Abstract
Listeria monocytogenes has, in 25 y, become a model in infection biology. Through the analysis of both its saprophytic life and infectious process, new concepts in microbiology, cell biology, and pathogenesis have been discovered. This review will update our knowledge on this intracellular pathogen and highlight the most recent breakthroughs. Promising areas of investigation such as the increasingly recognized relevance for the infectious process, of RNA-mediated regulations in the bacterium, and the role of bacterially controlled posttranslational and epigenetic modifications in the host will also be discussed.
Keywords: bacterial invasion, mitochondria, posttranslational modifications, epigenetics
Listeria monocytogenes was discovered in 1926 during an epidemic that affected rabbits and guinea pigs (1). It was later shown to infect wild animals and humans and was recognized as a food pathogen in 1986 (2). This bacterial pathogen is responsible for gastroenteritis in healthy individuals, meningitis in immunocompromised individuals, and abortions in pregnant women, with a high mortality rate (20–30%; Fig. 1). Cases of listeriosis are generally sporadic, but small epidemics occur (Table S1). Recovery from infection and protection against secondary infection rely on a T-cell response, a property widely exploited by immunologists. Early diagnosis of listeriosis is critical to prevent neurological after effects. Treatment involves amoxicillin and gentamicin, which are synergistic and bactericidal. Food contamination occurs because of the capacity of the organism to adapt to a variety of niches and growth conditions. It grows at temperatures as low as 4 °C, at extreme pHs, or in high salt concentrations, conditions normally used for food conservation.
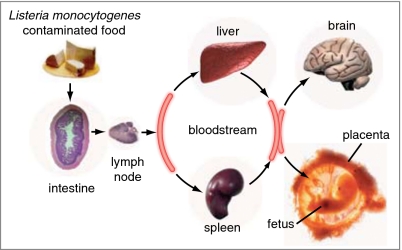
Fig. 1.
The infection by L. monocytogenes in vivo: bacteria, via contaminated food product, reach the intestinal barrier, cross it, and then disseminate to the brain and placenta (reprinted from ref. 5 with permission from Elsevier).
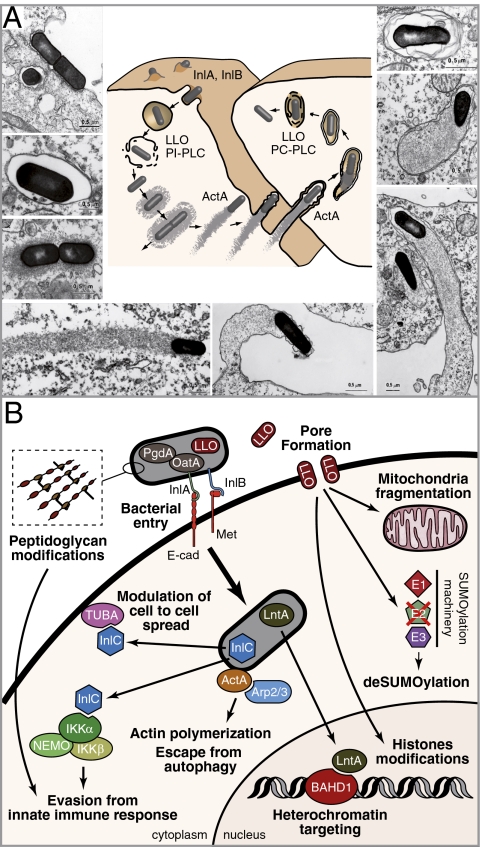
Since the late 1980s, cell biology approaches combined with molecular biology and genomics have unveiled the elegant strategies used by Listeria to enter into nonphagocytic cells, escape from the internalization vacuole, move intracellularly, avoid autophagy, and spread from cell to cell (Fig. 2). These studies have been instrumental to our understanding of the early steps of the infection in vivo. Transgenic and knock-in murine models were used to overcome species specificity and understand the way in which Listeria breaches the intestinal and placental barriers. Progress in unraveling how Listeria counteracts the innate immune system has highlighted the key role of peptidoglycan (PG) modifications. We are beginning to understand how both the bacterium and the host cell reprogram their transcription during infection. As in all systems, RNA-mediated regulations are more complex than initially anticipated, and Listeria appears as an appropriate organism in which to tackle these issues. Finally, research in Listeria has contributed to open the new field of pathoepigenetics with the recent finding that the bacterium induces histones modifications and chromatin remodeling in the nucleus of infected cells. In two decades, Listeria has become a model organism and promises to continue as such for some time to come (for reviews, see refs. 3–7).
Fig. 2.
The infection by L. monocytogenes in vitro. (A) The steps of the infection are schematically shown together with the bacterial factors involved and the corresponding EM images. (B) Schematic representation of the roles played by several virulence factors.
L. monocytogenes and the Genus Listeria
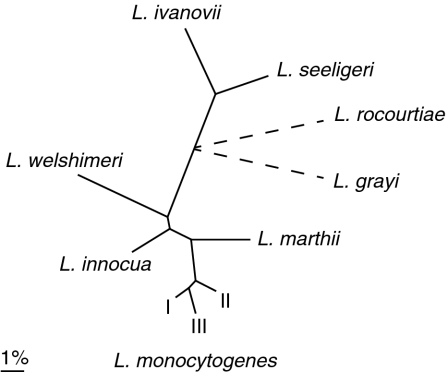
L. monocytogenes belongs to the Firmicutes phylum. It is a low guanine-cytosine content Gram-positive rod-shaped bacterium. It is motile at low temperatures, is a facultative anaerobe, and is nonsporulating. These properties and others are shared by all members of the Listeria genus—Listeria ivanovii, Listeria innocua, Listeria seeligeri, Listeria welshimeri, and Listeria grayi—as well as two newly discovered species, Listeria marthii and Listeria rocourtiae (8, 9) (Fig. 3). L. monocytogenes is pathogenic for humans and animals. L. ivanovii is predominantly an animal pathogen, affecting ruminants and sheep. The other species are nonpathogenic.
Fig. 3.
Phylogeny of the eight Listeria species. The tree depicted in continuous lines is based on nucleotide variation at 100 core genes, according to den Bakker et al. (21). The three major L. monocytogenes lineages are indicated with Roman numerals. Dotted lines indicate that the branching order and distance leading to L. rocourtiae and L. grayi, the two most distant species, are currently undefined based on this dataset (generated by S. Brisse).
Genetic Diversity Among L. monocytogenes Strains.
To differentiate L. monocytogenes strains, the old Listeria serotyping scheme based on somatic (O) and flagellar (H) antigens remains a commonly used typing system. Serotyping discriminates 13 serotypes, many of which represent genetically diverse groups of strains, and only four serotypes (1/2a, 1/2b, 1/2c and 4b) cause most cases of human listeriosis. Given its discriminatory power, pulse-field gel electrophoresis is considered accurate for epidemiological surveillance but can prove difficult for interlaboratory standardization. Based on pulse-field gel electrophoresis and multilocus enzyme electrophoresis, two lineages were initially identified, with a third subsequently recognized based on virulence gene variation, ribotyping, and DNA arrrays (10–15). Lineage I includes serotypes 4b, 1/2b, 3b, 4d, 4e, and 7, whereas lineage II includes serotypes 1/2a, 1/2c, 3a, and 3c. Lineage III contains serotypes 4a and 4c. Multilocus sequence typing applied on 360 strains demonstrated existence of clonal complexes that helped to further discrimate the different lineages (16). Most clinical isolates of L. monocytogenes belong to seven distinct clonal complexes. Whether all L. monocytogenes strains are able to induce an infection is particularly relevant to the food industry, as contamined food products must be rapidly recalled from the market.
Listeria Genomics.
The first genome sequence of an L. monocytogenes strain (strain EGD-e, serovar 1/2a) was published with that of a strain of L. innocua, the species most closely related to L. monocytogenes (17). The sequence revealed a high number of genes encoding surface proteins, transcriptional regulators, and sugar uptake systems, consistent with the capacity of Listeria to replicate in a variety of ecological niches. Comparison between L. monocytogenes and L. innocua genomes suggested multiple insertion and deletion events but no large rearrangements. Fifteen percent of the L. monocytogenes genes are absent in L. innocua. In particular, a 10-kb virulence locus, encoding factors responsible for the intracellular life of L. monocytogenes, is present in L. ivanovii and absent in L. innocua (18). It is also absent in L. welshimeri but is partially present in L. seeligeri (19, 20). Several L. monocytogenes genome sequences are now publically available. Strain differences can be high, i.e., as high as 15%. The genome of L. rocourtiae, together with those of several other species, has recently been sequenced (21). The genomes of L. grayi and L. marthii have not been reported yet. Comparative genomics has proven to be instrumental in identification of new virulence factors (as detailed later).
A Diversity of Lifestyles: From Planktonic to Biofilms and L Forms.
