Abstract
Purpose
There is increasing concern that environmental chemicals have a direct effect on fertility. Heavy metals such as mercury have been shown to affect various organ systems in humans including nervous system and skin, however they could also act as endocrine disrupting chemicals adversely affecting fertility. Metals such as zinc and selenium are essential micronutrients with diverse functions that may be important for reproductive outcomes. We measured mercury, zinc and selenium levels in the hair, a reliable reflection of long term environmental exposure and dietary status, to correlate with the outcome of ovarian hyperstimulation for in vitro fertilisation (IVF) treatment.
Methods
We analysed the hair of 30 subfertile women for mercury, zinc and selenium using inductively coupled mass spectrometry. Each woman underwent one cycle of IVF treatment. Correlation between the levels of these trace metals and treatment outcomes was investigated.
Results
Thirty women were recruited with mean (±SD) age of 32.7(4.4) years and BMI of 25.4(5.0)kg/m2. Hair mercury concentration showed a negative correlation with oocyte yield (p < 0.05,βcoefficient 0.38) and follicle number (p = 0.03,β coefficient0.19) after ovarian stimulation. Zinc and selenium levels in hair correlated positively with oocyte yield after ovarian stimulation (p < 0.05,β coefficient0.15) and (p = 0.03,β coefficient0.21) respectively. Selenium levels in hair correlated significantly with follicle number following stimulation (p = 0.04, βcoefficient0.22). There was no correlation between mercury, zinc and selenium in hair and their corresponding serum levels.
Conclusion
These data suggest that mercury had a deleterious effect whilst there was a positive effect for zinc and selenium in the ovarian response to gonadotrophin therapy for IVF. Hair analysis offers a novel method of investigating the impact of long-term exposure to endocrine disruptors and nutritional status on reproductive outcomes.
Keywords: IVF, Heavy metals, Endocrine disruptors
Subfertility affects approximately 1 in 6 couples in the developed world [1], a prevalence that is likely to increase as more women delay childbirth to a later age [2]; approximately 28% of couples investigated for subfertility have a diagnosis of ‘unexplained subfertility’ [3]. Current treatment largely consists of assisted reproductive techniques (ART) such as IVF or IVF-ICSI, often regardless of the underlying cause. The average success rate of 25–30% for ART in Europe remains unchanged over recent years [4], prompting the search for additional factors which may influence fertility treatments and optimise success, and the identification of adverse factors such as endocrine disrupting chemicals.
Although the overall contribution of environmental chemical exposure to infertility is unknown, the available literature suggests that exposure to various environmental factors, may dramatically affect adult fertility [5]. Studies of various contaminant-exposed wildlife populations suggest that multiple mechanisms contribute to changes in gonadal development, maturation of germ cells, fertilization and pregnancy, specifically, the endocrine processes supporting these events [6]. Heavy metal exposure has been identified as a factor affecting human fertility [7]. They may induce hormonal disorders, preventing ovulation and pregnancies [8, 9]. Mercury is one of the heavy metals known to be one of such endocrine disruptors and in a few studies exposure to mercury has been associated with reproductive problems, such as spontaneous abortion, stillbirths, congenital malformations, infertility, disturbances in the menstrual cycle, inhibition of the ovulation and behavioural effects of the offspring [10, 11]. Mercury can also affect the meiotic maturation of mouse oocytes and injure or reduce the reproductive capacity of the mouse [12].
Nutrition is critical in reproductive success [13]. An adequate intake of elements acting as enzyme co-factors for DNA synthesis and catalysing antioxidant reactions may be of significance; these elements are likely to have a role in folliculogenesis and oocyte maturation where DNA synthesis and reduction of harmful reactive oxygen species (ROS) are crucial processes [14]. However, the relevance of these elements to human infertility treatments is not clearly defined in the literature, particularly in the female. Zinc and selenium are two of such heavy metals which are important for human health.
Measurement of levels of trace elements in hair has been demonstrated to be a reliable indicator of the long term exposure to these elements [15] whilst serum levels are known to reflect more recent exposure. Both methods have previously been used to assess the impact of heavy metals on human health and disease [16–18].
