Abstract
The Primary Care Information Project is a New York City initiative aimed at improving population health through the improved delivery of preventive care. It has assisted with the adoption of a fully functional electronic health record (EHR) in over 300 primary care practices. Practices with EHRs automatically transmit summary data that can be used to track population health indicators for recommended preventive care. Early analysis, focusing on small practices with fewer than 10 providers serving Medicaid and uninsured populations, showed increases in the delivery of recommended services of 0.1–2.4% per month (p≤0.05). However, measurement of preventive care across this population is limited by some inconsistency of data transmission. This study shows that EHRs can be used to track the delivery of recommended preventive care across small primary care practices serving lower income communities in which few data are generally available for assessing population health.
Keywords: Clinical preventive services, electronic health record (EHR), preventive care, primary care, small physician office practices, small physician-owned practices, urban population
The consistent and timely delivery of recommended preventive services can reduce avoidable deaths and complications from chronic conditions.1 The availability of population estimates on the delivery of preventive services has traditionally been limited to standard methods of data collection through large-scale surveys (ie, National Health and Nutrition Examination Survey), analysis of claims data, or chart reviews. More recently, a growing number of researchers have recognized that the electronic health record (EHR) provides an alternative data source for tracking the delivery of recommended preventive services.2–4 The advantages of using EHRs to track population health include accessing information more quickly and utilizing an existing data source to reduce expending additional resources for data collection. In addition, through secured information networks, patient data can be aggregated or summarized to generate rates of preventive care minimizing the risk of exposure of patient information.5
In addition to tracking the delivery of preventive services, the use of EHRs has been associated with improving the quality of care for patients,6–9 particularly in the primary care setting.10–12 The Primary Care Information Project (PCIP),13 14 a bureau of the New York City (NYC) Department of Health and Mental Hygiene was established to improve population health, targeting communities with 10% or greater Medicaid-insured or uninsured patients. PCIP has assisted small physician-owned primary care practices (defined as having 10 or fewer providers at a practice), as well as community health centers, hospital outpatient facilities, and large independent practices to adopt EHR as a means to improve the delivery of preventive care. Through a competitive procurement process, PCIP selected eClinicalWorks, a commercial EHR software vendor, to co-develop a prevention-oriented EHR that included new functionality allowing providers to measure and report their rates of preventive care. Practices adopting the eClinicalWorks version of the EHR through PCIP have patient-specific point-of-care reminders, a quality-of-care reporting tool that displays in real time a list of patients in the practice meeting guidelines for recommended preventive and health-promoting services, and the capability to automatically transmit summarized preventive care data to PCIP. Currently, PCIP represents approximately 25% of the estimated 9000 primary care providers in NYC. Providers working with PCIP serve an estimated 2 million patients, in a city of 8.4 million residents.15 This communication describes the early results of preventive care trends across small physician-owned practices, representing approximately 60% of offices working with PCIP.
Methods
Architecture
The PCIP established an automated data transmission process, mediated by eClinicalWorks, to receive summarized data from each practice on the monthly delivery of recommended services; for many practices the transmissions do not start until a few of months after EHR implementation. Detailed individual patient records are never transmitted to PCIP and remain on the practice or vendor server. Only aggregated (count) information is transmitted to PCIP via a secure, encrypted public health information network system protocol.
Electronic reporting
The medical records adopted by practices in the project are fully functional EHR capable of capturing patient demographics, as well as longitudinal clinical information such as medical history, medications, and laboratory results.16 In collaboration with PCIP, eClinicalWorks developed programming within the EHR to calculate the delivery of recommended services by provider and by practice. The selected recommended services incorporated into the EHR are based on the Take Care New York (TCNY) initiative,17 the city's public health agenda to promote 10 basic areas of healthy habits people can follow to reduce preventable deaths and complications from chronic conditions. The TCNY indicators include primary and secondary prevention goals and were created to align with recommendations from Healthy People 201018/202019 as well as National Quality Forum endorsed quality measures. However, some measures were modified in order for providers to be able to act on the information at the point of care. TCNY measures programmed into the EHR generate counts of the eligible population for a specific recommended service (denominator) and those receiving the recommended service (numerator). For each practice, performance rates for each TCNY measure are generated by the EHR. For example, in the breast cancer screening measure, the denominator would include all women 40 years of age and older who had at least one visit in the past year, and the numerator would include the subset who had a mammogram within the past 2 years.
Study population
The study population consists of 309 small independent practices (≤10 providers) that adopted an EHR from August 2007 to March 2010 through PCIP. Practice characteristics such as staffing levels and patient insurance status were tabulated using self-reported data from the practice's application to join PCIP. The practices included in this study must have transmitted at least 1 month of summarized data, for at least one TCNY measure.
