Abstract
OBJECTIVE
To examine whether combined lifestyle behaviors have an impact on all-cause and cause-specific mortality in patients aged 30–94 years with type 2 diabetes (T2DM).
RESEARCH DESIGN AND METHODS
Participants included 5,686 patients >30 years old with T2DM who were enrolled in a Diabetes Care Management Program at a medical center in central Taiwan before 2007. Lifestyle behaviors consisted of smoking, alcohol drinking, physical inactivity, and carbohydrate intake. The main outcomes were all-cause and cause-specific mortality. Cox proportional hazards models were used to examine the association between combined lifestyle behaviors and mortality.
RESULTS
The mortality rate among men was 24.10 per 1,000 person-years, and that among women was 17.25 per 1,000 person-years. After adjusting for the traditional risk factors, we found that combined lifestyle behavior was independently associated with all-cause mortality and mortality due to diabetes, cardiovascular disease, and cancer. Patients with three or more points were at a 3.50-fold greater risk of all-cause mortality (95% CI 2.06–5.96) and a 4.94-fold (1.62–15.06), 4.24-fold (1.20–14.95), and 1.31-fold (0.39–4.41) greater risk of diabetes-specific, CVD-specific, and cancer-specific mortality, respectively, compared with patients with zero points. Among these associations, the combined lifestyle behavior was not significantly associated with cancer mortality.
CONCLUSIONS
Combined lifestyle behavior is a strong predictor of all-cause and cause-specific mortality in patients with T2DM.
Type 2 diabetes (T2DM) and its complications are leading causes of premature mortality, imposing a heavy burden at the individual and societal level (1,2). With the Westernization of diet behaviors, the prevalence of T2DM has increased dramatically in Taiwan. The National Nutrition Survey in Taiwan revealed that the prevalence of T2DM among men aged ≥65 years had increased dramatically: from 13.1 to 17.6 to 28.5% in 1993–1996, 2002, and 2005–2008, respectively (3). The International Diabetes Federation (2) proposed that the causes of the increase in diabetes prevalence were population aging and unhealthy lifestyle behaviors. The components of these unhealthy lifestyle behaviors included being physically inactive, smoking, alcohol drinking, and having an unhealthy diet (4–6).
T2DM is also an important cause of microvascular and macrovascular diseases. Lifestyle modifications in conjunction with antidiabetes medications can prevent premature morbidity and mortality (5,7). However, for individuals with diabetes, the most difficult task is to strike a balance between the individual’s desires and compliance with behavior modification for disease management. It has been reported that individuals with diabetes who practice healthy lifestyle behaviors have better glycemic control (8) and that better glycemic control is associated with lower mortality (9). Although the effects of these individual or combined lifestyle behaviors on mortality have been well studied in general populations (10–18), little is known about the association between these lifestyle behaviors and mortality in patients with T2DM (5,19). Understanding the relationships of these modifiable predictors on mortality in patients with T2DM will have great clinical significance for diabetes care.
The Taichung Diabetes Study is a population-based cohort study of ~6,000 middle-aged and older ethnic Chinese patients with T2DM who enrolled in the Diabetes Care Management Program (DCMP) of a medical center in Taiwan. The DCMP provides financial incentives for physicians to increase exhaustive follow-up visits, including annual self-care education and assessment by care managers and a clinical nutrition practitioner, annual eye examinations, and four annual laboratory tests. The DCMP provided a unique opportunity to quantify the overall impact of lifestyle factors, including smoking, alcohol drinking, regular exercise, and carbohydrate intake, on mortality. The purpose of this study was to fill this gap in knowledge by investigating the prospective associations among lifestyle factors and all-cause, diabetes-, cardiovascular disease (CVD)-, and cancer-specific mortality, independently of HbA1c, and several baseline traditional factors, in a large cohort of ethnic Chinese patients with T2DM who were followed up for more than 4 years.
RESEARCH DESIGN AND METHODS
Patients with T2DM were selected from among all participants in the DCMP at China Medical University Hospital (CMUH), a medical center in Taichung, Taiwan. The DCMP is a nurse case-management program established by the Taiwan Bureau of National Health Insurance in 2002. All patients with a clinically confirmed diagnosis of T2DM, based on the criteria of the American Diabetes Association (ICD-9-CM, diagnosis code 250), were invited to participate. At the time of entering the DCMP, enrollees underwent a series of blood tests, urine tests, and body measurements. In addition, participants were required to complete a standardized, computerized questionnaire administered by a case-management nurse to record previous or current disease status as well as lifestyle behaviors. All patients had to go through a nutrition education program with a clinical nutrition practitioner, and their 24-h recall-based diet report was taken during the nutrition education program. Patients with type 1 diabetes (ICD-9-CM, code 250.x1/x3) were excluded.
