Abstract
Objective: This study measured health literacy in a population of teens in treatment for asthma or diabetes and tested the association between health literacy and willingness to use online health resources. Materials and Methods: About 180 patients aged 13–18 years treated for asthma or diabetes in specialty care clinics completed assessments of demographic characteristics, health literacy, and Internet access and use. Teens were provided a resource page listing selected publically available health-related Web sites and asked about perceived ease of use, perceived usefulness, and intent to use the listed Web sites. The relationship between demographic characteristics, health literacy, and online health information use was tested using chi-squared or Fisher's exact test. Predictors of intent to use resource page Web sites were assessed using bivariate and multivariate ordinal logistic regression. Results: About 92% of participants had adequate health literacy. Over 50% of participants had previously searched online for health information. Older age was the only significant predictor of health information search. Most teens (79%) reported intent to use at least one Web site from the resource page at least occasionally within the next 3 months. Higher health literacy (odds ratio [OR]=6.24, p<0.01) and stronger perceived usefulness (OR=1.74, p=0.01) were associated with greater intent for regular use, after controlling for demographic and Internet access variables. Conclusions: Teens with lower health literacy searched online for health information as often as peers with higher literacy, but were less likely to express the intent to use recommended sites. Belief in the usefulness of a Web site is the strongest attitudinal predictor of intended future use.
Key words: adolescents, asthma, diabetes, health literacy, Internet
Introduction
Online health resources have the potential to help teens with chronic illnesses transition from parental care to self-management of their conditions. Such Web sites can provide disease-specific health information, disease management tools, provider support, and peer support that can engage youths in managing their conditions.1–3 Interactive and entertaining Web sites may also be preferable to traditional paper-based diaries and educational materials.4
While 90% of U.S. teens use the Internet and 30% use the Internet to find health information,5 little is known about predictors of use in teens with chronic diseases, a group in great need of health information and disease management support. To date, research on e-health use in adults has found significant correlations with factors including age, race, education, Internet access, perceived ease of use, and perceived usefulness.6–13 These relationships, however, are not fixed for all e-health activities or all populations.14
Another important factor in use of online health resources is health literacy, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate healthcare decisions.”15,16 Research in adults has found that health literacy limitations are associated with poorer health knowledge, behaviors, and outcomes.17–23 Adults' health literacy also predicts their use of the Internet for health information. Data from the 2003 National Assessment of Adult Literacy showed that 85% of individuals with proficient health literacy got information about health issues from the Internet compared to only 19% of those with below basic health literacy.19 There are also concerns that Internet users with limited literacy may get less value from online health information.24
Little is known about health literacy and other potential correlates of health Internet use by adolescents, particularly among those with significant healthcare needs. It is possible that predictors of use in today's populations of wired teens may differ meaningfully from those seen in adults. To maximize the benefits of online health resources for teens with chronic illnesses, we must learn more about patient factors that affect their use of online health resources.
In this study, we examined the relationships among health literacy, sociodemographic characteristics, perceptions of health Web sites, and intent to use online health information in a population of teens with asthma and diabetes. These conditions were selected in part because they represent two of the most common chronic conditions facing teens in the United States. Asthma affects over 2 million U.S. teens, whereas nearly 200,000 teens have been diagnosed with diabetes.25,26 In addition to prevalence, these conditions were selected because they require significant self-management,27,28 and because many public Web sites supporting disease management of these conditions are currently available.29,30
Methods
Sample
Adolescents aged 13–18 years were recruited from the four asthma and diabetes specialty care clinics affiliated with Nationwide Children's Hospital (Columbus, Ohio). Patients were excluded if they or their parent(s) did not have sufficient English communication skill to provide informed consent for participation, or if no parent was present to provide informed consent for youths under age 18.
Procedures
One research assistant (RA) recruited participants in all the clinics. Data collection days for each clinic were determined based on when asthma and diabetes clinics were held and based on the number of age-eligible patients scheduled for the clinic session.
All potential participants were approached by the RA in the clinic waiting room. The RA described the study using a standardized script. If the patient met the eligibility requirements and the parent and patient provided the required consent and assent, the RA either conducted the interview at the clinic while the patient waited to see the doctor, or scheduled a return data collection visit for the youth. If the patient was called in to see the doctor before the protocol was finished, data collection was completed during waiting time in the examination room or after the medical visit. Participants received a gift card as thanks for their participation. The study was approved by the Institutional Review Board at Nationwide Children's Hospital.