L. monocytogenes can adopt a planktonic life or exist as biofilms. Biofilm formation is in part regulated by PrfA, a major regulator of virulence genes, suggesting that this requirement may provide the selective pressure to maintain this regulator when Listeria is in the environment (22). A third form of life, has been reported, the L-form. L-forms are peptidoglycan (PG) and cell wall-deficient derivatives of bacteria. This phenotype was first described in 1935, and L-forms were named (as, of course, was Listeria itself) in honor of the British surgeon Joseph Lister (1860–1912). A recent report describes the generation of stable, nonreverting L-form variants of L. monocytogenes (23). Whether L-forms represent persistent cells that could be involved in chronic infection represents a fascinating field for future investigations.
Transcriptional Complexity and RNA Regulation
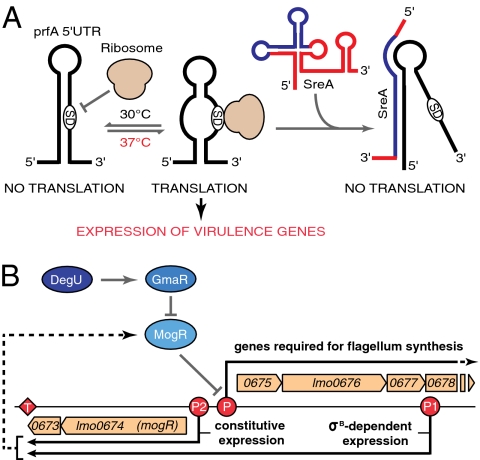
Most virulence factors are regulated by PrfA, a transcriptional regulator of the CRP family with a consensus binding site in the -35 region of the promoter (24). PrfA is under the control of a thermosensor, a 5′UTR that adopts alternative secondary structures depending on the temperature. This results in optimal PrfA expression at high temperatures and translational repression at low temperatures, explaining how virulence genes are maximally expressed at 37 °C (25) (Fig. 4A). The role of sugars in the activity of PrfA is well established, but the underlying molecular mechanisms remain elusive (26). Many virulence-associated genes are regulated by sigma B, one of five sigma factors in Listeria. Knowledge of the genome sequence allowed determination of complete regulons, e.g., the partially overlapping PrfA and sigma B regulons and the VirR regulon (27, 28). VirR, initially identified as a virulence factor by signature-tagged mutagenesis, is one of the 15 two-com-ponent regulators in L. monocytogenes. It controls cell wall and membrane modifications and plays a key role in the interaction with the host. VirR-regulated genes include dltA, involved in lipotechoic acid modification, and mprf, required for the lysinylation of phospholipids in listerial membranes, and which confers resistance to cationic antimicrobial peptides (29). The Fur regulon has also been examined (30). Fur is the regulator of ferric iron uptake in many bacteria although the situation in Listeria is not as simple as in Escherichia coli. Fur can bind DNA in absence of iron, as in Bacillus subtilis or Helicobacter pylori. As iron is critical for infection, this regulon deserves more investigation. A regulon similar to the Agr regulon of Staphylococcus aureus exists in Listeria and, to some extent, is controlling virulence. However, RNAIII, a key regulator RNA in S. aureus, does not have a homologue in Listeria (31, 32). Other regulators affecting virulence include CtsR, HcrA, and codY (reviewed in ref. 3).
Fig. 4.
Two examples of complex regulation. (A) PrfA expression regulation by an RNA thermosensor in the 5′UTR or a small RNA deriving from a SAM riboswitch (25, 38). (B) Regulation of flagella expression.
An extra layer of complexity in the regulation of gene expression was unveiled when tiling arrays were used to analyze the complete transcriptional landscape of L. monocytogenes during the transition from saprophytic life to virulence and in different genetic backgrounds (33). This analysis, which extended the first studies on noncoding RNAs (34, 35), showed that L. monocytogenes encodes at least 50 small RNAs, among which 20 are absent in L. innocua (33). Unexpectedly long antisense noncoding RNAs covering more than one ORF were identified. Deep sequencing of RNAs from strain 10403S in stationary phase or extracted from the ΔsigB mutant confirmed that sigma B controls expression of several small RNAs (36). Deep sequencing was also used to catalog the repertoire of small RNAs during intracellular growth of the strain EGD-e (37). It revealed extensive small RNA expression during intracellular growth. Three of the small RNAs highly expressed intracellularly—Rli31, Rli33, and Rli50—were shown to be critical for virulence. Interestingly, the hypothesis that transcripts generated at riboswitches could play a role in regulation was recently experimentally validated in the case of two S-adenosyl riboswitches, which can hybridize to the PrfA UTR and inhibit PrfA expression, highlighting a link between nutrient availability and virulence (38) (Fig. 4A).
Gene expression arrays coupled to tiling arrays provided a comprehensive operon map of the Listeria genome and revealed large transcriptional reprogramming upon switch from saprophytic life to virulence, with successive and coordinated global changes (33). When Listeria reaches the host intestinal lumen, an extensive transcriptional reshaping occurs with sigma B-mediated activation of virulence associated genes (39, 40). In the blood, PrfA controls transcription of the virulence genes. Ongoing deep sequencing analysis reveals that the transcription program is even more complex, with many more antisense and unsuspected internal transcriptional start sites.
Listeria motility is under an incredibly complex regulation. This is probably a result of the fact that flagella, in addition to allowing motility to acquire nutrients and colonization of surfaces, may stimulate Toll-like receptor (TLR) 5-dependent innate immune responses, explaining why many bacteria down-regulate flagella expression following initial infection. The flagella system in most Listeria strains is thermoregulated, with higher expression at low temperatures. Expression of motility genes is mediated by the opposing activities of MogR and DegU (41, 42). At high temperatures, MogR represses the flagellar genes. MogR can be transcribed from two promoters: a constitutive promoter and a sigmaB-regulated promoter located 2 kb upstream from the constitutive promoter (33) (Fig. 4B). Increasing the levels of the long mogR transcripts impairs motility, because this transcript not only increases MogR expression but also hybridizes to the flagellin polycistronic mRNA and promotes its degradation. At low temperatures, GmaR, whose expression is induced by DegU, interacts with and inhibits MogR, thus acting as an antirepressor allowing flagellin expression (Fig. 4B) (43). Interestingly, GmaR is a glycosyl transferase, which, in addition to its antirepressor activity, glycosylates the flagellin protein itself (44). Glycosylation may play a role in adaptation in particular environments. Whether flagellin contributes to virulence seems to vary among strains and with the animal model used (45, 46).
New Virulence Factors and New Roles for Well-Known Virulence Factors
L. monocytogenes has a versatile arsenal of virulence factors, which allows it to infect, survive, and replicate in a variety of host cell types. The virulence gene locus and other genes controlled by PrfA allow the bacterium to enter into nonphagocytic cells, escape from the internalization vacuole, replicate intracellularly, and spread from cell to cell (4). The best characterized genes of this regulon encode the pore-forming toxin listeriolysin O (LLO) (47); the actin polymerization factor ActA; the Mpl metalloprotease; two phospholipases, PlcA and PlcB; the two major internalins, InlA and InlB; the secreted protein InlC; and the sugar uptake system UhpT (reviewed in ref. 3). InlA and InlB were discovered as proteins involved in bacterial entry into cells (48, 49). InlA seems to be dedicated to this single function whereas InlB acts as both an invasion protein and a potent signaling molecule (50). InlC is a secreted PrfA-regulated protein highly expressed inside infected cells, where it interacts with IκB kinase (IKKα) and with the cytoskeletal protein Tuba (51, 52). Interaction with IKKα prevents NF-κB activation, thus dampening the innate immune response. Interaction with Tuba affects the cell to cell spread. The sugar uptake system UhpT allows G6P uptake inside cells and intracellular growth.
LLO and ActA are involved in several functions, and consequently ActA and LLO mutants are strongly affected in virulence. LLO, which promotes bacterial escape from the internalization vacuole, albeit not in human cells (53), has been described as critical for survival and replication in spacious Listeria containing phagosomes in macrophages (54). Its pore-forming activity allows Ca++ influx, which increases the entry rate (55), and K+ efflux, which activates caspase1 and inflammasome and triggers histone modifications (56, 57). LLO is also involved in posttranslational modifications such as deSUMOylation in infected cells and mitochondrial fragmentation (as detailed later) (58, 59). Interestingly, these latter functions, which are exerted before bacterial entry into cells, reveal that LLO can affect many more cells than those cells in which one can detect bacteria. ActA is the surface protein that allows Listeria to move intra- and intercellularly through activation of the Arp2/3 complex (60). It also protects bacteria from autophagy (61) (as detailed later).
