Abstract
Objectives
Musculoskeletal pain is associated with occupational physical activities and psychosocial risk factors. We evaluated the relative importance of work-related and psychological determinants of the number of anatomical sites affected by musculoskeletal pain in a cross-sectional survey.
Methods
The survey focused on musculoskeletal pain in six body regions (low-back, neck, shoulder, elbow, wrist/hand and knee) among 224 nurses, 200 office workers and 140 postal clerks in Crete (response rate 95%). Information was collected about demographic characteristics, occupational physical load, psychosocial aspects of work, perceptions about causes of pain, mental health, tendency to somatize, and experience of pain in the past 12 months. Poisson regression was used to assess associations of risk factors with the number of painful anatomical sites and interactions were explored using classification and regression trees (CART).
Results
Two-thirds of the study sample reported pain in at least two body sites during the past 12 months, and in 23%, more than three sites were affected. The number of painful anatomical sites was strongly related to both physical load at work and somatizing tendency (with relative risks increased five-fold or more for frequent and disabling multisite pain) , and was also significantly associated with work-related psychosocial factors, and beliefs about work causation. The CART analysis suggested that in the population studied, the leading determinant of the number of painful body sites was somatizing tendency.
Conclusions
In the population studied, pain at multiple anatomical sites is common, and is strongly associated with somatizing tendency, which may have a more important influence on multi-site pain than on pain that is limited to a single anatomical site.
Keywords: epidemiology, occupational health
Introduction
Musculoskeletal pain is a leading cause of disability among people of working age in Europe, with substantial social and economic impact (1). Much effort has gone into investigating its causes and prevention, but several aspects of the problem still require clarification.
A number of critical literarure reviews have provided evidence that psychosocial workplace factors correlate with occupational musculoskeletal disorders (2-4), and a number of studies also suggest that individual psychological factors relate to consultation for and disability from musculoskeletal disorders (5-8). One important area of uncertainty is the extent to which psychological factors influence musculoskeletal illness and associated disability. Marked variations have been reported between workers doing similar jobs in dissimilar settings (9, 10). And in two large community-based surveys, with subjects drawn from many different countries, striking differences were reported in the prevalence of chronic back pain and chronic persistent regional pain – too large to be explained simply by differences in occupational physical workload (11, 12).
Such observations suggest that mechanical overload is perhaps not the leading cause of regional musculoskeletal pain. Prevention may require multifaceted interventions aimed at addressing other factors, such as health beliefs, coping styles and mental ill health, as well as reducing the effort of work (13). In planning interventions, it would be helpful to establish with greater certainty the relative importance of occupational and non-occupational risk factors in the causation of common musculoskeletal symptoms and associated disability. Moreover, this research should cover non-occupational risk factors such as somatizing tendency, which have been less commonly studied in the workplace, but which associate strongly with musculoskeletal disability in the community (5, 6).
A further question is whether the relative importance of risk factors differs for pain occurring at multiple sites. In the general population, widespread pain is common (14), its extent varying across a biological continuum (15, 16). It has substantial impact on physical fitness, general health status and well-being, activities of daily living, and psychological distress (15, 17-20); and, among workers, it may predict future risk of long-term sickness absence (21, 22). But in most occupational investigations, musculoskeletal pain has been studied only at specific anatomical sites (23-25), assuming a model in which local physical stressors generate local mechanical problems. Widespread pain has been studied less often, usually as a confounder (26, 27) or prognostic indicator(28) , and rarely as a primary health outcome (29). Evidence from studies in the general population suggests that non-occupational risk factors, such as low mood and health anxiety, associate prominently with generalized pain (14, 30, 31), but relatively little is known about the determinants of widespread pain in the workplace (32). Furthermore, although widespread pain occurs in a continuum of severity, most epidemiological studies, including those carried out in occupational settings, have applied a pre-specified dichotomous case definition. It may be more informative to assess risks according to the number of regional sites with pain.
In this study we (i) assessed the prevalence of regional musculoskeletal pain in three occupational groups from Greece (a country which, according to one WHO study, lies in the lowest quintile for primary care attendance for musculoskeletal pain (12); (ii) determined the frequency of individual and work-related risk factors for pain at multiple anatomical sites; and (iii) undertook a novel analysis aimed at assessing the relative importance of occupational and non-occupational risk factors in determining the number of regional anatomical sites that are reported as painful. Data were collected as part of an international multi-centre collaborative investigation, designed to explore CUltural and Psychosocial Influences on musculoskeletal symptoms and Disability (the CUPID study).
