Abstract
Purpose
Ocular funduscopic examination is difficult in young children and is rarely attempted by nonophthalmologists. Our objective was to determine the feasibility of reliably obtaining high-quality nonmydriatic fundus photographs in children.
Methods
Nonmydriatic fundus photographs were obtained in both eyes of children seen in a pediatric ophthalmology clinic. Ease of fundus photography was recorded on a 10-point Likert scale (10 = very easy). Quality was graded from 1 to 5 (1, inadequate for any diagnostic purpose; 2, unable to exclude all emergent findings; 3, only able to exclude emergent findings; 4, not ideal, but still able to exclude subtle findings; and 5, ideal quality). The primary outcome measure was image quality by age.
Results
A total of 878 photographs of 212 children (median age, 6 years; range,1-18 years) were included. Photographs of at least one eye were obtained in 190 children (89.6%) and in both eyes in 181 (85.3%). Median rating for ease of photography was 7. Photographs of some clinical value (grade ≥2) were obtained in 33% of children <3 years and 95% >3 years. High-quality photographs (grade 4 or 5) were obtained in both eyes in 7% of children <3 years, 57% of children ≥3 to <7 years, 85% of children ≥7 to <9 years, and 65% of children ≥9 years. The youngest patient with high-quality photographs in both eyes was 22 months.
Conclusions
Nonmydriatic fundus photographs of adequate quality can be obtained in children over age 3 and in some children as young as 22 months.
Examination of the ocular fundus, especially the optic nerves, is often relevant to the diagnosis of various ophthalmic, neurologic, and systemic conditions1-4; however, particularly for the nonophthalmologist, it is challenging to perform ophthalmoscopy in children, especially without pupillary dilation. Even ophthalmologists may have difficulty visualizing the fundus of young, uncooperative patients with pupillary dilation and will sometimes augment their dilated fundus examination with fundus photography, especially when examination under anesthesia is not justifiable. These barriers to adequate fundus examination during routine physical examination, often coupled with a scarcity of ophthalmologists available for consultation, likely results in a high percentage of missed ocular findings that could be relevant to the urgent care of patients.5 Our goal was to evaluate the feasibility of obtaining adequate quality nonmydriatic ocular fundus photographs in children.
Methods
Between July 28, 2010, and September 16, 2010, a quality improvement project was undertaken to consider the deployment of a nonmydriatic fundus camera, approved by the Food and Drug Administration (FDA), in our pediatric ophthalmology unit. This project was deemed exempt by our institutional review board. During regular pediatric ophthalmology clinics, nondilated ocular fundus photographs were obtained on children with the commercially available, FDA-cleared, Kowa nonmydriatic alpha-D 5MP camera (Kowa α-D, Torrance, CA). The Kowa nonmydriatic alpha-D 5MP has an integrated digital camera within its unibody design, a feature we felt would discourage theft in a high-traffic clinical area. Either an ophthalmologist (DT) or a medical student (ADH), both of whom had received less than 30 minutes of training on use of the camera, obtained nondilated ocular fundus photographs centered at the optic disk and macula on children (ages 1 to 18 years). Fundus photographs were attempted on all children who were considered able to sit with correct head positioning (aided or unaided) at the ocular fundus camera.
Children either stood or were seated (alone or on an adult's lap) at the fundus camera and were instructed to position themselves at the headrest or were held into position by an adult. Children were instructed to look at the target inside the fundus camera. If the child did not understand the instructions or their vision was too poor to see the target, the child's position was altered or the photographer attempted to adjust the positioning of the camera to obtain an adequate view of the fundus, centered at the optic disk and macula. Photographers dimmed the lights and attempted to obtain at least one photograph per eye. Photographs were immediately evaluated on the liquid crystal display (LCD) monitor. If the photographs did not appear to be of adequate quality, additional photographs from each eye were attempted after the camera settings and patient positioning were readjusted.
Photographers could take as many fundus photographs as necessary to obtain an adequate view of the posterior pole of the retina. Ease of fundus photography on a 10-point Likert scale (10 = easiest) was noted for each patient session. If the photographer neglected to record a rating, then a rating of 1/10 was assigned. Length of photography session was calculated as the interval between the first and last photograph's time stamp, a feature automatically recorded by the camera. The photographs were taken to assist clinical care and were reviewed by the child's attending pediatric ophthalmologist.
