Abstract
Background/Aims
Although notably common, irritable bowel syndrome (IBS) has no specific cure. Lifestyle modification may be as important as medication; however, few studies support the effectiveness of such modifications. We performed this observational study of IBS patients to explore further the role of lifestyle changes in treatment.
Methods
This study included 831 men who enlisted in 2010 as armed surgeon cadets and 85 women who concurrently entered the Armed Forces Nursing Academy. Of these 916 participants, 89 were diagnosed with IBS using the Rome III criteria. Subjective changes in bowel habits, quality of life, pain, stress, stool frequency and stool consistency were surveyed before and after 9 weeks of army training. We evaluated the lifestyle risk factors that impacted improvement in IBS symptoms by comparing those who responded to lifestyle modification (the responding group) to those who did not respond (the nonresponding group).
Results
More than half of the participants (63%) reported that their symptoms improved after training. The quality of life and levels of pain and stress significantly improved after military training. Initial stress levels before military training and smoking history affected IBS symptom improvement.
Conclusions
Lifestyle modification may be effective in managing IBS patients.
Keywords: Irritable bowel syndrome, Life style, Smoking, Stress
INTRODUCTION
Irritable bowel syndrome (IBS) is a condition characterized by abdominal pain, bloating, and/or other discomforts associated with disturbed bowel patterns in the absence of organic causes detectable by routine medical tests.1 IBS is a very common disorder with a prevalence that ranges from 2.5% to 37% in many studies.2 A Korean study reported the prevalence of IBS as 6.6%.3 IBS accounts for 28% of the gastroenterology case load,4 and 12% of that is in primary care clinics.5 Although common, IBS is poorly understood. In particular, multiple factors interact, such as genetic background, gut infections, brain-gut interactions, and psychological disturbance.1 The multifactorial character and the absence of a cure for IBS compel patients and providers to work together over time to manage this condition.6 As in most chronic conditions that are not medically curable, self-management is crucially important in IBS. Interestingly, many physicians emphasize the importance of lifestyle modification in IBS, but have few resources to consult on the actual effectiveness of their recommendations. Relevant lifestyle modifications include sharp reductions in drinking and smoking, and maintenance of regular habits concerning sleep, meals, and exercise.
A community-based lifestyle modification study is likely to encounter poor compliance. In the Republic of Korea, all young men must perform obligatory military service. During military training, alcohol and smoking are curtailed, regular meals and physical training provided, and regular hours enforced. Hence military training imposes lifestyle modification in a controlled setting. We hypothesized that in this stable situation, the quality of life (QoL) and control of IBS symptoms would improve. Thus, we studied the impact of life style modification during military training in IBS patients and assessed which factors were associated with IBS symptom improvement. To our knowledge, this is the first prospective study of lifestyle modification in Korean patients with IBS.
MATERIALS AND METHODS
1. Participants
Screening for IBS was conducted among 831 armed surgeon cadets who were enlisted in 2010 and 85 women who concurrently entered the Armed Forces Nursing Academy. All armed surgeon cadets were males and had worked in civilian hospitals before joining the army. All trainees entering the Armed Forces Nursing Academy were females. Before gathering information, researchers obtained informed consent from all participants. No one was pressured or coerced to participate and no commercial incentive was given. IBS was diagnosed using Rome III criteria. A primary survey was conducted of the participants who were diagnosed with IBS to determine QoL, degree of abdominal pain and stress, and socioeconomic factors including age, cause of stress, smoking, alcohol intake, and marital status. In the survey, smoking meant current smoker, and alcohol meant a habit of drinking alcohol; quantity of smoking and alcohol consumption were not assessed. No participant had a history of any disease that could interfere with military training.
2. Lifestyle modification
During military training, drinking alcohol and smoking were forbidden. Regular meals were supplied and physical activities including jogging and muscle training were performed as scheduled. Military training also included shooting and marching. All participants kept regular hours. Observation was conducted during the training course with no intervention of any kind.