Methods
Population and questionnaires
We conducted a cross-sectional survey in Crete, Greece during June to December 2006. The study sample comprised a random subset of nurses (N=240) from the staff of Heraklion University Hospital, all office workers (N=202) employed at Heraklion University who were registered as computer users, and all postal clerks (N=154) from the central postal offices of the four prefectures of Crete. To be included, subjects had to be aged 21-60 years, and to have worked for at least one year in their current job. The study protocol was approved by the Scientific Board Committee of the University Hospital of Heraklion. Written informed consent was obtained from all participants.
We evaluated an integrated multifactorial model for musculoskeletal pain incorporating both work-related and psychological determinants. Information was collected from participants through a personal interview at their place of work, using a structured questionnaire.that covered demographic characteristics, physical and psychosocial risk factors at work, mental health (low mood), tendency to somatize, alexithymia, depression, health beliefs, musculoskeletal pain lasting for longer than one day in the past 12 months, and associated difficulty in carrying out everyday activities.
The occupational risk factors that we studied concerned the physical demands of work, the number of hours worked per week, and the perceived psychosocial work environment.
Physical demand was classified using a score between 0 and 5, with a one unit increase for each body site that was reported as being strained during a typical day at work (for this purpose the neck and shoulder were treated as a single site). Body sites were regarded as being strained if positive answers were elicited to questions as follows: low back – “lifting more than 25kg by hand”; neck/shoulder – “working with the hands above shoulder height for at least one hour in total”; elbow – “repeated bending and straightening of the elbow for at least one hour in total”; wrist/hand – either “typing for more than 4 hours in total” or “ doing other repeated movements of the wrist or hands for more than 4 hours in total”; and knee – either “ kneeling or squatting for more than one hour in total” or “ climbing more than 30 flights of stairs in total”.
Questions on job support, control and demand were based on the Karasek model (33) – with job control classed as ‘high’ if the respondent had discretion over what work was done, how, and according to what timetable, and job demands classed as ‘low’ in the absence of any of piecework, targets and time pressure. Questions were also asked about job satisfaction, job security, and support from colleagues and/or supervisor.
Mental health was assessed using questions derived from the mental health section of the SF-36 questionnaire (34), and tendency to somatize using elements of the somatic subscale of the Brief Symptom Inventory (BSI) (35), which is a measure of distress and psychopathology, comprising items on bothersome nausea, faintness, dizziness, weakness, numbness, chest pain and breathing difficulties in the past 7 days.. For the former, scores for individual questions were summed, and the totals were classified to thirds of their distribution in the study sample. Somatizing tendency was classified according to the number of somatic symptoms (out of a total of seven) that were rated as at least moderately distressing (5). Data on alexithymia (difficulty understanding and expressing one’s own feelings and those of others) were obtained using the 20-item Toronto Alexithymia Scale (TAS-20) (36), and depression was assessed by the Beck Depression Inventory (BDI-II) (37). For each of these two scales we employed standardized cut-off points for the Greek population (38, 39) (Anagnostopoulou and Kiosseoglou [unpublished manuscript] The greek validation of the TAS-20).
The health beliefs that we explored related to the work-relatedness of back and upper limb pain, and what a person should do if symptomatic. Belief in work as a cause of pain was considered strong if the participant completely agreed that pain, both in the low back and in the upper limb, was most commonly caused by work, weak when the perception was limited to only one of these anatomical sites, and otherwise was deemed absent. Questions about actions in response to symptoms were modified from the Fear-avoidance Beliefs Questionnaire (40), and answers were counted as positive if the participant completely agreed that one should avoid physical activity when in pain, and that rest was needed for recovery.
The questions on musculoskeletal symptoms were adapted from the Nordic questionnaire on musculoskeletal complaints (41), and related to six anatomical sites: low back, neck, shoulder, elbow, wrist/hand and knee.
Apart from the questions on alexithymia and depression, the questionnaire was a Greek version of that used in the international CUPID study (9). Originally formulated in English, this was translated into Greek, back translated to English, and administered in both languages to 5 volunteers. Anomalies that were identified were resolved by consensus between researchers in Crete (ES, LC, MK), the coordinator of the international study (DC) and the professional translator, and the wording was revised appropriately. A complete report of the translation protocol is available (42).