Subsequently, we conducted a retrospective study of all patients who had presented to the pediatric ophthalmology clinic during the quality improvement study to evaluate factors relevant to nonmydriatic fundus photography in children. This study was approved by our institutional review board and conformed to the requirements of the United States Health Insurance Portability and Accountability Act.
Fundus photographs were reviewed by two neuro-ophthalmologists. Quality was graded from 1 to 5 (Figure 1), as previously described (1, inadequate for any diagnostic purpose; 2, unable to exclude all emergent findings; 3, only able to exclude emergent findings; 4, not ideal, but still able to exclude subtle findings; and 5, ideal quality).6 Four regions were also evaluated independently on the best photograph (based on the 1-5 ratings) taken of each eye for a given patient for 4 different regions: the optic disk area, the macula, the superior vascular arcade area, and the inferior vascular arcade area. The quality of each area was assigned a letter (A, B, C) by the following procedure. The reviewer first answered the question, “Do I see the relevant area?” If not, the quality was graded C. If yes, the reviewer responded to the follow-up question, “Is the quality sufficient to allow me to state with certainty that the relevant area is normal or abnormal?” If not, the quality was graded B. If yes, the quality was graded A. If photographs were attempted but not obtained, quality was graded 1 and C.
FIG 1.
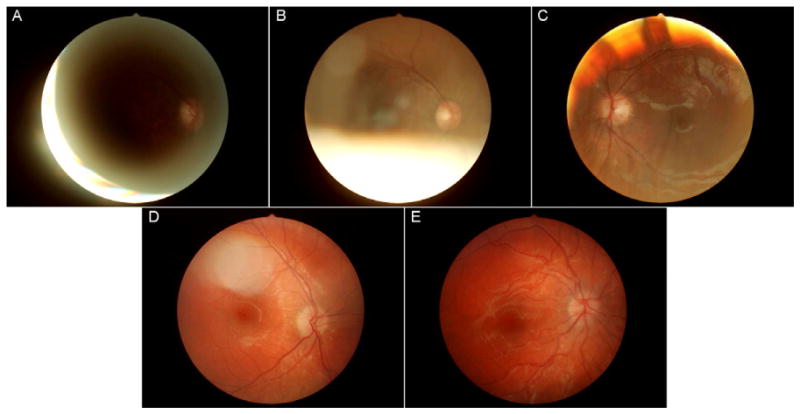
Examples of photographs from the study. A, Grade 1 photograph from a 5-year-old. B, Grade 2 photograph from a 10-year-old. C, Grade 3 photograph from a 5-year-old. D, Grade 4 photograph from a 3-year-old. E, Grade 5 photograph from a 7-year-old.
The child'a age, ocular diagnoses, and systemic clinical diagnoses were obtained by medical record review. The primary outcome measure was image quality by age. Ocular diagnoses were grouped into eight categories for analysis: normal examination, nystagmus, strabismus (defined as an intermittent or constant tropia), afferent neuroophthalmic disease, refractive error, abnormality of media, retinal abnormality, or multiple/other. Each child was assigned one primary ocular diagnosis. Systemic clinical diagnoses were grouped for analysis into categories: normal general health or not.
Statistical analysis was performed with R, a language and environment for statistical computing (R Foundation for Statistical Computing, available at http://www.R-project.org). Continuous and ordinal variables were summarized with means and medians as appropriate. Categorical variables were summarized with percentages. Tests were two-tailed, and significance was set at 5%. McNemar χ2 was used to compare the quality of the four fundus regions analyzed. One-way analysis of variance (ANOVA) of average quality for each patient by systemic and ocular diagnoses, as categorized above, were performed. Multiple testing was handled by Tukey's honest significant difference method for post hoc pairwise ANOVA comparisons or by Bonferroni correction. Interobserver agreement was calculated for each item (general quality assessment, each region quality assessment) using a weighted kappa statistic. Linear trends of proportions were assessed using the Cochran-Armitage test.
Results
A total of 878 ocular fundus photographs were obtained on 212 children (106 boys [50%]), ranging in age from 1 to 18 years (median, 6). Between 0 and 6 photographs were obtained per eye (median, 2). At least one ocular fundus photograph was obtained in 190 children (89.6%), with photographs of both ocular fundi obtained in 181 (85.3%).
