Abstract
OBJECTIVE:
In the present prospective double-blind randomized trial, the effects of intermittent paravertebral subpleural bupivacaine and morphine on pain management in patients undergoing thoracotomy were evaluated and compared with intermittent systemic analgesia.
METHODS:
Forty-five patients undergoing elective lobectomy were included in the present study. Three randomized groups consisting of 15 patients each were compared. Those in the control group were administered intravenously with tramadol 100 mg plus metamizol 1000 mg every 4 h for 3 days. We placed the catheter just below the parietal pleura along the paravertebral sulcus at the level of T5–T7. At the end of the operation and every 4 h thereafter, the patients received either 1.5 mg kg−1 bupivacaine (bupivacaine group) or 0.2 mg kg−1 morphine sulfate (morphine group) with paravertebral subpleural catheter for 3 days. Data regarding demographics, visual analog pain scores, need for supplementary intravenous analgesia, pulmonary function tests, and postoperative pulmonary complications were recorded for each patient.
RESULTS:
Visual analog pain scores (visual analog scale (VAS)) were lower in the morphine and bupivacaine groups compared with control group at all postoperative time points. The mean postoperative VAS was significantly different between the control and bupivacaine groups at postoperative hour 12, the control and morphine groups at postoperative hours 6, 12, 48, and 72, and the bupivacaine and morphine groups at postoperative hours 6 and 24 (p < 0.05). In the control group, additional analgesic requirement was significantly higher than in the bupivacaine and morphine groups (p < 0.05). Postoperative pulmonary complications occurred in three patients (20%) in the control group, in two patients (13%) in the bupivacaine group, and in one (6%) in the morphine group.
CONCLUSIONS:
The patients undergoing lung resection through a thoracotomy were observed with reduced postoperative pain and better surgical outcomes with respect to the length of hospital stay, postoperative forced expiratory volume in the first second, pulmonary complications, and need for bronchoscopic management, when paravertebral subpleural analgesia was induced by morphine.
Keywords: Paravertebral subpleural analgesia, Morphine, Bupivacaine, Tramadol
INTRODUCTION
Various strategies including epidural analgesia, intrapleural analgesia, intercostals nerve blockade, systemic opioids, and nonsteroidal anti-inflammatory drugs (NSAIDs) have been used for thoracotomy pain management. Epidural analgesia is associated with a considerable risk of epidural hematoma and respiratory depression [1]. Considerable pain relief may be achieved with systemic opioids; however, these drugs may cause respiratory depression and intestinal dysfunction [2]. NSAIDs may be associated with gastrointestinal bleeding and renal toxicity, although they are useful [3].
Intrapleural analgesia was first described by Reiestad and Stromskag [4], and previous studies evaluating intrapleural analgesia in patients undergoing a thoracotomy revealed conflicting results [3]. Unsatisfactory results may be explained by factors such as leakage of local anesthetic from chest tubes, dilution of anesthetic agent by residual fluid, binding of local anesthetic to blood proteins, and possible rapid absorption via the injured lung [5].
In this study, to eliminate the above-mentioned disadvantages of intrapleural analgesia, we placed a catheter just below the parietal pleura along the paravertebral sulcus at the level of T5–T7. In the present prospective double-blind randomized trial, the effects of intermittent paravertebral subpleural bupivacaine and morphine on pain management in patients undergoing thoracotomy were evaluated and compared with intermittent systemic analgesia.
MATERIAL AND METHOD
Forty-five patients undergoing elective lobectomy were included in this double-blind, randomized study. The study was approved by the Local Ethics Committee and written informed consent was obtained from all patients. Patients with a history of severe heart disease or hepatic or renal failure, those with American Society of Anesthesiology class IV or higher, those who underwent resection of the pleura or chest wall, those with hemorrhagic diathesis or those receiving anticoagulant therapy or acetylsalicylic acid, and those with a known allergy to local anesthetic agents were excluded from the study. The surgical approach in all patients was a posterolateral thoracotomy through the 5th intercostal space, usually extending from the midscapular to the anterior axillary line with an incision length of 12–15 cm.
