Abstract
OBJECTIVE
Our aim was to assess whether severe hypoglycemic attacks were cross-sectionally associated with abnormalities of the QTc interval in type 1 diabetic patients.
RESEARCH DESIGN AND METHODS
The study included 3,248 type 1 diabetic patients from the EURODIAB IDDM Complications Study. Severe hypoglycemia was defined as an attack serious enough to require the help of another person. A corrected QTc interval (QTc) >0.44 s was considered abnormally prolonged.
RESULTS
Nineteen percent of patients declared one to two attacks, and 13.2% of patients had three or more attacks. Prevalence of QTc prolongation was greater in patients who experienced three or more hypoglycemic attacks. Logistic regression analysis showed that the frequency of severe hypoglycemia was independently associated with QTc prolongation, even after adjustment for diabetes complications, including autonomic neuropathy (odds ratio 1.27, 95% CI 1.02–1.58).
CONCLUSIONS
We have provided evidence that severe hypoglycemic attacks are independently associated with a prolonged QTc interval in type 1 diabetic patients from the EURODIAB IDDM Complications Study.
Intensive glucose control increases the risk of severe hypoglycemia, and in the Diabetes Control and Complications Trial severe hypoglycemic episodes requiring assistance affected approximately one third of the intensively treated patients (1). Prolonged corrected QTc interval (QTc) reflects abnormalities of ventricular myocardial repolarization and is an independent marker of increased mortality in patients with type 1 diabetes (2). Physiologic and clinical studies have shown that provoked and spontaneous hypoglycemia induces QT lengthening (3,4). In the EURODIAB cohort, hypoglycemia was independently associated with autonomic neuropathy (5), which is common in patients with type 1 diabetes with prolonged QTc (6); however, the relationship between hypoglycemia and QTc prolongation was not explored. The aim of the current study was to assess whether severe hypoglycemic attacks were cross-sectionally associated with QTc abnormalities in this cohort.
RESEARCH DESIGN AND METHODS
The EURODIAB IDDM Complications Study is a clinic-based study designed to explore risk factors for diabetes complications (7,8). The local ethics committees approved this study at each center, and all persons provided written informed consent.
Definitions of severe hypoglycemia were based on information obtained from a questionnaire completed by recruited subjects. All patients were asked “Over the past year, how many hypoglycemic attacks have you had, serious enough to require the help of another person?” The questionnaire also provided information on physical activity, smoking habits, frequency of insulin injections, and number of daily insulin units injected per kilogram of body weight (5,7).
Hypertension, retinopathy, microalbuminuria, macroalbuminuria, and cardiovascular disease (CVD) were assessed and defined as previously described (7,8). Glomerular filtration rate (GFR) was estimated using the four-component abbreviated equation from the Modification of Diet in Renal Disease study (9). Subjects with an estimated GFR <60 mL/min/1.73 m2 were defined as having chronic kidney disease.
Distal symmetrical polyneuropathy (DSP) was assessed on the basis of neuropathic symptoms and signs, including measurement of vibration perception threshold (10). Autonomic neuropathy was defined as a loss of heart rate variability with an R-R ratio <1.04 or postural hypotension with a decrease in systolic blood pressure of ≥20 mmHg (10,11).
RR and QT intervals were measured blindly by two observers on the resting electrocardiogram tracing, using five consecutive beats on lead V5. The QTc for the previous cardiac cycle length was calculated according to Bazett’s equation (12). QTc >0.44 s was considered abnormally prolonged. RR and QT intervals were also measured for three consecutive cardiac cycles on the six thoracic leads. The dispersion of QTc was calculated using the difference between the maximal and the minimal QTc (QTd) in any thoracic leads. A QTd >0.080 s was considered abnormally increased (10).
Data were expressed as the mean and SD. Variables with skewed distributions were logarithmically transformed for statistical analysis. Group differences were tested by ANOVA or Pearson χ2 test, as appropriate. All variables were included in a logistic regression analysis and retained in the final model if they added significantly to the likelihood of models or to the estimated coefficients of predictors, as assessed using the –2 log likelihood ratio test. The analysis was hypothesis-oriented and did not use stepwise selection of variables (13). P value of less than 0.05 was considered to indicate statistical significance. Analyses were performed with Stata (Stata Release 10.0, StataCorp LP, College Station, TX).
