with friends and family members in the past month. We also used 2 county-level enabling variables from the Area Resource File based on the respondent’s county of residence: whole-county designation as a Primary Care Shortage Area,31 and rurality defined using 2003 county-level Urban Influence Codes (UIC),32 collapsed into categories of large and small metropolitan, micropolitan, and non-core rural.
Data Analysis
We used STATA 11.0 (Stata, College Station, TX) to conduct the PFA and generate descriptive statistics for all variables, and Mplus 6.0 (Muthén and Muthén, Los Angeles, CA) to conduct all multivariate models. With less than 10% missing, we reclaimed missing cases using conditional mean imputation to generate a single complete dataset.33 Path analysis was used to estimate, via simultaneous regression models, the total, direct, and indirect (mediated) effects shown in Figure 1 for pathways among depressive symptomatology (key independent variable) and Andersen model variables (control variables), perceived access variables (mediators), and total number of preventive services received (dependent variable). The total effects of depressive symptomatology are made up of both the direct effects (unmediated pathway) and indirect effects (pathways mediated through other variables such as perceived access to care). The indirect effects of depressive symptomatology on total preventive services received, via perceived access, were generated using the product of regression coefficients, which overcomes some documented shortcomings of Baron and Kenny’s causal steps approach, including low statistical power and effects of suppressor pathways.34 Because the sampling distribution of the product of coefficients is not normally distributed, we bootstrapped all standard errors and 95% confidence intervals.35
Sensitivity Analyses
We examined the sensitivity of our findings to alternative coding schemes and measures of depressive symptomatology, via the following analyses: 1) replacing the dichotomous CES-D measure with the continuous CES-D score; 2) using CES-D scores collected approximately 10 years prior to collection of the current study outcomes as the primary independent variable in place of CES-D scores measured concurrently; 3) adding CES-D scores collected 10 years prior as an additional control variable; 4) using alternative CES-D cutoff scores (CES-D >= 17, 18, 19, 20); 5) conducting a stratified analysis by age (<65 years vs. 65 years and up); and 6) treating the overall count of preventive services received as an ordered categorical variable in Mplus (i.e., ordered probit analysis using a weighted least squares estimator). Estimates for the primary relationships of interest between depressive symptomatology, perceived access and preventive service use did not change substantively in any of these analyses (results available upon request).
Further, to examine the impact of aggregating preventive services into a single count variable, we conducted separate analyses for each preventive service type and present results in Appendix Table 1.
RESULTS
Description of Sample
Table 2 illustrates the WLS respondent sample characteristics. Of the 5,465 respondents, 15.1% had clinically significant depressive symptomatology. The mean age was 64 years, 46% were male, and nearly 80% were married. Eighty-seven percent of respondents had private health insurance, 10% had public insurance only, and 3% reported no health insurance. Respondents had, on average, 3.1 diagnosed conditions, and had received 4.9 of the 7 preventive services.
Table 2.
Description of Sample (n=5,465)
| Variable Range in Sample |
||||
|---|---|---|---|---|
| Study Variables | Mean or Percent |
SD | Minimum | Maximum |
| Depressive symptomatology (CES-D ≥ 16), % | 15.1 | 0 | 1 | |
| Predisposing characteristics | ||||
| Age | 64.3 | 0.7 | 63 | 67 |
| Male, % | 45.6 | 0 | 1 | |
| Married, % | 79.7 | 0 | 1 | |
| Education, years | 13.8 | 2.4 | 12 | 21 |
| Any cognitive limitations, % | 25.4 | 0 | 1 | |
| Any dexterity limitations, % | 2.0 | 0 | 1 | |
| Any speech limitations, % | 2.0 | 0 | 1 | |
| Any hearing limitations, % | 3.9 | 0 | 1 | |
| Any vision limitations, % | 1.0 | 0 | 1 | |
| Count of diagnosed conditions | 3.1 | 2.3 | 0 | 17 |
| Diabetes, % | 11.7 | 0 | 1 | |
| Hypertension, % | 47.4 | 0 | 1 | |
| Heart problems, % | 14.9 | 0 | 1 | |
| Cancer in past 5 years, % | 5.2 | 0 | 1 | |
| Arthritis or rheumatism, % | 45.3 | 0 | 1 | |
| Stroke, % | 2.9 | 0 | 1 | |
| Individual-Level Enabling characteristics | ||||
| Perceived financial inadequacy | 3.6 | 1.5 | 1 | 10 |
| Health insurance | ||||
| Any private insurance, % | 86.6 | 0 | 1 | |
| Public insurance only, % | 10.1 | 0 | 1 | |
| Uninsured, % | 3.3 | 0 | 1 | |
| Currently employed, % | 42.9 | 0 | 1 | |