Survey Instruments
Participants completed baseline assessments that measured demographics, health literacy, and Internet access and use. Demographic information collected included age, race, gender, and zip code. Percentage of households below the federal poverty level in the participant's zip code of residence, based on U.S. Census data, was used as a proxy for socio-economic status (SES). Participants living in zip codes with over 10% poverty (75th percentile of the study population) were categorized as lower SES. Internet use was assessed using items adapted from the Pew Internet and American Life Survey.5 These items measured how often and where participants accessed the Internet, and assessed their activities (e.g., e-mail and health information search) while online.
Functional health literacy was measured using the brief version of test of functional health literacy in adults (TOFHLA).31–33 Although this tool was designed for adults, a validation study has shown that the TOFHLA has similar psychometric properties among adolescents.25 Scores from the TOFHLA were categorized as inadequate (0–53), marginal (54–66), or adequate (67–100). Because low health literacy was rare in our population, we grouped the inadequate and marginal groups in a single category of less than adequate, consistent with previous research.34–36
Brief Orientation to Online Resources
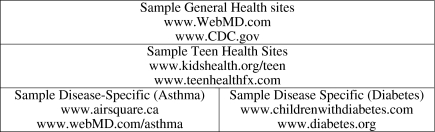
After the baseline data were collected, each participant was given an Online Health Resource Sheet. Separate sheets were developed for and provided to teens with asthma and teens with diabetes. Each resource sheet included disease-specific health information and disease management support Web sites, and also included general and teen-specific general health information Web sites (Fig. 1). Sites listed on the resource sheet were identified by the research team through a combination of Web searches, lay literature reviews, government agency recommendations, and personal experience. The goal was to select a small number of publically available sites with high face validity from reputable providers. The final list was approved by asthma and diabetes clinical specialists. All listed Web sites received HONCode certification from the Health on the Net (HON) Foundation, an international nongovernmental organization established to promote high-quality medical and health information on the Internet.37
Fig. 1.
Sample Web sites from the online health resource sheet.
The RA verbally explained the resource sheet to each participant using a standardized script. Participants were then asked about how they perceived the ease of use and usefulness of the described sites using items modified from previously validated Technology Acceptance Model questionnaires.38,39 The perceived ease of use score was calculated as the average agreement with the following statements: the system would be clear and understandable; the system would be easy to use; the system would be easy to learn; and the system would be easy to become skillful with. The perceived usefulness score was similarly calculated using the following three items: the system would be useful in managing my health; the system would help me accomplish tasks more quickly; the system would improve my chances of staying healthy. Patients expressed agreement with these perceptions using Likert scales anchored by 1=strongly disagree and 5=strongly agree.
Finally, intent to use these Web sites in the next 3 months using a single item which asked, “Which of these statements best describes your plans to use online health information sites like the ones presented today in the next 3 months?” The ordered response options were: I would…“never use one,” “try it once or twice but that's all,” “use it occasionally when I have a specific need,” or “use it regularly.”
Follow-Up Assessment of Use
Participants were each given a diary in which to record their use of online health information, including the sites listed on the resource sheet, over the subsequent 3 months. The diary pages were for personal use only and were not collected as part of the study. To minimize patient attrition from the study and maximize patients' retention of information about their online activity, we made four follow-up contacts with participants (two telephone calls and two mailings) reminding them to continue tracking their online health information use. At 3 months, participants were called and asked to complete a semi-structured telephone interview describing their use of health Web sites over the past 90 days. This interview asked specifically about the Web sites listed on the resource sheet. Participants were encouraged to refer to the diaries if they had used the diaries. Up to five attempts were made to contact each participant.
Statistical Analysis
We first determined the health literacy levels in the sample and tested associations between health literacy and participant characteristics including age, race, gender, health-related Internet use, and disease (asthma vs. diabetes). Association with health literacy as a categorical variable (adequate vs. less than adequate) was tested using a Fisher's exact test. Associations with literacy as a continuous variable were tested using the Wilcoxon rank sum test. Nonparametric options were selected because of small cell sizes and skewed data. Secondly, we examined the relationship between our ordinal intent to use variable and patient demographics, Internet access, health literacy, perceived ease of use, and perceived usefulness using ordinal logistic regression.
