Abstract
Despite the known efficacy of various psychotherapies and pharmacotherapies for posttraumatic stress disorder (PTSD), we know little about what factors predict treatment preference. In the present study, we first developed exploratory path models of treatment preference for a psychotherapy or pharmacotherapy (n = 273) and then conducted confirmatory analyses of these models in a second sample (n = 324) and in a third generalization sample of trauma-exposed women (n = 105). We examined demographic and psychopathology factors and treatment-related beliefs (i.e., credibility and personal reactions). Across all samples, treatment-related beliefs were the strongest predictors of treatment preference. Further, severity of depression directly reduced the likelihood of choosing psychotherapy, and severity of PTSD directly increased the likelihood of choosing pharmacotherapy. These results underscore the importance of better understanding individual’s beliefs regarding treatments. With a clearer understanding of these factors, we may be able to reduce barriers to treatment and increase access to effective treatments for those with trauma-related symptoms.
Keywords: Treatment preference, Choice, Pharmacotherapy, Sertraline, Psychotherapy, Prolonged exposure, PTSD, Trauma exposure
1. Introduction
Findings from the National Comorbidity Survey-Replication (NCS-R) highlight that many individuals with posttraumatic stress disorder (PTSD) do not seek treatment and that those who do wait a long time to do so (a median of 12 years from onset of the disorder to treatment contact; Kessler et al., 2005; Wang, Berglund, et al., 2005). In fact, only 7.1% made contact within the first year and projected proportions of those who eventually made treatment contact only reached 65.3% (Wang, Berglund, et al., 2005). When considering mental health service utilization only, these numbers further decrease (Wang, Lane, et al., 2005). Poor access to mental health services is one contributor to lack of treatment, but alone does not explain low rates of treatment seeking and service utilization. Accordingly, in a recent review of mental health service utilization, Gavrilovic, Schutzwohl, Fazel, and Priebe (2005) highlighted sociodemographic variables such as female gender, higher severity of current psychopathology, and more severe event-related characteristics as facilitating treatment seeking following trauma exposure.
One key to potentially enhancing treatment seeking may be better understanding patients’ treatment preferences and identifying factors that account for or influence these preferences. Clients in routine clinical practice often see a treatment provider after active shopping for a type of treatment (Seligman, 1995). Along these lines, a NIMH workshop report on greater public health relevance for psychotherapeutic intervention research (Street, Niederehe, & Lebowitz, 2000) has called for the specific study of patient attitudes, knowledge, and beliefs about treatment as they pertain to the treatment preferences. Accordingly, in recent years, studies examining preferences for mental health treatments, specifically psychotherapy and/or pharmacotherapy, have begun to emerge.
Across a variety of disorders and studies, when given a choice, there is a general preference for psychological interventions over pharmacological ones (Barlow, 2004). To date, four studies have explored treatment preferences regarding psychological reactions associated with trauma exposure (Becker, Darius, & Schaumberg, 2007; Roy-Byrne, Berliner, Russo, Zatzick, & Pitman, 2003; Tarrier, Liversidge, & Gregg, 2006; Zoellner, Feeny, Cochran, & Pruitt, 2003), with two studies directly examining and finding a preference for psychotherapy alone over pharmacotherapy alone (Roy-Byrne et al., 2003; Zoellner et al., 2003). With this emerging data, what we now need to better understand is what factors shape such preferences; in other words, why do people have the preferences they have?
Along these lines, some work has begun to explore potentially important demographic and psychopathology predictors of treatment preferences. Similar to findings from the service utilization literature, demographic factors such as age, education, ethnic minority status, and the presence or severity of psychopathology are emerging as promising predictors of treatment preference for mood and anxiety disorders (e.g., Angelo, Miller, Zoellner, & Feeny, 2008; Bedi et al., 2000; Hazlett-Stevens et al., 2002; Roy-Byrne et al., 2003; Zoellner et al., 2003). For example, when examining a sample of primary care individuals with anxiety disorders, Hazlett-Stevens et al. (2002) reported that among individuals with panic, older age, less education, and poorer health status were associated with willingness to consider medication. Minority status, however, was associated with less receptivity to medication. In Roy-Byrne et al.’s (2003) study of emergency room patients, being female and being sexually assaulted were predictive of preference for medication and for counseling; and, previous psychiatric treatment and perceived life threat during assault were predictive of a preference for counseling. Similarly, a recent study from Angelo et al. (2008) found that in a community sample of trauma-exposed women, more education was associated with an increased likelihood to choose psychotherapy over pharmacotherapy. Thus, demographic factors such as socioeconomic status and education may play a role in shaping treatment preferences and warrant further exploration.
In contrast, we know much less about the role of psychopathological predictors of preference. Hazlett-Stevens et al. (2002) reported that the presence of social phobia and/or PTSD symptoms was associated with preference for medication and psychosocial interventions, suggesting that these factors might reflect a more general preference for treatment in general. In Zoellner et al.’s (2003) analogue study, higher state anxiety was slightly related to less positive personal reaction rationales providing information about psychotherapy, suggesting that these individuals may be less inclined to participate in a therapy that may cause some distress. Clearly, the presence of more severe psychopathology may serve as a motivator toward treatment of any form but may also impact the type of treatment preferred.
Finally, an individual’s beliefs about, or attitudes toward, particular interventions may also influence his or her willingness to consider a treatment. Indeed, some studies have started to go beyond demographics and psychopathology factors to investigate actual beliefs about specific interventions (e.g., Wagner et al., 2005). Such beliefs include the patient’s perception of the scientific credibility of the treatment, their understanding of their symptoms, their perception of the treatment’s ability to alleviate these symptoms, and their personal reactions to treatment procedures. When examining such treatment beliefs in a sample of primary care patients with anxiety disorders, Wagner et al. (2005) reported that more severe depression was associated with more favorable attitudes toward pharmacotherapy. In an analogue sample, Cochran, Pruitt, Fukuda, Zoellner, and Feeny (2008), reported that perceived treatment effectiveness and positive feelings about the importance of talking about a traumatic event were associated with choosing psychotherapy; whereas, perceived need for help and practical considerations were associated with either choosing pharmacotherapy or no treatment. Similarly, in a community sample of trauma-exposed women, Angelo et al. (2008) reported that almost half of the respondents reported the main belief influencing their treatment preference was the mechanism (e.g., “You need to talk about the trauma.”) underlying the effectiveness of the treatment. Together these studies highlight the potential influence of existing beliefs toward particular treatments in shaping receptivity to such options.