| Environmental Mastery | 24.6 | 3.9 | 1 | 33 |
| Social involvement with friends/family (# visits/month) | 7.3 | 5.9 | 0 | 56 |
| County-Level Enabling characteristics | ||||
| County rurality | ||||
| Large metropolitan, % | 33.7 | 0 | 1 | |
| Small metropolitan, % | 38.0 | 0 | 1 | |
| Micropolitan, % | 15.0 | 0 | 1 | |
| Rural (non-core), % | 13.3 | 0 | 1 | |
| Primary Care Shortage Area, % | 2.9 | 0 | 1 | |
| Perceived Access Subscale Scores (potential mediators) | ||||
| Availability of services | 23.1 | 4.4 | 6 | 30 |
| Acceptability of services | 20.2 | 3.4 | 5 | 25 |
| Accommodation | 13.2 | 3.1 | 4 | 20 |
| Affordability | 3.1 | 1.1 | 1 | 5 |
| Total Number of Preventive Services Received* | 4.9 | 1.6 | 0 | 7 |
Total count of the following preventive care services received: influenza vaccination; screening for high cholesterol; screening for hypertension; screening for colon cancer; routine dental check-up; routine physical examination or check-up; and eye examination.
SD, standard deviation. CES-D, Center for Epidemiologic Studies – Depression scale.
Direct Effects of Study Variables on Perceived Access and Receipt of Preventive Services
Table 3 shows the direct (unmediated) effects of study variables on perceived access and total number of preventive services received. The first four columns display direct effects of depressive symptomatology and control variables on the four perceived access dimensions (relationship between independent variables and mediators). Depressive symptomatology was significantly associated with two of the access dimensions, acceptability (B = −.463, P < .01) and accommodation (B = −.428, P < .01), but was not significantly related to perceived availability and affordability. The last column shows both the direct effects of the perceived access variables on preventive service use, as well as the direct (unmediated) effects of depressive symptomatology and the control variables on total number of preventive services received. For all four access dimensions, greater perceived access was associated with increased use of preventive services.
Table 3.
Direct Effects†‡ of Study Variables on Perceived Access and Total Number of Preventive Services Received (n=5,465)
| Perceived Access |
|||||
|---|---|---|---|---|---|
| Availability | Acceptability | Accommodation | Affordability | # Preventive Services | |
| Bdirect | Bdirect | Bdirect | Bdirect | Bdirect | |
| Perceived Access | |||||
| Availability | -- | -- | -- | -- | .018** |
| Acceptability | -- | -- | -- | -- | .037** |
| Accommodation | -- | -- | -- | -- | .023* |
| Affordability | -- | -- | -- | -- | .093** |
| Depressive symptomatology | |||||
| (CES-D ≥ 16) | −.260 | −.463** | −.428** | −.001 | −.087 |
| Predisposing characteristics | |||||
| Age | −.015 | .014 | .103 | .083** | −.007 |
| Male | −.436** | −.261** | −.315** | −.019 | −.132** |
| Married | .347* | .161 | .221* | .016 | .275** |
| Education in years | .106** | .020 | −.001 | .046** | .080** |
| Any cognitive limitations | −.211 | −.129 | −.170 | −.097* | .158** |
| Any dexterity limitations | −.262 | .151 | −.139 | .011 | −.337* |
| Any speech limitations | −1.298** | −.952* | −.702* | −.156 | −.209 |
| Any hearing limitations | .160 | .253 | .207 | −.023 | .164 |
| Any vision limitations | −.073 | −.115 | .152 | .019 | .193** |
| Count of chronic illnesses | −.003 | −.028 | −.040 | .009 | .156** |
| Diabetes | .155 | .171 | .557** | .126* | .206** |
| Hypertension | .124 | .269** | .279** | .057 | .200** |
| Heart problems | .153 | .281* | .153 | −.015 | .087 |
| Cancer in past 5 years | 1.062** | .690** | .544** | .101 | .065 |
| Arthritis or rheumatism | .178 | .229* | .165 | .041 | .130** |
| Stroke | .406 | .242 | .535* | .046 | -.017 |
| Individual-Level Enabling | |||||
| Perceived financial inadequacy | −.211** | −.076* | −.152** | −.115** | −.060** |
| Health insurance | |||||
| Any private insurance (ref.) | |||||
| Public insurance only | −.096 | .015 | .096 | .078 | −.297** |
| Uninsured | −.374 | −.082 | .350 | −.181 | −1.164** |
| Currently employed | .219 | .005 | −.016 | .069* | −.204** |
| Environmental Mastery | .176** | .183** | .105** | .017** | .004 |
| Social involvement | .031** | .023** | .022** | −.002 | .010** |
| County-Level Enabling | |||||
| County rurality | |||||
| Large metropolitan (ref.) | |||||
| Small metropolitan | −.085 | .074 | .018 | −.004 | .078 |
| Micropolitan | −.349* | .192 | .118 | .065 | −.188** |
| Rural | −1.200** | .053 | .060 | −.159** | −.096 |
| Primary Care Shortage Area | −1.266* | .385 | −.287 | .072 | .196 |
| R2 (adjusted) | .080 | .079 | .053 | .059 | .196 |
significant at 5%;
significant at 1%
Direct effects are unstandardized regression coefficients (B) adjusted for all control variables.