Participants who were enrolled in the DCMP before the end of August 2007 were identified from an automated registry. There were 9,936 patients with diabetes identified in the dataset. All identified patients who had been continuously enrolled in the program until August 2008 or until death were included. Patients with <1 year of follow-up were excluded. A total of 1,818 patients were excluded. The rationale for those criteria was that we needed patients who could provide at least 1 year of follow-up in order to exclude deaths occurring in the first year of follow-up and avoid potential bias due to the existence of disease. After we excluded those who had missing data for any variables considered in the study, 5,686 patients with T2DM were included in the analysis.
Lifestyle-related factors
Data from baseline information were retrieved from the DCMP database to assess the lifestyle factors of interest. The lifestyle scores were assigned based on previous research (6,10,12,20) and age- and sex-adjusted mortality of the lifestyle behavior categories. The lifestyle behaviors of smoking, alcohol drinking, physical activity, and carbohydrate intake were each divided into two groups. The nonsmoking group included those who had never smoked, and those in the smoking group were current or past smokers. Individuals who self-reported alcohol drinking or regular exercise or not were classified into the group with this specific characteristic. “Regular” was defined as at least once per week for >1 month continuously. The high carbohydrate intake included those who had total kilocalories from carbohydrate intake ≥65% (20). The percentage of the total kilocalories from carbohydrate intake came from the 24-h food diary recording all food items an individual ate. The common unit or portion size for each food item was specified. The daily caloric intake was calculated by multiplying the amount of consumption of each item by its caloric content per serving and totaling the caloric intake for all food items. The percentage of total kilocalories from carbohydrate intake was then derived, and carbohydrate intake was further categorized according to the Acceptable Macronutrient Distribution Ranges for carbohydrate, which are 45–65%, provided by Institute of Medicine Dietary Reference Intakes for a healthy eating pattern for adults (20). The most common source of carbohydrate was rice, and next was wheat. The lifestyle score for each patient was created by assigning one point to each of the four lifestyle behaviors and then summing the accumulated points for the four factors, with a range of zero to four points. A higher score indicated an increase in lifestyle behaviors, and we hypothesized that mortality would increase as the lifestyle score increased.
Covariates
Weight and height were measured with an autoanthropometer (HW-666; Super-View), with the subjects shoeless and wearing light clothing. BMI was measured as kilograms divided by the square of height in meters. Blood was drawn with minimal trauma from an antecubital vein in the morning after a 12-h overnight fast and was sent for analysis within 4 hours of collection. Biochemical markers such as serum creatinine, fasting plasma glucose, HDL cholesterol, LDL cholesterol, and triglyceride were analyzed by a biochemical autoanalyzer (Lx-20; Beckman Coulter Synchron System, Beckman Coulter, Fullerton, CA) at the Clinical Laboratory Department of CMUH.
Outcome measures
Primary outcome measures were all-cause mortality and mortality owing to diabetes (ICD-9-CM, diagnosis code 250), CVD (ICD-9-CM, diagnosis codes 390–459), or cancer (ICD-9-CM, diagnosis codes 140–208). The Taiwan National Death Index, a database that contains records of deaths of Taiwanese citizens, was used to identify possible decedents during the follow-up period. After deaths had been identified, they were confirmed by our registry. By linking the unique identification numbers with this computerized file, we identified 429 deaths in this cohort by the end of 2008.
Statistical analyses
We used Cox proportional hazards models to evaluate the association between mortality and each lifestyle factor individually and then the lifestyle scores. We calculated adjusted hazard ratios (HRs) (95% CI) by adjusting for age, sex, and multiple variables. Linear trends were evaluated using the Wald test, with the lifestyle score treated as a continuous variable. To assess whether the estimates of the combined lifestyle behaviors on mortality were sensitive to diabetes complications, we excluded patients with stroke, CVD, diabetic ketoacidosis (DKA), and hyperglycemia hyperosmolar nonketoacidosis (HHNK) and performed a multivariate analysis. In addition, stratified analysis according to smoking status was performed to examine the effect of combined lifestyle behaviors on mortality. We examined the proportional hazards assumption, both graphically and by testing the significance of interaction terms for the lifestyle scores and years of follow-up, and found no statistically significant violation. All P values were two-tailed, and a P value <0.05 was considered statistically significant. All analyses were performed with the SAS statistical package for Windows (version 9.1; SAS, Cary, NC).