We conducted this prospective pilot study to assess the impact of long and short term heavy metal exposure status of mercury, zinc and selenium on the gonadal reponse to gonadotrophin stimulation during a standard long-protocol agonist IVF cycle.
Methods
The study was approved by Hull and East Riding Local Research Ethics Committee. Informed written consent was obtained from all patients. All women from couples presenting with subfertility, but without evidence of prior ovulation, were invited to participate in this study. A lock of hair of approximately 5 g was cut from the nape of the neck, between two and seven days prior to the start of the IVF cycle. At the same time a venous blood sample was collected.
Hair samples were weighed then washed 3x in acetone to remove external contamination, as recommended by the International Atomic Energy Association (IAEA) (Report on the Second Research Co-ordination Meeting of IAEA, Neuherberg, 1985), and left to dry in a vacuum oven at 40°C overnight. When dry, each sample was digested in 0.5 ml concentrated nitric acid in a Teflon PFA microdigestion vessel for 24 h. The samples were then microwave heated for 30 min at a maximum of 100°C. When cool, each digest was diluted to a standard volume (5 ml) with water incorporating internal standards. Analysis was performed using a Perkin Elmer Elan DRCII inductively coupled plasma mass spectrometer (ICP-MS).
Venous blood samples were centrifuged and the serum snap-frozen after collection. When ready for analysis, the samples were thawed at room temperature and a 0.5 ml aliquot mixed with 0.5 ml concentrated nitric acid. Mercury was not measured in blood, since it remains in the blood stream for only few days after exposure. The samples were centrifuged then diluted to a standard volume of 5 ml with water incorporating internal standards. Analysis was performed using a Perkin Elmer Elan DRCII ICP-MS.
Patients underwent down-regulation with Buserelin Acetate for at least 2 weeks before super-ovulation with a recombinant FSH preparation; the initial dose given based on the patient’s age and baseline serum FSH levels, then titrated to ovarian response. HCG was administered after USS monitoring of mature follicle development (size >17 mm). Follicle count was assessed by trans-vaginal ultrasound, and oocyte retrieval performed 36 h after HCG administration. The treatment cycle was abandoned prior to oocyte collection if the total follicle count was below 5, above 25 or if other signs/symptoms of hyperstimulation were observed. None of the patients had IVF cycles prior to study cycle. None of the patients were on hormonal contraceptives for at least 2 years prior to study cycle.
Correlation was sought between the levels of heavy metals hair (mercury, zinc, selenium) and serum (zinc and selenium) and outcomes of the subsequent classic IVF cycle (Follicle count, oocyte yield at collection, fertilisation and cleavage rates and average embryo quality) using Poisson regression analysis (independent of age and body mass index (BMI) and dose of stimulation drug used). A p value of < 0.05 was regarded as statistically significant.
The study was powered according to the sample size for pilot studies [19]. A minimum of 20°-of-freedom was required to estimate effect size and variability; hence, we intended to recruit 25–35 patients allowing for drop-outs and covariate adjustment.
Results
A total of 30 women were recruited to the study over a period of 18 month. The mean (±SD) age was 32.7 (4.4) years (range: 26–42 years) and BMI was 25.4 (5.0) kg/m2(range: 18.5–32.1 kg/m2). The mercury concentration in hair was 0.89 ± 0.3 μg/g. The hair and serum levels of zinc were 103.9 (37.0) μg/g and 897.3 (386.4) μg/g respectively. The hair and serum levels of selenium were 0.89 (0.5) μg/g and 100.2 (19.7) μg/g respectively. There was no correlation between the levels of zinc and selenium in hair and their corresponding serum levels.
The mean (SD) follicle count was 13.0 (8.5) and the mean oocyte yield was 9.1(4.9). The mean fertilisation and cleavage rates were 73.8(21.6)% and 77.8 (26.9)% respectively. The mean duration of ovulation stimulation was 11.1 (2.3) days (range: 8–13 days). The mean day 2 FSH was normal (5.8 (1.6) mIU/ml) suggesting sufficient baseline ovarian reserve. Two women had ovarian hyperstimulation (36 and 37 follicles respectively) and one failed to stimulate (0 follicles).