Direct effects for depressive symptomatology and control variables on preventive service use represent the effect of these variables that is not mediated through perceived access dimensions.
CES-D, Center for Epidemiologic Studies – Depression scale.
Formal Test of Perceived Access as Mediator between Depressive Symptoms and Preventive Service Use
Table 4 summarizes the total effects, indirect effects via perceived access, and the direct (unmediated) effect of depressive symptomatology on the number of preventive services used. The total effect (first row) of depressive symptomatology on preventive service use was statistically significant (B = −.119, P < .05). Taken together (second row), the four perceived access dimensions significantly mediated the effect of depressive symptomatology on receipt of preventive services (B = −.032, P < .01); representing 27% of the total effect of depressive symptomatology on receipt of preventive services (not shown in tables). Examination of the specific indirect effects of depressive symptomatology on receipt of preventive services via each perceived access dimension suggests that depressive symptomatology decreased preventive service use by decreasing perceived acceptability (B = −.017, P < .01) and accommodation (B = −.010, P < .01). The indirect effects of depressive symptomatology on receipt of preventive services via perceived availability and affordability were not statistically significant. The direct (unmediated) effect of depressive symptomatology on preventive service use (after accounting for indirect effects via perceived access) was not statistically significant.
Table 4.
Estimates and 95% Confidence Intervals for the Total, Direct, and Indirect Effects† of Depressive Symptomatology on Total Number of Preventive Services Received (n=5,465)
| B | 95% CI | |
|---|---|---|
| Total effect of depressive symptomatology (direct + indirect effects) | −.119* | −0.238, −0.003 |
| Total indirect effect via all perceived access dimensions | −.032** | −0.057, −0.008 |
| Specific indirect effect via Availability | −.005 | −0.015, 0.001 |
| Specific indirect effect via Acceptability | −.017** | −0.032, −0.007 |
| Specific indirect effect via Accommodation | −.010** | −0.023, −0.003 |
| Specific indirect effect via Affordability | .000 | −0.009, 0.009 |
| Direct (unmediated) effect | −.087 | −0.203, 0.026 |
significant at 5%;
significant at 1%
Total, direct, and indirect effects are unstandardized regression coefficients (B) adjusted for all control variables.
CES-D, Center for Epidemiologic Studies – Depression scale.
Sensitivity Analyses: Results for Individual Preventive Services
Results for individual service types (Appendix Table 1) are consistent with those found in Table 4 for the overall count of preventive services, although estimates of indirect effects of depressive symptomatology via accommodation were not significant for 3 of the preventive services (flu shot, colon cancer screen, dental check-up), and were not significant for flu shot via acceptability.
DISCUSSION
Despite the growing body of evidence on the associations between depression and reduced adherence to preventive care guidelines, the pathways through which depression exerts its influence are not well understood. The purpose of this study was to evaluate the role of altered perceptions of access as one possible pathway, and indeed, we found that older adults with depressive symptomatology expressed less favorable perceptions of access and received fewer recommended preventive services. This mediational analysis suggested that depression may largely influence preventive service use by negatively affecting 2 of 4 dimensions of perceived access: (1) acceptability, pertaining to poor patient-provider trust and communication, and (2) accommodation, pertaining to inconveniently organized services. The two other dimensions of access, availability of providers and affordability of services, were not significant mediators.