RESULTS
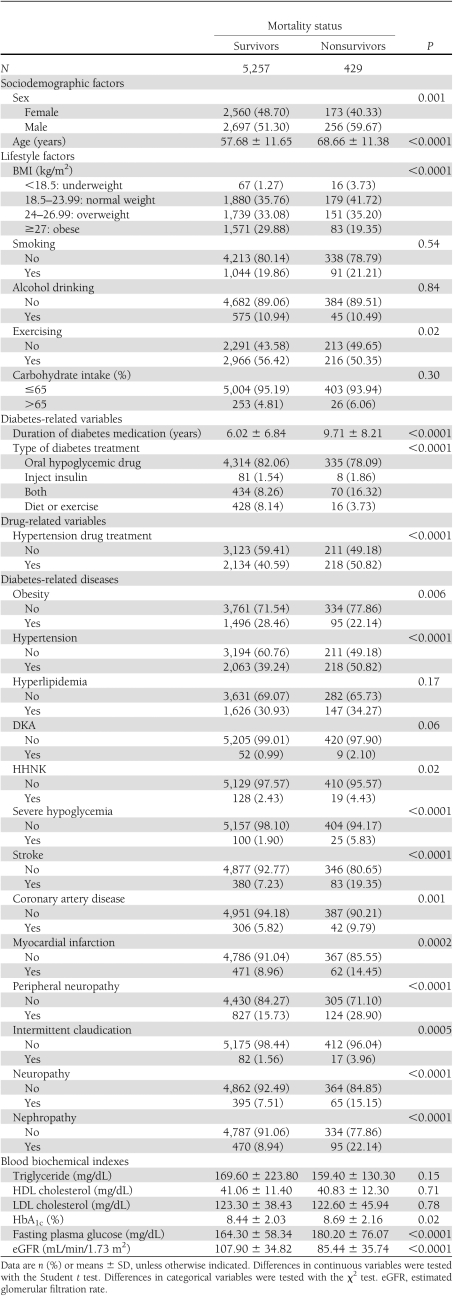
The median follow-up was 4.02 years, and 429 of the 5,686 patients died during this period. The crude mortality rate was 20.77 per 1,000 person-years (24.10 and 17.25 per 1,000 person-years for men and women, respectively). Cancer was the leading cause of death (n = 122; crude rate 5.91 per 1,000 person-years), followed by diabetes (n = 105; crude rate 5.08 per 1,000 person-years) and CVD (n = 83; crude rate 4.02 per 1,000 person-years). Altogether, these causes accounted for 72.26% of all deaths. For cancer prevalence, liver was the leading cause of cancer mortality (n = 29), followed by colon (n = 17) and lung (n = 15). Altogether, these cases accounted for 50.00% of all cancer deaths. Table 1 shows the comparisons of baseline sociodemographic factors, lifestyle behaviors, diabetes-related variables, drug-related variables, diabetes-related diseases, and blood biochemical indexes between survivors and nonsurvivors with T2DM enrolled in the DCMP at CMUH.
Table 1.
Comparisons of baseline sociodemographic factors, lifestyle behaviors, diabetes-related variables, drug-related variables, diabetes-related diseases, and blood biochemical indexes between survivors and nonsurvivors with T2DM enrolled in the DCMP at CMUH (n = 5,686)
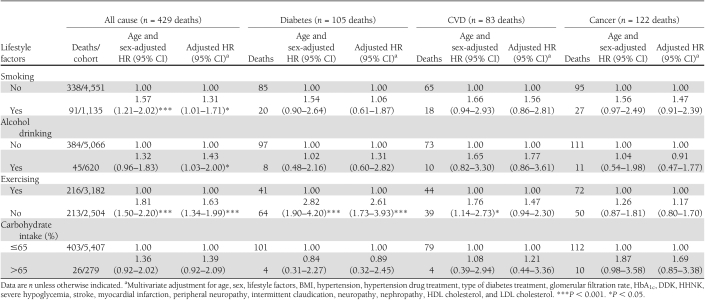
Table 2 shows the HRs for each of the four lifestyle behaviors with all-cause and cause-specific mortality. With multivariate adjustment for all other lifestyle behaviors and comorbidities, all individual lifestyle behaviors were significant for all-cause mortality except carbohydrate intake. The patterns of associations for physical inactivity were comparable with total mortality for deaths from diabetes. The HRs of CVD- or cancer-specific mortality for all individual lifestyle behaviors were generally absent.