Researchers in this area have yet to develop associative frameworks to begin to explore the relative influences of contributing factors (e.g., demographics, psychopathology, and treatment-related beliefs) associated with treatment preferences and the relationships among such factors. Thus, in the current study, we examined the prediction of treatment preference, as well as treatment-related beliefs, by generating and testing predictive models that examine the relationships among these as well as demographic characteristics and psychopathology factors. In particular, although a variety of effective treatments exist for chronic PTSD, we chose to focus on two very different and well-validated treatment approaches for PTSD, namely prolonged exposure (e.g., Foa et al., 2005; Resick et al., 2002; Schnurr et al., 2007) and sertraline (e.g., Brady et al., 2000; Davidson et al., 2001). To examine factors underlying treatment preference, we conducted exploratory and confirmatory path analyses in two large samples of undergraduate women, many of whom had experienced a potentially traumatic event (PTE).1 We chose these groups for model generation and confirmation process due to the ease of recruiting large samples and due to the age range being one where the issues of potential sexual assault are particularly salient (Tjaden & Thoennes, 1998). In the model generation process, we focused on demographic and psychopathology predictors of preference examined in previous studies. Given that different predictors may be involved in treatment-related beliefs and treatment preference (i.e., Hazlett-Stevens et al., 2002; Wagner et al., 2005), we chose to examine these constructs separately. Finally, we then examined generalization of the path models generated in the first sample, to a community sample of women who reported experiencing a PTE.
2. Method
2.1. Sample 1 participants (exploratory sample)
At two large urban universities, 273 female participants were recruited via undergraduate psychology subject pools. Participants were on average 19.41 (SD = 1.94) years old. Sixty-one percent (60.8%) were Caucasian, 27.5% Asian American, and 11.5% from other backgrounds. Fifty-six percent (56.4%) reported a DSM-IV Criterion A trauma using the Posttraumatic Stress Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997). For those who specified a Criterion A event, 22% reported a serious accident, 17.3% a life-threatening illness, 15.9% a sexual or non-sexual assault, 15.3% a natural disaster, and 29.5% reported other traumatic events including death of a loved one, witnessing violence, and witnessing accidents.
2.2. Sample 2 participants (confirmatory sample)
Using procedures identical to Sample 1, 324 women were recruited. Participants were on average 19.57 (SD = 4.20) years old. Sixty-five percent (65.4%) were Caucasian, 25.9% Asian American, and 8.7% were from other backgrounds. Forty-five percent (44.8%) reported experiencing a DSM-IV Criterion A trauma using the PSD (Foa et al., 1997). Of these, 16.2% reported a serious accident, 17.9% reported a life-threatening illness, 22.5% a sexual or non-sexual assault, 13.3% a natural disaster, and 30.1% reported other traumatic events, including death of a loved one, witnessing violence, and witnessing accidents.
2.3. Sample 3 participants (generalization, trauma-exposed sample)
One hundred and five women who had experienced a PTE event were recruited via advertisements seeking trauma-exposed women in two large metropolitan areas. Mean age was 31.58 years (SD = 12.02). Seventy-five percent (75.2%) of the participants were Caucasian, 18.1% African American, and 6.7% from other backgrounds. Overall, 68.8% of the sample had not completed college, and 44.1% earned less than $20,000 annual household income. Although all participants reported experiencing a PTE, 80% reported experiencing a DSM-IV qualifying Criterion A trauma on the PDS (Foa et al., 1997). When indicating which event bothered them the most, of these women, 1.9% reported a serious accident, 1.9% reported a life-threatening illness, 76.7% a sexual or non-sexual assault, 1.9% a natural disaster, and 17.6% reported other traumatic events, including death of a loved one, witnessing violence, and witnessing accidents.
Data from these three samples were collected as part of separate studies all examining treatment preference (Feeny, Zoellner, & Kahana, in press; Feeny, Zoellner, Mavissakalian, & Roy-Byrne, in press; Zoellner et al., 2003). In the present study, these samples were utilized in secondary data analysis to allow identification of potential stable predictors of treatment-related beliefs and preferences across multiple samples.
2.4. Materials
2.4.1. Treatment rationales
Treatment rationales for both sertraline (SER) and prolonged exposure (PE) included the following information: efficacy and background for treatment, a description of treatment procedures, and potential side effects. Whenever possible, wording across the rationales was matched, with the exception of side effect statements, which were based on existing literature (Brady et al., 2000; Foa & Rothbaum, 1998). Rationales were derived from those published in Zoellner et al. (2003) and are available upon request. SER and PE rationales did not differ in terms of sentence structure, grade level, and reading ease based on indices from Microsoft Word (Microsoft Inc., 2000). For the undergraduate samples, in order to anchor the treatment choices to trauma exposure and subsequent symptoms, participants read a vignette, using an “imagine self” perspective (Davis et al., 2004), describing the occurrence of a sexual assault and accompanying PTSD symptoms and functional impairment. With this vignette in mind (see Cochran et al., 2008) treatment beliefs and preference were solicited.
2.5. Treatment preference/beliefs measures
2.5.1. Treatment beliefs
To assess perceptions of treatment effectiveness and personal attitudes concerning the treatment descriptions, participants completed both the Credibility Scale (CS; Addis et al., 1999) and personal reactions to the rationales (PRR; Addis et al., 1999) for both the SER and PE treatment rationales. The Credibility Scale (CS) contains 7 items (e.g., “How logical does this therapy seem to you?”) rated on a 7-point scale from 1 (not at all) to 7 (extremely) with higher scores indicating higher credibility (range 7–49). Overall, the credibility scale assesses how much the participant generally perceives the treatment to be logical, scientifically based, and effective. In Addis et al. (1999), its internal consistency was strong (alphas = 0.87–0.93). The personal reactions to the rationales (PRR) contains 5 items (e.g., “If you had PTSD and went for treatment, how helpful do you think this therapy would be for you?”) rated on a 7-point scale from 1 (not at all) to 7 (extremely) with higher scores indicating more positive personal reactions (range 5–35). Overall, the PRR scale assesses how much the participant perceives the treatment will help them personally. In Addis et al. (1999), the PRR internal consistency was also strong (alphas = 0.94–0.95).
CS and PRR scales were combined into a composite variable used to assess “treatment beliefs” for either SER or PE. Internal consistency for both SER treatment-related beliefs and PE treatment-related beliefs was high for these composite scores with alpha coefficients ranging from 0.93 to 0.96 across all samples. Means, standard deviations, and ranges across all samples are found in Table 1.