Statistical analyses
Longitudinal regression analyses were conducted on the monthly rates for each of the TCNY measures using the first year of transmitted data, adjusting for the autocorrelation between observations within practice. Each practice contributed a monthly longitudinal series of data with a minimum of 1 month to a maximum of 12 months of data for each measure. The dependent variable is each practice's monthly performance on the TCNY measure. In order to estimate the trend, or the average monthly change in rate, the only predictor included in the model was time (months 1–12), where 1 is the first month of transmitted data. The trend was considered significant if the p value was ≤0.05. For each month and measure, only data that passed data quality checks were included in the analyses. All analyses were conducted using the PROC MIXED procedure in the SAS software, V.9.2. This study was deemed by the NYC Health Department's Institutional Review Board as research not involving human subjects.
Results
At the 309 practices, a total of 775 providers was included in this analysis (680 physicians, 95 medical support staff, eg, nurses and physician assistants). Practice-level characteristics are summarized in table 1. The most commonly reported specialties included internal medicine (41%), pediatrics (24%), family medicine (17%), and obstetrics and gynecology (5%). Across practices, the average time from the practice signing a PCIP agreement to EHR implementation was 6.4 months. Most practices had one to two full-time equivalent (FTE) physicians (82%); 81% of those practices did not have any medical support staff per physician FTE, while 90% reported at least one non-medical administrative support staff per practice or over 0.1 administrative staff per physician FTE (table 1). On average, Medicaid and uninsured patients accounted for 53% of patients seen. The average number of outpatient office visit encounters per practice was 596.6 per month, and the average total FTE per practice was 1.8.
Table 1.
Distribution of practice characteristics
| No of practices implementing EHR per year | |
| Year | No of practices (%) |
| All years | 309 (100.0) |
| 2007 | 33 (10.7) |
| 2008 | 103 (33.3) |
| 2009 | 142 (46.0) |
| 2010 | 31 (10.0) |
| Self-reported practice demographics | |
| No of practices (%) | |
| Practice-level staffing distribution | |
| No of FTE physicians (MD or DO) | |
| 1.0 | 183 (59.2) |
| 1.1–2.0 | 71 (23.0) |
| >2.0 | 55 (17.8) |
| No of medical support staff per FTE physician (PA, RN) | |
| 0 | 251 (81.2) |
| 0.1–1.0 | 52 (16.8) |
| >1.0 | 6 (1.9) |
| No of administrative support staff per FTE physician | |
| 0 | 31 (10.0) |
| 0.1–1.0 | 118 (38.2) |
| 1.1–2.0 | 93 (30.1) |
| 2.1–6.0 | 67 (21.7) |
| Practice-level patient insurance status distribution | |
| (%) Patients with Medicaid insurance or uninsured | |
| ≤20.0 | 53 (17.2) |
| 20.1–50.0 | 98 (31.7) |
| >50.1 | 158 (51.1) |
| Practice-level EHR implementation times | |
| No of practices (%) | |
| Time from signing enrollment contract to implementation of EHR | |
| 4 months | 36 (11.7) |
| 6 months | 124 (40.1) |
| 8 months | 86 (27.8) |
| 10 months | 35 (11.3) |
| 12 months | 18 (5.8) |
| >12 months | 10 (3.2) |
| Ambulatory services (derived from EHR) | |
| No of practices (%) | |
| No of patient encounters per month* | |
| ≤200 | 98 (33.9) |
| 201–1000 | 145 (50.2) |
| ≥1000 | 46 (15.9) |
The total number of practices is 289 for this variable as 20 practices transmitted less than 1 month of ambulatory services data within the first 12 months of implementing EHR.
DO, doctor of osteopathic medicine; EHR, electronic health records; FTE, full-time equivalent; MD, medical doctor; PA, physician assistant; RN, registered nurse.