The internalin family encodes proteins displaying leucine-rich repeats. It comprises, in addition to InlA, InlB, and InlC, other virulence factors (62). InlJ has unique leucine-rich repeats that form a cysteine ladder. It is barely detectable in vitro, behaves as an adhesin, and is expressed late during infection (63). InlH, in contrast, is well expressed in vitro. The only known function of InlH is its role in control of IL6 production during murine listeriosis (64). InlK is also only expressed in vivo and contributes to escape from autophagy (as detailed later) (65).
Other proteins involved in virulence include BSH, a bile salt hydrolase; the surface proteins Auto and VIP; the phosphatases STP and LipA; and the superoxyde dismutase (SOD) MnSOD (66–71). The PG-modifying enzyme PgdA deacetylates the N-acetylglucosamine residues of PG of L. monocytogenes and confers resitance to lysozyme (72). Strikingly, pgdA mutants are among the most attenuated mutants of L. monocytogenes (as detailed later). Another PG modification, acetylation of muramic acid residues, is induced by gene oatA and critical for the survival of Listeria in infected hosts (73). The cytokine responses to the pgdA and the oatA mutants are different, indicating specific recognition of cell wall components and nonredundant roles for the two modifications. The multidrug resistance transporters are efflux pumps associated with resistance to antibiotic or toxic compounds. One of them exports cyclic di-AMP and triggers a cytosolic type I IFN response (74) (as detailed later). The first listerial secreted factor able to target the nucleus and remodel chromatin was recently identified. This small basic protein LntA interacts with the BAHD1 silencing complex in the nucleus (75, 76). When LntA interacts with BAHD1 during infection, it induces expression of a type III IFN response, thus participating in the innate immune response (as detailed later). Listeriolysin S is a toxin similar to the modified peptide streptolysin S, a hemolytic and cytotoxic virulence factor that plays a key role in the virulence of group A Streptococcus (77). Interestingly it is only present in a subset of lineage I strains of L. monocytogenes, those responsible for most listeriosis outbreaks.
Cell Biology of the Infectious Process
Invasion and a New Role for Clathrin.
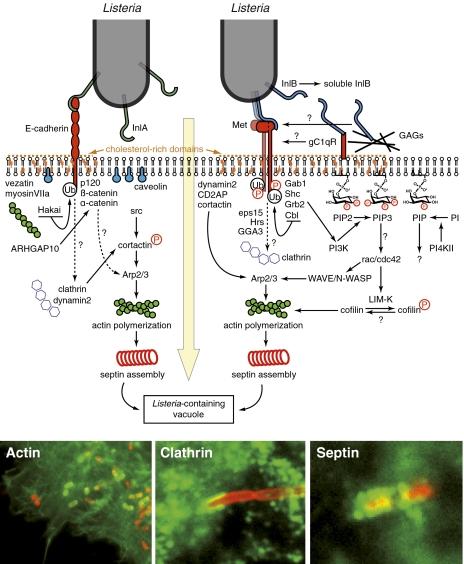
L. monocytogenes is able to invade a number of nonphagocytic cells. Invasion efficiency varies with the cell line or the type of cells used and never reaches the entry rate observed in macrophages. Entry into cells has been investigated in great detail since the discovery of the invasion proteins internalin (InlA) and InlB and that of their respective receptors E-cadherin (E-cad) and Met. The mechanism underlying the actin rearrangements and membrane phospholipids changes triggered by Listeria and required for entry are reviewed elsewhere (50, 78–80). How internalin exploits its receptor E-cad and how InlB hijacks the signaling pathway normally triggered by the growth factor HGF when it interacts with Met have been the focus of many studies, including the determination of the structure of the two corresponding cocrystals, which magnificently revealed how Listeria interacts with E-cad and Met at sites different from than those recognized by the physiological ligands (81, 82) (Figs. 5 and 6). An unexpected recent finding is the discovery that clathrin and clathrin-mediated endocytosis machinery are involved in entry and required for this event (83–87). Also new is the finding that septins are involved in entry. These GTPases form heteropolymeric, nonpolar filaments. They asso-ciate with actin and tubulin in an unclear fashion (88, 89). The recruitment of septins at the bacterial entry site and their absence in the presence of cytochalasin D indicate that septins control the late steps of the entry process.
Fig. 5.
The entry of L. monocytogenes into cells. Schematic representation of the signaling pathways triggered by InlA and InlB (Top). The three bottom images show recruitment of actin, clathrin, and septin (green fluorescence) at the site of bacterial entry (bacteria shown in red).
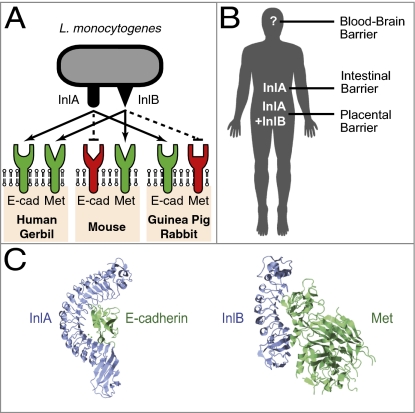
Fig. 6.
Roles of InlA and InlB in vivo. (A) The species specificities of InlA and InlB. (B) Schematic representation of the barriers where InlA and InlB play a role in vivo. (C) Tridimensional structure of the InlA-E-cadherin and InlB-Met cocrystals (reprinted from refs. 81 and 82 with permission from Elsevier).
Escape from the Vacuole.
This step of escape from the vacuole is mainly mediated by the pore-forming toxin LLO. Pore formation proceeds by oligomerization of cholesterol-associated monomers that insert in the membrane lipid bilayer (reviewed in ref. 47). The LLO-dependent perforation results in transient changes in vacuolar pH and calcium concentration, culminating in membrane disruption. LLO is required for vacuolar escape in mice but is dispensable in human cells, in which the two phospholipases PLcA and PlcB are critical. PlcB is critical for the lysis of the secondary vacuole (90). Contribution of host factors is less well defined. One report indicates that bacterial escape relies on the γ-IFN–induced lysosomal thiol reductase GILT, which would reduce the single cysteine residue of LLO (91). Additionally, a recent report revealed that the CFTR protein transiently increases phagosomal chloride concentration after infection, potentiating LLO pore formation and vacuole lysis (92). Together, the picture which is emerging is that several host factors significantly contribute to the phagosomal environment and bacterial escape.
Actin-Based Motility and Cell-to-Cell Spread.
Analysis of how bacteria move inside cells has provided the best example of bacterial mimicry used for efficent infection (60). The surface protein ActA mimics the host cell WASP family proteins, recruits the host Arp2/3 complex, and promotes actin polymerization, formation of an actin tail, and movement. Although a restricted number of proteins seem to be required for actin tail formation in vitro, mass-spectrometry (MS) analysis of the comet tails has revealed that many proteins are probably controlling this sophisticated force-generating nanomachine (93). Intriguingly, septins may form rings around actin tails, but do not affect speed of movement (94). Cell-to-cell spread and tissue dissemination rely on the actin-based movement and on InlC, which, by interacting with the actin-binding protein Tuba, regulates the passage from one cell to the other (51). Lysis of the secondary vacuole requires both LLO and PlcB.
Posttranslational Modifications in Infected Cells
Although phosphorylation and ubiquitination successively modify the Listeria receptors as a prelude for bacterial entry (83, 95), other posttranslational modifications (PTMs) may contribute to the host cell response to infection. A recent study revealed that Listeria interferes with the host SUMOylation machinery (58). SUMOylation is involved in transcription regulation, stress responses, and other processes. Similar to the ubiquitin system, conjugation of SUMO on a target protein involves an E1, an E2, and an E3 enzyme. Infection by Listeria leads to the degradation of Ubc9, the unique human E2 SUMO enzyme. LLO triggers degradation of Ubc9 as well as that of several SUMOylated proteins leading to a global decrease in the levels of SUMO-conjugated host proteins in host cells. Overexpressing SUMO counteracts infection revealing that bacterially induced deSUMOylation is critical for infection. Pharmacological experiments suggest the involvement of an aspartyl-protease in UBC9 degradation but the SUMO targets that are critical for infection are unknown.
Conversely some bacterial proteins are posttranslationally modified by the host including ActA and the SOD, which are phosphorylated, and LLO, which becomes ubiquitinated (71, 96–98). There are likely many other Listeria targets of host PTMs.
Gene Reprogramming, Histone Modifications, and Chromatin Remodeling
As for all pathogens, L. monocytogenes causes gene reprogramming during infection. This has been analyzed in vitro in epithelial cells (99) or various macrophages (100–103), and in vivo (104). A first response mediated by TLRs appears early and persists, with NF-κB–dependent gene expression of proinflammatory cytokines. A second response occurs when bacteria are cytosolic. It induces a distinct set of target genes, including IFN-β. Interestingly, when the response to Listeria was analyzed in vivo in the instestine of germ-free transgenic mice expressing the human E-cad, it was observed that the transcriptional response at 72 h p.i. was similar with the use of WT or InlA mutant, and that expression of LLO was the key determinant of the intensity of the host response (104).
