Abstract
OBJECTIVE
Although there have been several studies that compared the efficacy of percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), the impact of off-pump CABG (OPCAB) has not been well elucidated. The objective of the present study was to compare the outcomes after PCI, on-pump CABG (ONCAB), and OPCAB in patients with multivessel and/or left main disease.
METHODS
Among the 9877 patients undergoing first PCI using bare-metal stents or CABG who were enrolled in the CREDO-Kyoto Registry, 6327 patients with multivessel and/or left main disease were enrolled into the present study (67.9 ± 9.8 years old). Among them, 3877 patients received PCI, 1388 ONCAB, and 1069 OPCAB. Median follow-up was 3.5 years.
RESULTS
Comparing PCI with all CABG (ONCAB and OPCAB), propensity-score-adjusted all-cause mortality after PCI was higher than that CABG (hazard ratio (95% confidence interval): 1.37 (1.15–1.63), p < 0.01). The incidence of stroke was lower after PCI than that after CABG (0.75 (0.59–0.96), p = 0.02). CABG was associated with better survival outcomes than PCI in the elderly (interaction p = 0.04). Comparing OPCAB with PCI or ONCAB, propensity-score-adjusted all-cause mortality after PCI was higher than that after OPCAB (1.50 (1.20–1.86), p < 0.01). Adjusted mortality was similar between ONCAB and OPCAB (1.18 (0.93–1.51), p = 0.33). The incidence of stroke after OPCAB was similar to that after PCI (0.98 (0.71–1.34), p > 0.99), but incidence of stroke after ONCAB was higher than that after OPCAB (1.59 (1.16–2.18), p < 0.01).
CONCLUSIONS
In patients with multivessel and/or left main disease, CABG, particularly OPCAB, is associated with better survival outcomes than PCI using bare-metal stents. Survival outcomes are similar between ONCAB and OPCAB.
Keywords: Coronary artery bypass grafting, Percutaneous coronary intervention, Off-pump
INTRODUCTION
Several randomized controlled trials (RCTs) and meta-analyses comparing percutaneous coronary interventions (PCIs) with coronary artery bypass grafting (CABG) demonstrated similar long-term survival outcomes for PCI and CABG [1–4]. However, these studies may not accurately reflect current clinical practice of coronary revascularization for following reasons. First, these studies had limitations that mitigated against the prognostic and symptomatic benefits of CABG in many patients with left main disease and/or more complex disease in ‘real-world’ clinical practice [5,6]. Second, technical development of CABG has not been well reflected in those studies. CABG was primarily performed with the use of cardiopulmonary bypass (on-pump CABG (ONCAB)). In the mid-1990s, CABG without cardiopulmonary bypass (off-pump CABG (OPCAB)) has been introduced to reduce postoperative complications such as stroke which are associated with the use of cardiopulmonary bypass [7,8]. Thus, it is important to investigate the impact of OPCAB in patients with more complex coronary lesions.
The Coronary REvascularization Demonstrating Outcome Study in Kyoto (CREDO-Kyoto) is a multicenter registry in Japan enrolling consecutive 9877 patients undergoing first PCI or CABG and excluding those patients with acute myocardial infarction within a week before index procedure [9]. We reported that adjusted survival outcomes tended to be better after CABG than those after PCI in patients with multivessel disease without left main disease (hazard ratio (HR), 95% confidence interval (CI): 1.23 (0.99–1.53), p = 0.06 for PCI vs CABG). However, we did not evaluate the impact of OPCAB on outcomes. Thus, the purpose of the present study was to compare the outcomes of PCI, ONCAB, or OPCAB using the data from the CREDO-Kyoto Registry by propensity score model. To reflect the real world of coronary revascularization in the analysis, we included patients with multivessel and/or left main disease.
PATIENTS AND METHODS
Study population
The CREDO-Kyoto is a multicenter registry in Japan enrolling consecutive patients undergoing first PCI or CABG and excluding those patients with acute myocardial infarction within a week before index procedure. This study was approved by the institutional review boards or ethics committees of all participating institutions. As the study subjects were retrospectively enrolled, written informed consent was not obtained, in concordance with the guidelines for epidemiologic studies issued by the Ministry of Health, Labor and Welfare of Japan. However, 73 patients were excluded because of their refusal to participate in the study when contacted for the follow-up [9].
Between January 2000 and December 2002, 9877 patients were identified to have undergone either CABG (2999 patients) or PCI (6878 patients) without prior history of coronary revascularization. Among them, patients with multivessel and/or left main coronary artery disease were included in the present study. Four hundred eighty-four patients undergoing concomitant valvular, left ventricular, or major vascular operation were excluded from the current analysis. Patients with single-vessel disease without left main disease (PCI: 3001 patients and CABG: 65 patients) were also excluded. Therefore, the study group comprised 6327 patients with multivessel and/or left main coronary artery disease undergoing first coronary revascularization (PCI: 3877 patients and CABG: 2450 patients).
Data collection and definitions
Demographic, angiographic, and procedural data were collected from hospital charts or databases in each center by independent clinical research coordinators according to prespecified definitions. Follow-up data were obtained from hospital charts or by contacting patients or referring physicians. If sufficient follow-up data are unavailable, the investigators contact patients by telephone or letter. If the patient died at the time of contact, the investigators try to obtain data from the family regarding death including non-fatal events before the time of death as great an extent as possible.