Table 1.
Means, standard deviation, and range on psychopathology and treatment rationale measures
| Measure | Sample 1 |
Sample 2 |
Sample 3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | M | SD | Range | |
| Psychopathology | |||||||||
| Depression (BDI) | 7.27 | 6.34 | 0–31 | 7.61 | 6.58 | 0–41 | 17.01 | 11.53 | 0–53 |
| Anxiety Sensitivity (ASI) | 36.45 | 9.57 | 19–69 | 35.62 | 9.83 | 16–69 | 44.27 | 13.14 | 17–80 |
| State Anxiety (STAI-State) | 37.17 | 11.27 | 20–68 | 45.90 | 5.28 | 27–60 | 50.42 | 12.90 | 23–76 |
| Trait Anxiety (STAI-Trait) | 40.75 | 11.53 | 20–77 | 46.99 | 4.91 | 35–67 | 53.50 | 13.25 | 28–79 |
| PTSD Severity (PDS)a | 7.57 | 7.91 | 0–38 | 7.61 | 9.19 | 0–44 | 25.39 | 11.64 | 0–47 |
| PTSD Diagnosis (PDS) (%) | 9.9 | 9.3 | 67.3 | ||||||
| Treatment rationales | |||||||||
| SER credibility | 22.80 | 7.68 | 7–44 | 26.33 | 7.80 | 9–47 | 28.00 | 9.79 | 7–49 |
| SER personal reactions | 12.10 | 5.56 | 5–30 | 15.46 | 6.35 | 5–31 | 15.35 | 8.18 | 5–35 |
| SER belief composite | 5.66 | 2.10 | 2–12 | 6.21 | 2.40 | 2–14 | 7.07 | 2.91 | 2–14 |
| PE credibility | 35.73 | 7.15 | 11–48 | 33.53 | 6.45 | 9–49 | 35.77 | 9.02 | 8–49 |
| PE personal reactions | 26.86 | 6.13 | 5–35 | 24.56 | 5.46 | 8–35 | 26.65 | 7.45 | 5–35 |
| PE belief composite | 10.45 | 2.20 | 3–14 | 10.47 | 2.20 | 2–14 | 10.44 | 2.69 | 2–14 |
PTSD total symptoms is calculated for those reporting a Criterion A event. PDS = Post-Traumatic Stress Disorder Diagnostic Scale (range 0–51), BDI = Beck Depression Inventory (range 0–63), ASI = Anxiety Sensitivity Inventory (range 16–80), STAI = State-Trait Anxiety Inventory (range 20–80).
2.5.2. Forced choice
Participants were also asked, “If you had a choice between individual therapy, medication, or no treatment to help you with trauma-related symptoms (e.g., nightmares, upsetting thoughts, fear) which would you choose?” For analysis purposes, when examining preference for SER, data were coded as 1 = SER, 0 = PE/no treatment; and when examining preference for PE, data were coded as 1 = PE, 0 = SER/no treatment.
2.6. Psychopathology measures
The following self-report measures were utilized: PDS (Foa et al., 1997); Beck Depression Inventory (BDI; Beck, Ward, Mendelsohn, Mock, & Erbaugh, 1961); State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970); and Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986). Only those reporting a Criterion A event based on the PDS were considered eligible to report PTSD symptoms. Given potential fears of treatment side effects for both SER and PE and the potentially reactive nature of discussing trauma-related treatments, measures of State Anxiety (STAI) and Anxiety Sensitivity (ASI) were included. See Table 1 for descriptive statistics for each sample.
2.7. Procedure
After informed consent, participants completed demographic and psychopathology measures. Samples 1 and 2 then read “if this happened to you, what would you do?” scenario describing a sexual assault and accompanying psychological/functioning reactions. Sample 3 did not read this scenario, as they were asked to give their treatment preferences based on their own real-world traumatic experiences. Next, participants read (Sample 1, 2) or viewed on videotape (Sample 3) either the SER or PE description. The videotape mirrored the written descriptions, except that a clinician provided the rationales to provide a more realistic clinical experience. Participants then rated credibility (CS) of, and their personal reactions (PRR) to, the treatment option. The process was then repeated for the second rationale. After reading/viewing and rating both rationales, presented in counterbalanced order, participants chose among PE, SER, or no treatment. Participants were then debriefed and compensated with course credit (Samples 1 and 2) or with $20 per hour (Sample 3).
2.8. Data analytic strategy
Sample 1 was used for path model generation. Prediction of PE and SER were examined separately, given the divergence of potential predictors reported in the literature and given that three rather than two choices were given to all participants. Demographics (age, years of education, income, ethnicity, history of trauma exposure) and psychopathology (anxiety sensitivity, PTSD Severity, depression severity, trait anxiety, and state anxiety) were examined as direct and indirect predictors of treatment-related beliefs and treatment preference. To identify the final set of predictors, for highly correlated variables, the one with the highest correlation with treatment beliefs or preference was selected. Variables without significant correlation with treatment-related beliefs or treatment preference were dropped from the model. Missing data were imputed using the pairwise covariation matrix in EQS 6.1 for Windows, with less than 3% of cases having three or more missing variables across samples. The exploratory model that emerged from Sample 1 then underwent confirmatory analysis using Sample 2. Finally, to examine the generalization of the derived model to a sample of community trauma-exposed women, a final generalization, confirmatory analysis was undertaken using Sample 3. All path modeling was conducted using EQS 6.1 for Windows.
3. Results
3.1. Exploratory sample (Sample 1)
Initially, associations were examined among treatment choice (PE, where 1 = Choice of PE, 0 = no treatment or SER; SER, where 1 = Choice of SER, 0 = no treatment or PE), treatment-specific beliefs (CS, PRR), and measured demographic and psychopathology variables described above. Zero-order correlations are presented in Table 2 for key variables. In this sample, 87.4% preferred PE, 6.9% sertraline, and 5.7% no treatment. Based on the procedures described above, an exploratory path model was generated. This model predicted a direct pathway from treatment-specific related beliefs (CS, PRR) to treatment preference (PE, SER). The model also predicted five indirect pathways, minority status (0 = Caucasian, 1 = non-Caucasian), Anxiety Sensitivity (ASI), PTSD symptoms (PDS), depression (BDI), and State Anxiety (STAI-S) to treatment preference through treatment-specific beliefs.
Table 2.
