Abstract
Background and Objectives
Marijuana remains the most commonly used illicit substance. Marijuana craving, anxiety, and peer marijuana use are thought to play important roles in the etiology and maintenance of marijuana use. The present study aimed to identify patterns between marijuana use and these affective and situational risk factors in the natural environment.
Methods
The sample consisted of 49 current marijuana users (38.8% female), 63.2% of whom evinced a current cannabis use disorder. Ecological momentary assessment was used to collect multiple daily ratings of marijuana craving, state anxiety, and peer marijuana use over two weeks. Mixed effects linear models were used to examine within- and between-day antecedents, correlates, and consequences of marijuana use.
Results
Between-day analyses indicated that marijuana use days were associated with higher marijuana craving but lower state anxiety. Within-day analyses confirmed that marijuana craving was higher prior to marijuana use and lower following use. Anxiety was related to marijuana craving. Although anxiety was somewhat higher prior to marijuana use, it did not decrease significantly following use. The vast majority of marijuana use occurred when others were also using marijuana.
Limitations
The sample was comprised of college students, a group at particular risk for marijuana use and use-related problems. Future work is necessary to determine whether results generalize to other populations.
Conclusions
These data support the contention that marijuana craving, anxiety, and peer use play important roles in the maintenance of marijuana use.
Keywords: marijuana, cannabis, anxiety, craving, peer influence, ecological momentary assessment
1. Introduction
Marijuana is the most commonly used illicit drug (Substance Abuse and Mental Health Services Administration [SAMHSA], 2009) and more than one in four users experiences marijuana-related problems that cause such distress and/or functional impairment as to meet criteria for a cannabis use disorder (CUD; SAMHSA, 2009). The prevalence of CUD nearly equaled that of other illicit substance use disorders combined (SAMHSA, 2009). Given the prevalence of marijuana use and CUD, it is important to determine whether proximal factors that are believed to maintain marijuana use (e.g., marijuana craving, anxiety, peer use) are in fact related to use.
1.1 The Role of Marijuana Craving
Some evidence supports the notion that marijuana craving leads to use. Marijuana users report greater craving during abstinent periods compared to marijuana use periods (Budney, Hughes, Moore, & Novy, 2001) and users undergoing voluntary marijuana abstinence report greater craving than ex-users (Budney, Moore, Vandrey, & Hughes, 2003). Craving increases in response to imaginal and pictorial marijuana cues (Gray, LaRowe, & Upadhyaya, 2008; Wölfling, Flor, & Grüsser, 2008) and the administration of THC decreases marijuana craving (e.g., Haney et al., 2008). Although these data suggest that craving increase marijuana use vulnerability, little research has examined whether marijuana craving leads to marijuana use.
1.2 The Role of Anxiety
Substance use models such as tension-reduction (Conger, 1956) posit that negative affect increases risk of substance use as some individuals may chose to use substances in an effort to manage negative affective states. Anxiety is a very common type of negative affect that is systematically and uniquely related to marijuana use and use-related impairment. To illustrate, people with cannabis dependence are twice as likely to experience a co-occurring anxiety disorder compared to those without cannabis dependence (Agosti, Nunes, & Levin, 2002), suggesting that a significant portion of cannabis dependent patients suffer from co-occurring anxiety psychopathology. Additionally, patients who enter treatment for cannabis dependence with elevated anxiety experience more severe cannabis dependence and poorer outcomes, even after accounting for co-occurring depression (Buckner & Carroll, 2010). Third, chronically elevated anxiety may be a risk factor for more problematic marijuana use. Anxiety disorders tend to onset prior to cannabis dependence in the vast majority of dually diagnosed individuals (Agosti et al., 2002) and prospectively, adolescents with social anxiety disorder (SAD) were nearly five times more likely to develop cannabis dependence as young adults, even after controlling for depression and other relevant Axis I disorders (Buckner et al., 2008). Other work indicates that generalized anxiety and social anxiety are both prospectively related to greater risk of cannabis-related problems within the first year of using cannabis (Marmorstein, White, Loeber, & Stouthamer-Loeber, 2010). Taken together, data such as these suggest that elevated anxiety among cannabis users is related to greater cannabis-related impairment.
Consistent with tension-reduction models, elevated anxiety should be proximally related to increases in both marijuana craving and marijuana use; yet little research has tested these hypotheses and data from the few extant studies are mixed. Retrospective reports have found nervousness to be positively related to marijuana craving among adults seeking outpatient treatment for marijuana (Budney, Novy, & Hughes, 1999) but to be unrelated to craving among adolescents voluntarily seeking treatment for marijuana (Vandrey, Budney, Kamon, & Stanger, 2005). Regarding the relationship between anxiety and use, marijuana users report using marijuana to cope with stress and anxiety (Hathaway, 2003; Ogborne, Smart, Weber, & Birchmore-Timney, 2000) and relaxation or relief from tension is a commonly reported reason for and a commonly reported effect from marijuana use (Copeland, Swift, & Rees, 2001; Hathaway, 2003; Reilly, Didcott, Swift, & Hall, 1998). Higher anxiety has been noted among individuals who use marijuana more frequently (Oyefeso, 1991; Spalletta, Bria, & Caltagirone, 2006) and some types of anxiety are associated with using marijuana to cope with negative affect (e.g., Buckner, Bonn-Miller, Zvolensky, & Schmidt, 2007).
1.3 The Role of Peer Influence
People report that they tend to use marijuana in social situations (Freeland & Campbell, 1973; Reilly et al., 1998) and people attempting to reduce or quit marijuana reported exposure to others smoking marijuana as one of the two most difficult situations in which to control their use (Hughes, Peters, Callas, Budney, & Livingstone, 2008). Having more friends who use and/or approve of marijuana appears to maintain marijuana use (Kandel & Raveis, 1989; Sussman & Dent, 1999, 2004). These data suggest that being in the company of marijuana users may increase use vulnerability. Yet it remains unclear whether observed relations between peer use and self use translate to vulnerability to using marijuana around peers or whether peer normalization of marijuana use results in use even in the absence of peers.