Baseline clinical characteristics, such as myocardial infarction, heart failure, diabetes, hypertension, current smoker status, atrial fibrillation, chronic obstructive lung disease, and malignancy, were regarded as present when these diagnoses were recorded in the hospital charts. Left ventricular ejection fraction (LVEF) was measured either by contrast left ventriculography or by echocardiography. Chronic kidney disease was regarded as present when creatinine clearance estimated by Cockcroft–Gault formula was less than 60 ml min−1. Anemia was defined as blood hemoglobin level <12 g dl−1 as previously described [9].
Endpoints
An independent clinical events committee adjudicated events. Death was regarded as cardiovascular in origin unless obvious noncardiovascular causes could be identified. Any death during the index hospitalization was regarded as cardiovascular death. Myocardial infarction was adjudicated according to the definition in the Arterial Revascularization Therapy Study [1]. Within 1 week of the index procedure, only Q-wave myocardial infarction was adjudicated as myocardial infarction. Stroke was defined as any new permanent global or focal neurologic deficit that could not be attributed to other neurologic or medical processes. In the majority of patients, strokes were diagnosed by neurologists and confirmed by computed tomography or magnetic resonance imaging head scans. Stroke at follow-up was defined as symptomatic stroke.
Primary endpoint was death from any cause. Secondary endpoints were cardiovascular death, stroke, myocardial infarction, composite cardiovascular event (cardiovascular death, stoke, or myocardial infarction), and need for any revascularization procedures (PCI or CABG) during the follow-up period.
Statistical analyses
All continuous variables are expressed as the mean ± standard deviation. Differences in baseline characteristics across the three groups were examined by analysis of variance of χ2-test.
Propensity scores, which were the probabilities that a patient would undergo PCI or probability that a patient would undergo OPCAB, were calculated for each patient. The propensity scores were estimated with multivariable logistic regression analyses separately. Confounding factors in the logistic regression included age, gender, body mass index, emergency procedure, prior myocardial infarction, congestive heart failure, stroke, peripheral arterial disease, atrial fibrillation, chronic obstructive pulmonary disease, malignancy, hypertension, diabetes, hemodialysis, chronic kidney disease, anemia, current smoker status, LVEF, total occlusion, proximal left anterior descending artery (LAD) disease, triple-vessel disease, and left main disease.
Outcomes after PCI, ONCAB, or OPCAB are compared by the Cox proportional hazard models stratified by the quartiles of propensity scores. Propensity-score-adjusted HRs, 95% CIs, and p values are reported. The p values for multiple comparisons, namely PCI versus OPCAB and ONCAB versus OPCAB, were adjusted by the Bonferroni correction, that is, we multiplied the original p values by 2. All reported p values were two sided. Subgroup analysis was also conducted with regard to five prespecified risk factors, including triple-vessel disease, diabetes, left ventricular dysfunction, proximal LAD disease, and the elderly [9], and p values for the interaction term were reported additionally.
All reported p values were two sided. All analyses were conducted by a statistician with the use of SAS software version 9.2 (SAS Institute Inc. North Carolina, USA) and S-Plus version 7.0 (Insightful Corp. Seattle, USA). The authors had full access to the data and take responsibility for their integrity. All authors have read and agreed to the manuscript as written.
RESULTS
Baseline characteristics
Among the 6327 patients with multivessel and/or left main disease, 3877 patients (61%) received PCI, 1381 ONCAB (22%), and 1069 OPCAB (17%). Baseline characteristics of the patients in the three groups are shown in Table 1. ONCAB and OPCAB groups generally included more high-risk patients, such as those with left ventricular dysfunction, heart failure, prior myocardial infarction, chronic kidney disease, history of stroke, and anemia. Patient with diabetes was more common in ONCAB and OPCAB. Regarding the complexity of coronary artery anatomy, ONCAB and OPCAB groups included more complex patients, such as those with triple-vessel disease, left main disease, involvement of proximal LAD, and total occlusion. In the PCI group, bare-metal stents were used in 85% of patients. None of the patients received drug-eluting stents. Medications such as statins, thienopyridines, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta blockers, and nitrates were more frequently used in the PCI group than in the CABG group. Types of bypass grafts are shown in Table 2. OPCAB was performed using more arterial grafts than ONCAB.
Table 2:
CABG data
| ONCAB (n = 1381) |
OPCAB (n = 1069) |
p value | |||
|---|---|---|---|---|---|
| No. of anastomotic sites | 3.3 ± 1.0 | 3.2 ± 1.2 | <0.01 | ||
| Type of bypass grafts | |||||
| Left internal thoracic artery | 1263 | 91% | 1000 | 94% | 0.05 |
| Right internal thoracic artery | 185 | 13% | 577 | 54% | <0.01 |
| Right gastroepiploic artery | 279 | 20% | 371 | 35% | <0.01 |
| Radial artery | 550 | 40% | 253 | 24% | <0.01 |
| Saphenous vein | 1035 | 75% | 462 | 43% | <0.01 |
| Total arterial revascularization | 346 | 25% | 607 | 57% | <0.01 |
Mean ± standard deviation, or number of patients and percentage.