Eighty-two children (39%) had strabismus, 46 (22%) had media abnormalities, 19 (9%) had afferent neuroophthalmic disease, 18 (8%) had normal examinations, 16 (7%) had refractive issues, 15 (7%) had retinal abnormalities, 10 (5%) had multiple or other abnormalities, and 6 (3%) had nystagmus. One hundred forty-five (68%) children were in good general health.
Overall, 330 children were seen in the pediatric ophthalmology clinic during the study period. Of these, 31 were younger than 12 months of age, and no photography was attempted. Thus the overall inclusion rate of children at least one year of age was 71% (212/299). Evaluated by year of age, the inclusion rate was 54% to 57% for children ≥1 but <3 years, 78% for children 3 years of age, 82% for children 4 years of age, 72% for children 5 years of age, and 67% for children age 10 and older. Of the excluded children, 70% were in good health.
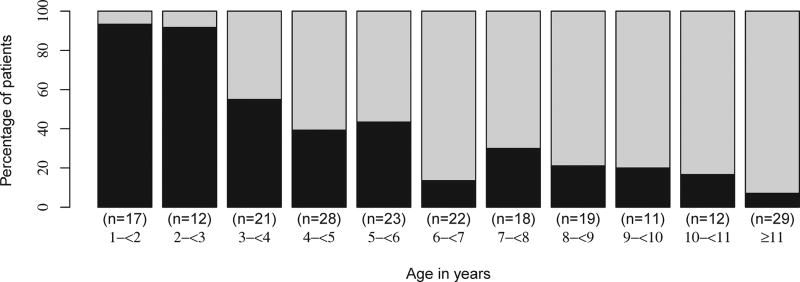
The median rating for ease of photography was 7. Three of the photography sessions that were not rated were assigned a rating of 1. Of 212 photography sessions, 28 (13.2%) were rated as 1 for ease and 23 (10.8%) were rated as 10. There was a linear relationship between the child's age and an increasing proportion of photography sessions rated as easier (P < 0.0008, Figure 2).
FIG 2.
Percentage of children with photography session rated ≥7 for ease (light gray) and ≤6 for ease (black) by age.
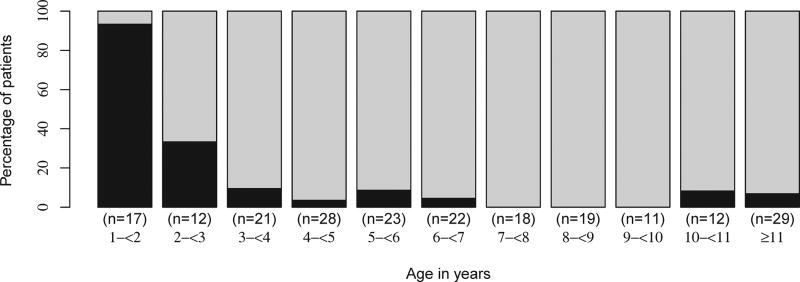
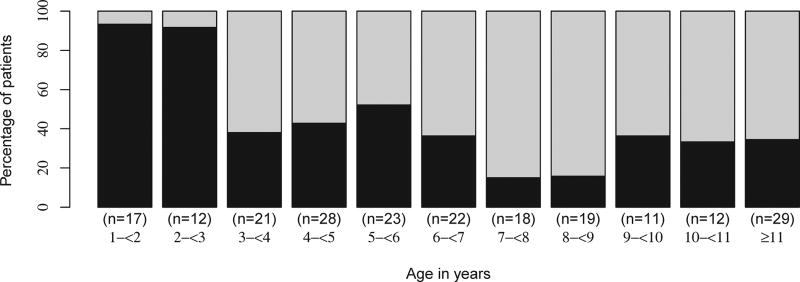
Photographs of some clinical value (grade 2 and above) were obtained in at least one eye in 9 of 27 children <3 years of age (33%) and in at least one eye in 176 of 185 children ≥3 years of age (95%) (Figure 3). Thirteen percent of children had photographs that were not gradable in either eye. The youngest patient with photographs of some clinical value was 22 months. The youngest patient with high-quality photographs in both eyes was the same 22-month-old girl. High-quality photographs (grade 4 or 5) were obtained in both eyes in 2 of 27 (7%) children <3 years of age and 121 of 185 (65%) children ≥3 years of age (54 of 94 [57%] children ≥ 3 to < 7 years old; 33 of 39 [85%] children ≥7 to <9 years old; 34 of 52 [65%] children ≥9 years old; Figure 4). The region of the optic disk was of better quality than the macula (17 better, 3 worse, 192 same; P = 0.008), but there was no difference between the disk region quality and the vascular arcade quality (P = 1.00).