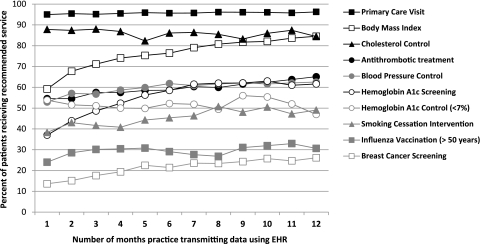
Figure 1 shows the average monthly performance rates using the first year of transmitted data for each of the TCNY measures, where month 1 is the first month of transmitted data for each practice. Table 2 shows that the starting rate for six of the 10 measures was greater than 50%; two of the measures, primary care visit (95.0%) and cholesterol control (87.8%), were higher, whereas initial rates of smoking cessation intervention (38.3%), breast cancer screening (13.6%), influenza vaccination for patients older than 50 years (24.0%) and hemoglobin A1c screening (37.0%) were lower. Estimated trends, as changes in rate per month, were generally positive (p≤0.05), ranging from 0.1% for primary care visits to 2.4% increases per month for hemoglobin A1c screening. Only hemoglobin A1c control (<7%) had a significant decrease in trend corresponding to −0.5% per month. Cholesterol control was also negative (−0.8%) but not significantly. However, for both these measures, less than half of the practices contributed data at the beginning of the study period (eg, start N<150).
Figure 1.
Average monthly rates of delivery recommended preventive care. EHR, electronic health record.
Table 2.
Longitudinal trends of monthly rates of recommended preventive care*
| Take Care New York measures | Average monthly denominator (per practice) | Start N† | End N† | Average rate (month 1) | % Change in rate per month |
| Primary care visit: % of patients ≥18 years with a documented visit who have seen their assigned primary care doctor in the past 12 months | 309.7 | 299 | 245 | 95.0% | 0.11‡ |
| BMI: % of patients ≥18 years who had a BMI recorded in the past 24 months | 329.7 | 282 | 231 | 59.2% | 1.96‡ |
| Smoking cessation intervention: % of patients ≥18 years classified as a ‘current smoker’ who received a prescription or counseling intervention in the past 12 months | 47.9 | 133 | 67 | 38.3% | 0.86‡ |
| Cholesterol control: % of men ≥35 years and % of women ≥45 years without a diagnosis of DM or IVD whose most recent measurement of LDL <160 or total cholesterol <240 in the past 5 years | 91.4 | 113 | 21 | 87.8% | −0.81 |
| Breast cancer screening: % of women ≥40 years who had a mammogram (ordered or self-reported) in the past 2 years | 211.4 | 97 | 54 | 13.6% | 1.09‡ |
| Influenza vaccination (>50 years): % of patients ≥50 years who received a flu shot in the most recent flu season (September 1—April 1) | 223.3 | 180 | 104 | 24.0% | 0.46‡ |
| HbA1c screening: % of patients 18–75 years with DM who had at least one HbA1c test result recorded in the past 6 months | 66.3 | 161 | 106 | 37.0% | 2.35‡ |
| HbA1c control (<7%): % of patients 18–75 years with DM whose most recent HbA1c level is <7.0% | 39.5 | 76 | 10 | 53.8% | −0.50‡ |
| Antithrombotic treatment: % of patients ≥18 years with IVD or patients ≥40 years with DM who have documented use of aspirin or other antithrombotic drug in the past 12 months | 82.2 | 202 | 153 | 54.6% | 0.85‡ |
| Blood pressure control: % of patients 18–75 years with hypertension (and no diagnosis of DM or IVD) whose most recent systolic pressure was <140, and diastolic pressure was <90 in the past 12 months | 79.3 | 177 | 155 | 52.9% | 0.72‡ |
Take Care New York measures designed to decrease the occurrence of preventable illnesses and deaths in New York City, originally based on the Healthy People 2010 guidelines (http://www.healthypeople.gov\2010\Publications).
Start N=number of physician office practices contributing data in the first months of the study (month 0); End N=number of physician office practices contributing data in the last month of the study (month 12).
p≤0.05.
BMI, body mass index; DM, diabetes mellitus; HbA1c, hemoglobin A1c; IVD, ischemic vascular disease; LDL, low-density lipoprotein.
Discussion
This study has shown that EHRs can be used to track the delivery of recommended preventive care across small, independent primary care practices that serve primarily lower-income patients; a population with few data currently available for assessing population health. In our summary data, early trends show significant improvements in eight out of 10 measures on the delivery of recommended services. Decreases observed for two of the control measures may have been due to increased screening rates during the study period. Across the measures, the number of patients in the denominator increased during the first year on the EHR by 30% on average, whereas the denominators more than doubled for the two control measures: cholesterol control (172%) and hemoglobin A1c control (101%). A separate study is being conducted to identify factors that are associated with increases or decreases in performance on these TCNY measures.
Unlike estimates of population health based on a sampling of patients, in which each patient represents many times more patients in the target population, this project aims to track whole segments of the population in almost real time. However, to achieve these goals, high rates of transmission on each of the measures is needed. In addition, in order for EHR to accurately tabulate rates of delivery of recommended services, providers have to become accustomed to documenting information in structured data fields linked to the capture of information used to calculate the measures. As a result of potential variation in documentation, the numerators, and sometimes the denominators, can undercount the number of patients. Observed increases in performance could be due to an actual improvement in performance, or in combination with improvements in providers appropriately documenting information in the EHR. Additional research is also being conducted to identify which measures can most reliably and accurately be tracked using EHRs.