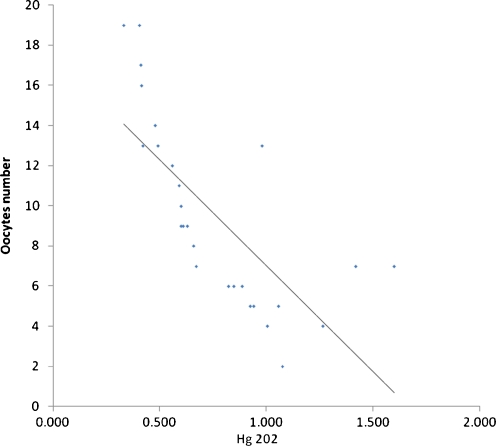
Mercury concentration in hair showed a strong negative correlation after adjustment for age and BMI with oocyte yield (number collected) (p < 0.05, β coefficient 0.38) (Fig. 1) and follicle number (p = 0.03, β coefficient 0.19) after ovarian stimulation.
Fig. 1.
Scatter plot with line of best fit showing a positive correlation between the hair level of mercury (Hg 202) in x axis and the number of oocytes collected after controlled ovarian stimulation in y axis. (n = 27)
Zinc levels in hair correlated significantly with oocyte yield (number collected) after ovarian stimulation (p < 0.05, β coefficient 0.15) after adjustment for age and BMI (Fig. 2). This relationship was linear within the range of values detected. There was no significant relationship between zinc levels in hair and follicle number.
Fig. 2.
Scatter plot with line of best fit showing a positive correlation between the hair level of zinc and the number of oocytes collected after controlled ovarian stimulation (n = 27)
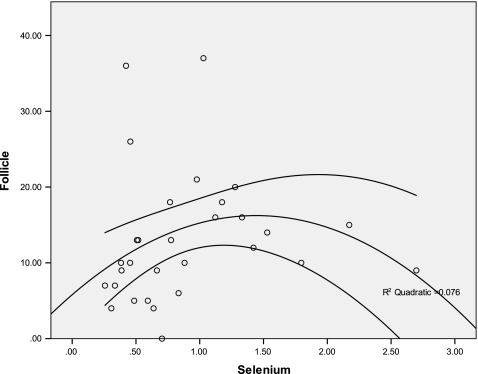
Selenium levels in hair also correlated significantly with oocyte yield after ovarian stimulation (p = 0.03, β coefficient 0.21). Selenium levels in hair correlated significantly with follicle number following stimulation (p = 0.04, β coefficient 0.22) after adjustment for age and BMI (Fig. 3). The correlation between selenium levels in hair and follicle and oocyte counts was non-linear and closest around a level of 1.5 μg/g.
Fig. 3.
Scatter plot with line of best fit showing correlation between the hair level of selenium and the number of follicles counted after controlled ovarian stimulation (n = 30)
There was no correlation between the levels of mercury, zinc and selenium in hair and the fertilisation rate, cleavage rate or average embryo quality after IVF in these women. There was no correlation between the serum levels of zinc and selenium and any IVF outcome parameter.
There was a negative correlation between the serum selenium level and BMI (p = 0.02), but no correlation between hair level of selenium and BMI. There was no significant correlation between zinc in hair or serum and BMI.
Discussion
There was a strong negative correlation between mercury concentration in hair and the ovarian response to gonadotrophin stimulation after an IVF cycle. Conversely, there was a positive correlation between the levels of zinc and selenium in hair in the ovarian response to gonadotrophin stimulation.