Results
We approached 387 youths to participate in the study, 164 youths with asthma, and 223 youths with diabetes. Twenty-one did not meet the study inclusion criteria leaving 366 eligible youths. Of these youths, 186 refused, citing reasons including “lack of time” or “not interested.” The resulting sample size was 180 with a participation rate of 49%. Included youths did not differ from refused/excluded youths by age, gender, or race (data not shown). Teens with asthma were more likely to participate than teens with diabetes (54% participation and 41% participation, respectively, p=0.01).
Health Literacy
Overall, 8% of the sample had less than adequate health literacy. The mean health literacy score was 88.9 with a range of 14–100. Higher health literacy was associated with being female, White, and older. Teens with asthma and teens with diabetes had similar levels of health literacy (Table 1).
Table 1.
Sample Description
| CHARACTERISTIC | NUMBER (%) | MEAN HEALTH LITERACY SCORE (SD) | % ADEQUATE HEALTH LITERACY |
|---|---|---|---|
| Total | 180 | 88.9 (15.0) | 92.2 |
| Age | |||
| 13 to 15 | 104 (57.8) | 87.4 (15.5)a | 92.3 |
| 16 to 18 | 76 (42.2) | 91.1 (14.2) | 92.1 |
| Gender | |||
| Male | 90 (50.0) | 86.9 (16.8)a | 90.0 |
| Female | 90 (50.0) | 91.0 (14.1) | 94.4 |
| Race | |||
| White | 130 (72.2) | 91.1 (12.0) | 95.4 |
| Black | 36 (20.0) | 80.6 (24.5)a | 77.8a |
| Other race | 14 (7.8) | 90.2 (7.9) | 100 |
| Disease | |||
| Asthma | 89 (49.4) | 89.3 (17.7) | 93.3 |
| Diabetes | 91 (50.6) | 88.6 (14.4) | 91.2 |
| Socio-economic status | |||
| High poverty zip | 114 (63.3) | 90.3 (13.8) | 93.9 |
| Low poverty zip | 66 (36.7) | 86.6 (16.8) | 89.4 |
Significant between group difference (p<0.05).
SD, standard deviation.
Use of Online Health Information
Ninety percent of the participants reported ever going online to surf the Web or to read e-mail and over half (57%) were daily Internet users (Table 2). Nearly half (48%) went online to find information about health, diet, or fitness and 20% searched online to find information about “things that are difficult to talk about like depression or substance use.” Use of the Internet for health information did not vary by disease. Use of online health information also did not vary significantly by health literacy level. Youth with lower health literacy were more likely to use the Internet for “things that are difficult to talk about …” (29% vs. 19%) but this difference did not reach statistical significance due to the small number of respondents who reported using the Internet for this purpose. Older teens and girls were more likely search for health information online.
Table 2.
Use of the Internet by Teens with Chronic Illness
| % EVER ACCESS THE INTERNET | % GOING ONLINE DAILY | % LOOKING FOR INFO ON HEALTH | % LOOKING FOR INFO ON SENSITIVE HEALTH ISSUES | |
|---|---|---|---|---|
| Total | 89.9 | 56.7 | 48.3 | 19.7 |
| Age | ||||
| 13 to 15 | 86.5 | 56.7 | 34.0a | 13.6a |
| 16 to 18 | 94.7 | 56.6 | 68.0 | 28.0 |
| Gender | ||||
| Male | 87.8 | 54.4 | 46.1 | 12.4a |
| Female | 92.1 | 58.9 | 50.6 | 27.0 |
| Race | ||||
| White | 90.7 | 53.1 | 47.3 | 17.8 |
| Black | 88.6 | 63.9 | 51.4 | 25.7 |
| Other race | 85.7 | 71.4 | 50.0 | 21.4 |
| Disease | ||||
| Asthma | 91.0 | 62.9 | 43.8 | 19.1 |
| Diabetes | 88.9 | 50.5 | 52.8 | 20.2 |
| High poverty zip | ||||
| No | 88.5 | 54.4 | 48.7 | 19.5 |
| Yes | 92.4 | 60.6 | 47.7 | 20.0 |
| Health literacy | ||||
| Adequate | 89.7 | 56.6 | 48.8 | 18.9 |
| Less than adequate | 92.9 | 57.1 | 42.9 | 28.6 |
Fishers exact test p<0.05.