FIG 3.
Percentage of children with at least one ocular fundus photograph of clinical value (quality rating of at least 2, light gray) and in whom photographs served no diagnostic purpose (quality rating of 1, black) by age. After age 3, a consistently high percentage of photographs of clinical value were obtained.
FIG 4.
Percentage of children with high quality (quality rating of 4-5, light gray) and low quality (quality rating of 1-3, black) photographs by age.
Average quality of fundus photographs was correlated with ocular diagnosis (P = 0.0001). Specifically, fundus photographs obtained in children with retinal pathology were of worse quality than those obtained in children with either normal ophthalmologic examinations or those with strabismus (greater than one quality level worse on average, P < 0.02). There was a trend toward photographs of worse quality in patients with media opacities compared with strabismus patients (P = 0.054). The general health of the child was not associated with quality of the fundus photograph (P = 0.10).
Interobserver agreement was very good for both overall quality (κ = 0.89 [0.81-0.98]) and for each of the regions evaluated on the alternative A-C scale (κ = 0.84-0.94). Interobserver agreement was best for disk quality (κ = 0.94 [0.88-1.0]) and poorest for quality of the macula (κ = 0.84 [0.76-0.92]).
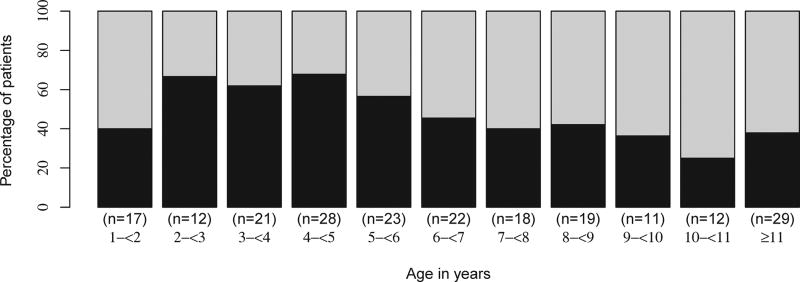
Median time to completion of fundus photographs was 1.9 minutes. There was a trend suggesting a linear relationship between increasing age and a higher proportion of shorter (<2 minute) sessions (P = 0.08) (Figure 5).
FIG 5.
Percentage of photography sessions less than or equal to 2 minutes (light gray) and greater than 2 minutes (black) by age.
Discussion
Our study found that it is feasible to obtain nonmydriatic fundus photographs of adequate quality in children >3 years of age and in children as young as 22 months. Despite multiple barriers, such as poor cooperation due to young age and ocular and systemic comorbidities, an ophthalmologist and medical student with limited training were independently able to obtain fundus photographs in over 85% of children. Among children >3 years of age, high-quality photographs were obtained in more than two-thirds of children, comparing favorably with recently published data from the Fundus photography versus Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study, in which high-quality nonmydriatic ocular fundus photographs were obtained in a similar proportion of adult patients.5
We believe that nonmydriatic ocular fundus photography could be a useful adjunct to ophthalmoscopy, a technique that is difficult to perform, and sometimes even neglected, by nonophthalmologists. 5 Indeed, in one study, most nonophthalmologist physicians surveyed felt they had inadequate training in the technique of direct ophthalmoscopy and more easily identified fundus pathology from fundus photographs than by performing direct ophthalmoscopy on adult patients.3
Ocular funduscopic examination is even more challenging in children and may be difficult even for ophthalmologists, sometimes necessitating examination under anesthesia. According to the American Academy of Pediatrics, direct ophthalmoscopy “may be possible to perform in very cooperative 3 to 4 year olds” (emphasis ours).1 Our findings suggest that nonmydriatic fundus photography may expand the age range of children who can have an evaluation of the ocular fundus areas generally visualized by direct ophthalmoscopy to almost all 3-year-olds and some cooperative 2-year-olds. Thus nonmydriatic fundus photography may represent a potential alternative to ophthalmoscopy in younger children, particularly in nonophthalmological settings.
In our study, only 13% of children had fundus photographs that were not gradable in either eye, similar to the proportion of ungradable nonmydriatic fundus photographs obtained in adult studies (6%-36%)6-9; however, most of these studies were for specific diseases, such as diabetic retinopathy, and used tailored rating scales. We used the same rating scale as the FOTO-ED study,6 which was designed to be a general-quality scale. The use of this scale may have reduced our proportion of ungradable photographs but is more relevant to our goal of improved diagnosis of ocular conditions most commonly encountered in an emergency setting rather than any disease-specific scale.