Three randomized groups consisting of 15 patients each were compared. The control group received intravenous tramadol 100 mg plus metamizol 1000 mg every 4 h for 3 days. At the time of rib approximation just before the chest closure, we placed the catheter just below the parietal pleura along the paravertebral sulcus at the level of T5–T7 [6,7]. At the end of the operation and every 4 h thereafter, the patients received either 1.5 mg kg−1 bupivacaine (bupivacaine group) or 0.2 mg kg−1 morphine sulfate (morphine group) with paravertebral subpleural catheter for 3 days. The catheter was removed 72 h postoperatively. Paracetamol at a dose of 1000 mg was administered as an additional analgesic, if required, for all groups. Data regarding demographics, visual analog pain scores, pulmonary function tests, and requirements for supplementary intravenous analgesia were recorded for each patient. Patients subjectively assessed the level of pain at 1, 6, 12, 24, 48, and 72 h postoperatively on a visual analog scale (VAS) ranging from 1 (no pain) to 10 (very severe pain).
Among the pulmonary function parameters, forced expiratory volume in the first second (FEV1) was measured preoperatively and on postoperative day 3. At the time of discharge, patients were questioned in terms of the efficacy of the pain control achieved during the in-hospital postoperative period. Analgesia was defined as optimal, good, sufficient, or insufficient, according to the patient’s satisfaction. Duration of the surgical intervention and of in-hospital stay was recorded in all patients. Postoperative complications and the eventual need for postoperative bronchoscopic aspirations were also recorded.
Statistical analysis was performed using the SPSS 15.0 for windows (SPSS Inc., Chicago, IL, USA). Shapiro–Wilk test was performed to check the normality of the data. For the normally distributed data, one-way analysis of variance (ANOVA) was used to compare the groups. If there was a significant difference between the groups, Tukey’s and Tamhane tests were used for the pairwise comparison of the groups according to the homogeneity of variances. ANOVA for repeated measures was used to compare the groups with normally distributed data. All quantitative data were expressed as mean ± standard deviation. A p-value < 0.05 was considered statistically significant.
RESULTS
Forty-five patients fulfilled the study criteria and were included in the trial. All patients underwent lobectomy for lung cancer or for benign disease. None of the patients enrolled in this study either underwent middle lobectomy or had bullous emphysema. There were no significant differences between the groups with respect to the resection types (upper or lower lobe). Pathological diagnosis presented in Table 1 shows comparable distribution between benign and malignant diseases in the three groups. There were no significant differences between the groups with respect to age, gender, preoperative pulmonary function, number of tube thoracostomy, and duration of the surgical procedure (Table 2).
Table 1:
Pathological diagnosis of the study groups
| Diagnosis | Control group (n) |
Bupivacaine group (n) |
Morphine group (n) |
|---|---|---|---|
| Adenocarcinoma | 4 | 1 | 3 |
| Squamous carcinoma | 5 | 7 | 8 |
| Large cell carcinoma | 1 | 0 | 1 |
| Bronchiectasis | 3 | 4 | 2 |
| Hydatid cyst | 1 | 1 | 0 |
| Metastasis | 1 | 2 | 1 |
Table 2:
Characteristics and surgical data of the study groups
| Variable | Control group | Bupivacaine group | Morphine group | P |
|---|---|---|---|---|
| Gender (male/female) | 9/6 | 8/7 | 10/5 | 0.77 |
| Age (years) | 51.86 ± 11.5 | 49.13 ±13.37 | 54.4 ±12.64 | 0.52 |
| Preoperative FEV1 (% predicted) | 65.6 ± 9.55 | 64.33 ± 9.98 | 64.33 ± 8.94 | 0.91 |
| Number of tube thoracostomy | 1.66 ± 0.48 | 1.73 ± 0.45 | 1.6 ± 0.5 | 0.75 |
| Duration of the surgical procedure | 156 ± 28.23 | 154 ± 27.46 | 152 ± 26.51 | 0.92 |
FEV1: Forced expiratory volume in the first second.