Zero-order correlations among study variables across the three samples
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|
| Sample 1 | |||||||||
| 1. BDI | - | ||||||||
| 2. PDS | 0.40* | - | |||||||
| 3. ASI | 0.41* | 0.21* | - | ||||||
| 4. STAI-S | 0.59* | 0.26* | 0.28* | - | |||||
| 5. Minority | 0.17* | 0.02 | 0.16* | 0.15* | - | ||||
| 6. Belief PE | −0.06 | −0.12 | −0.08 | −0.17* | −0.14* | - | |||
| 7. Belief SER | −0.04 | −0.08 | 0.01 | 0.03 | 0.09 | −0.24* | - | ||
| 8. Choice PE | −0.15* | −0.16* | −0.06 | −0.10 | −0.10 | 0.50* | −0.28* | - | |
| 9. Choice SER | 0.16* | 0.17* | 0.09 | 0.07 | 0.00 | −0.38* | 0.39* | −0.72* | - |
| Sample 2 | |||||||||
| 1. BDI | - | ||||||||
| 2. PDS | 0.49* | - | |||||||
| 3. ASI | 0.44* | 0.29* | - | ||||||
| 4. STAI-S | −0.19 | −0.02 | 0.03 | - | |||||
| 5. Minority | −0.05 | 0.05 | 0.02 | 0.08 | - | ||||
| 6. Belief PE | −0.14 | −0.15* | 0.01 | 0.14* | 0.17* | - | |||
| 7. Belief SER | 0.13* | 0.02 | 0.13* | −0.04 | −0.16* | 0.08 | - | ||
| 8. Choice PE | −0.14* | −0.15* | 0.01 | 0.09 | 0.02 | 0.30* | −0.13* | - | |
| 9. Choice SER | 0.11 | 0.08 | 0.07 | −0.01 | 0.03 | −0.11 | 0.24* | −0.75* | - |
| Sample 3 | |||||||||
| 1. BDI | - | ||||||||
| 2. PDS | 0.70* | - | |||||||
| 3. ASI | 0.46* | 0.39* | - | ||||||
| 4. STAI-S | 0.65* | 0.59* | 0.38* | - | |||||
| 5. Minority | 0.15 | 0.15 | 0.19 | 0.18 | - | ||||
| 6. Belief PE | −0.13 | −0.11 | −0.23* | −0.07 | −0.06 | - | |||
| 7. Belief SER | 0.10 | 0.12 | 0.14 | −0.05 | 0.14 | −0.11 | - | ||
| 8. Choice PE | −0.24* | −0.15 | −0.13 | −0.13 | −0.05 | 0.59* | −0.35* | - | |
| 9. Choice SER | 0.26* | 0.21* | 0.15 | 0.15 | 0.05 | −0.52* | 0.44* | −0.88* | - |
p < 0.05.
Note: PTSD total symptoms is calculated for those reporting a Criterion A event. BDI = Beck Depression Inventory; PDS = Post-Traumatic Stress Disorder Diagnostic Scale; STAI = State-Trait Anxiety Inventory; ASI = Anxiety Sensitivity Inventory; Minority = 1, Non-Caucasian, 0, Caucasian; Belief PE = Composite CS and PRR for PE; Belief SER = Composite CS and PRR for SER.
Using maximum likelihood estimation, for both PE and SER, the independent model that tests the hypothesis that all variables are uncorrelated was easily rejected, both for PE, χ2 (21, N = 273) = 295.47, p < 0.001, and for SER, χ2 (21, N = 273) = 306.16, p < 0.001. Initial model fit for both PE and SER treatment preference was evaluated with the chi-square goodness-of-fit statistic, Bentler-Bonett Normed Fit Index (NFI), comparative fit index (CFI), Lisrel Goodness-of-Fit Index (GFI), root mean square residual (SRMR), and root mean square error of approximation (RMSEA). For NFI, CFI, and GFI, high values, greater than 0.90, are indicative of a good-fitting model. For SRMR and RMSEA, values less than 0.05 are considered good and adequate fits to the data (Hu & Bentler, 1998), respectively. Support for both of the hypothesized models was next tested and found. As seen in Table 3, a chi-square difference test indicated a significant improvement in fit between the independent models and the hypothesized models.
Table 3.
Preference for psychotherapy or pharmacological treatment: fit indices for exploratory, confirmatory, and generalization models
| Model | χ2 | NFI | CFI | GFI | SRMR | RMSEA | χ2 difference test |
|---|---|---|---|---|---|---|---|
| Psychotherapy Treatment Model | |||||||
| 1. Sample 1: PE Model | |||||||
| Model 1: Hypothesized | 8.16 | 0.976 | 0.990 | 0.992 | 0.030 | 0.048 | |
| Model 2: Final Model - path added | 2.95 | 0.991 | 1.00 | 0.997 | 0.015 | 0.000 | M1 – M2 = 5.21* |
| Choice predicted from depression | |||||||
| 2. Sample 2: Confirmatory | 4.21 | 0.986 | 0.999 | 0.996 | 0.017 | 0.013 | |
| 3. Sample 3: Generalization | 1.31 | 0.994 | 1.00 | 0.996 | 0.015 | 0.000 | |
| Pharmacological Treatment Model | |||||||
| 1. Sample 1: SER Model | |||||||
| Model 1: Hypothesized | 19.59* | 0.936 | 0.949 | 0.981 | 0.054 | 0.104 | |
| Model 2: Final Model - path added | 6.40 | 0.979 | 0.992 | 0.993 | 0.021 | 0.047 | M1 – M2 = 13.19* |
| Choice predicted from PTSD Severity | |||||||
| 2. Sample 2: Confirmatory | 3.91 | 0.986 | 1.00 | 0.997 | 0.018 | 0.000 | |
| 3. Sample 3: Generalization | 3.52 | 0.983 | 1.00 | 0.991 | 0.026 | 0.000 |
p < 0.05.
Note: NFI = Benler-Bonnet Normed Fit Index; CFI = Comparative Fit Index; GFI = Lisrel Fit Index; SRMR = Standardized root mean square residual; RMSEA = Root Mean Square Error of Approximation. For PE Model, Sample 1 (PE (n = 239) vs SER/No Tx (n = 34)), Sample 2 (PE (n = 273) vs SER/No Tx (n = 51)), and Sample 3 (PE (n = 83) vs SER/No Tx (n = 22)). For SER Model, Sample 1 (SER (n = 19) vs PE/No Tx (n = 254)), Sample 2 (SER (n = 31) vs PE/No Tx (n = 293)), and Sample 3 (SER (n = 18) vs PE/No Tx (n = 87)).