There was a significant negative correlation between mercury concentration in hair with follicle count and number of oocytes retrieved after ovarian stimulation even after adjusting for age and BMI. There have been numerous studies on the effects of mercury on the immune system, renal system, cardiovascular, reproductive system and the central nervous system. Human exposure to organic, inorganic and metallic mercury occurs primarily from the consumption of fish, the use of medicinal and cosmetic compounds and dental amalgam, respectively [5, 20]. Additionally, the general population is primarily exposed to mercury through diet and dental amalgam [21]. Some studies have reported women's use of skin-lightening creams and soaps [22, 23] and its association with mercury exposure and this can be of significance for certain ethnic groups [24]. Exposure to metallic mercury alters oestrous cyclicity, but has no significant effect on ovulation, implantation or maintenance of first pregnancy during exposure of short duration in female rats [25]. Prenatal low exposure of mercury from fish consumption during pregnancy has detrimental effects on neurocognitive development in later life [26–28]. It has also been shown that the blood levels of mercury is higher in infertile couples than fertile couples [29]. The current study shows that higher mercury concentration in hair could signify a poorer response to IVF treatment.
This study showed a positive correlation between the levels of zinc and selenium in hair and the ovarian response to gonadotrophin stimulation for an IVF cycle. Levels of trace elements in hair have been shown to reliably reflect long term nutritional status [15]. Dietary sources of zinc are mainly from high protein foods such as red meats and seafood, and as such the vegetarian diet is prone to lead to deficiency [30]. High levels of selenium are found in brazil nuts, kidney, seafood and cereals, although this is soil dependent and it has been reported that European intake of selenium is falling [31]. Zinc acts as a co-factor for enzymes promoting DNA transcription and protein synthesis [32], has a role in expression of steroid hormone receptors [33] and has anti-apoptotic [34] and anti-oxidant properties [35]. Studies have demonstrated that a zinc deficiency can lead to subfertility and abnormal reproductive outcomes [36], and to pregnancy complications [37, 38]. However, previous studies have failed to confirm a role for zinc in human infertility or the response to fertility treatments. One case control study of 48 infertile women and 35 controls found no difference in plasma levels of zinc between the two groups so concluded there was no role for zinc in the pathogenesis of infertility [39]. However, the study measured only plasma zinc concentrations, which only reflect short term zinc turnover. A further study of the zinc levels in the follicular fluid of 33 follicles taken during ART found no difference in the levels between follicles of different sizes, and those that yielded oocytes that were successful and unsuccessful in fertilisation [40], but no additional confirmatory studies have been undertaken.
Selenium levels in hair correlated significantly with follicle number and oocyte yield after ovarian stimulation, this result remained significant after adjustment of age and BMI. Selenium is a key component of selenoproteins (selenium dependent enzymes with powerful antioxidant properties). In particular, the selenoenzyme glutathione peroxidase (GSHPx) catalyses the reduction of hydrogen peroxides and lipid hydroperoxides thereby protecting cellular structures from further oxidative damage [41]. In animal models selenium deficiency is associated with infertility and miscarriage, and selenium supplementation in sheep has been shown to prevent early miscarriage [42]. In humans, low levels of selenium have been shown to be associated with miscarriage [43], recurrent miscarriage in particular [44] and pre-eclampsia [45]. Previous studies have demonstrated an important role for GSHPx activity in human follicular fluid. One study on the follicular fluid of 112 patients about to undergo IVF demonstrated a significantly higher level of GSHPx activity in the follicular fluid of those who subsequently had successful fertilisation compared to those who did not [46].
It appears that the positive relationship between selenium and both oocyte and follicle counts becomes less so at around 1.5 μg/g which may reflect a level above which higher levels of selenium confer no additional benefit on outcome. We found no correlation between the hair and serum levels of zinc and selenium, or the serum levels and response to ovarian stimulation. This finding is supported by previous studies which demonstrated no correlation between hair and serum levels of trace elements; a previous study on levels of selenium in women with recurrent miscarriage found a significant influence of hair levels on outcome, but not serum levels [44]. This suggests that long term nutritional status is more important than short term turnover of trace elements on metabolic processes. The advantages of hair analysis over other biological samples are that trace metal concentrations in hair are not subjected to rapid fluctuations due to short term exposures hence reflects long term nutritional status. Analysis of hair offers a novel method of assessment of lifestyle factors which may be of relevance to infertility.
All subjects had normal FSH levels on day 2 suggesting sufficient baseline ovarian reserve, although anti-Mullerian hormone levels were not available to us and therefore not performed. It would be interesting to adjust for ovarian reserve and other variables and this should be clarified in larger prospective studies.