In this study, older adults with depressive symptomatology found their doctor-patient relationships less acceptable, and this in turn was associated with decreased preventive service use. This finding is consistent with previous research suggesting that depressive symptoms may adversely affect patients’ perceptions of doctor-patient communication,17 and that adherence and improved disease control are linked to satisfaction with interpersonal characteristics of providers.36,37 One explanation for our finding is that providers may be less likely to recommend or deliver preventive services in the presence of depressive symptoms. This possibility is consistent with prior research showing that the content of office visits initiated by depressed patients differs from that of non-depressed patients, with more focus on addressing symptoms and somatic complaints,38 more history taking,39 and less communication about medical topics.40 An alternative explanation is that depressed patients may be more inclined to reject their provider’s recommendations about preventive care because of less favorable views of their providers. As suggested by Williams et al,41 patient trust and rapport may be undermined by physician lack of awareness of patient depression and/or negative reactions to depressive symptoms in patients. Further, previous work suggests that physicians show greater negativity toward emotionally distressed patients,42 and less chatting may occur during depressed patient visits.43 This perceived lack of responsiveness in physicians is seen as a major barrier to seeking care by patients.44 Future research should apply objective measures of patient-physician communication to determine whether and how the content and quality of communication about preventive services, as well as other more general aspects of communication, differs for patients with and without depressive symptomatology, and whether these different aspects of communication are related to patients’ subsequent use of preventive services. Such research would help point to specific aspects of communication to target interventions with depressed patients and their providers to improve adherence to recommended preventive services. At a minimum, increased healthcare provider solicitation of the patient’s complete agenda, and use of open-ended questions during patient visits, may improve doctor-patient communication45 and strengthen the doctor-patient relationship in emotionally distressed older adults.
Our results also suggest that patients with depressive symptomatology perceive greater logistical barriers to scheduling and obtaining medical care, and in turn, this may reduce their tendency to seek recommended preventive services. Patients with depressive symptomatology perceive greater daily stressors46 and report fewer social support resources,47 which could make arranging appointments more difficult compared to non-depressed patients. Alternatively, the medical care system may be objectively similar with its ability (or inability) to accommodate the needs of both depressed and non-depressed patients, but depressed patients may perceive this objective level of accommodation less favorably and be more affected by it in terms of future care-seeking behavior. The latter explanation is consistent with literature suggesting that patients with depressive symptomatology may ruminate over and more readily recall past negative experiences.48 In either case, these results suggest that in order to improve preventive service use among patients with increased depressive symptoms, health care organizations may need to intensify their efforts, perhaps through collaborative care models,49 to reduce accommodation barriers to a range of primary and specialty care services for depressed patients to better meet their needs. Additionally, interventions such as motivational interviewing that are designed to enhance depressed patients’ resolve to seek preventive care in spite of perceived access barriers are avenues for future research.50
Several design and measurement limitations should be noted. First, the WLS includes a cohort of largely non-minority graduates from Wisconsin high schools in 1957, and we further restricted the sample to include only graduates responding to both the 1993 and 2004 survey waves to facilitate sensitivity analyses involving longitudinal data. The uniqueness of this sample may limit generalizeability of findings. Second, because of the non-experimental design, along with the modest explanatory power of our fully-adjusted model (R2=20%), we cannot confirm that the identified associations between depressive symptomatology, perceived access, and receipt of preventive services are causal. However, our adjustment for a range of potential confounders, and substantively unchanged results in sensitivity analyses using depressive symptoms lagged approximately 10 years prior to study dependent variables, reduce the likelihood of residual confounding or reverse causality. Third, receipt of preventive services was based on self-report, and recall bias is a potential concern. In addition, items available in the WLS for measuring perceived access were not designed to evaluate the full complexity of the access dimensions described by Penchansky; as a result, the Availability and Accessibility dimensions described in the Penchansky model may have factored together in the current study due to insufficient item “coverage” to establish discriminant validity. Finally, at the time of this wave of the WLS (2003/2004), adults under age 65 without any underlying chronic medical conditions were not considered a priority group for receiving influenza vaccination. However, because influenza vaccination was generally encouraged for all adults and 90% of adults <65 in our sample reported at least one chronic condition, we felt it important to include influenza vaccination in our summary measure of overall propensity for using preventive services.