Table 2.
Adjusted HRs for lifestyle-related factors and risk of all-cause, diabetes, cardiovascular, and cancer mortality in diabetic patients enrolled in the DCMP of a medical center (n = 5,686)
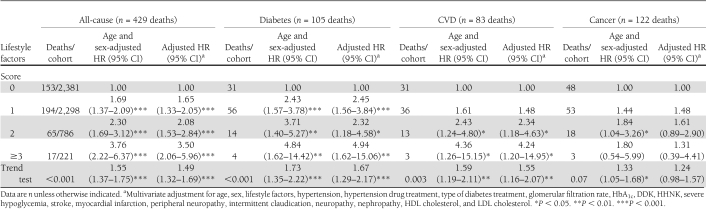
A higher lifestyle score was significantly associated with an increased risk of all-cause, diabetes-specific, CVD-specific, and cancer-specific mortality (P for trend <0.001, <0.001, 0.003, and 0.07, respectively) (Table 3). With multivariate adjustment, patients with more than three points had a 3.50-fold greater risk of all-cause mortality (95% CI 2.06–5.96), a 4.94-fold greater risk of diabetes-specific mortality (1.62–15.06), and a 4.24-fold greater risk of CVD-specific mortality (1.20–14.95), compared with patients with zero points.
Table 3.
Mortality lifestyle-related factors and risk of all-cause, diabetes, cardiovascular, and cancer mortality in diabetic patients enrolled in the DCMP of a medical center (n = 5,686)
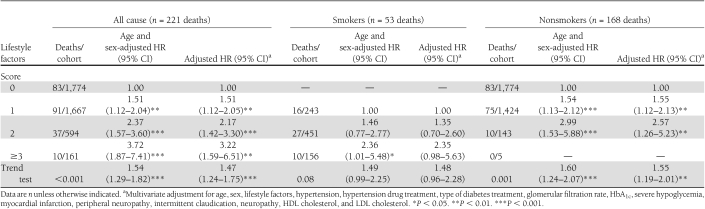
Sensitivity analyses were conducted to investigate the potential for bias due to the existence of comorbidities by excluding patients with stroke, CVD, DKA, HHNK, and nephropathy (n = 4,196) (Table 4). Similarly significant associations were found for all-cause and diabetes, CVD-, and cancer-specific mortality, although the HRs became attenuated. We also evaluated the association between all-cause mortality and a combined lifestyle score stratified by smoking status. The results in these two smoking groups were similar to the overall findings.
Table 4.
Mortality lifestyle-related factors and risk of all-cause mortality in diabetic patients enrolled in the DCMP of a medical center, excluding patients with stroke, CVD, DKA, HHNK, and nephropathy and stratified according to smoking status (n = 4,196)
CONCLUSIONS
In this population-based prospective cohort study of ethnic Chinese patients with T2DM and aged 30–94 years, we found that lifestyle-related factors—including smoking, alcohol drinking, physical inactivity, and high carbohydrate intake—were significantly and independently associated with a higher risk of all-cause and cause-specific mortality. The associations persisted when the confounding effect of clinical disease at baseline was removed by analyzing all patients without baseline comorbidities. To our knowledge, this is the first large prospective cohort study to quantify the combined impact of lifestyle-related factors, especially in relation to high carbohydrate intake, on mortality outcomes among patients with T2DM. Results showed that each individual lifestyle factor has a weak association with mortality; however, together they have a major combined impact on mortality.
In general, the literature is limited with regard to the study of combined lifestyle factors and mortality in general populations (10,12,16–18). A few studies have evaluated the effects of lifestyle intervention on glucose control (8). Little is known about the combined impact of lifestyle factors, such as active smoking, alcohol drinking, physical inactivity, and high carbohydrate intake, on mortality in patients with T2DM. The answer to this question is of particular importance, as the relationships of these lifestyle factors with mortality in patients with T2DM might be different from those in the general population. In a recent prospective cohort study of ethnic Chinese women in Shanghai who never smoked or drank alcohol regularly, the authors investigated the combined impact of normal weight, lower waist-to-hip ratio, daily exercise, total lack of exposure to spouse’s smoking, and higher daily fruit and vegetable intake. Nechuta et al. (12) showed that women with a lifestyle score of four to five had an HR of 0.57 (95% CI 0.44–0.74) for all-cause mortality and 0.29 (0.16–0.54) for CVD mortality compared with women with a score of zero. Although the individual lifestyle behaviors in this female population and in ours exerted a similar magnitude of strength of association, the effect of the highest score for these lifestyle behaviors in our study was slightly greater than that in the study of Nechuta et al.