Changes in gene expression involve transcriptional and translational regulators as well as chromatin modifications, which control access of the transcriptional machinery to the promoter regions. Several pathogen-induced histone modifications have already been reported (105). Interestingly, Listeria also induces histone modifications during infection (56). Dephosphorylation of serine 10 of histone H3 and deacetylation of H4 were shown to be LLO-dependent and to lead to the down-regulation of a subset of genes, including genes involved in the immune response of the host. These modifications can occur when LLO is outside the cell, implying that LLO can reprogram cells that are not infected and have a long-distance effect. They depend on LLO-induced potassium efflux but are independent of the concomitant caspase activation, suggesting that a K+ sensor might be involved in this pathway (57). Another listerial factor was recently shown to affect chromatin. This protein, named LntA (as described earlier), interacts in the nucleus with BAHD1, a protein that is part of a multiprotein complex involved in heterochromatin formation and gene silencing (75, 76). Upon infection, the BAHD1 complex targets a number of genes, including type III IFN genes and IFN-stimulated genes (ISGs). In absence of LntA, type III interferons are expressed but ISGs are poorly induced. When LntA is expres-sed, ISGs are highly induced. The LntA–BAHD1 interaction leads to sequestering of the BAHD1 complex and derepression of ISGs. However, how Listeria infection induces a BAHD1-mediated repression of ISGs is unknown.
Escape from Autophagy
Once in the cytosol, bacteria encounter the host innate surveillance system of autophagy. Autophagy is an evolutionary conserved catabolic pathway that allows eukaryotes to degrade and recycle intracellular components by sequestering proteins and organelles in specialized double-membrane vesicles named autophagosomes. Autophagy regulates cellular homeostasis but is also implicated in the host cell reaction to microbial invaders. Several observations suggested a link between escape from autophagy and actin-based motility until the demonstration that ActA protects the bacteria from being surrounded by ubiquitinated proteins as a prelude for autophagosome formation (61, 106). ActA mutants are targeted to autophagy, whereas ActA-expressing bacteria are not. InlK also contributes to autophagy by recruiting a cellular ribonucleoprotein, MVP (65). The role of autophagy in Listeria pathogenesis has been investigated in vitro (61, 65, 106, 107). Its relevance in vivo remains to be established.
Control of Mitochondrial Dynamics
Mitochondria are essential and dynamic organelles, providing most cellular ATP and several biosynthetic intermediates. They constantly undergo fusion and fission and have emerged as important integrators of several signaling cascades. Fusion and fission of mitochondria regulate their size and subcellular distribution and reflect their functional state. Infection with Listeria profoundly alters mitochondrial dynamics by causing fragmentation of the mitochondrial network (59). This does not occur with nonpathogenic species and is mediated by LLO. Fragmentation is transient, suggesting that the temporary shutdown of mitochondrial dynamics and function is a strategy used by Listeria at early stages of infection to impair cellular physiology.
Evasion from Innate Immunity
The innate immune system defends the host from infections in a nonspecific manner. The receptors involved recognize structures that are the signatures of nonself, or MAMPs for microbial-associated molecular patterns, and trigger various signaling pathways leading to activation of immune cell responses, such as expression and secretion of antimicrobial components or proinflammatory cytokines. The innate immune response prepares the host for the adaptive response. As shown for many pathogens, decreasing the innate immune recognition and response is beneficial for the bacterium. Listeria has developed tools to escape from this response. The protein InlC, which is abundantly secreted in infected cells, interacts with IKKα, prevents NF-κB activation, and impairs cytokine expression and neutrophil recruitment at the site of infection, thus dampening the innate immune response (52). The Listeria PG also plays a key role. It is modified by PgdA and OatA, a deacetylase and an acetyltransferase that confer resistance to lysozyme. pgdA and oatA mutants are strongly attenuated, demonstrating the key role of PG modifications in host defense (72). Strikingly, the pgdA mutant induces a high production of IFN-β. Type I interferons play a major role in antiviral immunity. During bacterial infections, they can have a detrimental or protective effect. During listeriosis, the effect is detrimental to the host. Strikingly, the robust induction of IFN-β by Listeria pgdA mutant is mediated by TLR2. The pgdA mutant is destroyed in the internalization vacuole and liberates components able to stimulate the innate immune response, including LTA, PG, lipoproteins, DNA, and RNA, which can be sensed by the cell. How all these components are sensed intracellularly remains to be clarified. Strikingly, IFN-β is induced by the efflux of cyclic di-AMP from Listeria (108). How this molecule and other bacterial metabolites like cyclic di-GMP (109) are sensed by the cell is the object of intense investigations (110). Finally, as discovered recently, Listeria as viruses triggers expression of type III IFN, whose receptor IL28R is mainly expressed in epithelial cells (76). How this response is triggered and controlled in vivo by LntA is unknown.
Although infected cells trigger host responses, noninfected cells also participate in orchestration of this cross-talk. Diffusible bacterial components such as LLO trigger signals in noninfected cells, increasing the danger signals induced by infected cells. In addition, cells adjacent to infected cells in epithelial cell layers may trigger a chemokine response greater than that observed in infected cells (111, 112). Whether gap junctions are involved in this intercellular communication is a matter of debate. A simple explanation for this higher chemokine expression in noninfected cells is that infected cells down-regulate the inflammatory response via bacterial secreted factors such as InlC, whereas adjacent cells do not. It will be important to investigate whether these phenomena do occur in vivo.
Infection in Vivo: Animal Models and Crossing of Host Barriers
Listeriosis has been widely—and still is—investigated in mice after i.v. inoculation. This has allowed to study the induction of the T-cell response and the role of important virulence factors (5, 113). Usually, BALB/c mice are used, as they are more sensitive to listeriosis than other lines such as C57Bl6. However, this mouse model, which has the advantage that KO mutants can be generated and/or crossed with other lines, has limitations. The internalin–E-cad interaction does not occur in the mouse as a result of a species specificity. InlA interacts with human and guinea pig E-cad but not with mouse and rat E-cad (114) (Fig. 6A). This species specificity relies on the 16th amino acid of the E-cad. The mouse model is thus not suitable for studying the pathophysiology of listeriosis after oral inoculation, the natural route of infection. The InlB–Met interaction is also species specific (115). InlB interacts with human and mouse Met but not with guinea pig or rabbit Met (Fig. 6A). To confer the mouse permissiveness to the InlA–E-cad interaction, two mouse lines have been engineered (116, 117). In the first transgenic line, human E-cad is exclusively expressed in small intestine enterocytes. This model has been instrumental to show the key role played by the internalin–E-cad interaction in the crossing of the intestinal barrier. It also showed that InlB is not critical for intestinal villus invasion (115) (Fig. 6B). However, the transgenic model does not allow the study of the role of InlA in E-cad–expressing cells located elsewhere than the small intestine, including the cecum and colon, as well as in the maternofetal and blood–brain barriers. In a knock-in E16P mouse model, the glutamic at position 16 of mE-cad was replaced by a proline (117). In these mice, all cells normally expressing mE-cad express a “humanized” E16PmE-cad and the InlA–E16PmE-cad interaction can take place in vivo, as in humans (as detailed later).
Gerbils, which, like humans, are naturally permissive to InlA–E-cad and InlB–Met interactions, have contributed to the study of targeting to the placental barrier (117). However, tools are lacking and interindividual variability precludes their wider use. Guinea pigs, although they do not allow the InlB–Met interaction, have been used to study some aspects of listeriosis; however, in this species, few tools are available (115). Other animals have been used to investigate Listeria infections, e.g., the zebrafish Danio rerio, which has become a popular vertebrate model for the study of infections because of the excellent optical accessibility at the larval stages when the innate immune sytem is already effective. Intravenous injection of zebrafish larvae resulted in fatal infections (118). Blood-borne bacteria were shown to be engulfed in macrophages. They escaped from the phagosome and polymerized actin. In addition, the LLO or actA mutants were attenuated, demonstrating that the genetically tractable zebrafish model might be useful for the study of L. monocytogenes and, in particular, its interactions with phagocytes in vivo, a key issue in L. monocytogenes virulence. Chicken embryos have been used to decipher differences between strains. The wax moth Galleria mellonella has also been proposed as a model, as essential aspects of the innate immune response to microbial infections are conserved between insects and mammals (119). Use of this insect allowed to distinguish between pathogenic and nonpathogenic Listeria species and to discriminate between L. monocytogenes serotypes exhibiting attenuated virulence properties. In the main insect model Drosophila, there seems to be little contribution of Listeria virulence factors to septic infection, and a recent study described some limitations of Drosophila melanogaster as a heterologous host for the study of several Gram-positive bacteria (120). Importantly, flies are not maintained at 37 °C, preventing studies at a temperature close to that of infected mammals. Finally, the nematode Caenorhabditis elegans seems of limited use, as some well established virulence factors, e.g., ActA, are dispensable whereas others are critical (121).