This project has demonstrated that data transmission from small physician-owned practices in primary care settings can be used by a municipal health department on a large scale to track the delivery of recommended preventive and health-promoting services; however, the architecture currently used for data transmission has limitations. For individual practices, data transmissions can be interrupted or fail to occur due to software upgrades or other technological issues specific to the practice. PCIP is currently developing a parallel query system that would enable authorized NYC Health Department staff to run queries, in real time, against patient de-identified data from the practice EHR. Establishing a flexible query system will reduce interruptions to data transmissions by allowing PCIP to supplement and validate automatically transmitted data from practices experiencing difficulties with the automated transmissions, while minimizing the privacy and security concerns with clinical data extraction.
This study provides an early perspective on the characteristics of over 300 small practices adopting new health information technology (IT) with the potential for population health tracking. EHRs are expected to improve the efficiency of the healthcare system,20–23 the quality of care and safety of patients.6–9 Yet EHR adoption remains fairly low in the USA, with only approximately 13–25% of providers using a basic EHR,24 25 and approximately 4% using a fully functional EHR,26 with features such as electronic reminders, computerized provider order entry or drug interaction alerts. As more providers adopt EHRs and more fully integrate health IT into their daily routines, more robust assessments of factors that impact the delivery of preventive services in ambulatory primary care settings will be identified.
Observed increases in the delivery of recommended preventive care within the first year of implementing EHRs were small but significant. Over time, continued increases in the performance on the TCNY measures will likely have a positive impact on overall population health. The practices assisted by PCIP are small physician-owned practices serving primarily low-income patients, a group that has historically struggled to adopt health IT.27–36 As part of the American Recovery and Reinvestment Act of 2009, federal funds have established regional extension centers to assist physician office practices across the country in implementing EHRs and achieving the meaningful use of EHRs.37 Despite challenges in data transmission, continued use of EHRs to track population health across primary care practices will be important in demonstrating the value of the broad adoption of health IT.
Footnotes
Funding: This work was fully supported by the New York City tax levy.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Farley TA, Dalal MA, Mostashari F, et al. Deaths preventable in the U.S. by improvements in use of clinical preventive services. Am J Prev Med 2010;38:600–9 [DOI] [PubMed] [Google Scholar]
- 2.Tang PC, Ralston M, Arrigotti MF, et al. Comparison of methodologies for calculating quality measures based on administrative data versus clinical data from an electronic health record system: implications for performance measures. J Am Med Inform Assoc 2007;14:10–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weber V, Bloom F, Pierdon S, et al. Employing the electronic health record to improve diabetes care: a multifaceted intervention in an integrated delivery system. J Gen Intern Med 2008;23:379–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Persell SD, Kho AN, Thompson JA, et al. Improving hypertension quality measurement using electronic health records. Med Care 2009;47:388–94 [DOI] [PubMed] [Google Scholar]
- 5.Diamond CC, Mostashari F, Shirky C. Collecting and sharing data for population health: a new paradigm. Health Aff (Millwood) 2009;28:454–66 [DOI] [PubMed] [Google Scholar]
- 6.Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc 2005;12:431–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorr D, Bonner LM, Cohen AN, et al. Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc 2007;14:156–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baron RJ. Quality improvement with an electronic health record: achievable, but not automatic. Ann Intern Med 2007;147:549–52 [DOI] [PubMed] [Google Scholar]
- 9.Welch WP, Bazarko D, Ritten K, et al. Electronic health records in four community physician practices: impact on quality and cost of care. J Am Med Inform Assoc 2007;14:320–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pham HH, Schrag D, Hargraves JL, et al. Delivery of preventive services to older adults by primary care physicians. JAMA 2005;294:473–81 [DOI] [PubMed] [Google Scholar]
- 11.Fiks AG, Grundmeier RW, Biggs LM, et al. Impact of clinical alerts within an electronic health record on routine childhood immunization in an urban pediatric population. Pediatrics 2007;120:707–14 [DOI] [PubMed] [Google Scholar]
- 12.Friedberg MW, Coltin KL, Safran DG, et al. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med 2009;151:456–63 [DOI] [PubMed] [Google Scholar]
- 13.Frieden TR, Mostashari F. Health care as if health mattered. JAMA 2008;299:950–2 [DOI] [PubMed] [Google Scholar]
- 14.Mostashari F, Tripathi M, Kendall M. A tale of two large community electronic health record extension projects. Health Aff (Millwood) 2009;28:345–56 [DOI] [PubMed] [Google Scholar]
- 15.New York City Department of City Planning Current Population Estimates 2000–2009. http://www.nyc.gov/html/dcp/html/census/popcur.shtml (accessed 10 Jun 2011).
