Abstract
OBJECTIVE
Secular trends in the epidemiology of diabetes are best described by studying the same population over time, but few such studies exist. Using surveys from Mauritius in 1987 and 2009, we examined 1) the change in the prevalence of diabetes, 2) the extent to which changes in traditional diabetes risk factors explained the increase, and 3) the change in the distribution of plasma glucose levels over time.
RESEARCH DESIGN AND METHODS
Independent population-based surveys were undertaken in Mauritius in 1987 and 2009 using similar methodology in adults aged 20–74 years. Physical measurements and fasting blood samples were taken, and an oral glucose tolerance test was performed at both surveys.
RESULTS
The age-standardized prevalence of diabetes in 2009 was 22.3% (95% CI 20.0–24.6) among men and 20.2% (18.3–22.3) among women, representing an increase since 1987 of 64 and 62% among men and women, respectively. Concurrent changes in the distribution of age, ethnicity, waist circumference, BMI, physical activity, smoking, family history of diabetes, and hypertension explained more of the increase in the prevalence of diabetes in men than in women. Increases in plasma glucose (especially fasting glucose) were seen across the population but were greater at the upper levels.
CONCLUSIONS
In Mauritius, there has been a marked increase in diabetes prevalence over 22 years. This mainly results from changes in traditional risk factors, leading to population-wide increases in plasma glucose levels. Interventions to control this escalation of diabetes should focus on population-wide strategies.
There are 285 million people with diabetes, and this is predicted to increase to 439 million by 2030, with larger increases in the developing than in the developed world (1). The reasons driving these increases include aging of populations, changes in physical activity levels, and patterns of dietary intake. Available data on the increasing prevalence of diabetes come from comparing studies of different designs in different populations, while most information on risk factors comes from cohort studies. Few publications to date have examined population-wide change in prevalence and in risk factors over time using consistent methodology at different time points.
Also unclear is to what extent the rise in the prevalence of diabetes is a result of a uniform increase across the whole spectrum of plasma glucose; the rise might be restricted to increases at the upper end of the glucose distribution. Data from the U.S. have shown that increases in the prevalence of diabetes have been accompanied by an increase in right skew of the fasting glucose distributions (2). There has been no detailed analysis of trends in the continuous distribution of glucose using 2-h postload glucose (2hrPG). Understanding the nature of the change in plasma glucose distribution is essential for determining the extent to which interventions should be directed at the whole population or just at those already at high risk.
Using national health surveys from Mauritius in 1987 and 2009, we sought to examine 1) the magnitude of the change in diabetes prevalence, 2) the extent to which changes in traditional diabetes risk factors can explain the increase in diabetes prevalence, and 3) whether increases in blood glucose levels were uniform across the population or were confined to those already at the upper end of the plasma glucose distribution.
RESEARCH DESIGN AND METHODS
Background and population
Mauritius has a population of 1.3 million people, which comprises 68% of South Asian (Indian) origin, 3% of Chinese, 27% of African (Creole), and 2% of Franco-Mauritian. In 1987 and 2009, population-based surveys using similar standardized protocols were conducted in Mauritius (3,4). In 1987, 11 randomly selected (with probability proportional to size) population clusters were surveyed. In this survey, all household members were invited to participate. In 2009, nine index clusters were chosen: one randomly selected from each of the nine districts in Mauritius. Then, two neighboring clusters were chosen surrounding the index cluster to form a “super cluster.” From this super cluster, one in three households was randomly selected and one adult per household was invited to participate.
A total of 11,454 people were recruited over the two surveys (1987, n = 5,083, age 22–74 years; 2009, n = 6371, age 20–74 years). The response rates for the 1987 (3) and the 2009 survey were both over 85%. The ethics committee of the Ministry of Health and Quality of Life, Mauritius, approved both surveys.
Risk factors at baseline
Weight, height, and waist and hip circumferences were measured. Waist circumference was measured using different methods in each survey but was adjusted accordingly based on previously published comparisons (5). BMI (measured as kilograms divided by the square of height in meters) was calculated from measured body weight and height. In both studies, a 75-g OGTT was undertaken. Blood was collected after an overnight fast of ≥8 h. Specimens for glucose were collected into fluoride/oxalate tubes, and glucose was assayed onsite using a YSI glucose analyzer (YSI, Yellow Springs, OH) instrument at both surveys. Glucose tolerance status was determined according to 1999 World Health Organization criteria (6). In 1987, blood pressure was measured with a standard mercury sphygmomanometer, while in 2009, blood pressure was measured using an automated blood pressure monitor (Omron Digital Auto Blood Pressure Monitor SEM-1).