A recent study examined whether lifestyle intervention, including physical activity, weight reduction, and dietary counseling, had an effect on 10-year mortality in middle-aged overweight people with impaired glucose tolerance (IGT) (5). The findings indicated that people in lifestyle intervention and control groups using mini-intervention had lower total mortality compared with those from a population-based cohort comprising individuals with IGT. In another quasi-experimental study with a 12-year follow-up of men with IGT, men participating in the diet and exercise intervention group experienced a lowering of overall and ischemic heart disease mortality (21). The current study adds evidence to findings that active smoking, physical inactivity, alcohol drinking, and high carbohydrate intake increase the risk of all-cause mortality and cause-specific mortality in patients with T2DM. These data support the idea that combined lifestyle behaviors may have an overall adverse impact on mortality in patients with T2DM.
Physical activity appeared to have the strongest effect on mortality among patients with diabetes. Possible contributors to the protective effect of physical activity observed in numerous epidemiologic studies included exercise-induced blood pressure lowering and improved body composition, glucose tolerance, insulin sensitivity, and platelet function (22,23). A meta-analysis showed that vigorous and moderate levels of physical activity were associated with reduced risk of coronary artery disease: 27 and 12% reductions, respectively (24).
Our findings have several clinical implications. First, lifestyle behaviors are important factors of all-cause and cause-specific mortality in patients with diabetes. Most of the lifestyle behaviors studied here may be changed by enhancing the subjects’ motivation to change through education interventions and through change in the social environment, such as the promotion of smoking bans in public settings. Second, nutritional education programs that guide patients with T2DM in maintaining a healthy diet should be designed and emphasized in diabetes care to reduce the number of premature deaths associated with higher carbohydrate intake.
Our study has several strengths, including a large number of patients with diabetes, a long follow-up period, the use of a standardized procedure for data collection, and available information on a large number of potential confounding factors. However, there are several limitations that need to be considered when interpreting our results. First, in common with other longitudinal studies, our study did not have a precise questionnaire-based assessment of physical activity, alcohol consumption, or smoking. Although the group indexing by specific characteristic should be regarded as reflecting common perceptions rather than precise measures of levels, this type of questionnaire is well suited for the care management of a larger number of patients with T2DM. Second, patients who self-reported any of these characteristics were placed into groups based on the specific characteristic. These individuals without the specific characteristic may have had these characteristics and have made changes because of their poor health, which could increase the mortality risk in the group without the specific characteristic. In addition, because these behaviors were reported at baseline, we do not know whether these practices were continued or changed during follow-up. Regardless of whether changes in these practices were related to poor health, this kind of measurement error would result in the underestimation of the effect—a lesser threat to validity. Third, despite adjustment for a large number of potential confounders, including medications and complications, residual and unrecognized confounding may be present because of the observational nature of our study. Fourth, we do not have enough power to examine the relationship between lifestyle behaviors and specific types of cancer. Finally, all patients with T2DM in this study were enrolled in a DCMP at a single medical center. They therefore may not be representative of all patients with diabetes in Taiwan. However, the lack of representativeness of our sample does not bias our results in our exploration of this analytic association.
In conclusion, we have shown that the effects of combined lifestyle behaviors led to adverse health consequences, relative to the health of those with no lifestyle behaviors, with respect to all-cause and cause-specific mortality. Mortality risk showed a dose-response relationship with the number of lifestyle behaviors. Clearly, since this was the first prospective population study to address this question, more research is needed.
Acknowledgments
This study was primarily supported by the National Science Council of Taiwan (NSC95-2314-B-039-009 and NSC97-2314-B-039-019), by China Medical University (CMU97-176), and by the Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH100-TD-B-111-004).
No potential conflicts of interest relevant to this article were reported.