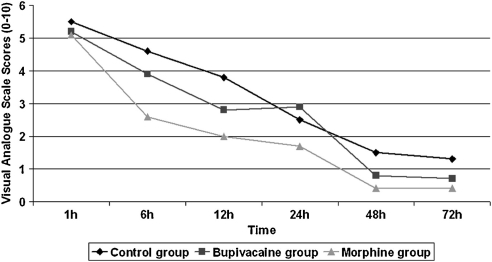
Visual analog pain scores were lower in the morphine and bupivacaine groups compared with the control group at all postoperative time points. The mean postoperative pain measured by VAS were as follows: 5.53 ± 0.99 at hour 1, 4.6 ± 0.91 at hour 6, 3.8 ± 1.01 at hour 12, 2.53 ± 1.18 at hour 24, 1.53 ± 0.99 at hour 48, and 1.33 ± 1.04 at hour 72 in the control group; 5.26 ± 1.53 at hour 1, 3.93 ± 1 .33 at hour 6, 2.8 ± 1.32 at hour 12, 2.93 ± 0.7 at hour 24, 0.86 ± 1.24 at hour 48, and 0.73 ± 0.93 at hour 72 in the bupivacaine group; and 5.13 ± 0.83 at hour 1, 2.66 ± 0.72 at hour 6, 2 ± 0.84 at hour 12, 1.73 ± 1.03 at hour 24, 0.4 ± 0.5 at hour 48, and 0.4 ± 0.5 at hour 72 in the morphine group. The mean postoperative pain score was significantly different between the control and bupivacaine groups at postoperative hour 12. There were also significant differences between the control and morphine groups in terms of postoperative pain scores at the postoperative 6, 12, 48, and 72 h. Additionally, a significant difference was determined between the bupivacaine and morphine groups in terms of pain score at postoperative 6 and 24 h (p < 0.05, Fig. 1).
Figure 1:
The median values of visual analog scale scores of each group at the postoperative 1st, 6th, 12th, 24th, 48th, and 72nd hours. The graph shows median values.
Supplementary analgesia was required during the first 3 postoperative days in seven patients (46%) in the control group, four patients (26%) in the bupivacaine group, and four (26%) in the morphine group. The mean amount of supplemental analgesic consumption (paracetamol clorhydrate, 1000 g, infusion solution) at 72 h postoperatively was 900 mg for patients in the control group, 333 mg for patients in the bupivacaine group, and 200 mg for those in the morphine group. There were significant differences between the control and morphine groups (p < 0.05). There were no significant differences between the control and bupivacaine groups (p = 0.10) and the bupivacaine and morphine groups (p = 0.87). The level of patient’s satisfaction regarding the efficacy of postoperative pain control is reported for the three groups in Table 3. The rate of patients subjectively reporting an optimal or good efficacy of analgesia in the morphine group was 73% (11/15 patients); this rate was significantly higher compared with the that of the control group (26%; 4/15 patients, p < 0.05).
Table 3:
Postthoracotomy analgesia-patient’s satisfaction
| Control group (n) |
Bupivacaine group (n) |
Morphine group (n) |
|
|---|---|---|---|
| Optimal or good | 4 | 5 | 11 |
| Sufficient | 6 | 9 | 2 |
| Insufficient | 5 | 1 | 2 |
The mean postoperative length of hospital stay was 8.13 ± 2.26 days in the control group, 7.66 ± 2.16 days in the bupivacaine group, and 6.53 ± 1.72 days in the morphine group. No significant difference was noted between the groups with respect to length of hospital stay (p = 0.10). The mean postoperative FEV1 values were 48.6 ± 6.59, 52.46 ± 8.46, and 54.86 ± 7.33 in percentages for the control, bupivacaine, and morphine groups, respectively. Although there were no significant differences between the control and bupivacaine groups (p = 0.32) and the bupivacaine and morphine groups (p = 0.36), there were significant differences between control and morphine groups (p < 0.05).
Postoperative pulmonary complications occurred in three patients (20%) in the control group, in two patients (13%) in the bupivacaine group, and in one (6%) in the morphine group. Data regarding the postoperative pulmonary complications and the need for bronchoscopic aspiration are presented in detail in Table 4. All of the three patients with atelectasis completely recovered through respiratory rehabilitation and bronchoscopic aspiration. The patient with pneumonia in the bupivacaine group was also treated without any sequela by an effective antibiotic management. Mortality was observed due to respiratory failure in one patient (6%) in the bupivacaine group. Bronchoscopic aspiration was performed because of pulmonary atelectasis or sputum retention in five patients (33%) in the control group and in two patients (13%) in the bupivacaine group. Nausea was observed in three patients receiving tramadol. Nausea and vomiting are well-known side effects of tramadol; thus, antiemetic prophylaxis was administered before tramadol treatment. Patients who were administered subpleural morphine did not experience nausea. In the morphine group, two patients developed transient pruritus without any need for treatment. No catheter-related complications were noted.