Statistical analysis
The main outcome measures were: (i) the total number of body sites that were painful for at least one day in the past 12 months, (ii) the number of sites that were frequently painful in the past 12 months, and (iii) the number of sites at which pain was disabling in the past month. ‘Frequent’ pain was defined as pain that had lasted for at least 30 days in total in the past 12 months. Pain was counted as ‘disabling’ when it had made it difficult or impossible to carry out at least two everyday activities in the past month from a pre-specified list (e.g. household chores, getting dressed). The questions about restriction of activities were limited to a more recent time period (one month rather than one year) to achieve more reliable recall (43).
Poisson regression (44, 45) was used to model relations between individual, physical and psychosocial factors and the three count outcomes (number of sites in pain, in frequent pain and in disabling pain). Each potential risk factor was examined one at a time, after adjusting for age, sex and main occupation. Risk factors that were significantly associated with the outcomes under study in this analysis were subsequently introduced simultaneously in a multivariable model together with age, sex and main occupation. Statistical significance was set to p<0.05. We applied Poisson regression after having set equal follow-up time for all subjects, and derived incidence rate ratios (IRR) per one year or 1 month incidence rates. This approach avoids problems of convergence on models examining prevalence. The percentage of change in the expected outcome count (or number of sites in pain) for the exposed category compared to the non-exposed was calculated as 100*(IRR-1). We used the statistical package STATA/SE 10 for the analysis.
Interactions between potential determinants of the number of painful anatomical sites were assessed using classification and regression trees (CART), implemented in the R statistical software (http://www.r-project.org/). CART , known as binary recursive splitting, uses non-parametric methods. It produces trees that represent a model in which every node is determined by splitting the data set on the basis of the variable that provides the best separation. At every succeeding branch, all variables are tested again for their usefulness in further splitting. The relative importance of each variable in the final tree is assessed based on its importance over all nodes and splits (46, 47). Its advantage over logistic regression is its ability to identify subgroups of individuals with different characteristics that are at high risk. All the potential determinants of pain that were examined in the Poisson regression analysis were included also in the CART models, and the number of painful sites in pain was introduced as a discrete outcome variable with levels from 0 to 6. Cross-validation was used to reduce over-fitted trees to their optimal size by randomly splitting the data into 10 equal parts and subsequently using a learning set (part of the data) to construct the tree model and a testing set to validate the model. This cross-validation process was repeated 10 times and was used to estimate the classification error and the cost-complexity parameter that determined the reduction of the trees to their optimal size (46, 47).
Results
A total of 564 workers (224 nurses, 140 postal clerks and 200 office workers) took part in the study with an overall response rate of 95%. Nurses and office workers were mostly women (88% and 75% respectively), while postal workers were predominantly men (84%). Postal workers (mean age 46 years) were older on average than nurses (37 years) and office workers (40 years).
Table 1 sets out the 12-month and 1-month prevalence of pain at different anatomical sites among the participants. Regional musculoskeletal pain, and especially low back and neck pain, were common in both sexes. Neck, shoulder, and wrist/hand pain were more prevalent in women than in men.
Table 1.
Twelve month and one month prevalence for the six localizations of pain by sex
| Past 12 months | Past month | |||
|---|---|---|---|---|
|
|
||||
| Pain site | Men | Women | Men | Women |
| Low back | 121(62%) | 233(63%) | 72(37%) | 149(40%) |
| Neck | 79(41%) | 191(52%) | 46(24%) | 139(38%) |
| Shoulder | 63(33%) | 146(40%) | 39(20%) | 100(27%) |
| Elbow | 39(20%) | 73(20%) | 23(12%) | 42(11%) |
| Wrist/hand | 47(24%) | 165(45%) | 30(16%) | 97(26%) |
| Knee | 48(25%) | 96(26%) | 37(19%) | 66(18%) |
Table 2 shows the frequency with which different numbers of body sites were reported as being painful. Multi-site pain (>3 sites affected) in the past 12 months was reported by some 23% of the study sample, but frequent pain in the past 12 months and disabling pain in the past month were less commonly multi-site (4-5% of participants).
Table 2.