C.-C.Li. and T.-C.L. developed the study design, obtained funding, drafted the manuscript, and read and approved the final manuscript. C.-I.L. and S.-Y.Y. acquired data, carried out the statistical analysis, analyzed and interpreted data, critically revised the manuscript, and read and approved the final manuscript. C.-S.L., W.-Y.L., M.M.-T.F., and C.-C.Le. contributed to discussion, reviewed and edited the manuscript, and read and approved the final manuscript.
References
- 1.National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease. National diabetes statistics: 2007 fact sheet [article online], 2008. Available from http://diabetes.niddk.nih.gov/dm/pubs/statistics Accessed 2 February 2011
- 2.International Diabetes Federation. The diabetes atlas [article online], 2006. 3rd ed. Available from http://www.eatlas.idf.org/media/ Accessed 2 February 2011
- 3.Department of Health and Executive Yuan. The prevalence of type 2 diabetes mellitus [article online], 2009. Taipei, Taiwan, Department of Health. Available from http://www.doh.gov.tw/EN2006/index_EN.aspx Accessed 2 February 2011
- 4.Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med 2009;169:798–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uusitupa M, Peltonen M, Lindström J, et al. ; Finnish Diabetes Prevention Study Group Ten-year mortality and cardiovascular morbidity in the Finnish Diabetes Prevention Study—secondary analysis of the randomized trial. PLoS ONE 2009;4:e5656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kruk J. Physical activity in the prevention of the most frequent chronic diseases: an analysis of the recent evidence. Asian Pac J Cancer Prev 2007;8:325–338 [PubMed] [Google Scholar]
- 7.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348:383–393 [DOI] [PubMed] [Google Scholar]
- 8.Ahmed AT, Karter AJ, Warton EM, Doan JU, Weisner CM. The relationship between alcohol consumption and glycemic control among patients with diabetes: the Kaiser Permanente Northern California Diabetes Registry. J Gen Intern Med 2008;23:275–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersson DK, Svärdsudd K. Long-term glycemic control relates to mortality in type II diabetes. Diabetes Care 1995;18:1534–1543 [DOI] [PubMed] [Google Scholar]
- 10.Hart CL, Davey Smith G, Gruer L, Watt GC. The combined effect of smoking tobacco and drinking alcohol on cause-specific mortality: a 30 year cohort study. BMC Public Health 2010;10:789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Savela S, Koistinen P, Tilvis RS, et al. Leisure-time physical activity, cardiovascular risk factors and mortality during a 34-year follow-up in men. Eur J Epidemiol 2010;25:619–625 [DOI] [PubMed] [Google Scholar]
- 12.Nechuta SJ, Shu XO, Li HL, Yang G, Xiang YB, Cai H, et al. Combined impact of lifestyle-related factors on total and cause-specific mortality among Chinese women: prospective cohort study. PLoS Med 2010;7:e1000339 [DOI] [PMC free article] [PubMed]
- 13.Byberg L, Melhus H, Gedeborg R, et al. Total mortality after changes in leisure time physical activity in 50 year old men: 35 year follow-up of population based cohort. BMJ 2009;338:b688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wen W, Shu XO, Gao YT, et al. Environmental tobacco smoke and mortality in Chinese women who have never smoked: prospective cohort study. BMJ 2006;333:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odegaard AO, Pereira MA, Koh WP, et al. BMI, all-cause and cause-specific mortality in Chinese Singaporean men and women: the Singapore Chinese health study. PLoS ONE 2010;5:e14000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knoops KT, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA 2004;292:1433–1439 [DOI] [PubMed] [Google Scholar]
- 17.van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ 2008;337:a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 2008;5:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu G, Eriksson J, Barengo NC, et al. Occupational, commuting, and leisure-time physical activity in relation to total and cardiovascular mortality among Finnish subjects with type 2 diabetes. Circulation 2004;110:666–673 [DOI] [PubMed] [Google Scholar]
- 20.Food and Nutrition Board, Institute of Medicine of the National Academies Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC, National Academies Press, 2002 [Google Scholar]
- 21.Eriksson KF, Lindgärde F. No excess 12-year mortality in men with impaired glucose tolerance who participated in the Malmö Preventive Trial with diet and exercise. Diabetologia 1998;41:1010–1016 [DOI] [PubMed] [Google Scholar]
- 22.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol 2003;551:673–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 2007;56:2655–2667 [DOI] [PubMed] [Google Scholar]
- 24.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil 2008;15:247–257 [DOI] [PubMed] [Google Scholar]