1.4 Ecological Momentary Assessment
Although extant research has provided insight into some correlates of marijuana use, little is known about the proximal antecedents of use due to methodological limitations of the extant research. First, although prospective data suggest that anxiety predicts onset of subsequent CUD (e.g., Buckner et al., 2008), the time intervals in these studies are often several years, making it unclear as to whether momentary increases in anxiety are related to marijuana use. Second, retrospective self-report data of antecedents of marijuana use may be subject to memory bias, which could be particularly relevant to marijuana using populations given evidence of memory problems among users (Wadsworth, Moss, Simpson, & Smith, 2006).
The incorporation of ecological momentary assessment (EMA) into prospective designs is one way to overcome such methodological limitations. EMA involves the use of daily monitoring of target behaviors. The benefits of EMA include: (1) collection of data in real-world environments, thereby enhancing ecological validity; (2) minimization of retrospective recall bias; and (3) aggregation of observations over multiple assessments to facilitate within-subject assessments of behaviors across time and context (Shiffman, Stone, & Hufford, 2008).
We know of only one published study using EMA to examine the relationship between anxiety and marijuana use (Tournier, Sorbara, Gindre, Swendsen, & Verdoux, 2003). In this study, state anxiety was unrelated to marijuana use. However, methodological issues may limit generalizability of findings. First, the sample was predominantly female so little is known about the relations between anxiety and use in mixed-gendered samples (important given men remain more likely to use marijuana; SAMHSA, 2009). Second, marijuana use was assessed over a relatively short time period (one week) which is problematic given one-third of their sample reported no marijuana use in the month prior to participation. Third, they relied solely on responses to random prompts. Asking participants to also complete assessments when they used marijuana could have provided more precise assessment of the relations between marijuana craving and use.
The relation between craving and marijuana use has been assessed using EMA among drug-dependent women in treatment, 34% of whom had cannabis dependence (Johnson, Barrault, Nadeau, & Swendsen, 2009). Relations between substance craving and use were assessed over one week using personal digital assistants (PDAs). There was a trending relation between marijuana craving and marijuana use (p=.07). However, interpretation of study findings are somewhat limited by several factors. For instance, all participants were in treatment, thereby limiting generalizability to non-treatment seeking marijuana users. And as in the Tournier et al. (2003) study, the sample was also entirely female, participants completed assessments only upon receipt of electronic signal, and other affective and situational antecedents of use were not assessed.
The present study evaluated the affective and situational antecedents of marijuana use using real word data about ad-lib marijuana use episodes. First, the cross-sectional and prospective relationships between anxiety and craving were examined. It was predicted that anxiety would be positively correlated with marijuana craving cross-sectionally. Prospectively, it was hypothesized that anxiety at one assessment point would be positively related to craving at the next assessment point. Second, it was predicted that (1) marijuana craving and anxiety would be greater on marijuana use days than non-use days, (2) marijuana craving and anxiety would be positively related to marijuana use at each assessment point, and (3) marijuana craving and anxiety at one assessment point would predict marijuana use at the next assessment point. Third, because individuals claim to use marijuana to decrease cravings and anxiety, it was predicted that participants would report decreased craving and anxiety after marijuana use. Fourth, it was hypothesized that marijuana use would be more likely to occur both in the presence of others and when others were using marijuana.
2. Method
2.1 Participants
Participants were recruited based on responses to a mass screening administered in undergraduate introductory psychology classes. A flowchart of study participants is presented in Figure 1. Eligibility criteria included current (past three months) marijuana use. The final sample was comprised of 49 (38.8% female) students and ages ranged from 18-22 years (M=19.14, SD = 1.02). Participants reported currently using marijuana an average of 5-6 times a week with lifetime average use in the 1-4 times per week range. Mean age of first marijuana use was 15.3 (SD = 1.6; range=12-19). Regarding prevalence of CUD, 13 (26.5%) met DSM-IV criteria for cannabis abuse and 18 (36.7%) met criteria for cannabis dependence. Twenty-two percent met criteria for a current anxiety disorder, the most common being SAD (20.4%) followed by OCD (6.1%), panic disorder (2.0%) and generalized anxiety disorder (2.0%). Only 2.0% met criteria for a depressive disorder. The racial/ethnic composition of the sample was: 2.0% American Indian, 83.7% Caucasian, 2.0% Hispanic/Latino, 10.2% mixed, and 2.0% other. For additional information on study recruitment, please see Buckner et al. (2011).
Figure 1.
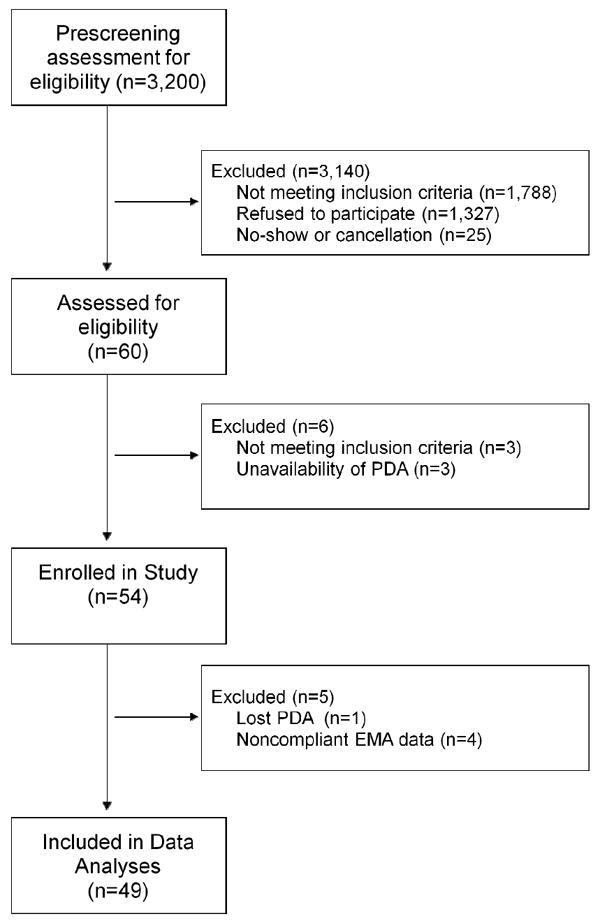
Flowchart of study participants.