Participants reporting a history of diabetes and using insulin or hypoglycemia medication or with FPG or 2hrPG in the diabetes range were defined as having diabetes. Diabetes case subjects almost exclusively had type 2 diabetes (7). For others, FPG <7.0 mmol/L and 2hrPG ≥7.8 but <11.1 mmol/L indicated impaired glucose tolerance (IGT), FPG 6.1–6.9 mmol/L and 2hrPG <7.8 mmol/L indicated impaired fasting glucose (IFG), and both FPG <6.1 mmol/L and 2hrPG <7.8 mmol/L indicated normal glucose tolerance. Hypertension was defined as mean systolic blood pressure ≥140 mmHg, mean diastolic blood pressure ≥90 mmHg, or treatment with antihypertensive medication.
In 1987 and 2009, similar interview-administered questionnaires were conducted to collect demographic, lifestyle, and medical history information including smoking, ethnicity, and family history of diabetes (first-degree family members with diabetes). Smoking was classified as current smokers, ex-smokers, or nonsmokers. Habitual physical activity was collected by different questionnaires in 1987 and 2009. In 1987, leisure and occupational physical activity was categorized on a four-level scale using questions developed specifically for the survey: sedentary (housebound), light (gardening and walking), moderate (e.g., aerobic activity 1–2 days per week), and heavy (e.g., aerobic activity ≥3 days per week), based on usual patterns over past years. In 2009, the General Physical Activity Questionnaire (8), which has been validated in an Indian population, was used to collect information about habitual physical activity. Because the measurement of physical activity was different at the two points, we applied a conservative approach to categorize 2009 participants into equivalent 1987 physical activity level categories. In brief, if participants in 2009 reported doing vigorous heavy physical activity for ≥3 days per week, they were categorized under the category “heavy” levels of physical activity and those reporting vigorous activity 1–2 days per week were categorized into the moderate level category. The remaining participants were classified into a combined category of sedentary and light physical activity.
Statistical analyses
Datasets from 1987 and 2009 were pooled for these analyses. Changes in the distribution of FPG and 2hrPG between surveys were illustrated by Tukey mean difference plots (9). In these plots, the difference between mean plasma glucose in the corresponding 12 quantiles of the two different surveys is plotted against the mean of the combined quantiles. Quantiles of 2hrPG that were outliers were excluded. To create the 12 quantiles, we used 2.5 and 97.5 percentiles as cut points to define the lowest and highest groups. The remaining population was divided into 10 groups with equal numbers. Polytomous multinominal logistic regression was used to test whether the glucose distributions were statistically different between the two surveys. For this, the 12 groups were created in the same way but all survey data were combined. These groups were used as the dependent outcome variable, and the effect of the year of survey was examined in crude models (year of survey only), followed by models adjusted by age, sex, ethnicity, waist circumference, hypertension, physical activity (occupational and leisure), and smoking.
Diabetes prevalence of both surveys was age and sex standardized to the 2008 population of Mauritius aged 22–74 years. Change in diabetes prevalence between the two cohorts was analyzed by logistic regression with diabetes status as the dependent outcome and year of survey as the independent outcome. The odds ratio (OR) of year of survey was computed in a crude model and after adjustment for the covariates as listed in the Tables.
To account for the clustered sampling design of the surveys, we used survey commands in the analyses. Stata (version 11.2; StataCorp, College Station, TX) was used for all analyses.
RESULTS
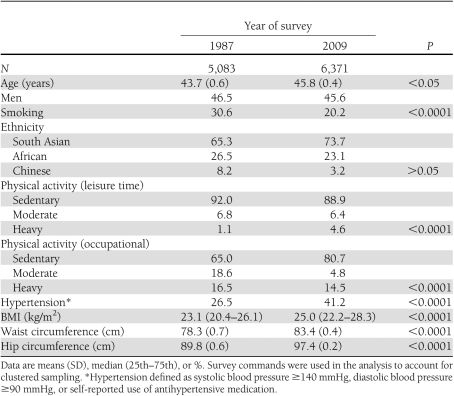
Table 1 shows that in 2009, participants had significantly larger BMI and waist and hip circumferences than in 1987 and were significantly older than in 1987. They were also significantly less likely to smoke but were more likely to have hypertension and to undertake leisure-time physical activity, though less likely to undertake physical activity at work.
Table 1.