Despite these limitations, our analysis raises concerns that reduced use of preventive services in older adults with depressive symptomatology may be due to greater perceived challenges in accessing medical care, specifically with the interpersonal aspects of the patient-provider relationship and how well the healthcare system is organized to accommodate their particular preferences and needs. Our analysis suggests that adherence to recommended preventive care guidelines may be improved directly through improved recognition and treatment of depression, and indirectly through interventions to mitigate the negative impact of depression on the patient-provider relationship, and organizational changes that better accommodate needs of depressed patients.
Appendix Table 1
Indirect Effects of Depressive Symptomatology on Each Preventive Service Type (n=5,465)
| Indirect Effects of Depressive Symptomatology on Each Preventive Service Via… |
||||
|---|---|---|---|---|
| Availability | Acceptability | Accommodation | Affordability | |
| Preventive Service | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) |
| Influenza vaccination | −.005 | −.001 | −.003 | .000 |
| Blood pressure screen | −.003 | −.007* | −.016** | .000 |
| Routine checkup | −.004* | −.008** | −.014* | .000 |
| Colon cancer screen | −.006 | −.005* | .000 | .000 |
| Dental checkup | −.003* | −.009* | .003 | .000 |
| Routine exe examination | .004 | −.006** | −.011** | .000 |
| Cholesterol screen | .000 | −.007** | −.015** | .000 |
Coefficients are unstandardized probit regression coefficients, adjusted for predisposing, enabling, and need variables.
significant at 5%;
significant at 1%
Appendix II. Detailed Description of Factor Analysis on Perceived Access Items
The 2003 WLS included 18 items pertaining to perceived access to health care. Twelve items originated from the Group Health Association of America (GHAA) Consumer Satisfaction Survey’s23 Access subscale and assessed respondent’s satisfaction (using a Likert scale of excellent, very good, fair, poor) with (1) access to emergency care, (2) access to specialty care, (3) access to a hospital, (4) access to mental health care, (5) services for filling prescriptions, (6) convenience of their provider’s location, (7) length of time between making an appointment and day of the appointment, (8) hours when the doctor’s office is open, (9) arrangements for making appointments by phone, (10) length of time spent waiting at the office to see the doctor, (11) availability of medical information or advice by phone, and (12) amount of time spent with doctors and staff during a visit. In addition, a single item (13) asked patients to rate the amount paid out-of-pocket for co-payments, deductibles or services not covered by insurance; and 5 items evaluated respondents’ perceptions of interpersonal aspects of health care providers, by asking respondents the extent to which they agreed that the doctor (14) sufficiently explains the purpose of medical procedures and tests; (15) is totally honest about all treatment options available; (16) always pays complete attention to what the patient is saying; (17) has involved them in discussing treatment options as much as they would like; and (18) discusses treatment options for as long as they would like. No significant skew or kurtosis (skew > 2, kurtosis > 7) was noted for any of the 18 items.1
We performed a factor analysis to examine item dimensionality and scale reliabilities. As suggested by Bartholomew et al. (2002),2 we first conducted a principal components analysis (PCA) of the 18 access items to determine the optimal number of factors to extract for subsequent principal axis factor analysis (PAF).3 PCA revealed a 3-dimension solution. Therefore, we conducted a PAF imposing a 3-factor solution followed by an oblique factor rotation, to allow for possible correlation among access dimensions. Following established guidelines,4 we chose to retain only items achieving a rotated factor loading of 0.45 or greater on their primary factor, and discarded items with cross-loadings of 0.30 or greater on any secondary factor. Item factor loadings from the PAF corresponded to three of the access dimensions described by Penchansky and Thomas: availability, accommodation, and acceptability.5 Items 8 and 9 were ultimately deleted due to low primary loadings or high cross-loadings. Item 13 (amount paid out-of-pocket), while not included in the final PAF because of a failure to load highly on any of the 3 dimensions, was retained as its own separate access dimension because it was the only item representing Penchansky’s affordability dimension. A final PAF was conducted on the remaining set of items, and internal consistency reliabilities (Cronbach’s alpha) were calculated for each dimension of access (see Table 1). We constructed scores for each access dimension by summing items within identified dimensions, with higher scores indicating greater perceived access. Higher scores on each subscale indicate greater perceived access.