Table 1:
Baseline characteristics
| PCI (n = 3877) | ONCAB (n = 1381) | OPCAB (n = 1069) | p value* | ||||
|---|---|---|---|---|---|---|---|
| Age | 68.3 ± 10.0 | 66.3 ± 9.3 | 68.6 ± 9.4 | <0.01 | |||
| Male gender | 2704 | 70% | 1000 | 72% | 757 | 71% | 0.17 |
| Body mass index | 23.7 ± 3.3 | 23.5 ± 3.2 | 23.6 ± 3.2 | 0.02 | |||
| No. of diseased vessels | 2.36 ± 0.53 | 2.58 ± 0.73 | 2.55 ± 0.74 | <0.01 | |||
| Two-vessel disease | 2351 | 61% | 305 | 22% | 271 | 25% | <0.01 |
| Triple-vessel disease | 1461 | 38% | 958 | 69% | 707 | 66% | <0.01 |
| Left main disease | 165 | 4% | 410 | 30% | 332 | 31% | <0.01 |
| Proximal LAD disease | 1545 | 40% | 791 | 57% | 639 | 60% | <0.01 |
| Total occlusion | 1301 | 34% | 672 | 49% | 457 | 43% | <0.01 |
| Emergency procedure | 191 | 5% | 77 | 6% | 75 | 7% | 0.03 |
| Ejection fraction (%) | 62.1 ± 13.6 | 58.6 ± 15.0 | 61.2 ± 13.7 | <0.01 | |||
| Prior myocardial infarction | 1006 | 26% | 489 | 35% | 342 | 32% | <0.01 |
| Heart failure | 569 | 15% | 316 | 23% | 303 | 28% | <0.01 |
| Atrial fibrillation | 254 | 7% | 80 | 6% | 60 | 6% | 0.40 |
| History of stroke | 607 | 16% | 237 | 17% | 289 | 27% | <0.01 |
| Peripheral artery disease | 367 | 9% | 239 | 17% | 243 | 23% | <0.01 |
| Chronic pulmonary disease | 83 | 2% | 30 | 2% | 22 | 2% | 0.98 |
| Current smoker | 1056 | 27% | 355 | 26% | 250 | 23% | 0.04 |
| Malignancy | 321 | 8% | 80 | 6% | 79 | 7% | 0.01 |
| Diabetes | 1651 | 43% | 642 | 46% | 499 | 47% | 0.01 |
| Hypertension | 2810 | 72% | 918 | 66% | 805 | 75% | <0.01 |
| Hyperlipidemia | 1955 | 50% | 710 | 51% | 609 | 57% | 0.00 |
| Chronic kidney disease | 1411 | 36% | 532 | 39% | 426 | 40% | 0.08 |
| Hemodialysis | 167 | 4% | 69 | 5% | 54 | 5% | 0.42 |
| Hemoglobin (g dr1) | 13.1 ± 2.0 | 12.7 ± 2.0 | 12.6 ± 2.0 | <0.01 | |||
| Medications at discharge | |||||||
| Statins | 1287 | 33% | 207 | 15% | 289 | 27% | <0.01 |
| Aspirin | 3441 | 89% | 1080 | 78% | 957 | 90% | <0.01 |
| Thienopyridines | 2964 | 76% | 87 | 6% | 197 | 18% | <0.01 |
| ACE inhibitor | 1025 | 26% | 135 | 10% | 136 | 13% | <0.01 |
| ARB | 599 | 15% | 102 | 7% | 153 | 14% | <0.01 |
| β antagonist | 847 | 22% | 123 | 9% | 117 | 11% | <0.01 |
| Calcium antagonist | 2320 | 60% | 801 | 58% | 682 | 64% | 0.02 |
| Nitrates | 2805 | 72% | 677 | 49% | 457 | 43% | <0.01 |
Mean ± standard deviation, or number of patients and percentage. LAD: left anterior descending artery; ACE: angiotensin converting enzyme inhibitors; ARB: angiotensin receptor blockers.
p value is for comparison among PCI, ON- and OPCAB by analysis of variance or x2 test.
PCI versus CABG
Clinical follow-up were completed in 98% at 1 year and 95% at 2 years. The median follow-up period was 1314 days in the PCI group (interquartile range, 979–1649) and 1267 days in the CABG group (interquartile range, 950–1584).
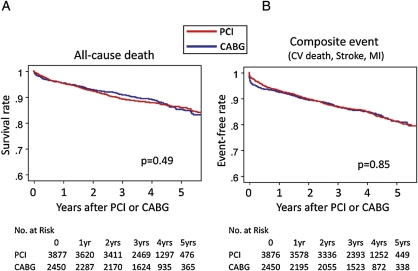
Propensity score analysis showed that all-cause mortality adjusted for confounders was higher after PCI than that after CABG (HR (95% CI): 1.37 (1.15–1.63), p < 0.01, Table 3). This finding was similar when patients were stratified to propensity score and institutes (1.30 (1.06–1.61), p = 0.01). The incidences after PCI were higher than those after CABG in the adjusted analysis regarding cardiovascular death (1.39 (1.12–1.73), p < 0.01) and myocardial infarction (1.82 (1.34–2.47), p < 0.01). However, the incidence of stroke was lower after PCI (0.75 (0.59–0.96), p = 0.02). The incidence of composite cardiovascular event was higher after PCI (1.19 (1.02–1.39), p = 0.03). The incidence of repeated revascularization was far higher after PCI (6.72 (5.84–7.73), p < 0.01). Kaplan–Meier survival curve and event-free curve for composite cardiovascular event are presented in Fig. 1A and B.