In conclusion, our results suggest that mercury may act as an endocrine disruptor with a deleterious effect on the ovarian response to gonadotrophin therapy, whilst conversely zinc and selenium may be important in reproductive success and their deficiency sought and addressed for optimum response to therapy.
Footnotes
Capsule Mercury concentration in hair had a deleterious effect where as zinc and selenium had a beneficial effect in ovarian response to gonadotrophin therapy for IVF.
References
- 1.Templeton A, Fraser C, Thompson B. The epidemiology of infertility in Aberdeen. BMJ. 1990;301(6744):148–152. doi: 10.1136/bmj.301.6744.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Botting B, Dunnell K. Trends in fertility and contraception in the last quarter of the 20th century. Popul Trends. 2000;100:32–39. [PubMed] [Google Scholar]
- 3.Hull MG, Glazener CM, Kelly NJ, et al. Population study of causes, treatment, and outcome of infertility. Br Med J (Clin Res Ed). 1985;291(6510):1693–1697. doi: 10.1136/bmj.291.6510.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andersen AN, Goossens V, Ferraretti AP, et al. Assisted reproductive technology in Europe, 2004: results generated from European registers by ESHRE. Hum Reprod. 2008;23(4):756–771. doi: 10.1093/humrep/den014. [DOI] [PubMed] [Google Scholar]
- 5.Al-Saleh I, Coskun S, Mashhour A, et al. Exposure to heavy metals (lead, cadmium and mercury) and its effect on the outcome of in-vitro fertilization treatment. Int J Hyg Environ Health. 2008;211(5–6):560–579. doi: 10.1016/j.ijheh.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Guillette LJ, Jr, Moore BC. Environmental contaminants, fertility, and multioocytic follicles: a lesson from wildlife? Semin Reprod Med. 2006;24(3):134–141. doi: 10.1055/s-2006-944419. [DOI] [PubMed] [Google Scholar]
- 7.Sharara FI, Seifer DB, Flaws JA. Environmental toxicants and female reproduction. Fertil Steril. 1998;70(4):613–622. doi: 10.1016/s0015-0282(98)00253-2. [DOI] [PubMed] [Google Scholar]
- 8.Choi SM, Yoo SD, Lee BM. Toxicological characteristics of endocrine-disrupting chemicals: developmental toxicity, carcinogenicity, and mutagenicity. J Toxicol Environ Health B Crit Rev. 2004;7(1):1–24. doi: 10.1080/10937400490253229. [DOI] [PubMed] [Google Scholar]
- 9.Gerhard I, Runnebaum B. The limits of hormone substitution in pollutant exposure and fertility disorders. Zentralbl Gynakol. 1992;114(12):593–602. [PubMed] [Google Scholar]
- 10.Gardella JR, Hill JA., 3rd Environmental toxins associated with recurrent pregnancy loss. Semin Reprod Med. 2000;18(4):407–424. doi: 10.1055/s-2000-13731. [DOI] [PubMed] [Google Scholar]
- 11.Takahashi Y, Tsuruta S, Arimoto M, Tanaka H, Yoshida M. Placental transfer of mercury in pregnant rats which received dental amalgam restorations. Toxicology. 2003;185(1–2):23–33. doi: 10.1016/s0300-483x(02)00588-7. [DOI] [PubMed] [Google Scholar]
- 12.Shen W, Chen Y, Li C, Ji Q. Effect of mercury chloride on the reproductive function and visceral organ of female mouse. Wei Sheng Yan Jiu. 2000;29(2):75–77. [PubMed] [Google Scholar]
- 13.Ebisch IM, Thomas CM, Peters WH, Braat DD, Steegers-Theunissen RP. The importance of folate, zinc and antioxidants in the pathogenesis and prevention of subfertility. Hum Reprod Update. 2007;13(2):163–174. doi: 10.1093/humupd/dml054. [DOI] [PubMed] [Google Scholar]