2.2 Baseline Assessments
Clinical interviews
Diagnostic status was determined via clinical interview using the Anxiety Disorders Interview Schedule-IV-L (ADIS; DiNardo, Brown, & Barlow, 1994). Percent agreement between clinical interviewers in our laboratory using the ADIS has been found to be over 80% (Buckner & Schmidt, 2009a).
Marijuan
Marijuana use was assessed with the Marijuana Use Form (MUF), a self-report instrument (Buckner et al., 2007). Lifetime frequency was rated from 0 (never) to 6 (once or more every day). Past-month frequency was rated from 0 (once per month or less) to 9 (at least 21 times per week). This questionnaire has successfully assessed marijuana use behaviors (e.g., Buckner et al., 2007; Buckner & Schmidt, 2008, 2009b).
2.3 EMA Assessments
EMA data were collected via PDAs that were manufactured by Palm (Z22 Handheld). EMA data collection included three types of EMA assessments (Wheeler & Reis, 1991): (1) signal contingent assessments that were completed upon receipt of PDA signal. Participants were signaled six semi-random times throughout the day. The time of the signal was determined randomly to be within 17 min of each of six anchor times distributed evenly throughout the day as this distribution was thought to reflect the most likely waking hours of our undergraduate sample: 10:20 a.m., 1:00 p.m., 3:40 p.m., 6:20 p.m., 8:00 p.m., 11:40 p.m.; (2) interval contingent assessments that were completed at predetermined intervals (i.e., bedtime); and (3) event contingent assessments that were completed each time participants were about to use marijuana. Participants were presented with the same questions regardless of which type of assessment they were completing. The below measures were completed at each assessment.
2.3.1 Craving
Participants rated current marijuana craving on an 11-point scale from 0 (No Urge) to 10 (Extreme Urge). Similar scales have been used in prior studies of marijuana craving and been found to respond similarly to longer self-report craving scales (e.g., Buckner, Silgado, & Schmidt, 2011).
2.3.2 State Anxiety
State anxiety was assessed using a Subjective Units of Distress (SUDs; Wolpe, 1968) in which participants rated current anxiety on an 11-point scale from 0 (Totally relaxed, on the verge of sleep) to 10 (The highest anxiety you have ever experienced).
2.3.3 Situation Type and Others’ Marijuana Use
Participants were asked to choose whether they were in a “Social Situation (with other people)” or “Alone (not in a situation with other people)”. If Social Situation was selected, participants were asked if other people were using or about to use marijuana.
2.3.4 Self Marijuana Use
Participants indicated whether they were about to use marijuana (yes or no).
2.4 Procedures
Procedures were approved by the University’s Institutional Review Board prior to data collection. Informed consent was obtained from all participants. During PDA training, participants were instructed to not complete assessments when it was not convenient (e.g., while in class) or unsafe (e.g., while driving). In these instances, they were asked to respond to any PDA signals within one hour if possible.
During the two-week monitoring period, participants were sent daily e-mails reminding them to complete the day’s assessments. A two-week monitoring period was chosen given prior work finding this time period to be sufficient to monitor other types of behaviors (e.g., Crosby et al., 2009; Smyth et al., 2007; Wonderlich et al., 2007) including substance use (Freedman, Lester, McNamara, Milby, & Schumacher, 2006). Participants then returned the PDA to laboratory personnel and received debriefing, research credit, and local marijuana treatment referrals. Research credit was awarded upon return of the PDA and was not contingent upon a particular level of reporting during the monitoring period.
2.5 Statistical analysis
The relationship between momentary anxiety and marijuana craving was evaluated using a series of mixed effects linear models. All models included a random effect for subject and fixed effects for other predictors. First, we examined whether anxiety at a given assessment point was related to marijuana craving at that same assessment point. Next, two time-lagged analyses were conducted to evaluate the temporal patterns between anxiety and marijuana craving. Specifically, anxiety at one assessment point was used to predict marijuana craving at the next assessment; and marijuana craving at one assessment point was used to predict anxiety at the next assessment. Pseudo R-squared values were calculated using error terms from the unrestricted and restricted models as described by Kreft and de Leeuw (1998). All analyses were conducted using mixed effects functions in PASW (formerly SPSS) version 18.0.
The cross-sectional and prospective relationships of anxiety and marijuana craving to marijuana use were then evaluated in four separate ways. First at the daily level, mixed effects linear models were used to compare mean levels of craving and anxiety on days in which marijuana use was reported to non-use days. Because many of these students completed assessments in the early morning hours (between midnight and 5:00AM), a new day was defined as beginning at 7:00AM. Data were aggregated by participant and day, thereby creating an average anxiety and craving rating for each participant on each day. Days were dummy coded (0=non-marijuana day, 1=marijuana use day). Next at the momentary level, generalized linear models with a logistic response function were used to evaluate whether momentary craving or anxiety was related to marijuana use at that time point. Then at the antecedent level, generalized linear models comparable to those above evaluated whether craving and anxiety at one time point predicted marijuana use at the next time point. Finally, the temporal pattern of anxiety and marijuana craving was evaluated using a mixed effects linear models. Specifically, pre- and post-marijuana use anxiety and craving was modeled using linear, quadratic and cubic effects centered around the first marijuana use of the day. These models included a random effect for subjects, and fixed effects for minutes prior to/after marijuana use, minutes2 prior to/after marijuana use, minutes3 prior to/after marijuana use, as well as interactions between these time components and pre/post marijuana use status.
Compliance with the EMA protocol was assessed by determining mean daily percentage of random prompts, mean daily percentage of end of day assessments, and mean percentage of both random and end of day assessments completed per participant. Participants completed a mean of 61% (SD=26%; range=2%-96% per participant) of random signals, 64% (SD=19%; range=21%-93% per participant) of end of day assessments, and 62% (SD=23%; range=11%-.94% per participant) of both random and end of day assessments. In line with prior work (Hopper et al., 2006), we retained data from participants with at least 20% compliance rates. Although GLM does allow for missing data, it did not seem prudent to include days where half or more of the ratings were missing. Using this strategy, four participants were excluded from data analyses (Figure 1). Excluded participants did not differ from the rest of the sample terms of demographic variables, or marijuana use frequency (p’s>.05).