Table 3:
Hazard ratios for outcomes after PCI compared with that after CABG adjusted by propensity score stratification
| Number of events |
HR | 95% CI | p value | ||
|---|---|---|---|---|---|
| PCI (n = 3877) | CABG (n = 2450) | ||||
| All-cause death | 454 | 279 | 1.37 | 1.15–1.63 | <0.01 |
| Cardiovascular death | 282 | 186 | 1.39 | 1.12–1.73 | <0.01 |
| Stroke | 192 | 171 | 0.75 | 0.59–0.96 | 0.02 |
| Myocardial infarction | 188 | 83 | 1.82 | 1.34–2.47 | <0.01 |
| Composite eventa | 564 | 369 | 1.19 | 1.02–1.39 | 0.03 |
| Any revascularization | 1873 | 277 | 6.72 | 5.84–7.73 | <0.01 |
a Composite event: cardiovascular death, stroke, or myocardial infarction e.g. all-cause mortality after PCI was 1.37 times higher than that after CABG (p < 0.01), whereas stroke rate after PCI was 0.75 times lower than CABG (p = 0.02).
Figure 1:
Kaplan–Meier curves for each endpoint comparing PCI with CABG. CV: cardiovascular; MI: myocardial infarction.
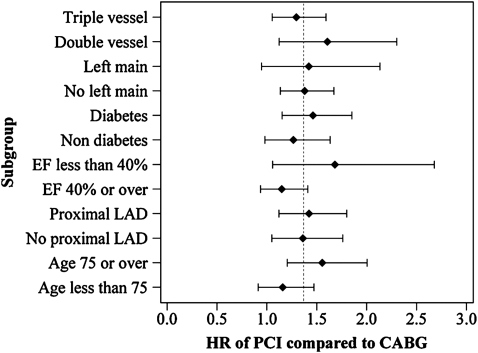
A forest plot in Fig. 2 presents subset analysis for all-cause death after adjusted for propensity score. Interaction p value indicated that CABG was associated with better survival outcomes than PCI particularly in patients with the age of ≥75 (interaction p = 0.04) and possibly in patients with LVEF of <40% (p = 0.09).
Figure 2:
Forest plot of propensity-score-adjusted hazard ratios for death after PCI as compared with that after CABG in subgroups. Dashed line indicates hazard ratio in all patients of 1.37. Interaction tests, which are design to detect whether the specific factor modifies the effect of PCI relative to CABG, were significant for age (p = 0.04) and borderline for ejection fraction (p = 0.09). These indicate that CABG is associated with better survival outcomes than PCI particularly in patients with the age of ≥75 and possibly in patients with LVEF of <40%.The other interaction tests were not significant.
OPCAB versus PCI or ONCAB
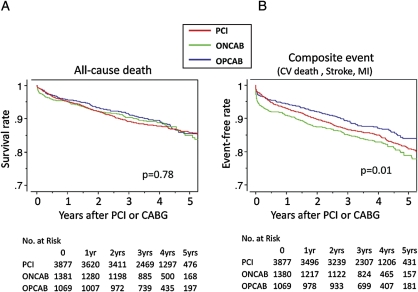
Propensity score analysis showed that all-cause mortality after PCI was higher than that after OPCAB (1.50 (1.20–1.86), p < 0.01; Table 4), but similar between ONCAB and OPCAB (1.18 (0.93–1.51), p = 0.33). Cardiovascular mortality after PCI and ONCAB was higher than that after OPCAB (1.74 (1.32–2.31), p < 0.01 and 1.49 (1.11–2.02), p = 0.02, respectively). The incidence of stroke after OPCAB was similar to that after PCI (0.98 (0.71–1.34), p > 0.99), but incidence of stroke after ONCAB was higher than that after OPCAB (1.59 (1.16–2.18), p < 0.01). The incidence of myocardial infarction after PCI was higher than that after OPCAB (2.41 (1.57–3.71), p < 0.01). The incidence of composite cardiovascular event after OPCAB was lower than that after PCI (1.52 (1.24–1.86), p < 0.01) or ONCAB (1.53 (1.24–1.90), p < 0.01). These findings were similar when patients were stratified to propensity score and institutes. Kaplan–Meier survival curve and event-free curve for composite cardiovascular event are presented in Fig. 3A and B.