Number of body sites in pain (and percentages) in the past 12 months, in frequent pain in the past 12 months and in disabling pain in the past month
| Number of body sites in pain |
Pain in the past 12 months |
Frequent pain in the past 12 months |
Disabling pain in the past month |
|---|---|---|---|
| 0 | 75 (13%) | 347 (62%) | 331 (59%) |
| 1 | 113 (20%) | 124 (22%) | 113 (20%) |
| 2 | 136 (24%) | 52 (9%) | 63 (12%) |
| 3 | 108 (19%) | 23 (4%) | 23 (4%) |
| 4 | 85 (15%) | 9 (2%) | 19 (3%) |
| 5 | 30 (5%) | 3 (1%) | 7 (1%) |
| 6 | 17 (3%) | 3 (1%) | 3 (1%) |
Table 3 presents the distribution of the independent variables in the study sample and their association with the outcomes under study. All incidence rate ratios (IRR) were adjusted for age, sex and main occupation. Women reported a higher number of body sites in pain for all three outcomes. Further analysis, however, suggested that this difference could be attributed to the difference in somatization scores between men and women (information not shown). Number of pain sites tended to increase with age. After allowing for these factors, increasing physical load showed a strong linear association with the number of pain sites affected, especially for frequent or disabling pain (IRRs 8.4 and 25.8 respectively), and so did somatizing tendency (IRRs raised about 5-fold for the same outcomes). Other risk factors which showed weaker but statistically significant associations with each outcome included were high job satisfaction and high job support (moderately protective); and strong beliefs in work as a cause of pain (positive relationship). Belonging in the grey zone for alexithymia (intermediate scores) seemed to have a moderately protective effect against multisite and frequent multisite pain in the past 12 months; no relation was found to depression (BDI-II) although a positive monotonic relationship was found with mental health score.
Table 3.
Association (Incidence Rate Ratio- IRR) of determinants of pain with number of sites in pain in the past 12 months, frequent pain in the past 12 months and disabling pain the last month. All IRRs are adjusted for age, sex and occupation.
| Characteristic | N* | Sites in pain in the past 12 months |
Sites in frequent pain in the past 12 months |
Sites in disabling pain in the past month |
||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |||
| Sex | ||||||||
| Men | 194 | 1.0 | 1.0 | 1.0 | ||||
| Women | 370 | 1.3 | 1.1-1.5 | 1.9 | 1.4-2.5 | 2.4 | 1.8-3.2 | |
| Occupation | ||||||||
| Nurse | 224 | 1.0 | 1.0 | 1.0 | ||||
| Postal Clerk | 140 | 1.1 | 0.9-1.3 | 1.5 | 1.0-2.0 | 1.4 | 1.0-1.9 | |
| Office Worker | 200 | 1.0 | 0.9-1.1 | 0.9 | 0.7-1.2 | 0.7 | 0.6-0.9 | |
| Age groups | ||||||||
| 20-29 | 29 | 1.0 | 1.0 | 1.0 | ||||
| 30-39 | 257 | 1.4 | 1.1-1.9 | 4.9 | 1.6-15.4 | 1.6 | 0.9-2.7 | |
| 40-49 | 206 | 1.6 | 1.2-2.2 | 8.9 | 2.8-27.8 | 2.3 | 1.3-4.1 | |
| 50-59 | 69 | 1.4 | 1.0-2.0 | 8.5 | 2.6-27.5 | 2.0 | 1.1-3.8 | |
|
Hours per week at
work | ||||||||
| ≤39 | 139 | 1.0 | 1.0 | 1.0 | ||||
| ≥40 | 423 | 1.1 | 0.9-1.3 | 1.1 | 0.9-1.5 | 1.4 | 1.1-1.8 | |
| Physical load score | ||||||||
| 0 | 17 | 1.0 | 1.0 | 1.0 | ||||
| 1 | 71 | 2.5 | 1.4-4.6 | 4.0 | 1.0-17.0 | 8.8 | 1.2-64.9 | |
| 2 | 169 | 3.4 | 1.9-6.1 | 6.1 | 1.5-24.9 | 16.4 | 2.3-118.1 | |