In an attempt to develop a better fitting and more parsimonious model, post hoc model modifications were performed. On the basis of the Lagrange multiplier test, the Wald test, and theoretical relevance, for both the PE and SER models, one path was added and none were deleted. Specifically, in the PE model, a direct path was added between depression and choice of PE; and in the SER model, a direct path was added between PTSD and choice of SER. Table 3 presents the models tested. The final model for both PE (χ2 (4, N = 273) = 2.95, p = 0.57) and SER (χ2 (4, N = 273) = 6.40, p = 0.17) fit the data well. In the PE model, 27% of the variance in treatment choice was accounted for by its predictors and 6% of the variance in treatment beliefs was accounted for by its predictors. In the SER model, 19% of the variance in choice was accounted for by its predictors and 2% of the variance in treatment beliefs was accounted for by its predictors. Because post hoc modifications were conducted, correlations between hypothesized model and final model estimates were calculated. For both PE and SER models, rs(6) = 1.00, p < 0.001, the relationship among the parameters did not change as a result of the modification.
3.2. Confirmatory (Sample 2) and generalization (Sample 3) samples
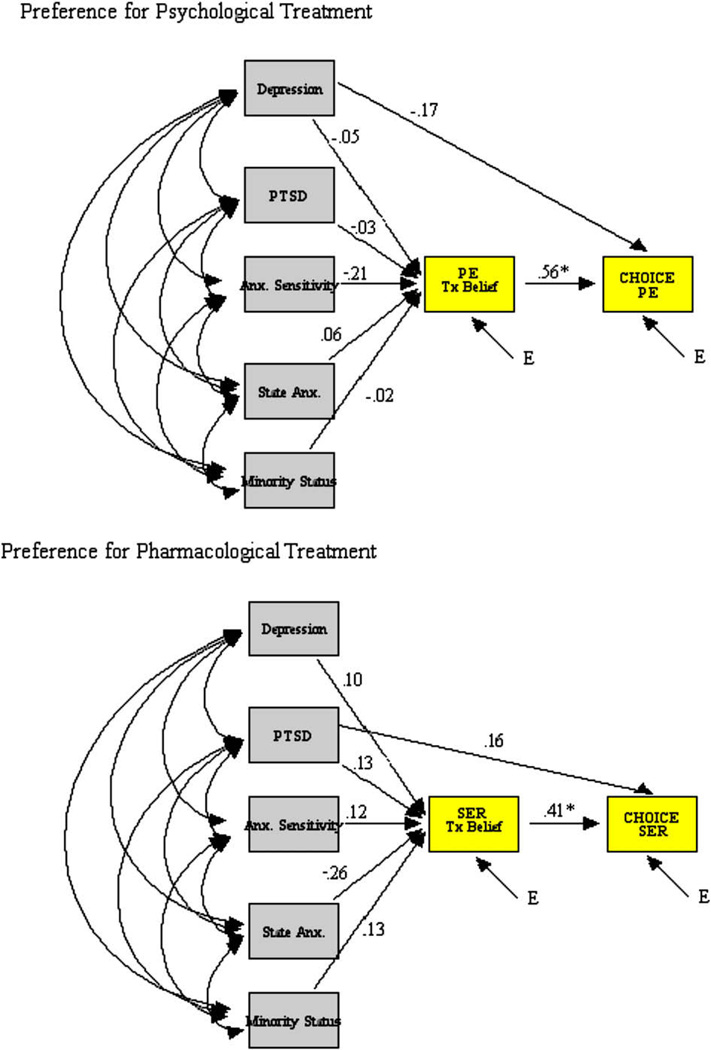
For both Samples 2 and 3, zero-order correlations are presented in Table 2. In Sample 2, 84.3% preferred PE; 9.6%, sertraline; and 6.2%, no treatment. In Sample 3, 79.4% preferred PE; 16.7%, sertraline; and 3.9%, no treatment. Fit indices for both confirmatory and generalization models are presented in Table 3, with standardized and unstandardized coefficients presented in Table 4. Within the confirmatory sample (Sample 2), both the final model for both PE (χ2 (4, N = 324) = 4.21, p = 0.38) and SER (χ2 (4, N = 324) = 3.91, p = 0.42) fit the data well. In the PE model, 23% of the variance in treatment choice was accounted for by its predictors and 7% of the variance in treatment beliefs was accounted for by its predictors. In the SER model, 21% of the variance in choice was accounted for by its predictors and 5% of the variance in treatment beliefs was accounted for by its predictors. Similarly, in the trauma-exposed generalization sample (Sample 3), the final model for both PE (χ2 (4, N = 105) = 1.31, p = 0.86) and SER (χ2 (4, N = 105) = 3.52, p = 0.48), as depicted in Fig.1, fit the data well. In the PE model, 37% the variance in choice was accounted for by its predictors and 5% of the variance in treatment beliefs was accounted for by its predictors. In the SER model, 21% of the variance in treatment choice was accounted for by its predictors and its predictors accounted for 7% of the variance in treatment beliefs.
Table 4.
Unstandardized and standardized coefficients for final models
| Model | Sample 1 |
Sample 2 |
Sample 3 |
|||
|---|---|---|---|---|---|---|
| B | β | B | β | B | β | |
| Psychotherapy Treatment Model | ||||||
| Choice PE | ||||||
| Belief Tx (PE) | 0.08 | 0.49* | 0.08 | 0.46* | 0.09 | 0.56* |
| Depression (BDI) | 0.01 | −0.12* | 0.00 | −0.08 | −0.01 | −0.17* |
| Belief Tx (PE) | ||||||
| Depression (BDI) | 0.04 | 0.11 | −0.03 | −0.08 | −0.01 | −0.05 |
| PTSD Severity (PDS) | −0.03 | −0.12 | −0.03 | −0.12 | −0.01 | −0.03 |
| Anxiety Sensitivity (ASI) | −0.00 | −0.01 | 0.02 | 0.07 | −0.04 | −0.21 |
| State Anxiety (STAI-S) | −0.04 | −0.18* | 0.04 | 0.10 | 0.01 | 0.06 |
| Minority status (1 = Minority) | −0.56 | −0.12* | −0.71 | −0.15* | −0.10 | −0.02 |
| Pharmacological Treatment Model | ||||||
| Choice SER | ||||||
| Belief Tx (SER) | 0.05 | 0.41* | 0.06 | 0.45* | 0.05 | 0.41* |
| PTSD Severity (PDS) | 0.01 | 0.20* | 0.00 | 0.07 | 0.01 | 0.16 |
| Belief Tx (SER) | ||||||
| Depression (BDI) | −0.03 | −0.08 | 0.04 | 0.12 | 0.02 | 0.10 |
| PTSD (PDS) | −0.02 | −0.09 | −0.02 | −0.07 | 0.03 | 0.13 |
| Anxiety Sensitivity (ASI) | 0.00 | 0.02 | 0.02 | 0.09 | 0.03 | 0.12 |
| State Anxiety (STAI-S) | 0.02 | 0.08 | 0.00 | −0.01 | −0.06 | −0.26* |
| Minority status (1 = Minority) | 0.39 | 0.09 | 0.79 | 0.16* | 0.85 | 0.13 |
p < 0.05.