3. Assessment and analysis
We evaluated subjective improvement of bowel habit, QoL, degree of pain, stool frequency, stool consistency, and stress level in IBS patients before and after military training. The primary survey asked about the past 3 months. After 9 weeks of observation, a follow-up survey asked about the most recent week. For subjective bowel habit change, the participants chose one of three following answers: improvement, no change, and aggravation. To assess QoL, participants completed an IBS-specific, 34-item questionnaire developed by Patrick using a self-rating scale for each health-related item.7 When scored, all items are reversed so that as the IBS-QOL score increases, QoL increases. All final raw scores are transformed into a 0 (poor QoL) to 100 (maximum QoL). The questionnaire was translated from English to Korean by the authors. Participants were asked to rate their subjective abdominal pain or discomfort and stress level on a visual analogue scale (score range, 0 to 100). Stool frequency by IBS subtype and Bristol Stool Form Scale were evaluated before and after military training. Comparisons before and after military training were performed to evaluate differences in QoL, abdominal pain, stress, stool frequency and stool consistency. The participants were divided into 2 groups based on the subjective bowel habit change, a responding group who chose "improvement" after training and a nonresponding group who chose "no change" or "aggravation." Group analysis was conducted to evaluate differences in age, body weight, smoking, sex, alcohol consumption, marital status, and degree of stress, and through this analysis, identify modifiable risk factors for IBS.
4. Statistics
Comparisons before and after military training were made using paired t-tests. Participants were divided into 2 groups: normal stool group (Bristol type 3, 4, and 5) and abnormal stool group (Bristol type 1, 2, 6, and 7). Difference in stool consistency was analyzed with the Mcnemar test. Kruskal-wallis test was used to evaluate stool frequency according to IBS subtype. Group analysis was performed using independent t-tests, Pearson's chi-square test, and Fisher's exact test. We performed multivariate logistic regression to evaluate lifestyle risk factors for IBS while adjusting for other covariates. The model included all the risk factors surveyed in this study. A p-value of less than 0.05 was considered statistically significant. All statistical evaluations were performed with SPSS for Windows version 13.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
1. Characteristics of subjects
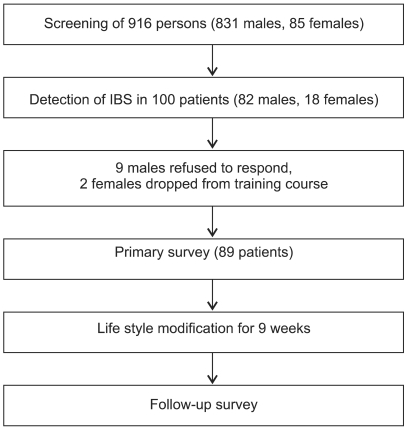
Among 831 armed surgeon cadets and 85 trainees in the Armed Forces Nursing Academy, 100 individuals (82 males, 18 females) were diagnosed with IBS from their first screening. Of the 100 persons diagnosed with IBS, 11 did not participate in the study. Nine armed surgeon cadets refused to respond to the questionnaire and 2 trainees at the nursing academy dropped out during the training course for personal reasons. Eighty-nine patients (73 males, 16 females) diagnosed with IBS completed both surveys, before and after military training (Fig. 1).
Fig. 1.
Study participant flow. Eighty-nine persons are eventually enrolled.
IBS, irritable bowel syndrome.
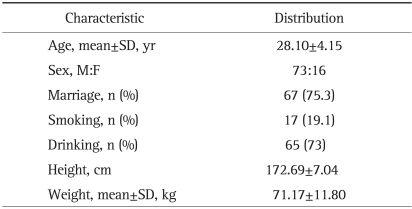
General characteristics of the study subjects are presented in Table 1. Participants' average age was 28.1 years (standard deviation, 4.15) and 73 participants (82%) were male. All participants were Korean. Mixed type of IBS was predominant (44.9%), followed by IBS with diarrhea (42.7%) and IBS with constipation (12.4%).
Table 1.