Characteristics of survey populations in Mauritius
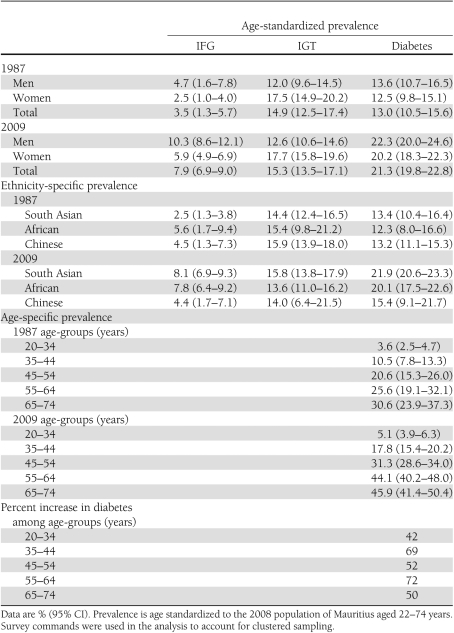
The age-standardized prevalence of diabetes, IGT, and IFG and by age group is shown in Table 2. Between 1987 and 2009, the prevalence of diabetes increased by 64%, of IGT by 3%, and of IFG by 126%. Diabetes prevalence increased by ~64% in South Asians, ~63% in Africans, and ~17% in Chinese. IGT prevalence increased by 10% in South Asians and decreased by 12% in Africans and Chinese. The prevalence of IFG increase by 224% in South Asians and 39% in Africans and decreased by 2% in Chinese. The prevalence of diabetes significantly increased from 1987 to 2009 in all age groups except for those aged <34 years (Table 2).
Table 2.
Prevalence of categories of abnormal glucose tolerance according to age-group and ethnicity
When 2hrPG was categorized into <7.8, 7.8–11.0, and ≥11.1 mmol/L independent of FPG, the proportion of those in the middle and upper groups increased between the two surveys by 19.5 and 14.4%, respectively. When FPG was categorized into <6.1, 6.1–6.9, and ≥7.0 mmol/L, the proportion in the middle and upper groups increased by 82 and 105%, respectively.
Among those with diabetes in both surveys, 14 and 35% were diagnosed, respectively, by their FPG and 2hrPG values only in 1987. In 2009, 22 and 28% were diagnosed by their FPG and 2hrPG only.
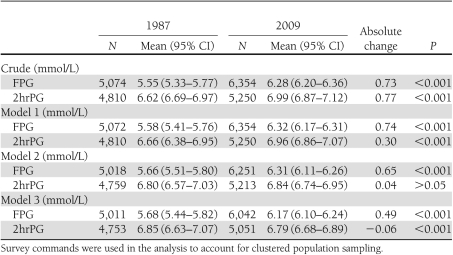
The geometric means of FPG and 2hrPG were significantly higher in 2009 than in 1987 after adjustment for age, sex, ethnicity, and waist circumference. With further adjustment for physical activity (leisure and occupational), smoking, and hypertension, mean FPG and 2hrPG remained significantly higher in 2009 than in 1987 but mean 2hrPG was slightly higher in 1987 than in 2009 (P < 0.001) (Table 3).
Table 3.
Geometric means and absolute changes in FPG and 2hrPG among Mauritian adults
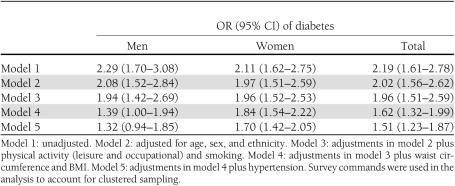
Table 4 shows a series of logistic regression models that are adjusted with demographic, lifestyle, and biological risk factors to examine which of these groups of variables could explain the increase in prevalence of diabetes from 1987 to 2009. The ORs for diabetes were attenuated after the addition of demographic factors (model 2) and lifestyle-based factors (model 3). Adjusting for waist circumference and BMI attenuated the difference further (model 4), as did the addition of hypertension (model 5). The addition of family history of diabetes completely explained the difference in diabetes prevalence in the total population (OR 1.11 [95% CI 0.99–1.25]) and in men (1.03 [0.86–1.22]) but not in women (1.32 [1.13–1.55]).
Table 4.