Figure 1.
Psychotherapy and pharmacological models with standardized coefficients for the generalization sample (Sample 3).
3.3. Direct and indirect effects
Across samples, there were direct effects of treatment-related beliefs on treatment choice for both PE (standardized coefficients for Sample 1 = 0.49, Sample 2 = 0.46, Sample 3 = 0.56) and SER models (standardized coefficients for Sample 1 = 0.41, Sample 2 = 0.45, Sample 3 = 0.41), suggesting that credibility and personal reactions toward a treatment predicted treatment choice. For the PE model, there was also a small direct effect of depression on choice (standardized coefficients for Sample 1 = −0.12, Sample 3 = −0.17), with increased depression associated with decreased likelihood of choosing PE. For the SER model, there was also a small direct effect of PTSD on treatment choice (standardized coefficients for Sample 1 = 0.20, Sample 3 = 0.16, z = 1.85, ns), with increased PTSD Severity associated with increased likelihood of choosing SER.
Within the PE model, for both of the undergraduate samples, minority status had a small indirect effect on treatment choice through treatment beliefs (standardized coefficients for Sample 1 = −0.12, Sample 2 = −0.15). Specifically, minority status was associated with lower positive beliefs about the psychotherapy. Consistent with this, in the SER model, in Sample 2 (standardized coefficient = 0.16), minority status was associated with increased positive beliefs regarding the pharmacotherapy. Finally, anxiety also had a small indirect effect on treatment choice through treatment beliefs. Within the PE model, greater state anxiety (standardized coefficient for Sample 1 = −0.18) and greater Anxiety Sensitivity (standardized coefficient for Sample 3 = −0.21, z = 1.91, ns) were associated with lower positive beliefs about the psychotherapy. Within the SER model, greater state anxiety (standardized coefficient for Sample 3 = −0.26) was also associated with lower positive beliefs about the pharmacotherapy.
4. Discussion
Across models and in multiple samples, treatment-related beliefs, specifically personal reactions and credibility of a treatment, were the strongest predictors of treatment preference. More severe psychopathology, either depression or PTSD, was also directly associated with either less likelihood of choosing psychotherapy, or increased likelihood of choosing pharmacotherapy. Notably, other predictors such as minority status and state anxiety accounted for only modest prediction of treatment-related beliefs and only indirectly predicted treatment choice. Overall, the models of treatment preference for either psychotherapy (i.e., prolonged exposure) or pharmacotherapy (i.e., sertraline), initially derived from an undergraduate sample of women, held up well across confirmation in a second undergraduate female sample and in a third trauma-exposed, community sample, suggesting a general robustness for the final path models.
Although seemingly intuitive, personal reactions and credibility of a treatment were the strongest predictors of treatment preference. That is, the more that someone reacted positively to a treatment and thought the treatment was credible, the more likely they were to choose that treatment. This strong association, well above other potential predictors, clearly argues for a more thorough understanding of what factors contribute to more positive or negative beliefs about various treatment options. Such beliefs have been shown to influence treatment seeking, adherence, and outcome for depression and psychotic disorders (e.g., Lobban, Barrowclough, & Jones, 2003; Sullivan et al., 2003). It is important to note that beliefs about treatments are most likely not unitary constructs, but instead multifaceted, dynamic constructs, made up of a variety of components and potentially changing over time (e.g., Levinthal & Coleman, 1997; Levinthal, Diefenbach, & Levinthal, 1992). Therefore, these components may contribute differentially to treatment preferences and treatment behavior. For instance, in a recent paper on treatment adherence, Spoont, Sayer, and Nelson (2005) suggested that aspects of treatment beliefs might contribute in different ways depending on the treatment under consideration. Specifically, they reported that patients’ own explanatory models of PTSD were related to psychiatric medication use; whereas, beliefs about consequences of their disorder predicted participation in psychotherapy. Findings such as this clearly argue that, to understand patients’ treatment-related behavior, we need a more nuanced understanding of mental health related beliefs.
The only other direct predictors of treatment preference were severity of depression and PTSD. When predicting preference for the psychotherapy, higher depression severity was associated with a decreased likelihood of choosing prolonged exposure. Further, PTSD Severity was associated with an increased likelihood of choosing the sertraline. Given the strong association between PTSD and depression, it may be that more severe psychopathology in general, or comorbidity with depression, is associated with preferences for pharmacological interventions. Consistent with this interpretation, Benkert et al. (1997), when examining an individual’s acceptance or rejection of the use of psychotropic drugs, reported that approval of pharmacotherapy depended on an assessment of the severity of the disease. It may be that those with more severe symptoms may want more immediate relief from their distress or may feel unable or unmotivated to exert the effort required to engage and participate in psychotherapy. This is consistent with conceptualizations of depression and its impact on positive affect and motivation systems (e.g., Clark & Watson, 1991). This said, it should be noted that the vast majority of all participants, even those within the more symptomatic third sample, preferred psychotherapy.
Importantly, none of the demographic variables emerged as strong predictors of treatment-related beliefs nor did they directly predict treatment preference. This low predictive ability and lack of stability is consistent with the growing treatment preference literature in which some demographic factors emerge as predictors in some samples and not in others (e.g., Hazlett-Stevens et al., 2002; Roy-Byrne et al., 2003; Wagner et al., 2005). Only minority status, that is not being Caucasian, emerged as a modest predictor, having less positive beliefs about the psychotherapy (Sample 1, 2) and more positive beliefs about the pharmacotherapy (Sample 2). In contrast to this, in several preference studies (Dwight-Johnson, Sherbourne, Liao, & Wells, 2000; Hazlett-Stevens et al., 2002; Wagner et al., 2005), ethnic minorities indicated being less receptive to medication than Caucasians. Similarly, in the broader ethnicity and mental health services literature, Sue et al. (e.g., Sue, Fujino, Li-tze, Takeuchi, & Zane, 1991) have consistently shown minority status (i.e., Asian Americans) to be related to under-utilization of health care. The composition of samples in this study differed greatly, with a larger proportion of Asian Americans in the undergraduate sample and African Americans in the community sample, raising the issue that minority status, or ethnicity, should not be treated as a monolithic entity. Moreover, we did not assess specific cultural variables such as acculturation, ethnic identity, or mental health beliefs about the role of the client and therapist that may underlie perceptions of treatment credibility. For example, in an analogue study, Wong et al. (2003) showed that cultural identity and self-construal (i.e., independence and interdependence), not ethic status per se, moderated perceived credibility of treatment rationales for depression. Thus, it is essential to move beyond studying basic ethnic categories and begin to examine culturally-based factors that may meaningfully shape treatment preferences (Betancourt & Lopez, 1993; Wong et al., 2003).