Crossing of host barriers is a hallmark of Listeria infections (4). Listeria crosses the intestinal, placental, and blood–brain barriers. It crosses the intestinal epithelial barrier upon interaction of its surface protein InlA and its species specific receptor E-cad. E-cad is an adherens junction protein typically located below tight junctions and considered inaccessible, and L. monocytogenes was reported to target accessible E-cad at the tips of intestinal villi at sites of cell extrusion (122, 123), where cell extrusion is associated with junction remodeling and transient exposition of E-cad. In addition, as shown recently, Listeria along villi preferentially targets goblet cells, where, upon mucus secretion, E-cad becomes accessible. Unexpectedly, bacteria enclosed in a vacuole transcytose across cells and reach rapidly the lamina propria, resulting in rapid systemic dissemination, thereby avoiding detection by the innate immune system (123). Listeria can also cross the intestinal barrier in an InlA-independent manner through M cells and be subsequently uptaken by antigen-presenting cells, in which LLO initiates the host response (104). The other barrier targeted by Listeria is the placental barrier. Here the situation is different. The barrier consists of a long multinucleated cell, the syncytiotrophoblast, which expresses E-cad on its luminal surface (124). Experiments with E-cad knock-in mice and gerbils have established that targeting and crossing of the barrier are dependent on InlA in a strict interdependency with InlB–Met interaction (117). Finally, how the blood– brain barrier is crossed by Listeria is still unknown.
Concluding Remarks
L. monocytogenes is now one of the best models in pathogenesis owing to the combined efforts of in vivo and in vitro approaches. However, many aspects of the Listeria infectious process remain unclear or appear more complex that previously thought, and deserve more investigation. Many virulence factors play several roles. For example, LLO is a multifaceted virulence factor that induces a variety of important signaling events and, in addition, can, as any diffusible molecule, act on cells that are not infected. The attenuated phenotype of LLO mutants is thus a result of the multiple functions of LLO and not solely its role in mediating escape from the vacuole. Many other factors probably also play several roles. As in other systems, it is expected that, in vivo, the various functions of one given virulence factor will be dictated by different PTMs so that they come into action at different stages of the infection process, as in the case of SopB of Salmonella (125). Deciphering when, how, and where virulence factors are acting is critical to understanding their precise function. It is also possible that new types of regulation such as RNA-mediated regulations are also involved.
Although early studies on the Listeria infectious process focused on the mechanics of the infection, i.e., the rearrangements of the cytoskeleton or the remodeling of the plasma membrane during invasion or cell-to-cell spread, recent work has focused on the mechanisms underlying the host cell response and survival. New themes of research are thus emerging, such as the role played by various cellular organelles, and the impact of PTMs for the bacterial infection or cell response. Another emerging theme is that pathogens have evolved mechanisms to target and remodel the chromatin, raising the possibily that chromatin marks may be stably acquired and remain after the infection has resumed.
Listeria has been and continues to be instrumental in cell biology. It is well known for the role it has played in the discovery of the role of the Arp2/3 complex in actin-based motility. More recently, it has been critical to establish a role for clathrin in bacterial invasion and adhesion, and reinforcing the increasingly recognized function of clathrin in actin organization in mammalian cells. The recent discovery of the BAHD1 complex in heterochromatin formation again illustrates that pathogens provide important tools to discover new components and new regulators of eukaryotic cells.
The recent observation that Listeria crosses the intestinal barrier by transcytosis highlights that it is critical to validate and make sense in vivo of the sophisticated mechanisms that are deciphered in vitro. Where, when, how, and whether some presumed cross-talks occur are the future key challenges in infection biology. Answers to such questions will help in the generation of vaccines that use Listeria as a vehicle for intracellular expression of antigens (126).
Finally, it will be necessary to take into account that infection occurs in the context of complex microbial flora, which also play a role at the onset and during establishment of infection. There are still many more surprises to come!
Supplementary Material
Acknowledgments
I thank all present and previous members of the laboratory for contributions to the discoveries that they made in the laboratory. I also apologize to my Listeria colleagues whose work could not be cited or discussed because of space imitations. I give special thanks to D. Ribet for help in manuscript preparation. I thank H. Bierne, O. Dussurget, M. Lecuit, J. Mellin, S. Mostowy, D. Ribet, and F. Stavru for critical comments on the manuscript and M. Bonazzi, S. Brisse, D. Ribet, and N. Sesto for help in figure preparation. Present work in the laboratory has received funding from Insitut Pasteur, Institut National de la Santé et de la Recherche Médicale, Institut National de la Recherche Agronomique, European Research Council (Advanced Grant 233348), The Howard Hughes Medical Institute, Agence Nationale de Recherches, and the Louis-Jeantet Foundation.
Footnotes
The author declares no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1112371108/-/DCSupplemental.
References
- 1.Murray EGD, Webb RA, Swann HBR. A disease of rabbits characterized by a large mononuclear leucoytosis caused by a hitherto undescribed bacillus Bacterium monocytogenes (n.sp.) J Pathol Bacteriol. 1926;29:407–439. [Google Scholar]
- 2.Schlech WF, 3rd, et al. Epidemic listeriosis—evidence for transmission by food. N Engl J Med. 1983;308:203–206. doi: 10.1056/NEJM198301273080407. [DOI] [PubMed] [Google Scholar]
- 3.Dussurget O, Pizarro-Cerda J, Cossart P. Molecular determinants of Listeria monocytogenes virulence. Annu Rev Microbiol. 2004;58:587–610. doi: 10.1146/annurev.micro.57.030502.090934. [DOI] [PubMed] [Google Scholar]
- 4.Lecuit M. Human listeriosis and animal models. Microbes Infect. 2007;9:1216–1225. doi: 10.1016/j.micinf.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Cossart P, Toledo-Arana A. Listeria monocytogenes, a unique model in infection biology: An overview. Microbes Infect. 2008;10:1041–1050. doi: 10.1016/j.micinf.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 6.Hamon M, Bierne H, Cossart P. Listeria monocytogenes: A multifaceted model. Nat Rev Microbiol. 2006;4:423–434. doi: 10.1038/nrmicro1413. [DOI] [PubMed] [Google Scholar]
- 7.Stavru F, Archambaud C, Cossart P. Cell biology and immunology of Listeria monocytogenes infections: Novel insights. Immunol Rev. 2011;240:160–184. doi: 10.1111/j.1600-065X.2010.00993.x. [DOI] [PubMed] [Google Scholar]
- 8.Leclercq A, et al. Listeria rocourtiae sp. nov. Int J Syst Evol Microbiol. 2010;60:2210–2214. doi: 10.1099/ijs.0.017376-0. [DOI] [PubMed] [Google Scholar]
- 9.Graves LM, et al. Listeria marthii sp. nov., isolated from the natural environment, Finger Lakes National Forest. Int J Syst Evol Microbiol. 2010;60:1280–1288. doi: 10.1099/ijs.0.014118-0. [DOI] [PubMed] [Google Scholar]
- 10.Piffaretti JC, et al. Genetic characterization of clones of the bacterium Listeria monocytogenes causing epidemic disease. Proc Natl Acad Sci USA. 1989;86:3818–3822. doi: 10.1073/pnas.86.10.3818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rasmussen OF, Beck T, Olsen JE, Dons L, Rossen L. Listeria monocytogenes isolates can be classified into two major types according to the sequence of the listeriolysin gene. Infect Immun. 1991;59:3945–3951. doi: 10.1128/iai.59.11.3945-3951.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graves LM, et al. Comparison of ribotyping and multilocus enzyme electrophoresis for subtyping of Listeria monocytogenes isolates. J Clin Microbiol. 1994;32:2936–2943. doi: 10.1128/jcm.32.12.2936-2943.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brosch R, Chen J, Luchansky JB. Pulsed-field fingerprinting of listeriae: Identification of genomic divisions for Listeria monocytogenes and their correlation with serovar. Appl Environ Microbiol. 1994;60:2584–2592. doi: 10.1128/aem.60.7.2584-2592.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiedmann M, et al. Ribotypes and virulence gene polymorphisms suggest three distinct Listeria monocytogenes lineages with differences in pathogenic potential. Infect Immun. 1997;65:2707–2716. doi: 10.1128/iai.65.7.2707-2716.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doumith M, et al. New aspects regarding evolution and virulence of Listeria monocytogenes revealed by comparative genomics and DNA arrays. Infect Immun. 2004;72:1072–1083. doi: 10.1128/IAI.72.2.1072-1083.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ragon M, et al. A new perspective on Listeria monocytogenes evolution. PLoS Pathog. 2008;4:e1000146. doi: 10.1371/journal.ppat.1000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glaser P, et al. Comparative genomics of Listeria species. Science. 2001;294:849–852. doi: 10.1126/science.1063447. [DOI] [PubMed] [Google Scholar]