ORs of having diabetes in 2009 compared with 1987
Supplementary Figure 1 (available in the Supplementary Data) shows that FPG and 2hPG rose at all levels of blood glucose between 1987 and 2009. For FPG, the increase was greater at higher levels of blood glucose. With the use of crude polytomous multinominal logistic regression with FPG in 12 groups, this differential increase was significant for each of the 12 groups (P < 0.001). When these models were adjusted for age, sex, ethnicity, waist circumference, hypertension, smoking, and family history of diabetes, the difference in distributions remained significant. Similar patterns were observed in men and women (data not shown). For 2hrPG, the rises were similar across the glucose distribution. In multinominal regression, the shift in glucose between years was significant for each of the 12 groups in crude models and remained significant after adjustment for sex, ethnicity, waist circumference, hypertension, smoking, and family history of diabetes (P < 0.001). Similar patterns were observed in men and women (data not shown).
CONCLUSIONS
Our analyses show that diabetes prevalence has increased by 64% over 22 years in Mauritius. The increase was similar in men and women. The prevalence of IGT was relatively stable over the 22 years, while the prevalence of IFG increased by over 100%. The increase can be fully explained in men, but not in women, by a combination of differences in age distribution and modifiable (lifestyle) factors. The increase in diabetes prevalence is accompanied by significant increases in means of FPG and 2hrPG affecting the whole population, with a greater increase in FPG seen at the upper end of the FPG distribution.
The distribution of ethnicities in Mauritius reflects approximately two-thirds of the world population. Thus, epidemiological data from this nation’s population provides a global perspective and will be relevant in many settings.
The findings suggest that the majority of the change in prevalence is due to modifiable factors and is not due to selection bias, diagnostic bias, or change in mortality rates. The change in prevalence is unlikely due to selection bias for several reasons. Both surveys were sampled across randomly selected clusters with excellent response rates and similar survey methods. Diabetes prevalence most likely has not risen as a result of declining mortality rates because the increase in diabetes prevalence in younger ages (35–44 years), in which mortality has not changed significantly over time, was 68%.
We have shown that age and modifiable (lifestyle based) risk factors are responsible for all of the increase in diabetes prevalence in men and most of the increase in women. The greatest contributory factors were obesity and family history of diabetes. We cannot be certain, however, of precisely what information is captured by family history of diabetes. While it captures genetic risk of diabetes, family history probably represents more than this. One may argue that since diabetes was more common in 2009 than in 1987, family history of diabetes collected in 2009 could simply reflect this and therefore may be inappropriate to include as an explanatory variable. However, we believe that family history of diabetes may also be a good surrogate for measuring lifestyle and cultural factors such as diet. We were unable to directly measure the effect of a changing diet because methods were not directly comparable across the two surveys.
In 2010, Mauritius had the fourth highest prevalence of diabetes in the world (1). We show that diabetes prevalence increased by 64 and 62% among men and women, respectively, over 22 years. This increase was observed in those of South Asian and African descent but was much smaller in Chinese. Other studies describing an increase in diabetes prevalence over time are limited. A study of 60-year-old Danes showed that diabetes prevalence had increased by 38% over 22 years (10). The authors attribute all of the difference to a concurrent increase in BMI. The increase in diabetes prevalence in our study is higher than that reported in the total population of the Danish study, but the estimate of increase in diabetes prevalence was similar in men. There are some key differences between populations in both studies in terms of age range and ethnicity that prevent close comparisons. Unlike the Danish study, our study shows that the increase in diabetes over time was not due to concurrent increases in obesity alone. Our reports are similar to the change in prevalence observed in the U.S. using National Health and Nutrition Examination Survey (NHANES) data, which showed an increase in prevalence of diabetes of 51% over the period of 1988–1994 to 2005–2006 (11). More recently, a study in Scotland showed an increase of 80% in diabetes prevalence over the period of 2003–2008 (12).
The relative stability of the prevalence of IGT over time observed in this survey is consistent with our previous work in Mauritius documenting changes between 1987 and 1998. However, our findings of a doubling (and greater in some ethnicities) in the prevalence of IFG are not consistent with previous findings in Mauritius or in other countries. Using NHANES data, Cowie et al. (11) showed that the prevalence of IGT and the prevalence of IFG were relatively stable between 1988–1994 and 2005–2006.
We also found that although both 2hrPG and FPG increased over the time period, FPG increased more than 2hrPG and more participants developed diabetes via their FPG value versus their 2hrPG value. This is consistent with the hypothesis that obesity is more related to FPG than to 2hrPG (J. Tuomilehto et al., unpublished data). When 2hrPG and FPG glucose were examined in categories independent of each other, we found that the increase in the proportion of those in the IFG classes of 6.1–6.9 and ≥7.0 mmol/L was much larger than the increase in the proportion in the categories 7.8–11.1 and ≥11.1 mmol/L.