Baseline Characteristics of Patients (n=89)
2. Comparison of major outcomes before and after military training
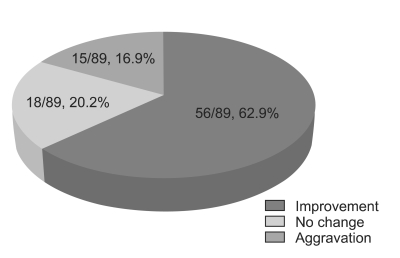
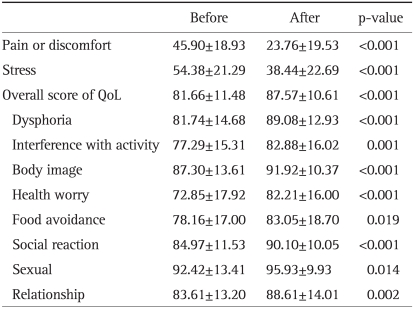
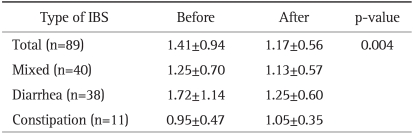
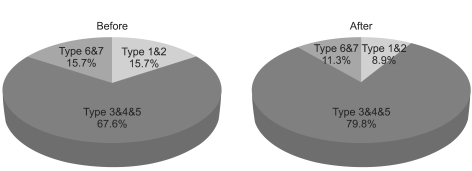
Bowel habits improved in 62.9% of participants, symptoms worsened in 16.9%, and 20.2% of participants showed no change in their bowel habits (Fig. 2). The mean scores of the pre-training survey for QoL, abdominal pain or discomfort, and stress were improved after 9 weeks of training. All subscale structures of the QoL scoring system,7 including dysphoria, interference with activity, and body image, also showed significant increases (p<0.05, Table 2). Mean stool frequency was also reduced. After training, there were no differences in stool frequency according to IBS subtype (Table 3). The number of participants with normal stool consistency (Bristol Stool Form Scale type 3, 4, or 5) increased after military training (p=0.049, Fig. 3).
Fig. 2.
Changes in bowel habits after training. Approximately 60% of participants reports improvement after training.
Table 2.
Comparison of Abdominal Pain or Discomfort, Stress, and Overall QoL
Data are presented as mean±SD.
QoL, quality of life; Before, before modification; After, after modification.
Table 3.
Comparison of Stool Frequency Based on IBS Subtype
Data are presented as mean±SD.
One bowel movement per 2 days was presented as 0.5/day.
Stool frequency, which was significantly different between groups before training (p=0.031, Kruskal-Wallis test), showed no difference when reexamined after training (p=0.335).
IBS, irritable bowel syndrome.
Fig. 3.
Changes in stool consistency after training. The percentage of stools of normal consistency (type 3, 4, 5) increases after training (Mcnemar test, p=0.049).
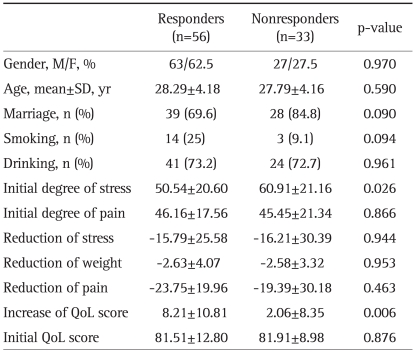
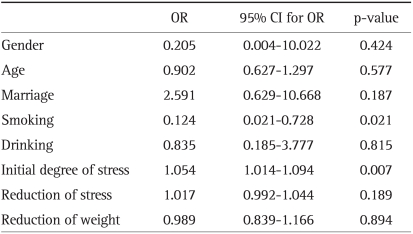
3. Comparison between responders and nonresponders
The responding group had a significantly lower initial stress level (Student's t-test). There was also a nonsignificant higher percentage of smokers in the responding group (p=0.094, Fisher's exact test). The responding group also showed a greater reduction in the QoL score (Table 4). Age, sex, marital status, use of alcohol, stool frequency, and Bristol Stool Form Scale did not differ between groups. Smoking and initial stress level were significant variables in logistic regression analysis (Table 5).
Table 4.
Comparison between Responders and Nonresponders
QoL, quality of life.
Table 5.
Results of the Multivariate Logistic Regression Model Predicting Subjective Bowel Habit Change
OR, odds ratio; CI, confidence interval.