- 14.Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:28. doi: 10.1186/1477-7827-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lorenzo Alonso MJ, Bermejo Barrera A, Cocho de Juan JA, Fraga Bermudez JM, Bermejo Barrera P. Selenium levels in related biological samples: human placenta, maternal and umbilical cord blood, hair and nails. J Trace Elem Med Biol. 2005;19(1):49–54. doi: 10.1016/j.jtemb.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Yokoi K, Egger NG, Ramanujam VM, et al. Association between plasma zinc concentration and zinc kinetic parameters in premenopausal women. Am J Physiol Endocrinol Metab. 2003;285(5):E1010–E1020. doi: 10.1152/ajpendo.00533.2002. [DOI] [PubMed] [Google Scholar]
- 17.Izquierdo Alvarez S, Castanon SG, Ruata ML, et al. Updating of normal levels of copper, zinc and selenium in serum of pregnant women. J Trace Elem Med Biol. 2007;21(Suppl 1):49–52. doi: 10.1016/j.jtemb.2007.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Razagui IB, Haswell SJ. The determination of mercury and selenium in maternal and neonatal scalp hair by inductively coupled plasma-mass spectrometry. J Anal Toxicol. 1997;21(2):149–153. doi: 10.1093/jat/21.2.149. [DOI] [PubMed] [Google Scholar]
- 19.Birkett MA, Day SJ. Internal pilot studies for estimating sample size. Stat Med. 1994;13(23–24):2455–2463. doi: 10.1002/sim.4780132309. [DOI] [PubMed] [Google Scholar]
- 20.Clifton JC., 2nd Mercury exposure and public health. Pediatr Clin North Am. 2007;54(2):237–269. doi: 10.1016/j.pcl.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 21.WHO. Environmental Health Criteria 118: Inorganic Mercury. In: World Health Organisation G, ed.
- 22.McRill C, Boyer LV, Flood TJ, Ortega L. Mercury toxicity due to use of a cosmetic cream. J Occup Environ Med. 2000;42(1):4–7. doi: 10.1097/00043764-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 23.al-Saleh I, Shinwari N. Urinary mercury levels in females: influence of skin-lightening creams and dental amalgam fillings. Biometals. 1997;10(4):315–323. doi: 10.1023/a:1018380501673. [DOI] [PubMed] [Google Scholar]
- 24.McKelvey W, Jeffery N, Clark N, Kass D, Parsons PJ. Population-based inorganic mercury biomonitoring and the identification of skin care products as a source of exposure in New York City. Environ Health Perspect. 2011;119(2):203–209. doi: 10.1289/ehp.1002396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis BJ, Price HC, O'Connor RW, Fernando R, Rowland AS, Morgan DL. Mercury vapor and female reproductive toxicity. Toxicol Sci. 2001;59(2):291–296. doi: 10.1093/toxsci/59.2.291. [DOI] [PubMed] [Google Scholar]
- 26.Oken E, Radesky JS, Wright RO, et al. Maternal fish intake during pregnancy, blood mercury levels, and child cognition at age 3 years in a US cohort. Am J Epidemiol. 2008;167(10):1171–1181. doi: 10.1093/aje/kwn034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geier DA, Kern JK, Geier MR. A prospective study of prenatal mercury exposure from maternal dental amalgams and autism severity. Acta Neurobiol Exp (Wars). 2009;69(2):189–197. doi: 10.55782/ane-2009-1744. [DOI] [PubMed] [Google Scholar]
- 28.Myers GJ, Thurston SW, Pearson AT, et al. Postnatal exposure to methyl mercury from fish consumption: a review and new data from the Seychelles Child Development Study. Neurotoxicology. 2009;30(3):338–349. doi: 10.1016/j.neuro.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choy CM, Lam CW, Cheung LT, Briton-Jones CM, Cheung LP, Haines CJ. Infertility, blood mercury concentrations and dietary seafood consumption: a case-control study. BJOG. 2002;109(10):1121–1125. doi: 10.1111/j.1471-0528.2002.02084.x. [DOI] [PubMed] [Google Scholar]