When interpreting the current findings, it is important to note several limitations. First, two samples in the present study, where the models were derived and confirmed, were female college students with limited ranges on factors such as age, education, income, and ethnicity. Accordingly, future studies should examine potential influences on preference in more diverse samples, including both men and women. Further, individuals with PTSD from combat exposure may respond with different treatment preferences given the unique aspects of military culture that may affect treatment seeking (e.g., stigma). Second, the present study did not systematically examine other potentially important factors influencing treatment beliefs such as people’s explanatory models for their symptoms, beliefs about the consequences of their symptoms, and perceived necessity of the treatment, that may more directly underlie treatment-related beliefs. It may be that a qualitative approach and analysis of individuals’ beliefs may help identify key factors influencing beliefs about psychotherapy and pharmacotherapy for trauma-related symptoms. With this, it is not entirely clear that “beliefs” are not inextricably intertwined with “preferences;” however, it is entirely possible to have strong positive beliefs about various therapies and yet have a clear preference for one vs the other. Third, we examined preference for only two forms of treatment for trauma-related symptoms, prolonged exposure and sertraline; and thus, the path models may not hold for other treatment options. We further did not provide detailed information regarding the option of not seeking treatment. Similarly, the forced choice scenario, although letting us look directly at specific treatment preferences for one option or the other, does not explore the possibility of preference for combined treatment or the other forms of treatment. We also did not include information about prior treatment history in our models, and it may be that such history indirectly or directly relates to treatment choices. Finally, for the undergraduate samples, treatment preference was hypothetical; and accordingly, more weight may need to be placed on the generalization, community trauma-exposed model. Given the general consistency across models however, similar factors may impact hypothetical and real treatment preferences, or it may be that women, even prior to trauma exposure, have strong opinions regarding psychotherapy and pharmacotherapy for trauma-related symptoms.
In terms of clinical implications, as seen in our path models, higher severity of PTSD and depression symptoms, or their comorbidity, may make engaging in trauma-specific psychotherapy less desirable than engaging in pharmacotherapy. For those with more severe psychopathology who are more interested in receiving pharmacotherapy, it may be beneficial to include a discussion of clients’ issues surrounding the psychotherapy and to discuss the possibility of a combined or stepped treatment approach. Indeed, such augmentation strategies have been shown to be useful among partial responders to sertraline (Rothbaum et al., 2006).
Given that treatment-related beliefs appear to be the most robust predictors of treatment preferences for trauma-related symptoms, clinicians ought to be especially attuned to their patients’ personal reactions to and perceptions of the credibility of various treatment options. Consistent with Wagner et al. (2005), rather than making a priori assumptions about beliefs and expectations regarding a treatment option, ideographic clinical assessment of these beliefs and more thorough orientation to treatment options are likely critical for increasing treatment adoption and adherence. Speculating beyond our data, client-treatment “mismatches” may be fundamentally clashes in belief systems. The importance of understanding beliefs is further underscored by evidence that individuals who agree with treatment rationales improve more quickly and have better outcomes than those who do not (e.g., Addis & Carpenter, 1999; Addis & Jacobson, 2000; Ilardi & Craighead, 1994). Psychoeducation about the treatment approach may help mitigate these clashes for those who endorse significant doubts about or disagreement with the approach. With that said, however, we do not yet know the extent to which perceptions about treatment are modifiable, nor the extent to which such beliefs are actually shaped by what clinicians (or rationales) say, as opposed to being shaped by pre-existing beliefs that clients bring with them to the office.
Ultimately, from a public health perspective, a better understanding of patients’ treatment-related beliefs may inform knowledge about treatment barriers and shape public education campaigns or outreach efforts designed at engaging trauma survivors in need of treatment.
Acknowledgments
Preparation of this manuscript was supported in part by a grant to Drs. Feeny and Zoellner from the Anxiety Disorders Association of America. The authors would like to acknowledge Larry Pruitt, Bryan Cochran, Matt Wilms, and Seiya Fukuda for their contribution to the collection and scoring of the data at the University of Washington. The authors would also like to acknowledge Eric Youngstrom, Ph.D., for help with data collection procedures and for his statistical advice. The authors would also like to thank Peter Roy-Byrne, MD, and Matig Mavissakalian, MD, for their mentorship on the ADAA grant.
Footnotes
The term PTE used here and throughout the manuscript is used in convention with the larger trauma literature to denote the presence of an event that has the potential to meet DSM-IV Criterion A.