The remaining 49 participants completed 66% of the random assessments, with slightly higher compliance rates on marijuana use days (71%) than non-use days (66%). These rates are somewhat higher than those obtained in other EMA studies of substance use in non-treatment samples (Hopper et al., 2006) and somewhat lower than rates obtained with participants undergoing SUD treatment (e.g., Epstein et al., 2009). The 49 participants completed 4,069 signal contingent (M=83.19, SD= 3.33 per participant), 518 interval contingent (M=10.73, SD= 3.50 per participant), and 452 event contingent (M=10.75, SD= 10.05 per participant) assessments. Signal contingent assessments were completed on average 14.8 (SD=62.5) minutes after the signal occurred1.
3. Results
3.1 Patterns of Marijuana Use
Participants recorded 732 marijuana use entries (M=16.26, SD= 15.08 per participant) and 51.9% of all entries occurred on marijuana use days. Participants reported an average of 1.33 (SD=1.63) marijuana use episodes per day. Figure 2 graphically presents percent of days on which marijuana use occurred (2a), time of day marijuana use occurred (2b), and number of times marijuana was used on marijuana use days (2c). Interestingly, marijuana use was as likely to occur during the week as on weekends. Marijuana use appears most likely to occur from 6PM-midnight, with an additional peak in use from 3-4PM. When marijuana use did occur, approximately 40% of the time participants reported they used marijuana only one time that day.
Figure 2.
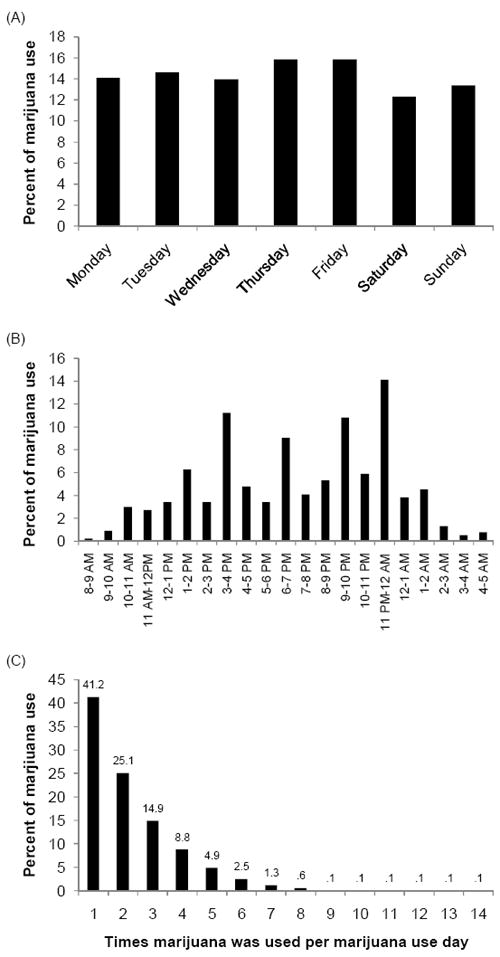
(A) Days of the week that marijuana was used, (b) time of day when marijuana was used, and (C) number of times marijuana used per marijuana use day.
3.2 Does Anxiety Level Predict Marijuana Craving?
First, results suggest anxiety was positively, significantly related to marijuana craving at the momentary level, β=.48, SE=.01, p<.001, pseudo R2=.084. Second, regarding temporal relations, anxiety demonstrated a positive relationship with later craving, β=.36, SE=.01, p<.001, pseudo R2=.047. The specificity of the observed temporal relations between anxiety and craving were next examined by testing whether craving at one assessment point predicted anxiety at the next assessment. Craving demonstrated a positive relationship with later anxiety, β=.13, SE=.01, p<.001, although the strength of this association was somewhat weaker than the relation between anxiety and subsequent craving, pseudo R2=.024.
3.3 Did Marijuana Craving Predict Marijuana Use?
Table 1 shows the results for all analyses conducted to examine whether craving was related to marijuana use. Cross-sectionally, average craving ratings were higher on marijuana use days than non-use days. Also, craving was higher when participants were about to use marijuana than when they were not about to use. Relations between craving and marijuana use were next examined at the antecedent level. Consistent with expectation, craving was higher among those who subsequently used marijuana than those who did not use marijuana.
Table 1.
Relations Between Marijuana Craving or Anxiety and Marijuana Use as assessed by (1) Whether Marijuana was Used that Day, (2) Momentary Relations between Craving/Anxiety and Marijuana Use, and (3) Whether Craving/Anxiety at One Assessment Point Predicted Marijuana Use at Next Assessment Point
| Predictor | Marijuana use | No marijuana use | β | SE | p | pseudo R2 |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | |||||
| Marijuana Use Day Status | ||||||
| Craving | 3.77 (2.18) | 2.46 (2.05) | .29 | .02 | <.001 | .066 |
| Anxiety | 2.08 (1.31) | 2.24 (1.68) | -.08 | .02 | <.001 | .002 |
| Momentary Marijuana Use | ||||||
| Craving | 5.39 (2.75) | 2.65 (2.53) | .36 | .02 | <.001 | .151 |
| Anxiety | 2.40 (1.87) | 2.04 (1.90) | .09 | .02 | <.001 | .005 |
| Subsequent Marijuana Use | ||||||
| Craving | 4.17 (2.98) | 2.91 (2.68) | .16 | .02 | <.001 | .032 |
| Anxiety | 2.21 (1.80) | 2.06 (1.91) | .04 | .02 | .074 | .001 |
The temporal pattern between marijuana craving and use were next examined by determining patterns of craving before and after marijuana use. Figure 3a represents the trends in craving ratings in the hours prior to and following marijuana use. Results indicate that marijuana craving increased at a significant rate prior to marijuana use, F(1, 1409.75)=60.30, p<.001. Craving also decreased at a significant rate following marijuana use, F(1, 1412.33)=109.83, p<.001.
Figure 3.