As was the case with the FOTO-ED study, we found that the quality of the photographs in the optic disk region was better than in the macular region, indicating that this technique may be more suitable for evaluation of pathology related to the optic disk compared to other ocular regions.6 Furthermore, quality of fundus photography was correlated with ocular diagnoses. For example, children with retinal pathologies or media opacities tended to have fundus photographs of worse quality than patients with strabismus. Among the children with retinal pathology, this was likely due to difficulty focusing on the target inside the camera. General health of the child, however, was not associated with fundus photograph quality, suggesting that patient capability and cooperation were relatively minor factors in obtaining quality photographs.
While this is the first study to our knowledge that has evaluated the quality of nonmydriatic fundus photography in the routine ocular funduscopic evaluation of children, two previous studies used nonmydriatic fundus photography to determine the prevalence of retinopathy among diabetic children.10,11 They showed that the overall quality of nonmydriatic fundus photographs obtained was excellent, but the children were much older than in our study (average age, 13 years in both studies).
Different imaging techniques have also been evaluated to overcome the barriers to pediatric funduscopy. One study assessed the use of the RetCam 120 (Massie Research Laboratories, Inc, Dublin, CA) in 8 children from 2 to 36 months of age who were unable to cooperate during ophthalmological examination or who required a more detailed examination.12 Although this technique allowed for a diagnosis to be made in all cases, it required immobilization of the child, an eyelid speculum, pupillary dilation, and ocular contact with the camera. Of the 8 children, 3 were at least 24 months of age and had pathologies (optic disk drusen, optic atrophy, chorioretinal scar) that potentially could have been detected with a nonmydriatic fundus camera.
Another study evaluated the use of a scanning laser ophthalmoscope (SLO) in obtaining funduscopic images in children from 9.6 weeks to 10 years of age. 13 Advantages of the handheld nonmydriatic SLO device included high tolerability, feasibility in children with poor fixation, and portability; however, there were several disadvantages, including inability to produce color images and long acquisition times (up to 15 minutes). The SLO device used was also only a prototype device that is not commercially available. Finally, the SLO device detected optic nerve head pallor poorly, suggesting that it may not be the ideal modality to image the optic nerve head.
The nonmydriatic camera used in our study also has limitations: it requires that the child sit-up, place his or her chin and forehead on a headrest, and briefly maintain fixation. Our finding that nonmydriatic photography was most feasible in children 3 years of age and older is consistent with prior studies of other tabletop ophthalmic instruments that are unsuitable for use in very young infants.15 Fundus photography in such children would likely require a handheld device, which could be held over the supine child. Adequate photography would also likely require pupillary dilation because of the typically small pupillary diameters of infants.14 Furthermore, nonmydriatic photography is best suited to image conditions affecting the posterior pole, with a 45° field-of-view that extends to just beyond the vascular arcades. Thus this technology cannot alleviate the need for dilated funduscopic examinations and examinations under anesthesia in specific ophthalmology settings.
Our study had two primary limitations. First, the acquisition of fundus photographs took place in a pediatric ophthalmology clinic setting where some children in our study were coming for follow-up visits and had previous exposure to slit-lamp examination or to automated refractors (and hence they were not naive to this type of head positioning). Second, photographs were not attempted in all children. In most cases, this was because of clinic patient flow or because the parent refused; in some cases the patient could clearly not cooperate. Uncooperativeness was primarily a concern among the youngest children (those under 3 years of age), but our overall inclusion rate was excellent (over 70% of children ≥1 year of age and similar within each year of age >3). Both factors would be expected to overestimate the speed and ease of nonmydriatic photography compared with a more general medical setting, such as a pediatric emergency department.
In conclusion, we found that nonmydriatic fundus photography is easy and time-efficient, allowing for the acquisition of fundus photographs of adequate quality in children over the age of three years and in some children as young as 22 months. This supports our previous finding5,6 that nonmydriatic ocular fundus photography may be an alternative to routine ophthalmoscopy by nonophthalmologists in selected clinical settings, including pediatric clinics.
Acknowledgments
We thank Drs. Amy Hutchinson, Scott Lambert, and Phoebe Lenhart of the Pediatric Ophthalmology Service at Emory University for their assistance.