References
- Addis ME, Carpenter KM. Why, why, why?: reason giving and rumination as predictors of response to activation-and insight oriented treatment rationales. Journal of Clinical Psychology. 1999;55(7):881–894. doi: 10.1002/(sici)1097-4679(199907)55:7<881::aid-jclp9>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Addis ME, Jacobson NS. A closer look at the treatment rationale and homework compliance in cognitive therapy for depression. Cognitive Therapy and Research. 2000;24:313–326. [Google Scholar]
- Angelo FN, Miller HE, Zoellner LA, Feeny NC. Why prefer one treatment over another?: a qualitative analysis of women’s reasons for treatment choice in chronic PTSD. Behavior Therapy. 2008;39:13–21. doi: 10.1016/j.beth.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH. Psychological treatments. American Psychologist. 2004;59:869–878. doi: 10.1037/0003-066X.59.9.869. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Becker CB, Darius E, Schaumberg K. An analog study of patient preferences for exposure versus alternative treatments for posttraumatic stress disorder. Behavior Therapy. 2007 doi: 10.1016/j.brat.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Bedi N, Chilvers C, Churchill R, Dewey M, Duggan C, Fielding K, et al. Assessing effectiveness of treatment of depression in primary care: partially randomized preference trial. British Journal of Psychiatry. 2000;177:312–318. doi: 10.1192/bjp.177.4.312. [DOI] [PubMed] [Google Scholar]
- Benkert O, Graf-Morgenstren M, Hillert A, Sandmann J, Ehmig S, Weissbecker H, et al. Public opinion on psychotropic drugs: an analysis on factors influencing acceptance or rejection. The Journal of Nervous and Mental Disease. 1997;185:151–158. doi: 10.1097/00005053-199703000-00004. [DOI] [PubMed] [Google Scholar]
- Betancourt H, Lopez SR. The study of culture, ethnicity and race in American psychology. American Psychologist. 1993;48:629–637. [Google Scholar]
- Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. Journal of the American Medical Association. 2000;283(14):1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cochran B, Pruitt L, Fukuda S, Zoellner LA, Feeny NC. Prolonged exposure and medication rationales for the treatment of PTSD: what factors predict treatment choice? Journal of Interpersonal Violence. 2008;23:276–291. doi: 10.1177/0886260507309836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JRT, Rothbaum BO, van der Kolk B, Sikes CR, Farfel GM. Multicenter, double blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Archives of General Psychiatry. 2001;58:485–492. doi: 10.1001/archpsyc.58.5.485. [DOI] [PubMed] [Google Scholar]
- Davis M, Sonderlund T, Cole J, Gadol E, Kute M, Myers M, et al. Cognitions associated with attempts to empathize: how do we imagine the perspectives of another? Personality and Social Psychology Bulletin. 2004;20:1625–1635. doi: 10.1177/0146167204271183. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. Journal of General Internal Medicine. 2000;15:527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Kahana SY. Providing a treatment rationale for PTSD: does what we say matter? Behaviour Research and Therapy. doi: 10.1016/j.brat.2009.06.007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Mavissakalian MR, Roy-Byrne PP. What would you choose? Sertraline or prolonged exposure for chronic PTSD. Depression and Anxiety. 26(6) doi: 10.1002/da.20588. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox LH, Perry K. The validation of a self-report measure of PTSD: the PTSD Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SL, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape. New York: Guilford Press; 1998. [Google Scholar]
- Gavrilovic JJ, Schutzwohl M, Fazel M, Priebe S. Who seeks treatment after a traumatic event and who does not? A review of findings on mental health service utilization. Journal of Traumatic Stress. 2005;18:595–605. doi: 10.1002/jts.20068. [DOI] [PubMed] [Google Scholar]
- Hazlett-Stevens H, Craske MG, Roy-Byrne PP, Sherbourne CD, Stein MB, Bystritsky A. Predictors of willingness to consider medication and psychosocial treatment for panic disorder in primary care patients. General Hospital Psychiatry. 2002;24:316–321. doi: 10.1016/s0163-8343(02)00204-9. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology Science and Practice. 1994;1:138–156. [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinthal H, Coleman S. Quality of life: a process view. Psychology & Health. 1997;12(6):753–767. [Google Scholar]
- Levinthal H, Diefenbach M, Levinthal EA. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognitive Therapy and Research. 1992;16(2):143–163. [Google Scholar]
- Lobban F, Barrowclough C, Jones S. A review of the role of illness models in severe mental illness. Clinical Psychology Review. 2003;23:171–196. doi: 10.1016/s0272-7358(02)00230-1. [DOI] [PubMed] [Google Scholar]
- MicrosoftInc. Microsoft Office 2000 Service Pack 2. [Computer Software] Redmond, Washington: Microsoft Corporation; 2000. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the predictions of fearfulness. Behaviour Research & Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Cahill SP, Foa EB, Davidson JRT, Compton J, Connor KM, et al. Augmentation of sertraline with prolonged exposure in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress. 2006;19:625–638. doi: 10.1002/jts.20170. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Berliner L, Russo J, Zatzick D, Pitman R. Treatment preferences and determinants in victims of sexual and physical assault. Journal of Nervous and Mental Disorders. 2003;191:161–165. doi: 10.1097/01.NMD.0000055343.62310.73. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for post-traumatic stress disorder in women: a randomized controlled trial. Journal of the American Medical Association. 2007;297(8):820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Seligman ME. The effectiveness of psychotherapy: the Consumer Reports study. American Psychologist. 1995;50:956–974. doi: 10.1037//0003-066x.50.12.965. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Spoont M, Sayer N, Nelson D. PTSD and treatment adherence. The Journal of Nervous and Mental Disease. 2005;193:515–522. doi: 10.1097/01.nmd.0000172474.86877.2b. [DOI] [PubMed] [Google Scholar]
- Street LL, Niederehe G, Lebowitz BD. Toward greater public health relevance for psychotherapeutic intervention research: an NIMH workshop report. Clinical Psychology: Science and Practice. 2000;7(2):127–137. [Google Scholar]
- Sue S, Fujino DC, Li-tze H, Takeuchi DT, Zane NWS. Community mental health services for ethnic minority groups: a test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology. 1991;59:533–540. doi: 10.1037//0022-006x.59.4.533. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, Katon WJ, Russo JE, Frank E, Barrett JE, Oxman TE, et al. Patient beliefs predict response to paroxetine among primary care patients with dysthymia and minor depression. Journal of the American Board of Family Practice. 2003;16:22–31. doi: 10.3122/jabfm.16.1.22. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Liversidge T, Gregg L. The acceptability and preference for the psychological treatment of PTSD. Behaviour Research and Therapy. 2006;44(11):1643–1656. doi: 10.1016/j.brat.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Prevalence, incidence, and consequences of violence against women: Findings from the National Violence Against Women Survey. National Institute of Justice Centers for Disease Control and Prevention: Research in Brief. Washington, DC: U.S. Department of Justice; 1998. [Google Scholar]
- Wagner AW, Bystritsky A, Russo JE, Craske MG, Sherbourne CD, Stein MB, et al. Beliefs about psychotropic medication and psychotherapy among primary care patients with anxiety disorders. Depression and Anxiety. 2005;21:99–105. doi: 10.1002/da.20067. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wong EC, Kim BSK, Zane NW, Jim IJ, Huang JS. Examining culturally based variables associated with ethnicity: influences on credibility perceptions of empirically supported treatments. Cultural Diversity and Ethnic Minority Psychology. 2003;9:88–96. doi: 10.1037/1099-9809.9.1.88. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Cochran B, Pruitt L. Treatment choice for PTSD. Behaviour Research and Therapy. 2003;41:879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]