Table 4:
Hazard ratios for outcomes after PCI or ONCAB compared with that after OPCAB adjusted by propensity score stratification
| Number of events |
Versus OPCAB | HR | 95% CI | p value* | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 3877) | ONCAB (n = 1381) | OPCAB (n = 1069) | |||||
| All-cause death | 454 | 154 | 125 | PCI | 1.50 | 1.20–1.86 | <0.01 |
| ONCAB | 1.18 | 0.93–1.51 | 0.33 | ||||
| Cardiovascular death | 282 | 113 | 73 | PCI | 1.74 | 1.32–2.31 | <0.01 |
| ONCAB | 1.49 | 1.11–2.02 | 0.02 | ||||
| Stroke | 192 | 107 | 64 | PCI | 0.98 | 0.71–1.34 | 1.00 |
| ONCAB | 1.59 | 1.16–2.18 | <0.01 | ||||
| Myocardial infarction | 188 | 54 | 29 | PCI | 2.41 | 1.57–3.71 | <0.01 |
| ONCAB | 1.61 | 1.01–2.55 | 0.09 | ||||
| Composite eventa | 564 | 230 | 139 | PCI | 1.52 | 1.24–1.86 | <0.01 |
| ONCAB | 1.53 | 1.24–1.90 | <0.01 | ||||
| Any revascularization | 1873 | 152 | 125 | PCI | 6.61 | 5.46–8.01 | <0.01 |
| ONCAB | 0.97 | 0.77–1.24 | 1.00 | ||||
a Composite event : cardiovascular death, stroke, or myocardial infarction.
*Adjusted for multiple comparison by the Bonferroni correction, i.e. we multiplied the original p values by 2 e.g. all-cause mortality after PCI was 1.50 times higher than that after OPCAB (p < 0.01), whereas that after ONCAB was similar to OPCAB (hazard ratio = 1.18, p = 0.33).
Figure 3:
Kaplan–Meier curves for each endpoint comparing PCI, ONCAB, and OPCAB. CV: cardiovascular; MI: myocardial infarction.
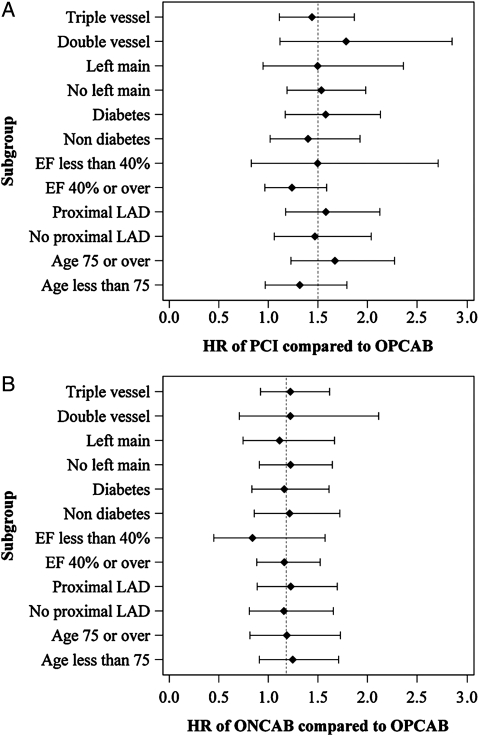
Forest plots in Fig. 4 show subset analysis for comparison of all-cause mortalities after OPCAB, ONCAB, and PCI. There were no significant interactions between PCI compared to OPCAB or ONCAB compared to OPCAB, and subgroups, indicating that there was no evidence against consistency of the adjusted HRs across subgroups.
Figure 4:
Forest plot of propensity-score-adjusted hazard ratios for death after PCI (A) or ONCAB (B) as compared with that after OPCAB in subgroups. Dashed line indicates hazard ratio in all patients of 1.50 (A) or 1.18 (B). Interaction tests, which are design to detect whether the specific factor modifies the effect of PCI or ONCAB relative to OPCAB, were not significant for all subgroups.
DISCUSSION
Main findings
In the present study, we investigated the impact of CABG, particularly OPCAB, on long-term outcomes after PCI or CABG in Japanese patients with multivessel and/or left main disease. In this population, we showed that CABG reduced the incidences of propensity adjusted all-cause and cardiovascular mortality compared with PCI and reduced the incidences of myocardial infarction and repeated revascularization. In addition, CABG was associated with better adjusted survival outcomes than PCI in high-risk subgroups such as with triple-vessel disease, diabetes, left ventricular dysfunction, proximal LAD disease, and the elderly. However, CABG was associated with higher stroke rate than PCI.
When comparing OPCAB with PCI or ONCAB, OPCAB was associated with better survival outcomes than PCI. Importantly, OPCAB significantly reduced the incidence of stroke compared with ONCAB, which was similar to PCI. OPCAB reduced the incidence of composite cardiovascular event in comparison to PCI or ONCAB. Need for any revascularization of OPCAB was far lower than that of PCI, which was similar to ONCAB. OPCAB was associated with better adjusted survival outcomes than PCI in high-risk subgroups such as with triple-vessel disease, diabetes, proximal LAD disease, and the elderly. There were no differences in survival outcomes between ONCAB and OPCAB in those prespecified high-risk subgroups. These outcomes strongly support the novel guidelines on myocardial revascularization of European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EACTS) [10], which strongly recommends CABG in complex coronary lesions such as triple-vessel and/or left main disease.