RESULTS
Of the 3,250 patients recruited at baseline, response data on severe hypoglycemic episodes were available for 3,248 subjects (99.9%). At the baseline examination, 2,202 patients (68%) declared no severe hypoglycemic attacks over the past year (H0), 618 patients (19%) declared one to two attacks (group H1-2), and 428 patients (13.2%) declared three or more attacks (H3). As previously reported (7), the latter group of patients was older, had longer diabetes duration, and had lower mean HbA1c levels.
Estimated GFR values were lower in patients declaring hypoglycemic episodes (H0: 120.1 ± 53.6; [H1-2]: 113.9 ± 30.1; H3: 106.7 ± 34.3; P = 0.02). Prevalence of hypertension (H0: 22.7%; [H1-2]: 25.7%; H3: 30.8%; P = 0.001), CVD (H0: 9.4%; [H1-2]: 8.4%; H3: 13.2%; P = 0.02), nonproliferative/proliferative retinopathy (H0: 44.7%; [H1-2]: 46.3%; H3: 54.6%; P = 0.007), DSP (H0: 34.3%; 1H–2: 36.9%; H3: 44.6%; P < 0.0001), and QTc prolongation (H0: 14.8%; [H1-2]: 16.9%; H3: 19.3%; P = 0.05) was greater in patients who experienced three or more hypoglycemic attacks. No significant differences were observed in the prevalence of prolonged QTd (H0: 6.3%; [group H1-2]: 7.3%; H3: 8.5%; P = 0.27).
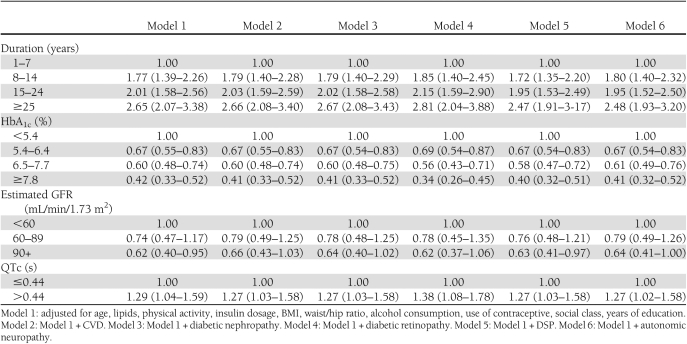
Logistic regression analysis showed that the frequency of severe hypoglycemia was associated with longer diabetes duration, lower HbA1c, chronic renal disease, and QTc prolongation independently of confounders, as shown in Table 1 (Model 1). The relation between prolonged QTc and frequency of severe hypoglycemia was independent of diabetic macro/microvascular complications. Indeed, as shown in Table 1 (Models 2–6), the association remained significant even after further adjustment for CVD (odds ratio [OR] 1.27 [95% CI 1.01–1.58]), diabetic nephropathy (1.27 [ 1.03–1.58]), diabetic retinopathy (1.38 [1.08–1.78]), DSP (1.27 [1.01–1.58]), and autonomic neuropathy (1.27 [95% CI 1.02–1.58]).
Table 1.
Odds ratio for severe hypoglycemic attacks in the EURODIAB IDDM Complications Study
CONCLUSIONS
Previous small physiologic and clinical studies have reported that provoked/spontaneous hypoglycemia can induce QT prolongation (3,4). However, this issue has never been explored in large series, and our data provide the first evidence of an independent association between hypoglycemia and QTc prolongation in a large epidemiologic study on type 1 diabetes. This finding is of clinical relevance because in type 1 diabetes, the so-called dead in bed syndrome has been related to nocturnal hypoglycemia leading to QT prolongation followed by ventricular tachyarrhythmia (3,14).
Autonomic neuropathy itself can be associated with QTc lengthening (5), and a recent study has found QTc prolongation to be common in adolescents with type 1 diabetes with early autonomic dysfunction (15). Furthermore, in the EURODIAB cohort, autonomic neuropathy was independently associated with severe hypoglycemia (5). Nonetheless, the relationship between prolonged QTc and hypoglycemia was not mediated by autonomic neuropathy in the current study.
The lack of serum electrolyte measures in the EURODIAB study may limit the interpretation of results. However, the sample of patients is relatively young; therefore, the percentage of patients with electrolyte disturbances or taking drugs potentially interfering with QT duration is likely to be small and to have little impact on our findings. On the other hand, lowering of serum potassium is known to augment the arrhythmogenic effect of QT prolongation and may expose patients with type 1 diabetes with frequent severe hypoglycemic episodes and prolonged QTc to a higher risk of ventricular tachyarrhythmia and sudden death. Our results are based on self-reports of severe hypoglycemia; however, any potential misclassification was randomly distributed; thus, it is unlikely to affect observed significant associations.