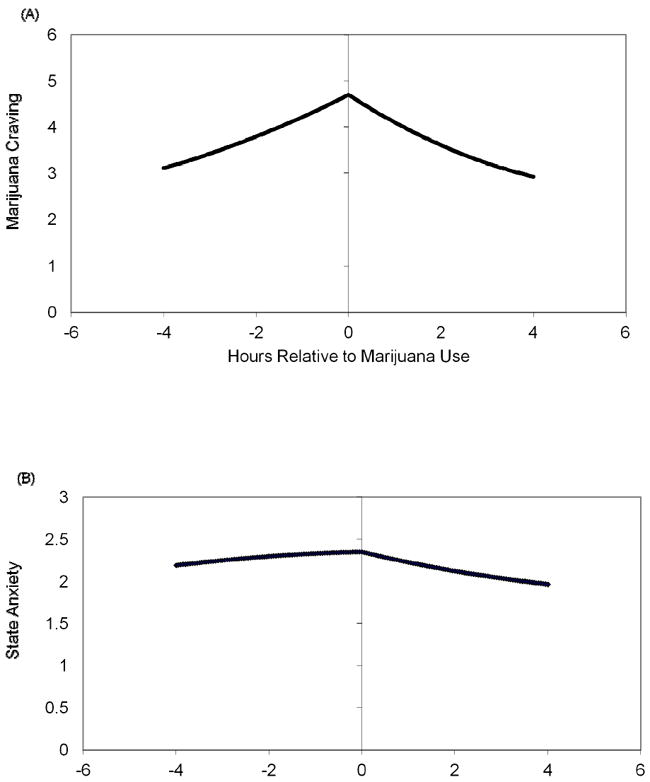
(A) Craving levels pre- and post-marijuana use and (B) Anxiety levels pre- and post-marijuana use.
3.4 Did Anxiety Level Predict Marijuana Use?
Table 1 also shows the results for all analyses conducted to examine whether anxiety was related to marijuana use. At the daily level, average anxiety ratings were somewhat lower on marijuana use days than non-use days, although average anxiety only accounted for 0.2% of the variance in marijuana use day status. Also, anxiety was somewhat higher when participants were about to use marijuana than when they were not about to use.
The temporal relations between anxiety and marijuana use were examined. Consistent with expectation, anxiety was somewhat higher among those who subsequently used marijuana than those who did not use marijuana, although again anxiety accounted for a small percent (0.1%) of the variance in marijuana use. The temporal patterns between anxiety and marijuana use were next examined by determining patterns of anxiety in the hours before and after marijuana use (Figure 3b). Anxiety ratings did not increase at a significant rate prior to marijuana use, F(1, 1410.34)=.04, p=.846. There was a non-significant trend for anxiety to decrease following marijuana use, F(1, 1413.73)=2.91, p=.088.
3.5 Individual Differences in Relationships between Craving/Anxiety and Marijuana Use
In line with prior work (Shiffman et al., 2007), we examined whether there were individual differences in the relationships between state craving/anxiety and marijuana use. For each participant, we computed the differences in means between marijuana use and non-use episodes. Figure 4 shows the distribution of these differences. The distribution for marijuana craving scores (Figure 4a) suggests that craving was almost always higher during marijuana use than non-use episodes.
Figure 4.
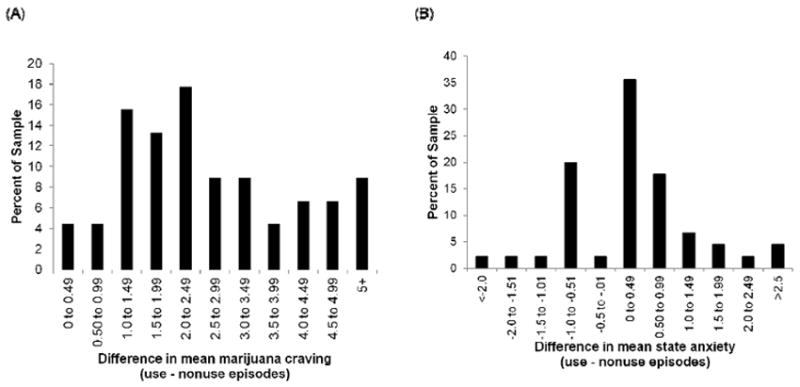
Distribution of differences in mean ratings of state (A) marijuana craving and (B) anxiety for marijuana use and non-use occasions.
The distribution of state anxiety scores (Figure 4b) suggests that, although scores tended to cluster around zero (suggesting minimal difference in state anxiety when comparing marijuana use to non-use episodes), there was some degree of individual differences in the pattern of responses such that 35.5% of participants reported higher state anxiety during marijuana use episodes compared to non-use episodes (i.e., state anxiety ratings were ≥ 0.50 during use episodes) whereas 29.9% reported higher state anxiety during non-use episodes relative to marijuana use episodes.
3.6 Did Peers Influence Marijuana Use?
Participants were significantly more likely to use marijuana in social situations than when alone, β=4.91, SE=.19, p<.001, pseudo R2=.948. Specifically, 77.3% of marijuana use occurred in social situations. When participants were in social situations, they were significantly more likely to use if others were using, β=-4.91, SE=.19, p<.001, pseudo R2=.991. In fact, 93.3% of participants’ marijuana use in social situations occurred when others were also using.
4. Discussion
Findings from this study contribute to our understanding of marijuana use in several significant ways. First, anxiety and marijuana craving appear closely related. Second, marijuana craving and state anxiety seem to play an important role in marijuana use. Third, participants were especially vulnerable to using marijuana when in the company of others who were using marijuana.
4.1 The Role of Marijuana Craving
Despite theoretical models that craving predicts marijuana use (e.g., Marlatt & Gordon, 1980) and treatment strategies devoted explicitly to helping patients manage marijuana cravings to prevent relapse (e.g., Carroll, 1999), very little empirical work has examined whether craving actually predicts marijuana use. We found marijuana craving to be related to marijuana use in all four of our tests of these relations, providing strong support for the importance of craving in marijuana use. We also found evidence of individual differences in the strength of the relationship between craving and marijuana use that suggests that some individuals use marijuana even under conditions of low craving. Nearly 9% reported mean difference scores between marijuana use and non-use episodes to be less than 1 point, suggesting there may be a small group of individuals that use for reasons other than to manage marijuana craving. However, for the vast majority of participants, craving was notably higher during marijuana use compared to non-use episodes.