- 16.Healthcare Information and Management Systems Society (HIMSS) Electronic Health Record 2011. http://www.himss.org/ASP/topics_ehr.asp (accessed 10 Jun 2011).
- 17.New York City Department of Health and Mental Hygiene Take Care New York 2012, posted September 2009. http://www.nyc.gov/html/doh/html/tcny/index.shtml (accessed 10 Jun 2011).
- 18.US Department of Health and Human Services Healthy People 2010. In: 2nd edn Washington, DC: US Government Printing Office, 2000. http://www.healthypeople.gov/2010/document/tableofcontents.htm (accessed 10 Jun 2011). [Google Scholar]
- 19.US Department of Health and Human Services Healthy People 2020. http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx (accessed 10 Jun 2011).
- 20.Tierney WM, Miller ME, Overhage JM, et al. Physician inpatient order writing on microcomputer workstations. Effects on resource utilization. JAMA 1993;269:379–83 [PubMed] [Google Scholar]
- 21.Shojania KG, Yokoe D, Platt R, et al. Reducing vancomycin use utilizing a computer guideline: results of a randomized controlled trial. J Am Med Inform Assoc 1998;5:554–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen P, Tanasijevic MJ, Schoenenberger RA, et al. A computer-based intervention for improving the appropriateness of antiepileptic drug level monitoring. Am J Clin Pathol 2003;119:432–8 [DOI] [PubMed] [Google Scholar]
- 23.Bates DW, Kuperman GJ, Rittenberg E, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med 1999;106:144–50 [DOI] [PubMed] [Google Scholar]
- 24.Burt CW, Sisk JE. Which physicians and practices are using electronic medical records? Health Aff (Millwood) 2005;24:1334–43 [DOI] [PubMed] [Google Scholar]
- 25.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care – a national survey of physicians. N Engl J Med 2008;359:50–60 [DOI] [PubMed] [Google Scholar]
- 26.Hing ES, Hsiao CJ. Electronic Medical Record Use by Office-based Physicians and Their Practices: United States, 2007. Hyattsville, MD: National Center for Health Statistics, 2010. Report no. 0147–3956 (Print) 0147–3956 (Linking). [PubMed] [Google Scholar]
- 27.Rind DM, Safran C. Real and imagined barriers to an electronic medical record. Proc Annu Symp Comput Appl Med Care 1993:74–8 [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson KB. Barriers that impede the adoption of pediatric information technology. Arch Pediatr Adolesc Med 2001;155:1374–9 [DOI] [PubMed] [Google Scholar]
- 29.Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23:116–26 [DOI] [PubMed] [Google Scholar]
- 30.Valdes I, Kibbe DC, Tolleson G, et al. Barriers to proliferation of electronic medical records. Inform Prim Care 2004;12:3–9 [DOI] [PubMed] [Google Scholar]
- 31.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: report of a 2004 ACMI discussion. J Am Med Inform Assoc 2005;12:8–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee J, Cain C, Young S, et al. The adoption gap: health information technology in small physician practices. Understanding office workflow can help realize the promise of technology. Health Aff (Millwood) 2005;24:1364–6 [DOI] [PubMed] [Google Scholar]
- 33.Rosenfeld S, Bernasek C, Mendelson D. Medicare's next voyage: encouraging physicians to adopt health information technology. Health Aff (Millwood) 2005;24:1138–46 [DOI] [PubMed] [Google Scholar]
- 34.Ford EW, Menachemi N, Peterson LT, et al. Resistance is futile: but it is slowing the pace of EHR adoption nonetheless. J Am Med Inform Assoc 2009;16:274–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gans D, Kralewski J, Hammons T, et al. Medical groups' adoption of electronic health records and information systems. Health Aff (Millwood) 2005;24:1323–33 [DOI] [PubMed] [Google Scholar]
- 36.Bates DW. Physicians and ambulatory electronic health records. Health Aff (Millwood) 2005;24:1180–9 [DOI] [PubMed] [Google Scholar]
- 37.Health Information Technology Extension Program U.S. Department of Health and Human Services. 2010. http://healthit.hhs.gov/portal/server.pt/community/hit_extension_program_-_regional_centers_cooperative_agreement_program/1335/home/16374 (accessed 23 Apr 2011).