Acknowledgments
This work was supported by the Compagnia di San Paolo, the University of Turin, the European Community, and the Wellcome Trust.
No potential conflicts of interest relevant to this article were reported.
G.G. and G.B. researched data, wrote the manuscript, and are the guarantors for the article. S.G. wrote the manuscript. F.B. reviewed and edited the manuscript. N.C. researched data and reviewed and edited the manuscript. D.R.W. researched data. M.T. reviewed and edited the manuscript. J.H.F. and P.C.P. contributed to discussion.
The authors thank all the investigators and patients who took part.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1739/-/DC1.
A complete list of investigators can be found in the Supplementary Data online.
References
- 1.The Diabetes Control and Complications Trial Research Group Hypoglycemia in the Diabetes Control and Complications Trial. Diabetes 1997;46:271–286 [PubMed] [Google Scholar]
- 2.Rossing P, Breum L, Major-Pedersen A, et al. Prolonged QTc interval predicts mortality in patients with Type 1 diabetes mellitus. Diabet Med 2001;18:199–205 [DOI] [PubMed] [Google Scholar]
- 3.Gill GV, Woodward A, Casson IF, Weston PJ. Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes—the ‘dead in bed’ syndrome revisited. Diabetologia 2009;52:42–45 [DOI] [PubMed] [Google Scholar]
- 4.Marques JL, George E, Peacey SR, et al. Altered ventricular repolarization during hypoglycaemia in patients with diabetes. Diabet Med 1997;14:648–654 [DOI] [PubMed] [Google Scholar]
- 5.Stephenson JM, Kempler P, Perin PC, Fuller JH. Is autonomic neuropathy a risk factor for severe hypoglycaemia? The EURODIAB IDDM Complications Study. Diabetologia 1996;39:1372–1376 [DOI] [PubMed] [Google Scholar]
- 6.Weston PJ, Gill GV. Is undetected autonomic dysfunction responsible for sudden death in Type 1 diabetes mellitus? The ‘dead in bed’ syndrome revisited. Diabet Med 1999;16:626–631 [DOI] [PubMed] [Google Scholar]
- 7.Stephenson J, Fuller JH. Microvascular and acute complications in IDDM patients: the EURODIAB IDDM Complications Study. Diabetologia 1994;37:278–285 [DOI] [PubMed] [Google Scholar]
- 8.Koivisto VA, Stevens LK, Mattock M, et al. ; EURODIAB IDDM Complications Study Group Cardiovascular disease and its risk factors in IDDM in Europe. Diabetes Care 1996;19:689–697 [DOI] [PubMed] [Google Scholar]
- 9.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D; Modification of Diet in Renal Disease Study Group A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999;130:461–470 [DOI] [PubMed] [Google Scholar]
- 10.Veglio M, Giunti S, Stevens LK, Fuller JH, Perin PC; EURODIAB IDDM Complications Study Group Prevalence of Q-T interval dispersion in type 1 diabetes and its relation with cardiac ischemia: the EURODIAB IDDM Complications Study Group. Diabetes Care 2002;25:702–707 [DOI] [PubMed] [Google Scholar]
- 11.Tesfaye S, Stevens LK, Stephenson JM, et al. Prevalence of diabetic peripheral neuropathy and its relation to glycaemic control and potential risk factors: the EURODIAB IDDM Complications Study. Diabetologia 1996;39:1377–1384 [DOI] [PubMed] [Google Scholar]
- 12.Bazett HC. An analysis of the time relations of electrocardiograms. Heart 1920;7:353–370 [Google Scholar]
- 13.Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 1998 [Google Scholar]
- 14.Tattersall RB, Gill GV. Unexplained deaths of type 1 diabetic patients. Diabet Med 1991;8:49–58 [DOI] [PubMed] [Google Scholar]
- 15.Karavanaki K, Kazianis G, Kakleas K, Konstantopoulos I, Karayianni C. QT interval prolongation in association with impaired circadian variation of blood pressure and heart rate in adolescents with Type 1 diabetes. Diabet Med 2007;24:1247–1253 [DOI] [PubMed] [Google Scholar]