- 18.Gouin E, Mengaud J, Cossart P. The virulence gene cluster of Listeria monocytogenes is also present in Listeria ivanovii, an animal pathogen, and Listeria seeligeri, a nonpathogenic species. Infect Immun. 1994;62:3550–3553. doi: 10.1128/iai.62.8.3550-3553.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hain T, et al. Whole-genome sequence of Listeria welshimeri reveals common steps in genome reduction with Listeria innocua as compared to Listeria monocytogenes. J Bacteriol. 2006;188:7405–7415. doi: 10.1128/JB.00758-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steinweg C, et al. Complete genome sequence of Listeria seeligeri, a nonpathogenic member of the genus Listeria. J Bacteriol. 2010;192:1473–1474. doi: 10.1128/JB.01415-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.den Bakker HC, et al. Comparative genomics of the bacterial genus Listeria: Genome evolution is characterized by limited gene acquisition and limited gene loss. BMC Genomics. 2010;11:688. doi: 10.1186/1471-2164-11-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lemon KP, Freitag NE, Kolter R. The virulence regulator PrfA promotes biofilm formation by Listeria monocytogenes. J Bacteriol. 2010;192:3969–3976. doi: 10.1128/JB.00179-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dell'Era S, et al. Listeria monocytogenes L-forms respond to cell wall deficiency by modifying gene expression and the mode of division. Mol Microbiol. 2009;73:306–322. doi: 10.1111/j.1365-2958.2009.06774.x. [DOI] [PubMed] [Google Scholar]
- 24.de las Heras A, Cain RJ, Bielecka MK, Vázquez-Boland JA. Regulation of Listeria virulence: PrfA master and commander. Curr Opin Microbiol. 2011;14:118–127. doi: 10.1016/j.mib.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Johansson J, et al. An RNA thermosensor controls expression of virulence genes in Listeria monocytogenes. Cell. 2002;110:551–561. doi: 10.1016/s0092-8674(02)00905-4. [DOI] [PubMed] [Google Scholar]
- 26.Herro R, et al. How seryl-phosphorylated HPr inhibits PrfA, a transcription activator of Listeria monocytogenes virulence genes. J Mol Microbiol Biotechnol. 2005;9:224–234. doi: 10.1159/000089650. [DOI] [PubMed] [Google Scholar]
- 27.Milohanic E, et al. Transcriptome analysis of Listeria monocytogenes identifies three groups of genes differently regulated by PrfA. Mol Microbiol. 2003;47:1613–1625. doi: 10.1046/j.1365-2958.2003.03413.x. [DOI] [PubMed] [Google Scholar]
- 28.Mandin P, et al. VirR, a response regulator critical for Listeria monocytogenes virulence. Mol Microbiol. 2005;57:1367–1380. doi: 10.1111/j.1365-2958.2005.04776.x. [DOI] [PubMed] [Google Scholar]
- 29.Thedieck K, et al. The MprF protein is required for lysinylation of phospholipids in listerial membranes and confers resistance to cationic antimicrobial peptides (CAMPs) on Listeria monocytogenes. Mol Microbiol. 2006;62:1325–1339. doi: 10.1111/j.1365-2958.2006.05452.x. [DOI] [PubMed] [Google Scholar]
- 30.Ledala N, Sengupta M, Muthaiyan A, Wilkinson BJ, Jayaswal RK. Transcriptomic response of Listeria monocytogenes to iron limitation and Fur mutation. Appl Environ Microbiol. 2010;76:406–416. doi: 10.1128/AEM.01389-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riedel CU, et al. AgrD-dependent quorum sensing affects biofilm formation, invasion, virulence and global gene expression profiles in Listeria monocytogenes. Mol Microbiol. 2009;71:1177–1189. doi: 10.1111/j.1365-2958.2008.06589.x. [DOI] [PubMed] [Google Scholar]
- 32.Rieu A, Weidmann S, Garmyn D, Piveteau P, Guzzo J. Agr system of Listeria monocytogenes EGD-e: Role in adherence and differential expression pattern. Appl Environ Microbiol. 2007;73:6125–6133. doi: 10.1128/AEM.00608-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Toledo-Arana A, et al. The Listeria transcriptional landscape from saprophytism to virulence. Nature. 2009;459:950–956. doi: 10.1038/nature08080. [DOI] [PubMed] [Google Scholar]
- 34.Christiansen JK, et al. Identification of small Hfq-binding RNAs in Listeria monocytogenes. RNA. 2006;12:1383–1396. doi: 10.1261/rna.49706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mandin P, Repoila F, Vergassola M, Geissmann T, Cossart P. Identification of new noncoding RNAs in Listeria monocytogenes and prediction of mRNA targets. Nucleic Acids Res. 2007;35:962–974. doi: 10.1093/nar/gkl1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oliver HF, et al. Deep RNA sequencing of L. monocytogenes reveals overlapping and extensive stationary phase and sigma B-dependent transcriptomes, including multiple highly transcribed noncoding RNAs. BMC Genomics. 2009;10:641. doi: 10.1186/1471-2164-10-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mraheil MA, et al. The intracellular sRNA transcriptome of Listeria monocytogenes during growth in macrophages. Nucleic Acids Res. 2011;39:4235–4238. doi: 10.1093/nar/gkr033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Loh E, et al. A trans-acting riboswitch controls expression of the virulence regulator PrfA in Listeria monocytogenes. Cell. 2009;139:770–779. doi: 10.1016/j.cell.2009.08.046. [DOI] [PubMed] [Google Scholar]
- 39.Garner MR, Njaa BL, Wiedmann M, Boor KJ. Sigma B contributes to Listeria monocytogenes gastrointestinal infection but not to systemic spread in the guinea pig infection model. Infect Immun. 2006;74:876–886. doi: 10.1128/IAI.74.2.876-886.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gahan CG, Hill C. Gastrointestinal phase of Listeria monocytogenes infection. J Appl Microbiol. 2005;98:1345–1353. doi: 10.1111/j.1365-2672.2005.02559.x. [DOI] [PubMed] [Google Scholar]
- 41.Gründling A, Burrack LS, Bouwer HG, Higgins DE. Listeria monocytogenes regulates flagellar motility gene expression through MogR, a transcriptional repressor required for virulence. Proc Natl Acad Sci USA. 2004;101:12318–12323. doi: 10.1073/pnas.0404924101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mauder N, Williams T, Fritsch F, Kuhn M, Beier D. Response regulator DegU of Listeria monocytogenes controls temperature-responsive flagellar gene expression in its unphosphorylated state. J Bacteriol. 2008;190:4777–4781. doi: 10.1128/JB.00258-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kamp HD, Higgins DE. Transcriptional and post-transcriptional regulation of the GmaR antirepressor governs temperature-dependent control of flagellar motility in Listeria monocytogenes. Mol Microbiol. 2009;74:421–435. doi: 10.1111/j.1365-2958.2009.06874.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shen A, Kamp HD, Gründling A, Higgins DE. A bifunctional O-GlcNAc transferase governs flagellar motility through anti-repression. Genes Dev. 2006;20:3283–3295. doi: 10.1101/gad.1492606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Way SS, et al. Characterization of flagellin expression and its role in Listeria monocytogenes infection and immunity. Cell Microbiol. 2004;6:235–242. doi: 10.1046/j.1462-5822.2004.00360.x. [DOI] [PubMed] [Google Scholar]
- 46.Shen A, Higgins DE. The MogR transcriptional repressor regulates nonhierarchal expression of flagellar motility genes and virulence in Listeria monocytogenes. PLoS Pathog. 2006;2:e30. doi: 10.1371/journal.ppat.0020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schnupf P, Portnoy DA. Listeriolysin O: A phagosome-specific lysin. Microbes Infect. 2007;9:1176–1187. doi: 10.1016/j.micinf.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 48.Gaillard JL, Berche P, Frehel C, Gouin E, Cossart P. Entry of L. monocytogenes into cells is mediated by internalin, a repeat protein reminiscent of surface antigens from gram-positive cocci. Cell. 1991;65:1127–1141. doi: 10.1016/0092-8674(91)90009-n. [DOI] [PubMed] [Google Scholar]
- 49.Dramsi S, et al. Entry of Listeria monocytogenes into hepatocytes requires expression of inIB, a surface protein of the internalin multigene family. Mol Microbiol. 1995;16:251–261. doi: 10.1111/j.1365-2958.1995.tb02297.x. [DOI] [PubMed] [Google Scholar]