References
- 1.Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. [Google Scholar]
- 2.Bartholomew DJ, Steele F, Moustaki I, Galbraith JI. The Analysis and Interpretation of Multivariate Data for Social Scientists. Boca Raton, FL: Chapman & Hall; 2002. [Google Scholar]
- 3.Horn JL. A rationale and technique for estimating the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 4.Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 5.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981 Feb;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
REFERENCES
- 1.Fiore AE, Shay DK, Broder K, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep. 2009 Jul 31;58(RR-8):1–52. [PubMed] [Google Scholar]
- 2.Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008 Nov 4;149(9):638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force. Summaries for patients. Screening for coronary heart disease: recommendations from the United States Preventive Services Task Force. Ann Intern Med. 2004 Apr 6;140(7):I95. doi: 10.7326/0003-4819-140-7-200404060-00049. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Service. Healthy People 2010: With Understanding and Improving Health and Objectives for Improving Health. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 5.Kilmer G, Roberts H, Hughes E, et al. Surveillance of certain health behaviors and conditions among states and selected local areas--Behavioral Risk Factor Surveillance System (BRFSS), United States, 2006. MMWR Surveill Summ. 2008 Aug 15;57(7):1–188. [PubMed] [Google Scholar]
- 6.Witt WP, Kahn R, Fortuna L, et al. Psychological distress as a barrier to preventive healthcare among U.S. women. J Prim Prev. 2009 Sep;30(5):531–547. doi: 10.1007/s10935-009-0190-z. [DOI] [PubMed] [Google Scholar]
- 7.Thorpe JM, Kalinowski CT, Patterson ME, Sleath BL. Psychological distress as a barrier to preventive care in community-dwelling elderly in the United States. Med Care. 2006 Feb;44(2):187–191. doi: 10.1097/01.mlr.0000196965.54871.d5. [DOI] [PubMed] [Google Scholar]
- 8.Thorpe JM, Sleath BL, Thorpe CT, et al. Caregiver psychological distress as a barrier to influenza vaccination among community-dwelling elderly with dementia. Med Care. 2006 Aug;44(8):713–721. doi: 10.1097/01.mlr.0000215905.36968.76. [DOI] [PubMed] [Google Scholar]
- 9.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000 Jul 24;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 10.Nutt DJ. Rationale for, barriers to, and appropriate medication for the long-term treatment of depression. J Clin Psychiatry. 71 Suppl E1:e02. doi: 10.4088/JCP.9058se1c.02gry. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez J, Williams JW., Jr . The effects of clinical depression and depressive symptoms on treatment adherence. In: Bosworth HB, Oddone EZ, Weinberger M, editors. Patient Treatment Adherence: Concepts, Interventions, and Measurement. Mahwah (NJ): Lawrence Erlbaum; 2005. [Google Scholar]
- 12.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010 Jan 6;303(1):47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas JW, Penchansky R. Relating satisfaction with access to utilization of services. Med Care. 1984 Jun;22(6):553–568. doi: 10.1097/00005650-198406000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Weinberger MI, Mateo C, Sirey JA. Perceived barriers to mental health care and goal setting among depressed, community-dwelling older adults. Patient Prefer Adherence. 2009;3:145–149. doi: 10.2147/ppa.s5722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shavers VL, Shankar S, Alberg AJ. Perceived access to health care and its influence on the prevalence of behavioral risks among urban African Americans. J Natl Med Assoc. 2002 Nov;94(11):952–962. [PMC free article] [PubMed] [Google Scholar]
- 16.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995 Apr 5;273(13):1026–1031. [PubMed] [Google Scholar]
- 17.Schenker Y, Stewart A, Na B, Whooley MA. Depressive symptoms and perceived doctor-patient communication in the Heart and Soul study. J Gen Intern Med. 2009 May;24(5):550–556. doi: 10.1007/s11606-009-0937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981 Feb;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981 Dec;19(12 Suppl):4–27. [PubMed] [Google Scholar]
- 20.Hauser R. Survey Response in the Long Run: The Wisconsin Longitudinal Study. Field Methods. 2005;17:3–29. [Google Scholar]
- 21.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. 1977;1:385–401. [Google Scholar]
- 22.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997 Jun;12(2):277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 23.McDowell I. Measuring Health: A Guide to Rating Scales and Questionnaires. 3rd ed. Oxford: Oxford University Press; 2006. [Google Scholar]
- 24.Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. [Google Scholar]
- 25.Horn JL. A rationale and technique for estimating the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 26.Bartholomew DJ, Steele F, Moustaki I, Galbraith JI. The Analysis and Interpretation of Multivariate Data for Social Scientists. Boca Raton, FL: Chapman & Hall; 2002. [Google Scholar]
- 27.Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 28.U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. Washington, DC: U.S. Department of Health and Human Services; 1996. [Google Scholar]
- 29.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 30.Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002 Feb;40(2):113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Bureau of Primary Health Care Programs, Health Resources and Services Administration. [Accessed May 2007];Guidelines for Primary Care HPSA Designation. http://bhpr.hrsa.gov/shortage/hpsaguidepc.htm.