The strong relationship between craving and marijuana use in the present study is contrary to the results of the only other known EMA study of the relations between craving and marijuana use which found a weak relationship between craving and use (Johnson et al., 2009). There are several methodological differences between the two studies that may account for these differences. First, participants in the Johnson et al. study only completed signal contingent assessments, whereas participants in our study also completed assessments before marijuana use and at bedtime (which for many participants was a time they used marijuana). In fact, of the 732 marijuana use episodes recorded, 452 (i.e., over half) were recorded in response to event contingent assessments, suggesting assessing using only signal contingent assessments may have resulted in fewer marijuana use episode recordings in the Johnson et al. study. In other words, our assessment strategy may have captured more marijuana use episodes permitting us greater statistical power to detect the relation between marijuana craving and use. Second, the other sample was comprised of women in substance dependence treatment and only 34% met criteria for cannabis dependence. It is unclear how many of these participants actually used marijuana during the course of the study. It may be that other substances (e.g., cocaine, given that 65% of participants presented with cocaine dependence) were more likely to be used during their one-week monitoring period. On the other hand, out study sample was comprised entirely of current marijuana users who reported on their marijuana use during a two-week monitoring period. Third, participants in the Johnson et al. study were in treatment whereas our participants were non-treatment seeking. It may be that the participants in treatment were motivated to under-report craving while in treatment and/or had learned alternative means by which to cope with cravings other than using marijuana.
Our finding that marijuana craving is closely related to marijuana use has implications for the treatment of marijuana use. For instance, cognitive-behavioral treatments (CBT) for marijuana currently teach patients skills to help manage cravings to prevent relapse (e.g., Carroll, 1999). Our findings support the use of such techniques as cravings appear to increase the likelihood of use, at least in this non-treatment seeking sample. However, future work is necessary to determine whether the skills currently taught in treatment are in fact effective in reducing cravings, and subsequently, marijuana use.
4.2 The Role of Anxiety
Predictions regarding the role of anxiety in marijuana craving and marijuana use were only partially supported. Anxiety was cross-sectionally and prospectively related to marijuana craving. That anxiety predicted subsequent craving in this sample has important implications. First, this finding supports tension reduction (Conger, 1956) models of substance use as this directionality suggests people may want to use marijuana to manage increases in anxiety. Interestingly, we also found that craving can result in increased anxiety. Given that anxiety is related to marijuana withdrawal (e.g., Bonn-Miller, Zvolensky, Marshall, & Bernstein, 2007), it may be that if craving is not addressed by using marijuana, the individual begins to experience withdrawal, a component of which is increased anxiety.
Taken together, our findings suggest that anxiety can increase marijuana craving and craving can increase anxiety. Such a pattern would support the “mutual maintenance model” of anxiety and substance use (e.g., Stewart & Conrod, 2008) which suggests that regardless of whether anxiety or marijuana use begins first, once the problems have emerged, if people use marijuana to manage anxiety, they may experience short-term perceived relief, but anxiety related to marijuana use (e.g., anxiety produced as a result of unsatisfied cravings) may emerge, resulting in a “vicious cycle” between anxiety and marijuana use. Specifically, at least some individuals may crave marijuana so they can escape unpleasant anxiety sensations. The desire to use marijuana to manage anxiety may increase the likelihood that these individuals will become reliant on marijuana to help manage anxiety and may thus place these people at risk for marijuana problems and CUD. In fact, using marijuana to cope with negative affect has been found to mediate the relations between some forms of anxiety and marijuana-related problems (Buckner et al., 2007).
However, our data provide only partial support for the idea that increases in anxiety are associated with actual marijuana use. At the momentary level, anxiety was higher when participants were about to use marijuana compared to when they were not about to use and time-lagged analyses suggest that anxiety at one time point was related to marijuana use at the subsequent assessment point. However, the size of these effects was generally smaller than those of craving. Thus it may be that anxiety is indirectly related to marijuana use through its effects on marijuana craving.
Alternatively, it may be that only those participants with particular psychological vulnerabilities (e.g., CUD, anxiety disorder) use marijuana to manage anxiety. There was some degree of heterogeneity in the differences in anxiety during marijuana use episodes compared to non-use ones. Approximately one-third of participants reported greater anxiety during marijuana use compared to non-use episodes suggesting these may be the participants vulnerable to using marijuana to manage their anxiety. On the other hand, nearly 29% of participants reported higher anxiety during non-use episodes, suggesting these participants may choose to abstain when experiencing elevated anxiety due to the anxiogenic properties of marijuana. In fact, marijuana use seems to lead to increases in anxiety for some users (Zvolensky et al., 2006; Zvolensky et al., 2008). Future research aimed at further delineating the individual difference variables related to marijuana use will be an important next step in this line of work.
Notably, marijuana use was not associated with substantial reductions in anxiety, suggesting that although some people may use marijuana to manage their anxiety, marijuana use may not actually decrease subjective anxiety. This finding has important treatment implications. For instance, patients who use marijuana to decrease anxiety could be given psychoeducation that marijuana use may not actually decrease their subjective anxiety. Such psychoeducation could serve as rationale for teaching them more effective methods of managing unpleasant affective states.
4.3 The Role of Peer Influence
This is the first known EMA study to examine the role of peer marijuana use on participant use. Consistent with work relying on retrospective self-reports (e.g., Reilly et al., 1998), marijuana use was most likely to occur when others were using marijuana. In fact, over 75% of marijuana use occurred in the presence of others and when with others, 93% of participants’ use occurred when others were using marijuana. These data suggest that peer use may play a particularly powerful role in marijuana use behaviors. This finding has very important implications for the treatment of marijuana use. For instance, patients may benefit from spending a larger amount of time in therapy learning skills specifically designed to manage marijuana-using peers (e.g., refusal skills, planning for high-risk situations). Also given the robust relation between social anxiety and problematic marijuana use (e.g., Buckner et al., 2008), future work could benefit from examining whether increases in state social anxiety play a role in marijuana use behaviors when in the presence of others who are using marijuana. It is possible, for example, that at least some individuals use marijuana for fear of negative evaulation from marijuana-using peers should they refuse to use.