PCI versus CABG in multivessel without left main disease
A number of RCTs and meta-analyses have compared revascularization by PCI or CABG in the management of coronary artery disease with multivessel without left main disease [1–4]. A meta-analysis of four RCTs comparing PCI that involves bare-metal stents with CABG (Arterial Revascularization Therapies Study (ARTS), Coronary Angioplasty With Stenting Versus Coronary Bypass Surgery in Patients With Multiple Vessel Disease (ERACI-II), Medicine, Angioplasty or Surgery Study for Multi-Vessel Coronary Artery Disease (MASS-II), and the Stent or Surgery trial (SoS) showed similar 5-year survival outcomes but higher revascularization rates among patients with bare-metal stents [1,2]. Similarly, a meta-analysis of 23 RCTs by Bravata et al. has reported that survival outcomes up to 10 years were similar between PCI and CABG, although CABG was superior to PCI in that it relieved angina and led to fewer repeated revascularization [3]. Recently, pooled analysis of 10 RCTs by Hlatky et al. reported that long-term mortality is similar after PCI and CABG, although CABG might be a better option for patients with diabetes and those aged 65 years or older in terms of lower mortality [4]. However, all these trials used selected study population which tended to exclude high-risk patients such as with left main disease, the elderly, or left ventricular dysfunction. Thus, their results may not be generalized to current clinical practice [5,6].
On the other hand, several registry data that included more complex patients than RCTs have shown superiority of CABG in comparison to PCI [11–14]. Hannan et al. reported that CABG is associated with better 3-year adjusted survival outcomes than PCI in patients with two or more diseased coronary arteries using the data from the New York Registry, which included approximately 60 000 patients [11]. Similarly, Malenka et al. reported that adjusted survival is better after CABG than that after PCI in patients with triple-vessel disease [12]. Hannan et al. also compared outcomes between PCI using drug-eluting stent and CABG and showed that CABG constitutes to be associated with lower mortality than does treatment with drug-eluting stents, and is associated with lower mortality or myocardial infarction and repeat revascularization [13]. Meta-analysis of observational cohorts by Benedetto et al. also demonstrated that overall major adverse cardiac and cerebrovascular event rate continues to be higher after PCI by drug-eluting stents due to an excess of redo revascularization compared with CABG [14]. These results indicate that survival outcomes are similar between PCI and CABG in low- or moderate-risk patients; however, CABG is associated with better survival outcomes than PCI in high-risk patients [5,6].
PCI versus CABG in multivessel with left main disease
There are few registry data that investigated patients including left main disease. Brener et al. studied 6033 patients with high risks in which half of the patients had significant LV dysfunction or diabetes [15]. In addition, the study population included approximately 20% patients with left main disease. They showed that PCI was associated with an increased risk of death (propensity-adjusted HR = 2.3, p < 0.0001). Left main disease was one of significant independent predictors for mortality (p < 0.01). Biryukova et al. reported that CABG is associated with improved major adverse cardiovascular and cerebrovascular events in patients with three-vessel and/or left main stem disease compared with PCI at 6 and 12 months [16]. Recently, a larger RCT of drug-eluting stents versus CABG for left main disease (the Synergy between PCI and Taxus and Cardiac Surgery (SYNTAX) trial) demonstrated that CABG was associated with better outcomes at 1 year proportionally with the increase in SYNTAX score [17]. In patients undergoing CABG, the binary 12-month rates of major adverse cardiac or cerebrovascular events were similar among patients with low (0–22, 14.7%) and those with high scores (>33, 10.9%). By contrast, in patients with PCI, the rate of those events was significantly increased among patients with high SYNTAX scores (23.4%) as compared with those with low scores (13.6%) (p = 0.002 for high vs low scores). This result also indicates that CABG is associated with better outcomes than PCI in high-risk patients with more complex coronary lesions, including left main disease. Registry arm of SYNTAX trial also reported that CABG still remains the dominant revascularization strategy in patients with multivessel or left main disease [18].
In our previous report, we could not demonstrate the superiority of CABG in comparison to PCI regarding adjusted survival outcomes (p = 0.06) in patients with multivessel disease without left main disease in the CREDO-Kyoto Registry [9]. In the present study, however, we have shown that CABG, particularly OPCAB, is associated with better adjusted survival and event-free outcomes than PCI. Furthermore, OPCAB was associated with better survival outcomes in high-risk subgroups such as those with LV dysfunction and the elderly. The present analysis additionally included patients with left main disease into analysis data set, and the differences in outcomes between the two studies appear to be attributable to inclusion of patients with left main disease. It should be noted that PCI for left main disease was adopted more selectively in the era of bare-mental stent (BMS) as compared with contemporary clinical practice and, therefore, patients with left main disease are more prone to be subjected to selection bias.