We were also able to explore the changing distribution of both FPG and 2hrPG. For both FPG and 2hrPG, all parts of the distribution showed increases in plasma glucose. The magnitude of the increase in glucose was larger at the upper than at the lower part of the glucose distribution. This was more obvious in the FPG distribution and less so with the 2hrPG distribution.
This study is not without limitations. Given the different instruments used to collect physical activity information, we were only able to account for physical activity using a crude method. This may have introduced some misclassification of physical activity status. Further, we were not able to assess the impact of changing dietary patterns on the increase in diabetes prevalence. Furthermore, we cannot rule out that the use of two different methods to measure blood pressure in the two surveys may have influenced our results.
The projections of diabetes for the coming years are modeled on expected changes in demographics and do not consider changes in modifiable risk factors such as obesity (1). Since much of the increase in diabetes prevalence can be explained by lifestyle factors, it is likely that these projections are an underestimate. The sheer magnitude of the increases in diabetes in 2009 in Mauritius portends a bleak future for Mauritians in terms of diabetes complications, associated disorders, and the costs of diabetes-related health care.
Acknowledgments
The 1987 survey was funded by the World Health Organization, Baker IDI Heart and Diabetes Institute, the University of Newcastle upon Tyne (Newcastle upon Tyne, U.K.), and the National Public Health Institute (Helsinki, Finland) and by National Institutes of Health Grant DK-25446. The 2009 survey was funded by the Ministry of Health and Quality of Life in Mauritius. S.S. is supported by grants from the Västerbotten County Council and the Swedish Heart and Lung Foundation. J.E.S. is supported by a National Health and Medical Research Council fellowship (586623). D.J.M. is supported by the Victorian Cancer Agency Public Health Fellowship.
No potential conflicts of interest relevant to this article were reported.
D.J.M. analyzed data, wrote the manuscript, and is the guarantor of this work. S.S., P.Z.Z., L.C., S.K., V.P., J.T., K.G.M.M.A., and J.E.S. reviewed and edited the manuscript. N.J., J.L., and D.G. collected and reviewed data.
We are most grateful to the Ministry of Health and Quality of Life in Mauritius for conducting both the baseline and the follow-up study. We also thank the participants for volunteering their time to be involved in the study. We also acknowledge Associate Professor Beverley Balkau from the Centre for Research in Epidemiology and Public Health, INSERM, for her statistical review of this work.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-0886/-/DC1.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Cheng YJ, Kahn HS, Gregg EW, Imperatore G, Geiss LS. Recent population changes in HbA(1c) and fasting insulin concentrations among US adults with preserved glucose homeostasis. Diabetologia 2010;53:1890–1893 [DOI] [PubMed] [Google Scholar]
- 3.Söderberg S, Zimmet P, Tuomilehto J, et al. High incidence of type 2 diabetes and increasing conversion rates from impaired fasting glucose and impaired glucose tolerance to diabetes in Mauritius. J Intern Med 2004;256:37–47 [DOI] [PubMed] [Google Scholar]
- 4.Söderberg S, Zimmet P, Tuomilehto J, et al. Increasing prevalence of type 2 diabetes mellitus in all ethnic groups in Mauritius. Diabet Med 2005;22:61–68 [DOI] [PubMed] [Google Scholar]
- 5.Wang J. Standardization of waist circumference reference data. Am J Clin Nutr 2006;83:3–4 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Diagnosis and Classification of Diabetes Mellitus and Its Complications. Part 1. Diagnosis and Classification of Diabetes Mellitus. Geneva, World Health Organization, 1999. (Tech. Rep. Ser., no. 99.2) [Google Scholar]
- 7.Tuomilehto J, Dabee J, Karvonen M, et al. Incidence of IDDM in Mauritian children and adolescents from 1986 to 1990. Diabetes Care 1993;16:1588–1591 [DOI] [PubMed] [Google Scholar]
- 8.Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health 2009;6:790–804 [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. Int J Obes Relat Metab Disord 2000;24:807–818 [DOI] [PubMed] [Google Scholar]
- 10.Drivsholm T, Ibsen H, Schroll M, Davidsen M, Borch-Johnsen K. Increasing prevalence of diabetes mellitus and impaired glucose tolerance among 60-year-old Danes. Diabet Med 2001;18:126–132 [DOI] [PubMed] [Google Scholar]
- 11.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamer M, Kengne AP, Batty GD, Cooke D, Stamatakis E. Temporal trends in diabetes prevalence and key diabetes risk factors in Scotland, 2003-2008. Diabet Med 2011;28:595–598 [DOI] [PubMed] [Google Scholar]