Table 4:
Postoperative pulmonary complications
| Complication | Control group (n) |
Bupivacaine group (n) |
Morphine group (n) |
|---|---|---|---|
| Atelectasis | 2 | 1 | – |
| Pneumonia | – | 1 | – |
| Air leak | – | – | 1 |
| Respiratory failure | 1 | – | – |
| Need for bronchoscopic aspiration | 5 | 2 | – |
DISCUSSION
Postoperative pain after thoracic surgery remains a challenging clinical problem that may be associated with increased morbidity and mortality. Previous studies have found that ineffective pain management may lead to serious pulmonary complications because of insufficient clearance of secretions, mucous plugging, and atelectasis [2,8,9]. The results of the present study suggested that the analgesic effect of paravertebral subpleural morphine was superior to the analgesic effects of paravertebral subpleural bupivacaine and intravenously administered tramadol + metamizol in the postoperative pain management after thoracic surgery. Thus, we consider that morphine can be recommended in preference to subpleural paravertebral bupivacaine and intravenously administered tramadol + metamizol for pain relief after thoracotomy
One of the most effective ways to both prevent respiratory complications and achieve a rapid functional recovery after lung surgery is adequate pain control in the early postthoracotomy period [3,10]. Thus, we focused our analysis on the evaluation of pain scores in the first 3 postoperative days and on the comparison of complications, postoperative FEV 1, length of hospitalization, and need for bronchoscopic management, all of which are indicators of the quality of postoperative outcome.
Various treatment modalities have been introduced for the management of postthoracotomy pain. Many strategies to control this pain have been attempted, but when the origin of the pain is considered, regional anesthesia is the most logical approach. Intercostal nerve blockade has recently come into practice as an alternative technique for the management of postthoracotomy pain. However, this technique was reported to have some disadvantages associated with serial injections and long-term intercostal neuralgia, causing discomfort to patients [11]. Another alternative that has been introduced recently, with very promising results, is the method of diffuse intrapleural analgesia performed by the infusion of a local anesthetic through a catheter positioned inside the pleural cavity [3]. The mechanism of action seems to be diffusion across the parietal pleura [12]. Some previous studies have shown limited or no improvement in analgesia with this technique [13–16].
In the present study, to eliminate the factors that limit the efficacy of intrapleural analgesia, intermittent intercostal nerve blockade was performed at the level of T5–T7 via a cannula inserted into the tunnel created just below parietal pleura along the paravertebral sulcus. In the systemic review consisting of nine studies, Detterbeck [17] reported that continuous intercostal nerve blockade following thoracotomy with an extrapleural catheter results in a reasonably consistent better pain relief and preservation of pulmonary function as compared with systemic narcotics, and appears to be at least as good as an epidural approach.
In the present study, intermittent paravertebral subpleural morphine also resulted in reduced pain and improved pulmonary function in the early postoperative period. Only four patients from each of the morphine and bupivacaine groups needed supplemental analgesic medication, whereas in the control group seven patients required supplemental analgesic medication. The mean amount of supplemental analgesic consumption at 72 h postoperatively was lowest for patients in the morphine group. The pain relief in the morphine group was observed to result in better outcomes, including higher postoperative FEV1, fewer pulmonary complications, lesser need for bronchoscopic management, and shorter length of hospital stay.
In conclusion, we observed that patients undergoing lung resection through a thoracotomy showed reduced postoperative pain and better surgical outcomes with respect to length of hospital stay, postoperative FEV1, pulmonary complications, and need for bronchoscopic management, when paravertebral subpleural analgesia was induced by morphine. Because of its associated safety and efficacy, paravertebral subpleural morphine administration may be a suitable alternative to intermittent systemic opioids for analgesia after thoracotomy.
ACKNOWLEDGEMENT
The authors thank Yüksel Terzi, MD (Department of Statistics, School of Art and Science, 19 Mayis University, Samsun) for his assistance.
Conflict of interest: none declared.