Impact of OPCAB on coronary revascularization
Several RCTs and meta-analyses have been conducted over the last decade comparing outcomes of OPCAB and ONCAB. Equivalent short- and long-tem angiographic graft patency has also been demonstrated [19,20]. However, the benefit of OPCAB regarding mortality and morbidity (stroke and myocardial infarction) has been controversial [7,8,20–22]. This may be because these studies have been underpowered to determine significant differences in these endpoints [23]. Recently, a large RCT by Shroyer et al. (The ROOBY trial) reported that patients undergoing OPCAB had worse 1-year composite outcomes (death, myocardial infarction, or repeated revascularization) and poorer graft patency than those undergoing ONCAB [22]. However, the study excluded high-risk patients with small target vessels or diffuse coronary disease. More importantly, most of the operations were performed by relatively inexperienced surgeons. Thus, a study involving surgeons with more experience and high-risk patients will more accurately reflect real-world CABG outcomes.
On the other hand, several large registry data have provided compelling evidence in favor of OPCAB. The New York State Registry reported that OPCAB had significantly lower risk-adjusted 30-day mortality, as well as postoperative stroke and respiratory failure [24]. Survival outcome was similar between ONCAB and OPCAB, although patients undergoing OPCAB needed more repeated revascularization. An intension-to-treat analysis of 42 477 patients from the Society of Thoracic Surgeons National Adult Cardiac database showed a reduction in risk-adjusted mortality, stroke, and preoperative myocardial infarction in patients undergoing OPCAB [25]. In the present study of the CREDO-Kyoto Registry, there were no differences in survival and event-free (myocardial infarction and repeated revascularization) between ONCAB and OPCAB. However, the incidences of stroke and composite cardiovascular event were lower after OPCAB [9].
Study limitations
There are several important limitations of this study. First, this study deals with patients with PCI using bare-metal stents. Further study comparing CABG with PCI using drug-eluting stents will be favorable. Second, important medications, statins in particular, to prevent cardiovascular events are obviously underused. Although inclusion or exclusion of medications did not influence the survival outcomes in the present study, more optimal use of medications might have changed the long-term outcome of both PCI and CABG.
CONCLUSIONS
CABG, particularly OPCAB, is associated with better survival and event-free outcomes than PCI in patients with multivessel and/or left main disease in bare-metal stent era. The incidence of stroke after OPCAB was lower than that after ONCAB and is similar to PCI. OPCAB may be a favorable coronary revascularization strategy, especially in high-risk populations. Further study comparing CABG with drug-eluting stents with longer follow-up is favorable.
Funding
This work was supported in part by a Grant for Clinical Research for Evidence Based Medicine from the Ministry of Health, Labor and Welfare in Japan to T. Kimura and an educational grant from the Research Institute for Production Development (Kyoto, Japan).
Conflict of interest: none declared.
REFERENCES
- 1.Serruys PW, Ong ATL, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJRM, Schonberger JPMA, Buller N, Bonser R, Disco C, Backx B, Hugenholtz PG, Firth BG, Unger F. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575–81. doi: 10.1016/j.jacc.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 2.Daemen J, Boersma E, Flather M, Booth J, Stables R, Rodriguez A, Rodriguez-Granillo G, Hueb WA, Lemos PA, Serruys PW. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation. 2008;118:1146–54. doi: 10.1161/CIRCULATIONAHA.107.752147. [DOI] [PubMed] [Google Scholar]
- 3.Bravata DM, Gienger AL, McDonald KM, Sundaram V, Perez MV, Varghese R, Kapoor JR, Ardehali R, Owens DK, Hlatky MA. Systematic review: the comparative effectiveness of percutaneous coronary interventions and coronary artery bypass graft surgery. Ann Intern Med. 2007;147:703–16. doi: 10.7326/0003-4819-147-10-200711200-00185. [DOI] [PubMed] [Google Scholar]
- 4.Hlatky MA, Boothroyd DB, Bravata DM, Boersma E, Booth J, Brooks MM, Carrié D, Clayton TC, Danchin N, Flather M, Hamm CW, Hueb WA, Kähler J, Kelsey SF, King SB, Kosinski AS, Lopes N, McDonald KM, Rodriguez A, Serruys P, Sigwart U, Stables RH, Owens DK, Pocock SJ. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373:1190–7. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 5.Taggart DP. PCI or CABG in coronary artery disease? Lancet. 2009;373:1150–2. doi: 10.1016/S0140-6736(09)60574-2. [DOI] [PubMed] [Google Scholar]
- 6.Falk V. The ‘real world’ asks for coronary artery bypass grafting. Eur J Cardiothorac Surg. 2009;36:609–10. doi: 10.1016/j.ejcts.2009.03.070. [DOI] [PubMed] [Google Scholar]
- 7.Puskas JD, Kilgo PD, Lattouf OM, Thourani VH, Cooper WA, Vassiliades TA, Chen EP, Vega JD, Guyton RA. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Ann Thorac Surg. 2008;86:1139–46. doi: 10.1016/j.athoracsur.2008.05.073. [DOI] [PubMed] [Google Scholar]