- 50.Bierne H, Cossart P. InlB, a surface protein of Listeria monocytogenes that behaves as an invasin and a growth factor. J Cell Sci. 2002;115:3357–3367. doi: 10.1242/jcs.115.17.3357. [DOI] [PubMed] [Google Scholar]
- 51.Rajabian T, et al. The bacterial virulence factor InlC perturbs apical cell junctions and promotes cell-to-cell spread of Listeria. Nat Cell Biol. 2009;11:1212–1218. doi: 10.1038/ncb1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gouin E, et al. The Listeria monocytogenes InlC protein interferes with innate immune responses by targeting the IkappaB kinase subunit IKKalpha. Proc Natl Acad Sci USA. 2010;107:17333–17338. doi: 10.1073/pnas.1007765107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Portnoy DA, Jacks PS, Hinrichs DJ. Role of hemolysin for the intracellular growth of Listeria monocytogenes. J Exp Med. 1988;167:1459–1471. doi: 10.1084/jem.167.4.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Birmingham CL, et al. Listeriolysin O allows Listeria monocytogenes replication in macrophage vacuoles. Nature. 2008;451:350–354. doi: 10.1038/nature06479. [DOI] [PubMed] [Google Scholar]
- 55.Dramsi S, Cossart P. Listeriolysin O-mediated calcium influx potentiates entry of Listeria monocytogenes into the human Hep-2 epithelial cell line. Infect Immun. 2003;71:3614–3618. doi: 10.1128/IAI.71.6.3614-3618.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hamon MA, et al. Histone modifications induced by a family of bacterial toxins. Proc Natl Acad Sci USA. 2007;104:13467–13472. doi: 10.1073/pnas.0702729104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hamon MA, Cossart P. K+ efflux, is required for histone-H3 dephosphorylation by Listeria LLO and other pore forming toxins. Infect Immun. 2011;79:2839–2846. doi: 10.1128/IAI.01243-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ribet D, et al. Listeria monocytogenes impairs SUMOylation for efficient infection. Nature. 2010;464:1192–1195. doi: 10.1038/nature08963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stavru F, Bouillaud F, Sartori A, Ricquier D, Cossart P. Listeria monocytogenes transiently alters mitochondrial dynamics during infection. Proc Natl Acad Sci USA. 2011;108:3612–3617. doi: 10.1073/pnas.1100126108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gouin E, Welch MD, Cossart P. Actin-based motility of intracellular pathogens. Curr Opin Microbiol. 2005;8:35–45. doi: 10.1016/j.mib.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 61.Yoshikawa Y, et al. Listeria monocytogenes ActA-mediated escape from autophagic recognition. Nat Cell Biol. 2009;11:1233–1240. doi: 10.1038/ncb1967. [DOI] [PubMed] [Google Scholar]
- 62.Bierne H, Sabet C, Personnic N, Cossart P. Internalins: A complex family of leucine-rich repeat-containing proteins in Listeria monocytogenes. Microbes Infect. 2007;9:1156–1166. doi: 10.1016/j.micinf.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 63.Sabet C, et al. The Listeria monocytogenes virulence factor InlJ is specifically expressed in vivo and behaves as an adhesin. Infect Immun. 2008;76:1368–1378. doi: 10.1128/IAI.01519-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Personnic N, et al. The stress-induced virulence protein InlH controls interleukin-6 production during murine listeriosis. Infect Immun. 2010;78:1979–1989. doi: 10.1128/IAI.01096-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dortet L, et al. Recruitment of the major vault protein by InlK: A Listeria monocytogenes strategy to avoid autophagy. PLoS Pathog. 2011;7:e1002168. doi: 10.1371/journal.ppat.1002168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dussurget O, et al. European Listeria Genome Consortium. Listeria monocytogenes bile salt hydrolase is a PrfA-regulated virulence factor involved in the intestinal and hepatic phases of listeriosis. Mol Microbiol. 2002;45:1095–1106. doi: 10.1046/j.1365-2958.2002.03080.x. [DOI] [PubMed] [Google Scholar]
- 67.Cabanes D, Dussurget O, Dehoux P, Cossart P. Auto, a surface associated autolysin of Listeria monocytogenes required for entry into eukaryotic cells and virulence. Mol Microbiol. 2004;51:1601–1614. doi: 10.1111/j.1365-2958.2003.03945.x. [DOI] [PubMed] [Google Scholar]
- 68.Cabanes D, et al. Gp96 is a receptor for a novel Listeria monocytogenes virulence factor, Vip, a surface protein. EMBO J. 2005;24:2827–2838. doi: 10.1038/sj.emboj.7600750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Archambaud C, Gouin E, Pizarro-Cerda J, Cossart P, Dussurget O. Translation elongation factor EF-Tu is a target for Stp, a serine-threonine phosphatase involved in virulence of Listeria monocytogenes. Mol Microbiol. 2005;56:383–396. doi: 10.1111/j.1365-2958.2005.04551.x. [DOI] [PubMed] [Google Scholar]
- 70.Kastner R, et al. LipA, a tyrosine and lipid phosphatase involved in the virulence of Listeria monocytogenes. Infect Immun. 2011;79:2489–2498. doi: 10.1128/IAI.05073-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Archambaud C, Nahori MA, Pizarro-Cerda J, Cossart P, Dussurget O. Control of Listeria superoxide dismutase by phosphorylation. J Biol Chem. 2006;281:31812–31822. doi: 10.1074/jbc.M606249200. [DOI] [PubMed] [Google Scholar]
- 72.Boneca IG, et al. A critical role for peptidoglycan N-deacetylation in Listeria evasion from the host innate immune system. Proc Natl Acad Sci USA. 2007;104:997–1002. doi: 10.1073/pnas.0609672104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aubry C, et al. OatA, a peptidoglycan O-acetyltransferase involved in Listeria monocytogenes immune escape, is critical for virulence. J Infect Dis. 2011;204:731–740. doi: 10.1093/infdis/jir396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Crimmins GT, et al. Listeria monocytogenes multidrug resistance transporters activate a cytosolic surveillance pathway of innate immunity. Proc Natl Acad Sci USA. 2008;105:10191–10196. doi: 10.1073/pnas.0804170105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bierne H, et al. Human BAHD1 promotes heterochromatic gene silencing. Proc Natl Acad Sci USA. 2009;106:13826–13831. doi: 10.1073/pnas.0901259106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lebreton A, et al. A bacterial protein targets the BAHD1 chromatin complex to stimulate type III interferon response. Science. 2011;331:1319–1321. doi: 10.1126/science.1200120. [DOI] [PubMed] [Google Scholar]
- 77.Cotter PD, et al. Listeriolysin S, a novel peptide haemolysin associated with a subset of lineage I Listeria monocytogenes. PLoS Pathog. 2008;4:e1000144. doi: 10.1371/journal.ppat.1000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pizarro-Cerdá J, Cossart P. Bacterial adhesion and entry into host cells. Cell. 2006;124:715–727. doi: 10.1016/j.cell.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 79.Pizarro-Cerdá J, Cossart P. Listeria monocytogenes membrane trafficking and lifestyle: The exception or the rule? Annu Rev Cell Dev Biol. 2009;25:649–670. doi: 10.1146/annurev.cellbio.042308.113331. [DOI] [PubMed] [Google Scholar]
- 80.Seveau S, Pizarro-Cerda J, Cossart P. Molecular mechanisms exploited by Listeria monocytogenes during host cell invasion. Microbes Infect. 2007;9:1167–1175. doi: 10.1016/j.micinf.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 81.Niemann HH, et al. Structure of the human receptor tyrosine kinase met in complex with the Listeria invasion protein InlB. Cell. 2007;130:235–246. doi: 10.1016/j.cell.2007.05.037. [DOI] [PubMed] [Google Scholar]
- 82.Schubert WD, et al. Structure of internalin, a major invasion protein of Listeria monocytogenes, in complex with its human receptor E-cadherin. Cell. 2002;111:825–836. doi: 10.1016/s0092-8674(02)01136-4. [DOI] [PubMed] [Google Scholar]
- 83.Veiga E, Cossart P. Listeria hijacks the clathrin-dependent endocytic machinery to invade mammalian cells. Nat Cell Biol. 2005;7:894–900. doi: 10.1038/ncb1292. [DOI] [PubMed] [Google Scholar]
- 84.Veiga E, Cossart P. The role of clathrin-dependent endocytosis in bacterial internalization. Trends Cell Biol. 2006;16:499–504. doi: 10.1016/j.tcb.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Veiga E, et al. Invasive and adherent bacterial pathogens co-opt host clathrin for infection. Cell Host Microbe. 2007;2:340–351. doi: 10.1016/j.chom.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bonazzi M, et al. Clathrin phosphorylation is required for actin recruitment at sites of bacterial adhesion and internalization. J Cell Biol. 2011;195:525–536. doi: 10.1083/jcb.201105152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pizarro-Cerdá J, Bonazzi M, Cossart P. Clathrin-mediated endocytosis: What works for small, also works for big. Bioessays. 2010;32:496–504. doi: 10.1002/bies.200900172. [DOI] [PubMed] [Google Scholar]