Footnotes
Study conducted at Emory University, Atlanta, Georgia.
Literature Search: The authors searched PubMed and Google using the following search terms: nonmydriatic photography, nonmydriatic fundus photography, nonmydriatic children, and nonmydriatic camera. The search was not limited by date but was restricted to English-language articles. We also searched the reference lists of articles cited.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Committee on Practice and Ambulatory Medicine Section on Ophthalmology; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians: Organizational principles to guide and define the child health care system and/or improve the health of all children. Ophthalmology. 2003;110:860–65. doi: 10.1016/S0161-6420(03)00414-7. [DOI] [PubMed] [Google Scholar]
- 2.Morad Y, Barkana Y, Avni I, Kozer E. Fundus anomalies: What the pediatrician's eye can't see. Int J Qual Health Care. 2004;16:363–5. doi: 10.1093/intqhc/mzh065. [DOI] [PubMed] [Google Scholar]
- 3.Roberts E, Morgan R, King D, Clerkin L. Funduscopy: A forgotten art? Postgrad Med J. 1999;75:282–4. doi: 10.1136/pgmj.75.883.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breen DP, Duncan CW, Pope AE, Gray AJ, Al-Shahi Salman R. Emergency department evaluation of sudden, severe headache. QJM. 2008;101:435–43. doi: 10.1093/qjmed/hcn036. [DOI] [PubMed] [Google Scholar]
- 5.Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. New Engl J Med. 2011;364:387–9. doi: 10.1056/NEJMc1009733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruce BB, Lamirel C, Biousse V, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: The FOTO-ED Study. Acad Emerg Med. 2011;18:928–33. doi: 10.1111/j.1553-2712.2011.01147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Massin P, Erginay A, Ben Mehidi A, et al. Evaluation of a new nonmydriatic digital camera for detection of diabetic retinopathy. Diabet Med. 2003;20:635–41. doi: 10.1046/j.1464-5491.2003.01002.x. [DOI] [PubMed] [Google Scholar]
- 8.Lim JI, LaBree L, Nichols T, Cardenas I. A comparison of digital nonmydriatic fundus imaging with standard 35-millimeter slides for diabetic retinopathy. Ophthalmology. 2000;107:866–70. doi: 10.1016/s0161-6420(00)00057-9. [DOI] [PubMed] [Google Scholar]
- 9.Bursell SE, Cavallerano JD, Cavallerano AA, et al. Stereo nonmydriatic digital-video color retinal imaging compared with Early Treatment Diabetic Retinopathy Study seven standard field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology. 2001;108:572–85. doi: 10.1016/s0161-6420(00)00604-7. [DOI] [PubMed] [Google Scholar]
- 10.Massin P, Erginay A, Mercat-Caudal I, et al. Prevalence of diabetic retinopathy in children and adolescents with type-1 diabetes attending summer camps in France. Diabetes Metab. 2007;33:284–9. doi: 10.1016/j.diabet.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Stillman JK, Gole GA, Wootton R, et al. Telepaediatrics and diabetic retinopathy screening of young people with diabetes in Queensland. J Telemed Telecare. 2004;10:92–4. doi: 10.1258/1357633042614203. [DOI] [PubMed] [Google Scholar]
- 12.Hussein MA, Coats DK, Paysse EA. Use of the RetCam 120 for fundus evaluation in uncooperative children. Am J Ophthal. 2004;137:354–5. doi: 10.1016/S0002-9394(03)00867-5. [DOI] [PubMed] [Google Scholar]
- 13.Kelly JP, Weiss AH, Zhou Q, Schmode S, Dreher AW. Imaging a child's fundus without dilation using a handheld confocal scanning laser ophthalmoscope. Arch Ophthalmol. 2003;121:391–6. doi: 10.1001/archopht.121.3.391. [DOI] [PubMed] [Google Scholar]
- 14.Roarty JD, Keltner JL. Normal pupil size and anisocoria in newborn Infants. Arch Ophthalmol. 1990;108:94–5. doi: 10.1001/archopht.1990.01070030100037. [DOI] [PubMed] [Google Scholar]
- 15.Borchert M, Wang Y, Tarczy-Hornoch K, Cotter S, et al. Testability of the Retinomax autorefractor and IOLMaster in preschool children: The Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2008;115:1422–5. doi: 10.1016/j.ophtha.2007.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]