4.4 Limitations and Directions for Future Research
Results of the present study should be considered in light of limitations that point to additional avenues of work in this area. First, unlike some EMA studies (e.g., Shiffman et al., 2002; Smyth et al., 2007), participants were not given a “practice period” during which to practice the assessment procedures and obtain feedback on their compliance with the protocol. Failure to provide such feedback may have contributed to compliance rates lower than those obtained in some other EMA studies. Rather, we emailed participants daily to remind them to complete the assessments. This strategy resulted in compliance rates somewhat higher than those reported in other EMA studies of non-treatment samples of substance users (Hopper et al., 2006). Thus, future work may want to combine these strategies with non-treatment seeking substance use populations to maximize compliance. Second, the present sample was comprised of undergraduate students. Although our data are thereby generalizable to groups particularly vulnerable to marijuana use and marijuana-related impairment (i.e., young adults, college students; Buckner, Ecker, & Cohen, 2010; Caldeira, Arria, O’Grady, Vincent, & Wish, 2008; SAMHSA, 2009), future study is needed to examine whether the observed relations generalize to other marijuana-using populations. Third, participants were not treatment-seeking, permitting the examination of factors that maintain marijuana use among users not in treatment. An important next step will be to identify factors that increase lapse and/or relapse vulnerability among marijuana users attempting marijuana cessation. Fourth, only one negative affective state was examined and future work could benefit from examining the momentary relations between other negative emotional states (e.g., sadness, anger) and marijuana use.
4.5 Summary
Findings highlight the important roles craving, anxiety, and peer marijuana use play in maintaining marijuana use. Further, our study supports the feasibility of collecting EMA data with marijuana users. Given the prevalence of marijuana use and CUD, it is our hope that this study will serve as a first step in continued EMA studies aimed at understanding factors that maintain marijuana use and/or place individuals at risk for marijuana-related problems.
Acknowledgments
Role of Funding Sources This research was supported in part by a National Institute on Drug Abuse (NIDA) grant F31 DA021457 awarded to Julia D. Buckner, Ph.D. This funding agency had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
The authors thank Scott Engle, Ph.D., for his input on data analyses.
Footnotes
Contributors Authors Buckner, Schmidt, and Wonderlich designed the study and wrote the protocol. Author Buckner wrote reviews of prior research and author Silgado wrote portions of the method section. Authors Buckner and Crosby conducted the statistical analysis. All authors contributed to and have approved the final manuscript.
Conflict of Interest All authors declare that they have no conflicts of interest.
Analyses were also conducted excluding all signal contingent data that was not compliant with study instructions (i.e., completed more than 60 minutes after signal prompt). A similar pattern of significant findings was obtained.
References
- Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse. 2002;28:643–652. doi: 10.1081/ADA-120015873. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Marshall EC, Bernstein A. Incremental validity of anxiety sensitivity in relation to marijuana withdrawal symptoms. Addictive Behaviors. 2007;32:1843–1851. doi: 10.1016/j.addbeh.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, Schmidt NB. Marijuana use motives and social anxiety among marijuana-using young adults. Addictive Behaviors. 2007;32:2238–2252. doi: 10.1016/j.addbeh.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Carroll KM. Effect of anxiety on treatment presentation and outcome: Results from the Marijuana Treatment Project. Psychiatry Research. 2010;178:493–500. doi: 10.1016/j.psychres.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Ecker AH, Cohen AS. Mental health problems and interest in marijuana treatment among marijuana-using college students. Addictive Behaviors. 2010;35:826–833. doi: 10.1016/j.addbeh.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Marijuana effect expectancies: Relations to social anxiety and marijuana use problems. Addictive Behaviors. 2008;33:1477–1483. doi: 10.1016/j.addbeh.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. A randomized pilot study of motivation enhancement therapy to increase utilization of cognitive-behavioral therapy for social anxiety. Behaviour Research and Therapy. 2009a;47:710–715. doi: 10.1016/j.brat.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Social anxiety disorder and marijuana use problems: The mediating role of marijuana effect expectancies. Depression and Anxiety. 2009b;26:864–870. doi: 10.1002/da.20567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Silgado J, Schmidt NB. Marijuana craving during a public speaking challenge: Understanding marijuana use vulnerability among women and those with social anxiety disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2011;42:104–110. doi: 10.1016/j.jbtep.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Smits J, Norton PJ, Crosby RD, Wonderlich SA, Schmidt NB. Anxiety sensitivity and marijuana use: An analysis from ecological momentary assessment. Depression and Anxiety. 2011;28:420–426. doi: 10.1002/da.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Novy PL. Marijuana abstinence effects in marijuana smokers maintained in their home environment. Archives of General Psychiatry. 2001;58:917–924. doi: 10.1001/archpsyc.58.10.917. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. Journal of Abnormal Psychology. 2003;112:393–402. doi: 10.1037/0021-843X.112.3.393. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Novy PL, Hughes JR. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–1322. doi: 10.1046/j.1360-0443.1999.94913114.x. [DOI] [PubMed] [Google Scholar]
- Caldeira KM, Arria AM, O’Grady KE, Vincent KB, Wish ED. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addictive Behaviors. 2008;33:397–411. doi: 10.1016/j.addbeh.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM. MET/CBT: A combined strategy for stopping problem substance use: Clinician Manual 1999 [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Copeland J, Swift W, Rees V. Clinical profile of participants in a brief intervention program for cannabis use disorder. Journal of Substance Abuse Treatment. 2001;20:45–52. doi: 10.1016/S0740-5472(00)00148-3. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47:181–188. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin J-L, Preston KL. Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Archives of General Psychiatry. 2009;66:88–94. doi: 10.1001/archgenpsychiatry.2008.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman MJ, Lester KM, McNamara C, Milby JB, Schumacher JE. Cell phones for ecological momentary assessment with cocaine-addicted homeless patients in treatment. Journal of Substance Abuse Treatment. 2006;30:105–111. doi: 10.1016/j.jsat.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Freeland JB, Campbell RS. The social context of first marijuana use. Substance Use and Misuse. 1973;8:317–324. doi: 10.3109/10826087309057478. [DOI] [PubMed] [Google Scholar]