Intent to Use Recommended Online Resources
After receiving and reviewing the Online Health Resource Sheets, participants had favorable attitudes toward online health resources. Perceived ease of use ratings averaged 3.9 (out of 5) and perceived usefulness ratings averaged 3.5 (also out of 5). Neither perceived ease of use nor perceived usefulness was significantly associated with health literacy.
Most teens (62%) planned to access the provided sites “occasionally, for a specific need” and 19% planned to use them “regularly.” Six respondents (3%) said that they would “never” use any of the suggested Web resources. In bivariate analysis, intentions to use were significantly associated with greater health literacy, perceived ease of use and perceived usefulness (Table 3). After controlling for potential confounding variables, only health literacy (odds ratio [OR]=6.74; 95% confidence interval [CI]=2.06–21.97) and perceived usefulness (OR=1.85; 95% CI=1.17–2.92) remained significant. Demographic factors, condition (asthma vs. diabetes), and Internet access were not significantly associated with intent to use online health information resources in any model.
Table 3.
Correlates of Intent to Use Online Health Resources
| PARTICIPANT CHARACTERISTIC | ODDS RATIOa | ADJUSTED ODDS RATIOb |
|---|---|---|
| Health literacy | 4.84 (1.67–14.02)c | 7.16 (2.18–23.5)c |
| Perceived usefulness | 1.91 (1.34–2.72)a | 1.78 (1.12–2.83)a |
| Perceived ease of use | 1.85 (1.26–2.70)a | 1.26 (0.78–2.02) |
| Female gender | 1.31 (0.73–2.35) | 1.35 (0.73–2.51) |
| African-American | 1.39 (0.66–2.93) | 1.44 (0.61–3.37) |
| Other race | 2.25 (0.75–6.76) | 1.70 (0.51–5.66) |
| Age 13–15 | 1.18 (0.65–2.14) | 1.27 (0.65–2.50) |
| Low SES | 1.74 (0.94–3.22) | 1.80 (0.92–3.52) |
| Asthma (vs. diabetes) | 0.74 (0.41–1.34) | 0.66 (0.35–1.25) |
| Ever used Internet | 0.78 (0.30–2.12) | 0.87 (0.30–2.50) |
| Ever searched for health info | 0.93 (0.52–1.68) | 0.78 (0.40–1.51) |
Odds ratio from ordinal logistic regression model including the single characteristic.
Odds ratio from ordinal logistic regression model including all listed characteristics.
Wald chi-squared test p<0.05.
Relationship Between Intent and Self-Reported Use
One hundred twenty-nine of the 180 participants (72%) responded to the 90-day follow-up telephone interview. Respondents did not differ from nonrespondents on the basis of age, gender, race, or health literacy. Sixty percent of participants reported using at least one of the recommended sites. Intent to use was found to be significantly associated with self-reported use. Of those who had expressed the intention to use the sites “only once or twice,” 49% reported use. In comparison, those who had intended to use the sites “occasionally” had a 63% use rate, and those who stated they would use sites regularly had a 79% use rate. Of the respondents who indicated on the baseline survey that that they would not use the sites, none reported use in the follow-up survey.
Discussion
Over 90% of the teens with asthma and diabetes in our study met the criteria for adequate health literacy. Although there are no other studies of health literacy in this specific population, other studies using variations of the TOFHLA in other populations have found adequate literacy rates among English-speaking adults that have ranged from 60 to over 90%.21,40,41 We found a significant racial disparity in that black teens evidenced lower health literacy than White teens, and this difference was not explained by socioeconomic status. This finding was consistent with previous research in adults, which has found independent relationships between health literacy, race, and socioeconomic status.42,43 Given the relatively small minority population in our study, additional research will be needed to explore potential causes.
Patterns of variations in the rates of Internet use among teens with chronic illnesses were consistent with patterns found in a general population survey of adolescents. For example, the percentages of teens in our study who reported using the Internet and who reported using it daily were nearly identical to those found for teens in the 2005 Pew Internet and American Life Survey.5 Not surprisingly, the area where Internet use diverged was in the search for health-related information. We found that 48% of teens in our study searched for information about health, diet, and physical fitness compared to only 30% of teens in the national survey. We found that teens' use of the Internet to search for online health information did not differ by gender, race, zip code median income, or disease. Younger teens, however, were significantly less likely to seek such information than older teens. This finding is consistent with developmental research showing that teens do not begin to take independent responsibility for disease management until mid-adolescence (ages 15–17).44 Contrary to research in adults, our analysis did not find a significant relationship between search for online health information and health literacy. Youths with lower health literacy are seeking health information online at the same rate as those with higher literacy.