- 88.Mostowy S, et al. Septins regulate bacterial entry into host cells. PLoS ONE. 2009;4:e4196. doi: 10.1371/journal.pone.0004196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mostowy S, et al. Septin 11 restricts InlB-mediated invasion by Listeria. J Biol Chem. 2009;284:11613–11621. doi: 10.1074/jbc.M900231200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vazquez-Boland JA, et al. Nucleotide sequence of the lecithinase operon of Listeria monocytogenes and possible role of lecithinase in cell-to-cell spread. Infect Immun. 1992;60:219–230. doi: 10.1128/iai.60.1.219-230.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Singh R, Jamieson A, Cresswell P. GILT is a critical host factor for Listeria monocytogenes infection. Nature. 2008;455:1244–1247. doi: 10.1038/nature07344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Radtke AL, et al. Listeria monocytogenes exploits cystic fibrosis transmembrane conductance regulator (CFTR) to escape the phagosome. Proc Natl Acad Sci USA. 2011;108:1633–1638. doi: 10.1073/pnas.1013262108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Van Troys M, et al. The actin propulsive machinery: The proteome of Listeria monocytogenes tails. Biochem Biophys Res Commun. 2008;375:194–199. doi: 10.1016/j.bbrc.2008.07.152. [DOI] [PubMed] [Google Scholar]
- 94.Mostowy S, et al. Entrapment of intracytosolic bacteria by septin cage-like structures. Cell Host Microbe. 2010;8:433–444. doi: 10.1016/j.chom.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 95.Bonazzi M, Veiga E, Pizarro-Cerdá J, Cossart P. Successive post-translational modifications of E-cadherin are required for InlA-mediated internalization of Listeria monocytogenes. Cell Microbiol. 2008;10:2208–2222. doi: 10.1111/j.1462-5822.2008.01200.x. [DOI] [PubMed] [Google Scholar]
- 96.Brundage RA, Smith GA, Camilli A, Theriot JA, Portnoy DA. Expression and phosphorylation of the Listeria monocytogenes ActA protein in mammalian cells. Proc Natl Acad Sci USA. 1993;90:11890–11894. doi: 10.1073/pnas.90.24.11890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chong R, et al. Regulatory mimicry in Listeria monocytogenes actin-based motility. Cell Host Microbe. 2009;6:268–278. doi: 10.1016/j.chom.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schnupf P, Portnoy DA, Decatur AL. Phosphorylation, ubiquitination and degradation of listeriolysin O in mammalian cells: Role of the PEST-like sequence. Cell Microbiol. 2006;8:353–364. doi: 10.1111/j.1462-5822.2005.00631.x. [DOI] [PubMed] [Google Scholar]
- 99.Baldwin DN, Vanchinathan V, Brown PO, Theriot JA. A gene-expression program reflecting the innate immune response of cultured intestinal epithelial cells to infection by Listeria monocytogenes. Genome Biol. 2003;4:R2. doi: 10.1186/gb-2002-4-1-r2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nau GJ, et al. Human macrophage activation programs induced by bacterial pathogens. Proc Natl Acad Sci USA. 2002;99:1503–1508. doi: 10.1073/pnas.022649799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.McCaffrey RL, et al. A specific gene expression program triggered by Gram-positive bacteria in the cytosol. Proc Natl Acad Sci USA. 2004;101:11386–11391. doi: 10.1073/pnas.0403215101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Leber JH, et al. Distinct TLR- and NLR-mediated transcriptional responses to an intracellular pathogen. PLoS Pathog. 2008;4:e6. doi: 10.1371/journal.ppat.0040006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tchatalbachev S, Ghai R, Hossain H, Chakraborty T. Gram-positive pathogenic bacteria induce a common early response in human monocytes. BMC Microbiol. 2010;10:275. doi: 10.1186/1471-2180-10-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lecuit M, Sonnenburg JL, Cossart P, Gordon JI. Functional genomic studies of the intestinal response to a foodborne enteropathogen in a humanized gnotobiotic mouse model. J Biol Chem. 2007;282:15065–15072. doi: 10.1074/jbc.M610926200. [DOI] [PubMed] [Google Scholar]
- 105.Hamon MA, Cossart P. Histone modifications and chromatin remodeling during bacterial infections. Cell Host Microbe. 2008;4:100–109. doi: 10.1016/j.chom.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 106.Birmingham CL, et al. Listeria monocytogenes evades killing by autophagy during colonization of host cells. Autophagy. 2007;3:442–451. doi: 10.4161/auto.4450. [DOI] [PubMed] [Google Scholar]
- 107.Mostowy S, et al. p62 and NDP52 proteins target intracytosolic Shigella and Listeria to different autophagy pathways. J Biol Chem. 2011;286:26987–26995. doi: 10.1074/jbc.M111.223610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Woodward JJ, Iavarone AT, Portnoy DA. c-di-AMP secreted by intracellular Listeria monocytogenes activates a host type I interferon response. Science. 2010;328:1703–1705. doi: 10.1126/science.1189801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.McWhirter SM, et al. A host type I interferon response is induced by cytosolic sensing of the bacterial second messenger cyclic-di-GMP. J Exp Med. 2009;206:1899–1911. doi: 10.1084/jem.20082874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Burdette DL, et al. STING is a direct innate immune sensor of cyclic di-GMP. Nature. 2011;478:515–518. doi: 10.1038/nature10429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dolowschiak T, et al. Potentiation of epithelial innate host responses by intercellular communication. PLoS Pathog. 2010;6:e1001194. doi: 10.1371/journal.ppat.1001194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kasper CA, et al. Cell-cell propagation of NF-κB transcription factor and MAP kinase activation amplifies innate immunity against bacterial infection. Immunity. 2010;33:804–816. doi: 10.1016/j.immuni.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 113.Pamer EG. Immune responses to Listeria monocytogenes. Nat Rev Immunol. 2004;4:812–823. doi: 10.1038/nri1461. [DOI] [PubMed] [Google Scholar]
- 114.Lecuit M, et al. A single amino acid in E-cadherin responsible for host specificity towards the human pathogen Listeria monocytogenes. EMBO J. 1999;18:3956–3963. doi: 10.1093/emboj/18.14.3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Khelef N, Lecuit M, Bierne H, Cossart P. Species specificity of the Listeria monocytogenes InlB protein. Cell Microbiol. 2006;8:457–470. doi: 10.1111/j.1462-5822.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- 116.Lecuit M, et al. A transgenic model for listeriosis: Role of internalin in crossing the intestinal barrier. Science. 2001;292:1722–1725. doi: 10.1126/science.1059852. [DOI] [PubMed] [Google Scholar]
- 117.Disson O, et al. Conjugated action of two species-specific invasion proteins for fetoplacental listeriosis. Nature. 2008;455:1114–1118. doi: 10.1038/nature07303. [DOI] [PubMed] [Google Scholar]
- 118.Levraud JP, et al. Real-time observation of listeria monocytogenes-phagocyte interactions in living zebrafish larvae. Infect Immun. 2009;77:3651–3660. doi: 10.1128/IAI.00408-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mukherjee K, et al. Galleria mellonella as a model system for studying Listeria pathogenesis. Appl Environ Microbiol. 2010;76:310–317. doi: 10.1128/AEM.01301-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jensen RL, Pedersen KS, Loeschcke V, Ingmer H, Leisner JJ. Limitations in the use of Drosophila melanogaster as a model host for gram-positive bacterial infection. Lett Appl Microbiol. 2007;44:218–223. doi: 10.1111/j.1472-765X.2006.02040.x. [DOI] [PubMed] [Google Scholar]
- 121.Thomsen LE, Slutz SS, Tan MW, Ingmer H. Caenorhabditis elegans is a model host for Listeria monocytogenes. Appl Environ Microbiol. 2006;72:1700–1701. doi: 10.1128/AEM.72.2.1700-1701.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pentecost M, Otto G, Theriot JA, Amieva MR. Listeria monocytogenes invades the epithelial junctions at sites of cell extrusion. PLoS Pathog. 2006;2:e3. doi: 10.1371/journal.ppat.0020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nikitas G, et al. Transcytosis of Listeria monocytogenes across the intestinal barrier upon specific targeting of goblet cell accessible E-cadherin. J Exp Med. 2011;208:2263–2277. doi: 10.1084/jem.20110560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lecuit M, et al. Targeting and crossing of the human maternofetal barrier by Listeria monocytogenes: Role of internalin interaction with trophoblast E-cadherin. Proc Natl Acad Sci USA. 2004;101:6152–6157. doi: 10.1073/pnas.0401434101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Patel JC, Hueffer K, Lam TT, Galan JE. Diversification of a Salmonella virulence protein function by ubiquitin-dependent differential localization. Cell. 2009;137:283–294. doi: 10.1016/j.cell.2009.01.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Paterson Y, Guirnalda PD, Wood LM. Listeria and Salmonella bacterial vectors of tumor-associated antigens for cancer immunotherapy. Semin Immunol. 2010;22:183–189. doi: 10.1016/j.smim.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.