- Gray KM, LaRowe SD, Upadhyaya HP. Cue reactivity in young marijuana smokers: A preliminary investigation. Psychology of Addictive Behaviors. 2008;22:582–586. doi: 10.1037/a0012985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Hart CL, Vosburg SK, Comer SD, Reed SC, Foltin RW. Effects of THC and lofexidine in a human laboratory model of marijuana withdrawal and relapse. Psychopharmacology. 2008;197:157–168. doi: 10.1007/s00213-007-1020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hathaway AD. Cannabis effects and dependency concerns in long-term frequent users: A missing piece of the public health puzzle. Addiction Research & Theory. 2003;11:441–458. doi: 10.1080/1606635021000041807. [DOI] [Google Scholar]
- Hopper JW, Su Z, Looby AR, Ryan ET, Penetar DM, Palmer CM, Lukas SE. Incidence and patterns of polydrug use and craving for ecstasy in regular ecstasy users: an ecological momentary assessment study. Drug and Alcohol Dependence. 2006;85:221–235. doi: 10.1016/j.drugalcdep.2006.04.012. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Peters EN, Callas PW, Budney AJ, Livingstone AE. Attempts to stop or reduce marijuana use in non-treatment seekers. Drug and Alcohol Dependence. 2008;97:180–184. doi: 10.1016/j.drugalcdep.2008.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EI, Barrault M, Nadeau L, Swendsen J. Feasibility and validity of computerized ambulatory monitoring in drug-dependent women. Drug and Alcohol Dependence. 2009;99:322–326. doi: 10.1016/j.drugalcdep.2008.06.010. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Raveis VH. Cessation of illicit drug use in young adulthood. Archives of General Psychiatry. 1989;46:109–116. doi: 10.1001/archpsyc.1989.01810020011003. [DOI] [PubMed] [Google Scholar]
- Kreft I, de Leeuw J. Introducing multivlevel modeling. Thousand Oaks, CA US: Sage Publications, Inc; 1998. [Google Scholar]
- Marlatt GA, Gordon JR. Determinants of relapse: Implications for the maintenance of behavior change. In: Davidson P, Davidson S, editors. Behavioral medicine: Changing health lifestyles. New York: Brunner/Mazel; 1980. pp. 410–452. [Google Scholar]
- Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. Journal of Abnormal Child Psychology. 2010;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogborne AC, Smart RG, Weber T, Birchmore-Timney C. Who is using cannabis as a medicine and why: An exploratory study. Journal of Psychoactive Drugs. 2000;32:435–443. doi: 10.1080/02791072.2000.10400245. [DOI] [PubMed] [Google Scholar]
- Oyefeso A. Personality differences among five categories of student cannabis users. Indian Journal of Behaviour. 1991;15:28–35. [Google Scholar]
- Reilly D, Didcott P, Swift W, Hall W. Long-term cannabis use: Characteristics of users in an Australian rural area. Addiction. 1998;93:837–846. doi: 10.1080/09652149835350. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Balabanis MH, Gwaltney CJ, Paty JA, Gnys M, Kassel JD, Hickcox M, Paton SM. Prediction of lapse from associations between smoking and situational antecedents assessed by ecological momentary assessment. Drug and Alcohol Dependence. 2007;91:159–168. doi: 10.1016/j.drugalcdep.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Hickcox M, Gnys M. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal of Abnormal Psychology. 2002;111:531–545. doi: 10.1037/0021-843X.111.4.531. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Spalletta G, Bria P, Caltagirone C. Differences in temperament, character and psychopathology among subjects with different patterns of cannabis use. Psychopathology. 2006;40:29–34. doi: 10.1159/000096387. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ. Anxiety disorder and substance use disorder co-morbidity: Common themes and future directions. In: Stewart SH, Conrod PJ, editors. Anxiety and substance use disorders: The vicious cycle of comorbidity. New York: Springer; 2008. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings (HHS Publication No SMA 09-4434, NSDUH Series H-36) Rockville, MD: 2009. [Google Scholar]
- Sussman S, Dent CW. One-year prospective prediction of marijuana use cessation among youth at continuation high schools. Addictive Behaviors. 1999;24:411–417. doi: 10.1016/S0306-4603(98)00048-3. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW. Five-year prospective prediction of marijuana use cessation of youth at continuation high schools. Addictive Behaviors. 2004;29:1237–1243. doi: 10.1016/j.addbeh.2004.03.024. [DOI] [PubMed] [Google Scholar]
- Tournier M, Sorbara F, Gindre C, Swendsen JD, Verdoux H. Cannabis use and anxiety in daily life: A naturalistic investigation in a non-clinical population. Psychiatry Research. 2003;118:1–8. doi: 10.1016/s0165-1781(03)00052-0. [DOI] [PubMed] [Google Scholar]
- Vandrey R, Budney AJ, Kamon JL, Stanger C. Cannabis withdrawal in adolescent treatment seekers. Drug and Alcohol Dependence. 2005;78:205–210. doi: 10.1016/j.drugalcdep.2004.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth EJ, Moss SC, Simpson SA, Smith AP. Cannabis use, cognitive performance and mood in a sample of workers. Journal of Psychopharmacology. 2006;20:14–23. doi: 10.1177/0269881105056644. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. doi: 10.1111/1467-6494.ep9110141804. [DOI] [Google Scholar]
- Wölfling K, Flor H, Grüsser SM. Psychophysiological responses to drug-associated stimuli in chronic heavy cannabis use. European Journal of Neuroscience. 2008;27:976–983. doi: 10.1111/j.1460-9568.2008.06051.x. [DOI] [PubMed] [Google Scholar]
- Wolpe J. Psychotherapy by reciprocal inhibition. Conditional Reflex. 1968;3:234–240. doi: 10.1007/BF03000093. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Rosenfeldt S, Crosby RD, Mitchell JE, Engel SG, Smyth J, Miltenberger R. The effects of childhood trauma on daily mood lability and comorbid psychopathology in bulimia nervosa. Journal of Traumatic Stress. 2007;20:77–87. doi: 10.1002/jts.20184. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Lifetime associations between cannabis, use, abuse, and dependence and panic attacks in a representative sample. Journal of Psychiatric Research. 2006;40:477–486. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lewinsohn P, Bernstein A, Schmidt NB, Buckner JD, Seeley J, Bonn-Miller MO. Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. Journal of Psychiatric Research. 2008;42:1017–1023. doi: 10.1016/j.jpsychires.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]