While health literacy was not associated with self-reported use of online health information, we found a highly significant relationship between health literacy and intent to use recommended sites in the near future. Significant bivariate relationships were also seen between intent to use online health information and perceived ease of use, and with perceived usefulness. In the multivariate model only health literacy and perceived usefulness remained significantly associated with intent to use. A qualitative analysis of the information from the telephone interviews conducted for this study supported the importance of perceived usefulness in the decision to try and to continue to use online health resources.45 Those who did not visit any Web sites in the follow-up period cited reasons, including lack of need, lack of time, and lack of interest while those who used Web sites and reported the intention to continue use described the Web sites they used with words including “helpful,” “useful,” and “informative.”
Interestingly, demographic and Internet use characteristics were not significant predictors of intent to use. The lack of race or income effects in our study is important because much discussion has revolved around sociodemographic barriers to Internet use, commonly referred to as the “digital divide,” and whether such barriers limit the value of Internet-based health tools in health disparity populations.46–48 We cannot generalize our findings to the larger population of teens with asthma and diabetes because the sample of teens in this study all had access to and chose to use healthcare services in a specialty care clinic; however, the absence of disparities associated with race or income in our sample suggests that Web-based patient tools may be acceptable to diverse teens receiving treatment in clinic settings, and hence these tools are unlikely to exacerbate existing health disparities in such patients.
Limitations
Teens in our study may differ from the general population due to self-selection factors. Teens, or parents of teens, who had low perceived health literacy may have opted to decline participation to avoid potential discomfort or embarrassment associated with the literacy assessment process. Such self-selection may have biased our sample toward higher literacy youths. The exclusion of a small number of potential participants due to significant English or communication deficiencies also biased the literacy of our sample upward. Additional research is needed to understand the relationship between health literacy and use of online health resources in broader populations of teens with more varied health literacy levels. Such research should also include additional measures of health literacy. While the TOFHLA is one of the most widely used and validated measures of functional health literacy, it does not directly measure all elements of health literacy (e.g., ability to obtain information or ability to understand oral communication).
Assessment of perceived ease of use and perceived usefulness of resource sheet Web sites occurred after a verbal description of the Web sites rather direct exposure to the sites. This is consistent with much of the counseling or social marketing that patients receive about online health information. Direct exposure to Web sites or previous experience with the Web sites (which was not assessed) may, however, have generated higher or lower perceptions of ease of use and usefulness. Finally, our study design did not permit the validation of self-reported use of online health resources. Reported use may reflect a degree of social desirability bias yielding an over-reporting of actual use.
This study shows that many teens with asthma and diabetes are currently using the Internet as a resource for health information and support. After receiving a verbal description of selected Web sites and an information sheet, most teens in our study reported the intent to try recommended health resource Web sites, but their anticipated commitment to become regular users of such sites depended on their health literacy and their beliefs about the usefulness of the sites. Belief that a Web site was easy to use was not a significant predicator of intent to use after controlling for health literacy and perceived usefulness. These findings suggest that just making a Web site easy to use may not generate sustained use. Instead, teens with asthma and diabetes are most likely to intend to use online health resources when they believe that the Web site will improve their health or healthcare practices and when they have the underlying skills to be effective users.
Acknowledgments
This work was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant #1R03HD053715- 01A2). Special thanks to Dr. Kelly J. Kelleher for his thoughtful comments.
Disclosure Statement
No competing financial interests exist.