- 8.Sedrakyan A, Wu AW, Parashar A, Bass EB, Treasure T. Off-pump surgery is associated with reduced occurrence of stroke and other morbidity as compared with traditional coronary artery bypass grafting: a meta-analysis of systematically reviewed trials. Stroke. 2006;37:2759–69. doi: 10.1161/01.STR.0000245081.52877.f2. [DOI] [PubMed] [Google Scholar]
- 9.Kimura T, Morimoto T, Furukawa Y, Nakagawa Y, Shizuta S, Ehara N, Taniguchi R, Doi T, Nishiyama K, Ozasa N, Saito N, Hoshino K, Mitsuoka H, Abe M, Toma M, Tamura T, Haruna Y, Imai Y, Teramukai S, Fukushima M, Kita T. Long-term outcomes of coronary-artery bypass graft surgery versus percutaneous coronary intervention for multivessel coronary artery disease in the bare-metal stent era. Circulation. 2008;118(Suppl.):S199–209. doi: 10.1161/CIRCULATIONAHA.107.735902. [DOI] [PubMed] [Google Scholar]
- 10.Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI) Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2010;(Suppl.):S1–52. [Google Scholar]
- 11.Hannan EL, Racz MJ, Walford G, Jones RH, Ryan TJ, Bennett E, Culliford AT, Isom OW, Gold JP, Rose EA. Long-term outcomes of coronary-artery bypass grafting versus stent implantation. N Engl J Med. 2005;352:2174–83. doi: 10.1056/NEJMoa040316. [DOI] [PubMed] [Google Scholar]
- 12.Malenka DJ, Leavitt BJ, Hearne MJ, Robb JF, Baribeau YR, Ryan TJ, Helm RE, Kellett MA, Dauerman HL, Dacey LJ, Silver MT, VerLee PN, Weldner PW, Hettleman BD, Olmstead EM, Piper WD, O’Connor GT Northern New England Cardiovascular Disease Study Group. Comparing long-term survival of patients with multivessel coronary disease after CABG or PCI: analysis of BARI-like patients in northern New England. Circulation. 2005;112(Suppl.):I-371–6. doi: 10.1161/CIRCULATIONAHA.104.526392. [DOI] [PubMed] [Google Scholar]
- 13.Hannan EL, Wu C, Walford G, Culliford AT, Gold JP, Smith CR, Higgins RS, Carlson RE, Jones RH. Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358:331–41. doi: 10.1056/NEJMoa071804. [DOI] [PubMed] [Google Scholar]
- 14.Benedetto U, Melina G, Angeloni E, Refice S, Roscitano A, Fiorani B, Di Nucci GD, Sinatra R. Coronary artery bypass grafting versus drug-eluting stents in multivessel coronary disease. A meta-analysis on 24,268 patients. Eur J Cardiothorac Surg. 2009;36:611–5. doi: 10.1016/j.ejcts.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Brener SJ, Lytle BW, Casserly IP, Schneider JP, Topol EJ, Lauer MS. Propensity analysis of long-term survival after surgical or percutaneous revascularization in patients with multivessel coronary artery disease and high-risk features. Circulation. 2004;109:2290–5. doi: 10.1161/01.CIR.0000126826.58526.14. [DOI] [PubMed] [Google Scholar]
- 16.Biryukova E, Williams FM, Valencia O, Kaski JC, Bland M, Jahangiri M. Comparison of mid-term outcome in patients with three-vessel and/or left main disease undergoing percutaneous coronary intervention and coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2010;37:905–11. doi: 10.1016/j.ejcts.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 17.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 18.Kappetein AP, Dawkins KD, Mohr FW, Morice MC, Mack MJ, Russell ME, Pomar J, Serruys PW. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease: insights from the SYNTAX run-in phase. Eur J Cardiothorac Surg. 2006;29:486–91. doi: 10.1016/j.ejcts.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 19.Magee MJ, Alexander JH, Hafley G, Ferguson TB, Jr, Gibson CM, Harrington RA, Peterson ED, Califf RM, Kouchoukos NT, Herbert MA, Mack MJ PREVENT IV Investigators. Coronary artery bypass graft failure after on-pump and off-pump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg. 2008;85:494–9. doi: 10.1016/j.athoracsur.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Angelini GD, Culliford L, Smith DK, Hamilton MC, Murphy GJ, Ascione R, Baumbach A, Reeves BC. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trials. J Thorac Cardiovasc Surg. 2009;137:295–303. doi: 10.1016/j.jtcvs.2008.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C. Clinical outcomes in randomized trials of off- vs. on-pump coronary artery bypass surgery: systematic review with meta-analyses and trial sequential analyses. Eur Heart J. 2008;29:2601–16. doi: 10.1093/eurheartj/ehn335. [DOI] [PubMed] [Google Scholar]
- 22.Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, Lucke JC, Baltz JH, Novitzky D Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med. 2009;361:1827–37. [Google Scholar]
- 23.Kerendi F, Morris CD, Puskas JD. Off-pump coronary bypass surgery for high-risk patients: only in expert centers? Curr Opin Cardiol. 2008;23:573–8. doi: 10.1097/HCO.0b013e328312c311. [DOI] [PubMed] [Google Scholar]
- 24.Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, Culliford AT, Gold JP, Jones RH. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation. 2007;116:1145–52. doi: 10.1161/CIRCULATIONAHA.106.675595. [DOI] [PubMed] [Google Scholar]
- 25.Puskas JD, Edwards FH, Pappas PA, O’Brien S, Peterson ED, Kilgo P, Ferguson TB., Jr Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg. 2007;84:1447–54. doi: 10.1016/j.athoracsur.2007.06.104. [DOI] [PubMed] [Google Scholar]