DISCUSSION
IBS is a life-long disease. Despite the continual development of new drugs, the management of IBS remains a challenge. As in other chronic illnesses, "control" rather than "treatment" is the key management concept in IBS, and the importance of self-management as an effective alternative to drug therapy is becoming increasingly accepted. Self-managing IBS patients continue to visit their physicians but spend much less time with them.8 In the U.S.A., IBS patients expect a greater benefit from lifestyle modifications than from drugs, and tend to comply with doctors' advice on diet, stress reduction, and exercise.9 However, this approach raises some concern, because there are only a few studies that clearly support the benefits of lifestyle modification on IBS.
Stressful life events can induce gastrointestinal symptoms in most individuals, but those with IBS may be especially sensitive.10 Evidence suggests that IBS patients report more lifetime and daily stressful events than healthy controls.11-14 Measuring psychosocial responses to health problems poses a unique challenge for the clinician searching for empirical indicators of these abstract constructs. Visual analogue scales proved a valid and reliable solution to this challenging measurement problem15 and we used a visual analogue scale to assess stress level in our study. We found that initial stress levels among responders were lower than among nonresponders, but the extent of stress reduction did not differ between groups. We did not actively intervene with a stress reduction protocol, therefore we could not evaluate the effectiveness of stress reduction in IBS. However, we observed that lifestyle modification was more effective in persons experiencing low stress than in those who felt highly stressed. These findings indicate a potential need for psychological and pharmacologic intervention to manage IBS effectively in patients under stress.
A recent Korean study identified current smoking as a risk factor for IBS.16 Smoking also plays a role in the development of post-infectious functional gastrointestinal diseases.17 In this study, participants were not allowed to smoke for 9 weeks. Previous smoking was more prevalent among responders than nonresponders, suggesting that smoking cessation is a very effective tool in managing IBS. Although smoking was a significant factor in Logistic regression analysis, it was not in Fisher's exact test. Small sample size could have caused such differences in statistical analysis. Studies with a large scale randomized controlled trial will be needed in order to solve this question.
In more than 60% of patients, specific foods are found to aggravate IBS symptoms.18 Although the general effect of eating may contribute to symptoms, certain dietary substances, including fatty foods, beans, gas-producing foods, alcohol, and caffeine may aggravate symptoms in some individuals.6 In this study, during training the participants were supplied with a balanced diet and alcohol was forbidden. These dietary changes may have favorably affected the bowel symptoms of the participants, but we did not conduct a comparative study to confirm this. Dietary factors in IBS have not been clearly identified.
Studies involving healthy adults indicate that exercise can improve mood and symptoms of fatigue, bloating, and constipation.19 A recent randomized controlled trial showed that exercise is particularly effective in relieving constipation.20 However, these studies provide no consensus concerning the type, intensity, and duration of exercise appropriate for patients with IBS. In some patients with IBS, strenuous exercise may act on the bowel as a stressor. Typical military training is strenuous, and aggravation of bowel symptoms can be observed. In this study, male recruits performed more strenuous exercises and military training than the female group, but we found no difference between males and females in response. Our observations suggest that exercise at an appropriate level may favorably influence bowel symptoms in IBS.
First of all, this study is limited by its observational design and lack of control data. Many factors may influence the symptoms of IBS and using our protocol we could not separate the effect of each factor or identify all related factors that contributed to improvement of symptoms and QoL. Secondly, the results of our study can only be applied to young people because we included only young people as study participants. Thirdly, the observational period was short. As a result, our results do not reflect fluctuation of a patient's symptoms. Psychological factors, such as sense of relief after military training, might have influence on bowel symptoms. Also, the total observation period was a relatively short period. This could cause conflicting bias that affects the present results. Lastly, the original questionnaire was translated from English to Korean by the authors. Validity of our translation has not been tested.
Our study is significant for several reasons. First, it is the first Korean prospective study to evaluate the effects of lifestyle modification on IBS. The time and expense involved, and difficulties with compliance tend to discourage use of the prospective study design. In the context of military training, we achieved a relatively high level of compliance in lifestyle modification. Secondly, the modifications achieved in our study, including regular exercise, smoking cessation, abstinence from alcohol, and maintenance of regular habits can be easily achieved in daily life by patients without their physicians' assistance.