References
- 1.Gentles S. Lokker C. McKibbon K. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: A scoping review. J Med Internet Res. 2010;12:2. doi: 10.2196/jmir.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neil A, et al. Predictors of adherence by adolescents to a cognitive behavior therapy Website in school and community-based settings. J Med Internet Res. 2009;11:e6. doi: 10.2196/jmir.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nordfeldt S. Hanberger L. Bertero C. Patient and parent views on a Web 2.0 diabetes portal—the management tool, the generator, and the gatekeeper: Qualitative study. J Med Internet Res. 2010;12:e17. doi: 10.2196/jmir.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moreno M. Ralston J. Grossman D. Adolescent access to online health services: Perils and promise. J Adolesc Health. 2009;44:244–251. doi: 10.1016/j.jadohealth.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 5.Lenhart A. Madden M. Hiltin P. Teens and technology: Youth are leading the transition to a fully wired and mobile nation. Washington, DC: Pew Internet and American Life Project; 2005. [Google Scholar]
- 6.Bansil P, et al. Health-related information on the Web: Results from the Healthstyles survey, 2002–2003. Preventing chronic disease 2006. www.cdc.gov/pcd/issues/2006/apr/05_0155.htm. www.webcitation.org/5upTG4rFk. [Feb 14;2011 ]. www.cdc.gov/pcd/issues/2006/apr/05_0155.htmwww.webcitation.org/5upTG4rFk [PMC free article] [PubMed]
- 7.Bundorf M, et al. Who searches for Internet health information? Health Serv Res. 2006;41(Part I):819–835. doi: 10.1111/j.1475-6773.2006.00510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chau P. Hu P. Investigating healthcare professionals' decisions to accept telemedicine technology: An empirical test of competing theories. Inf Manage. 2002;39:297–311. [Google Scholar]
- 9.Chismar W. Wiley-Patton S. Does the extended technology acceptance model apply to physicians?. Proceedings of the 36th Hawaii International Conference on System Sciences (HICSS '03), Hawaii; Washington, DC. IEEE Computer Society; 2003. p. 160a. [Google Scholar]
- 10.Chisolm DJ, et al. Adolescent satisfaction with computer-assisted risk screening in primary care. Child Adolesc Ment Health. 2008;13:163–168. doi: 10.1111/j.1475-3588.2007.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holden RJ. Karsh B. The technology acceptance model: Its past and its future in health care. J Biomed Inform. 2010;43:159–172. doi: 10.1016/j.jbi.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorence D. Park H. Group disparities and health information: A study of online access for the underserved. Health Inform J. 2008;14:29–38. doi: 10.1177/1460458207086332. [DOI] [PubMed] [Google Scholar]
- 13.Wilson E. Lankton N. Modeling patient's acceptance of provider delivered e-health. J Am Med Inform Assoc. 2004;11:241–248. doi: 10.1197/jamia.M1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chisolm DJ. Does online health information seeking act like a health behavior: A test of the behavioral model. Telemed J E Health. 2010;16:154–160. doi: 10.1089/tmj.2009.0102. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 16.Ratzan S. Parker RM. Introduction, in national library of medicine current bibliographies in medicine: Health literacy. In: Seldon C, et al., editors. National Library of Medicine current biographies in medicine: Health literacy. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services; 2000. p. v. [Google Scholar]
- 17.Gazmararian JA, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 18.Howard D. Gazmararian JA. Parker RM. The impact of low health literacy in the medical costs of medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Kutner M, et al. The health literacy of adults: Results from the 2003 National Assesment of Adult Literacy, U.S.D.O. Education, Editor. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- 20.Rothman R, et al. The influence of patient literacy on the effectiveness of a primary-care based diabetes disease management intervention. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 21.Schillinger D, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 22.Scott TL, et al. Health literacy and preventive health care use among medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Rothman R, et al. The relationship between literacy and glycemic control in a diabetes disease management program. Diabetes Educator. 2004;30:263–273. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 24.Birru M, et al. Internet usage by low literacy adults seeking health information: An observational analysis. J Med Internet Res. 2004;6:e25. doi: 10.2196/jmir.6.3.e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. National Diabetes Fact Sheet. 2007. www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf. www.webcitation.org/5vsuTKQ8t. [Feb 14;2011 ]. www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdfwww.webcitation.org/5vsuTKQ8t