- 32.U.S. Department of Agriculture Economic Research Service. Measuring Rurality: Urban Influence Codes. 2003 http://www.ers.usda.gov/Briefing/Rurality/urbaninf/.
- 33.Shrive FM, Stuart H, Quan H, Ghali WA. Dealing with missing data in a multi-question depression scale: a comparison of imputation methods. BMC Med Res Methodol. 2006;6:57. doi: 10.1186/1471-2288-6-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mackinnon DP, Fairchild AJ. Current directions in mediation analysis. Curr Dir Psychol Sci. 2009 Feb 1;18(1):16. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yung Y, Chan W. Statistical Analyses Using Bootstrapping: Concepts and Implementation. In: Hoyle R, editor. Statistical Strategies for Small Sample Research. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 36.Harris LE, Luft FC, Rudy DW, Tierney WM. Correlates of health care satisfaction in inner-city patients with hypertension and chronic renal insufficiency. Soc Sci Med. 1995 Dec;41(12):1639–1645. doi: 10.1016/0277-9536(95)00073-g. [DOI] [PubMed] [Google Scholar]
- 37.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet Med. 2003 Jun;20(6):486–490. doi: 10.1046/j.1464-5491.2003.00957.x. [DOI] [PubMed] [Google Scholar]
- 38.Howren MB, Suls J, Martin R. Depressive symptomatology, rather than neuroticism, predicts inflated physical symptom reports in community-residing women. Psychosom Med. 2009 Nov;71(9):951–957. doi: 10.1097/PSY.0b013e3181b9b2d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Callahan EJ, Jaen CR, Crabtree BF, Zyzanski SJ, Goodwin MA, Stange KC. The impact of recent emotional distress and diagnosis of depression or anxiety on the physician-patient encounter in family practice. J Fam Pract. 1998 May;46(5):410–418. [PubMed] [Google Scholar]
- 40.Roter D. Elderly patient-physician communication: A descriptive study of content and affect during the medical encounter. Advances in Health Education. 1991;3:179–190. [Google Scholar]
- 41.Williams SL, Haskard KB, DiMatteo MR. The therapeutic effects of the physician-older patient relationship: effective communication with vulnerable older patients. Clin Interv Aging. 2007;2(3):453–467. [PMC free article] [PubMed] [Google Scholar]
- 42.Hall JA, Roter DL, Milburn MA, Daltroy LH. Patients' health as a predictor of physician and patient behavior in medical visits. A synthesis of four studies. Med Care. 1996 Dec;34(12):1205–1218. doi: 10.1097/00005650-199612000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Callahan EJ, Bertakis KD, Azari R, Robbins J, Helms LJ, Miller J. The influence of depression on physician-patient interaction in primary care. Fam Med. 1996 May;28(5):346–351. [PubMed] [Google Scholar]
- 44.Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to health care access among the elderly and who perceives them. Am J Public Health. 2004 Oct;94(10):1788–1794. doi: 10.2105/ajph.94.10.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient's agenda: have we improved? JAMA. 1999 Jan 20;281(3):283–287. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- 46.Serido J, Almeida DM, Wethington E. Chronic stressors and daily hassles: unique and interactive relationships with psychological distress. J Health Soc Behav. 2004 Mar;45(1):17–33. doi: 10.1177/002214650404500102. [DOI] [PubMed] [Google Scholar]
- 47.Mitchell RE, Moos RH. Deficiencies in social support among depressed patients: antecedents or consequences of stress? J Health Soc Behav. 1984 Dec;25(4):438–452. [PubMed] [Google Scholar]
- 48.Mineka S, Nugent K. Mood-congruent memory biases in anxiety and depression. In: Schacter D, editor. Memory Distortion: How Minds, Brains, and Societies Reconstruct the Past. Cambridge, MA: Harvard University Press; 1995. [Google Scholar]
- 49.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006 Nov 27;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 50.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005 Apr;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]