REFERENCES
- 1.Chaney MA, Labovsky JK. Thoracic epidural anesthesia and cardiac surgery: balancing postoperative risks associated with hematoma formation and thromboembolic phenomenon. J Cardiothorac Vasc Anesth. 2005;19:768–71. doi: 10.1053/j.jvca.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 2.Takamori S, Yoshida S, Hayashi A, Matsuo T, Mitsuoka M, Shirouzu K. Intraoperative intercostal nerve blockade for postthoracotomy pain. Ann Thorac Surg. 2002;74:338–41. doi: 10.1016/s0003-4975(02)03710-4. [DOI] [PubMed] [Google Scholar]
- 3.Soto RG, Fu ES. Acute pain management for patients undergoing thoracotomy. Ann Thorac Surg. 2003;75:1349–57. doi: 10.1016/s0003-4975(02)04647-7. [DOI] [PubMed] [Google Scholar]
- 4.Reiestad F, Stromskag KE. Intrapleural catheter in the management of postoperative pain: a preliminary report. Reg Anaesth. 1986;11:89–91. [Google Scholar]
- 5.Ogus H, Selimoglu O, Basaran M, Ozcelebi C, Ugurlucan M, Sayin OA, Kafali E, Ogus TN. Effects of intrapleural analgesia on pulmonary function and postoperative pain in patients with chronic obstructive pulmonary disease undergoing coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2007;21:816–9. doi: 10.1053/j.jvca.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Cucu O, Karaca P, Enc Y, Yucel O, Aksoy T, Senay S, Canik S. Comparison of thoracic paravertebral and epidural blocks for pain relief after thoracotomy. 2006;14:42–7. [Google Scholar]
- 7.Hadzic A, Vloka JD. Thoracic paravertebral block. In: Hadzic A, Vloka JD, editors. Peripheral nerve blocks. Principles and practice. 1st ed. Columbus: Mc Graw Hill; 2004. pp. 194–207. [Google Scholar]
- 8.Kaiser AM, Zollinger A, De Lorenzi D, Largiader F, Weder W. Prospective, randomized comparison of extrapleural versus epidural analgesia for postthoracotomy pain. Ann Thorac Surg. 1998;66:367–72. doi: 10.1016/s0003-4975(98)00448-2. [DOI] [PubMed] [Google Scholar]
- 9.Ballantyne JC, Carr DB, deFerranti S, Suarez T, Lau J, Chalmers TC, Angelillo IF, Mosteller F. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86:598–612. doi: 10.1097/00000539-199803000-00032. [DOI] [PubMed] [Google Scholar]
- 10.Slinger P. New trends in anaesthesia for thoracic surgery including thoracoscopy. Can J Anaesth. 1995;42:77–84. [Google Scholar]
- 11.Tetik O, Islamoglu F, Ayan E, Duran M, Buket S, Cekirdekci A. Intermittent infusion of 0.25% bupivacaine through an intrapleural catheter for post-thoracotomy pain relief. Ann Thorac Surg. 2004;77:284–8. doi: 10.1016/s0003-4975(03)01338-9. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie AG, Mathe S. Interpleural local anesthesia: anatomical basis for mechanisms of action. Br J Anaesth. 1996;76:297–9. doi: 10.1093/bja/76.2.297. [DOI] [PubMed] [Google Scholar]
- 13.Silomon M, Claus T, Huwer H, Biedler A, Larsen R, Molter G. Interpleural analgesia does not influence post-thoracotomy pain. Anesth Analg. 2000;91:44–50. doi: 10.1097/00000539-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Scheinin B, Lindgren L, Rosenberg PH. Treatment of postthoracotomy pain with intermittent instillations of intrapleural bupivacaine. Acta Anaesthesiol Scand. 1989;33:156–9. doi: 10.1111/j.1399-6576.1989.tb02880.x. [DOI] [PubMed] [Google Scholar]
- 15.Schneider RF, Villamena PC, Harvey J, Surick BG, Surick IW, Beattie EJ. Lack of efficacy of intrapleural bupivacaine for postoperative analgesia following thoracotomy. Chest. 1993;103:414–6. doi: 10.1378/chest.103.2.414. [DOI] [PubMed] [Google Scholar]
- 16.Kambam JR, Hammon J, Parris WC, Lupinetti FM. Intrapleural analgesia for post-thoracotomy pain and blood levels of bupivacaine following intrapleural injection. Can J Anaesth. 1989;36:106–9. doi: 10.1007/BF03011428. [DOI] [PubMed] [Google Scholar]
- 17.Detterbeck FC. Efficacy of methods of intercostals nerve blockade for pain relief after thoracotomy. Ann Thorac Surg. 2005;80:1550–9. doi: 10.1016/j.athoracsur.2004.11.051. [DOI] [PubMed] [Google Scholar]