- 26.Centers for Disease Control and Prevention. Child asthma data: Prevalence tables. 2008. www.cdc.gov/asthma/brfss/08/child/current/tableC3.htm. www.webcitation.org/5vsvF2eQX. [Feb 14;2011 ]. www.cdc.gov/asthma/brfss/08/child/current/tableC3.htmwww.webcitation.org/5vsvF2eQX
- 27.Danne T. Becker D. Paediatric diabetes: Acheiving practical,effective insulin therapy in type 1 and type 2 diabetes. Acta Paediatrica. 2007;96:1560–1570. doi: 10.1111/j.1651-2227.2007.00494.x. [DOI] [PubMed] [Google Scholar]
- 28.de Benedictis D. Bush A. The challenge of asthma in adolescence. Pediatr Pulmonol. 2007;42:683–692. doi: 10.1002/ppul.20650. [DOI] [PubMed] [Google Scholar]
- 29.U.S. National Library of Medicine and National Institutes of Health. Medline Plus: Diabetes. 2011. www.nlm.nih.gov/medlineplus/diabetes.html. www.webcitation.org/5vsuDv6TV. [Feb 14;2011 ]. www.nlm.nih.gov/medlineplus/diabetes.htmlwww.webcitation.org/5vsuDv6TV
- 30.U.S. National Library of Medicine and National Institutes of Health. Medline Plus: Asthma in children. 2011. www.nlm.nih.gov/medlineplus/asthmainchildren.html. www.webcitation.org/5vsxEMNcz. [Feb 14;2011 ]. www.nlm.nih.gov/medlineplus/asthmainchildren.htmlwww.webcitation.org/5vsxEMNcz
- 31.Baker DW, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 32.Nurss J, et al. TOFHLA: Test of functional health literacy in adults. Snow Camp, NC: Peppercorn Books & Press; 1995. [Google Scholar]
- 33.Parker RM, et al. The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 34.Hironaka L, et al. Caregiver health literacy and adherence to a daily multi-vitamin with iron regimen in infants. Patient Educ Couns. 2009;75:376–380. doi: 10.1016/j.pec.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Sox C, et al. Patient-centered design of an informtion managment module for a personally controlled health record. J Med Internet Res. 2010;12:e36. doi: 10.2196/jmir.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yin H, et al. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7:292–298. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Health on the Net. HON Code of Conduct (HONcode) for Medical and Health Websites. 1997. www.hon.ch/HONcode/conduct.html. www.webcitation.org/5upTf8WNq. [Feb 14;2011 ]. www.hon.ch/HONcode/conduct.htmlwww.webcitation.org/5upTf8WNq
- 38.Davis F. User acceptance of information technology: System characteristics, user perceptions and behavioral impacts. Int J Man-Machine Stud. 1993;38:475–487. [Google Scholar]
- 39.Venkatesh V, et al. User acceptance of information technology: Toward a unified view. MIS Quarterly. 2003;27:425–478. [Google Scholar]
- 40.Gazmararian JA. Parker RM. Baker DW. Reading skills and family planning knowledge and practices in a low-income managed-care population. JAMA. 1999;281:545–551. doi: 10.1016/s0029-7844(98)00431-1. [DOI] [PubMed] [Google Scholar]
- 41.Kalichman SC, et al. Health literacy and health-related knowledge among persons living with HIV/AIDS. Am J Prev Med. 2000;18:325–331. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- 42.Arnold C, et al. Smoking status, reading level, and knowledge of tobacco effects among low income pregnant women. Prev Med. 2001;32:313–320. doi: 10.1006/pmed.2000.0815. [DOI] [PubMed] [Google Scholar]
- 43.Gazmararian J, et al. Health literacy among medicare enrollees in a managed care organization. JAMA. 1999;281:545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 44.Schilling L. Knafl K. Grey M. Changing patterns of self-management in youth with type I diabetes. J Pediatr Nurs. 2006;21:412–424. doi: 10.1016/j.pedn.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 45.Chisolm DJ. Johnson LD. McAlearney AS. What makes teens start using and keep using health information Websites: A mixed model analysis of teens with chronic illnesses. Telemed E Health. 2011;17:324–328. doi: 10.1089/tmj.2010.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brodie M, et al. Health information, the Internet, and the digital divide. Health Aff. 2000;19:255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 47.Hsu J, et al. Use of e-Health services between 1999 and 2002: A growing digital divide. J Am Med Inform Assoc. 2005;12:164–171. doi: 10.1197/jamia.M1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Watson A, et al. Reevaluating the digital divide: Current lack of Internet use is not a barriers to adoption of novel health information technology. Diabetes Care. 2008;31:433–435. doi: 10.2337/dc07-1667. [DOI] [PubMed] [Google Scholar]