We conclude that lifestyle modification can favorably influence IBS symptoms and improve the QoL in patients with IBS. A prospective, randomized controlled trial is needed to confirm the findings presented here.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gwee KA, Bak YT, Ghoshal UC, et al. Asian consensus on irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1189–1205. doi: 10.1111/j.1440-1746.2010.06353.x. [DOI] [PubMed] [Google Scholar]
- 2.Spiller R, Aziz Q, Creed F, et al. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007;56:1770–1798. doi: 10.1136/gut.2007.119446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han SH, Lee OY, Bae SC, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. J Gastroenterol Hepatol. 2006;21:1687–1692. doi: 10.1111/j.1440-1746.2006.04269.x. [DOI] [PubMed] [Google Scholar]
- 4.Thompson WG, Heaton KW, Smyth GT, Smyth C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78–82. doi: 10.1136/gut.46.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drossman DA, Whitehead WE, Camilleri M. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology. 1997;112:2120–2137. doi: 10.1053/gast.1997.v112.agast972120. [DOI] [PubMed] [Google Scholar]
- 6.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 7.Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 8.Dorn SD. Systematic review: self-management support interventions for irritable bowel syndrome. Aliment Pharmacol Ther. 2010;32:513–521. doi: 10.1111/j.1365-2036.2010.04374.x. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead WE, Levy RL, Von Korff M, et al. The usual medical care for irritable bowel syndrome. Aliment Pharmacol Ther. 2004;20:1305–1315. doi: 10.1111/j.1365-2036.2004.02256.x. [DOI] [PubMed] [Google Scholar]
- 10.Drossman DA, Sandler RS, McKee DC, Lovitz AJ. Bowel patterns among subjects not seeking health care: use of a questionnaire to identify a population with bowel dysfunction. Gastroenterology. 1982;83:529–534. [PubMed] [Google Scholar]
- 11.Whitehead WE, Crowell MD, Robinson JC, Heller BR, Schuster MM. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825–830. doi: 10.1136/gut.33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker LS, Garber J, Smith CA, Van Slyke DA, Claar RL. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol. 2001;69:85–91. [PMC free article] [PubMed] [Google Scholar]
- 13.Dinan TG, O'Keane V, O'Boyle C, Chua A, Keeling PW. A comparison of the mental status, personality profiles and life events of patients with irritable bowel syndrome and peptic ulcer disease. Acta Psychiatr Scand. 1991;84:26–28. doi: 10.1111/j.1600-0447.1991.tb01416.x. [DOI] [PubMed] [Google Scholar]
- 14.Levy RL, Cain KC, Jarrett M, Heitkemper MM. The relationship between daily life stress and gastrointestinal symptoms in women with irritable bowel syndrome. J Behav Med. 1997;20:177–193. doi: 10.1023/a:1025582728271. [DOI] [PubMed] [Google Scholar]
- 15.Mottola CA. Measurement strategies: the visual analogue scale. Decubitus. 1993;6:56–58. [PubMed] [Google Scholar]
- 16.Nam SY, Kim BC, Ryu KH, Park BJ. Prevalence and risk factors of irritable bowel syndrome in healthy screenee undergoing colonoscopy and laboratory tests. J Neurogastroenterol Motil. 2010;16:47–51. doi: 10.5056/jnm.2010.16.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parry SD, Barton JR, Welfare MR. Factors associated with the development of post-infectious functional gastrointestinal diseases: does smoking play a role? Eur J Gastroenterol Hepatol. 2005;17:1071–1075. doi: 10.1097/00042737-200510000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Simrén M, Månsson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108–115. doi: 10.1159/000051878. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan SN, Wong C, Heidenheim P. Does running cause gastrointestinal symptoms? A survey of 93 randomly selected runners compared with controls. N Z Med J. 1994;107:328–331. [PubMed] [Google Scholar]
- 20.Daley AJ, Grimmett C, Roberts L, et al. The effects of exercise upon symptoms and quality of life in patients diagnosed with irritable bowel syndrome: a randomised controlled trial. Int J Sports Med. 2008;29:778–782. doi: 10.1055/s-2008-1038600. [DOI] [PubMed] [Google Scholar]