- 30.Craig WJ. Health effects of vegan diets. Am J Clin Nutr. 2009;89(5):1627S–1633S. doi: 10.3945/ajcn.2009.26736N. [DOI] [PubMed] [Google Scholar]
- 31.Rayman MP. Dietary selenium: time to act. BMJ. 1997;314(7078):387–388. doi: 10.1136/bmj.314.7078.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Falchuk KH. The molecular basis for the role of zinc in developmental biology. Mol Cell Biochem. 1998;188(1–2):41–48. [PubMed] [Google Scholar]
- 33.Freedman LP. Anatomy of the steroid receptor zinc finger region. Endocr Rev. 1992;13(2):129–145. doi: 10.1210/edrv-13-2-129. [DOI] [PubMed] [Google Scholar]
- 34.Stefanidou M, Maravelias C, Dona A, Spiliopoulou C. Zinc: a multipurpose trace element. Arch Toxicol. 2006;80(1):1–9. doi: 10.1007/s00204-005-0009-5. [DOI] [PubMed] [Google Scholar]
- 35.Prasad AS. Zinc: mechanisms of host defense. J Nutr. 2007;137(5):1345–1349. doi: 10.1093/jn/137.5.1345. [DOI] [PubMed] [Google Scholar]
- 36.Bedwal RS, Bahuguna A. Zinc, copper and selenium in reproduction. Experientia. 1994;50(7):626–640. doi: 10.1007/BF01952862. [DOI] [PubMed] [Google Scholar]
- 37.Favier AE. The role of zinc in reproduction. Hormonal mechanisms. Biol Trace Elem Res. 1992;32:363–382. doi: 10.1007/BF02784623. [DOI] [PubMed] [Google Scholar]
- 38.Shah D, Sachdev HP. Zinc deficiency in pregnancy and fetal outcome. Nutr Rev. 2006;64(1):15–30. doi: 10.1111/j.1753-4887.2006.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 39.Soltan MH, Jenkins DM. Plasma copper and zinc concentrations and infertility. Br J Obstet Gynaecol. 1983;90(5):457–459. doi: 10.1111/j.1471-0528.1983.tb08944.x. [DOI] [PubMed] [Google Scholar]
- 40.Ng SC, Karunanithy R, Edirisinghe WR, Roy AC, Wong PC, Ratnam SS. Human follicular fluid levels of calcium, copper and zinc. Gynecol Obstet Invest. 1987;23(2):129–132. doi: 10.1159/000298848. [DOI] [PubMed] [Google Scholar]
- 41.Rayman MP. The importance of selenium to human health. Lancet. 2000;356(9225):233–241. doi: 10.1016/S0140-6736(00)02490-9. [DOI] [PubMed] [Google Scholar]
- 42.Munoz C, Carson AF, McCoy MA, et al. Effect of supplementation with barium selenate on the fertility, prolificacy and lambing performance of hill sheep. Vet Rec. 2009;164(9):265–271. doi: 10.1136/vr.164.9.265. [DOI] [PubMed] [Google Scholar]
- 43.Zachara BA, Dobrzynski W, Trafikowska U, Szymanski W. Blood selenium and glutathione peroxidases in miscarriage. BJOG. 2001;108(3):244–247. doi: 10.1111/j.1471-0528.2001.00030.x. [DOI] [PubMed] [Google Scholar]
- 44.Al-Kunani AS, Knight R, Haswell SJ, Thompson JW, Lindow SW. The selenium status of women with a history of recurrent miscarriage. BJOG. 2001;108(10):1094–1097. doi: 10.1111/j.1471-0528.2001.00253.x. [DOI] [PubMed] [Google Scholar]
- 45.Rayman MP, Bode P, Redman CW. Low selenium status is associated with the occurrence of the pregnancy disease preeclampsia in women from the United Kingdom. Am J Obstet Gynecol. 2003;189(5):1343–1349. doi: 10.1067/s0002-9378(03)00723-3. [DOI] [PubMed] [Google Scholar]
- 46.Paszkowski T, Traub AI, Robinson SY, McMaster D. Selenium dependent glutathione peroxidase activity in human follicular fluid. Clin Chim Acta. 1995;236(2):173–180. doi: 10.1016/0009-8981(95)98130-9. [DOI] [PubMed] [Google Scholar]