| 3 | 151 | 3.4 | 1.9-6.0 | 5.3 | 1.3-21.5 | 14.5 | 2.0-104.1 | |
| 4 | 111 | 3.9 | 2.2-7.0 | 8.9 | 2.2-36.2 | 19.5 | 2.7-140.0 | |
| 5 | 45 | 4.7 | 2.6-8.4 | 8.4 | 2.0-34.7 | 25.8 | 3.6-186.5 | |
|
Psychosocial factors at
work | ||||||||
| Job satisfaction | low | 114 | 1.0 | 1.0 | 1.0 | |||
| high | 448 | 0.7 | 0.6-0.8 | 0.6 | 0.5-0.8 | 0.5 | 0.4-0.6 | |
| Job demand | low | 107 | 1.0 | 1.0 | 1.0 | |||
| high | 455 | 1.1 | 0.9-1.3 | 1.6 | 1.1-2.2 | 1.0 | 0.8-1.3 | |
| Job control | low | 331 | 1.0 | 1.0 | 1.0 | |||
| high | 233 | 1.0 | 0.9-1.1 | 0.9 | 0.7-1.1 | 0.8 | 0.7-1.1 | |
| Job support | low | 101 | 1.0 | 1.0 | 1.0 | |||
| high | 455 | 0.9 | 0.8-1.0 | 0.7 | 0.5-0.8 | 0.7 | 0.6-0.9 | |
| Job security | low | 114 | 1.0 | 1.0 | 1.0 | |||
| high | 1.0 | 0.9-1.1 | 0.7-1.2 | 448 | 0.9 | 0.9 | 0.7-1.1 | |
|
Mental Health Score
(tertiles) |
Best | 183 | 1.0 | 1.0 | 1.0 | |||
| Middle | 201 | 1.2 | 1.0-1.4 | 1.3 | 0.9-1.7 | 1.4 | 1.1-1.9 | |
| Worst | 180 | 1.5 | 1.3-1.7 | 1.7 | 1.3-2.3 | 2.1 | 1.6-2.7 | |
| Somatizing symptoms | ||||||||
| 0 | 261 | 1.0 | 1.0 | 1.0 | ||||
| 1 | 84 | 1.3 | 1.1-1.6 | 2.7 | 1.9-3.8 | 2.1 | 1.5-3.1 | |
| 2+ | 218 | 2.0 | 1.8-2.3 | 4.8 | 3.6-6.4 | 5.5 | 4.2-7.2 | |
| Alexithymia | ||||||||
| Non alexithymic | 400 | 1.0 | 1.0 | 1.0 | ||||
| Grey zone | 76 | 0.9 | 0.7-1.0 | 0.6 | 0.4-0.9 | 0.9 | 0.6-1.2 | |
| Alexithymic | 54 | 1.1 | 0.9-1.3 | 1.1 | 0.8-1.5 | 1.0 | 0.7-1.4 | |
| Depression | ||||||||
| Normal | 368 | 1.0 | 1.0 | 1.0 | ||||
| Mild | 101 | 1.0 | 0.9-1.1 | 0.8 | 0.6-1.1 | 0.9 | 0.7-1.2 | |
| Moderate/Severe | 67 | 1.0 | 0.9-1.2 | 0.9 | 0.7-1.3 | 1.0 | 0.7-1.4 | |
| Fear avoidance beliefs | ||||||||
| No | 272 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 292 | 1.0 | 0.9-1.2 | 1.0 | 0.8-1.3 | 1.3 | 1.1-1.6 | |
| Work causation beliefs | ||||||||
| No | 168 | 1.0 | 1.0 | 1.0 | ||||
| Weak | 88 | 1.1 | 0.9-1.3 | 1.6 | 1.1-2.3 | 1.1 | 0.8-1.5 | |
| Strong | 308 | 1.3 | 1.1-1.5 | 1.7 | 1.3-2.2 | 1.5 | 1.2-2.0 | |
Responses may not all add up to 564 due to a few missing answers.
Risk factors that were significantly associated with the outcomes under study when examined one at a time, were subsequently introduced simultaneously in a multivariable model together with age, sex and main occupation (Table 4). The corresponding IRRs that were statistically significant are presented in Table 4, except for age, sex and occupation that were included in all models. Somatizing tendency was statistically significant in all three models and was very strongly associated with disabling pain and frequent pain. Increasing physical load at work was also significantly associated with the three outcomes. Being in the grey zone for alexithymia reduced significantly the number of occurrences of any pain and of frequent pain in the past 12 months, thus implying a U-shaped curve type of association. Job satisfaction and job support were both present as protective factors for disabling pain in the past month, whereas strong beliefs about work as a cause of musculoskeletal pain were positively associated with any pain and frequent pain in the past 12 months.
Table 4.
Multivariable model (Incidence Rate Ratio- IRR) for the determinants of the number of sites in pain in the past 12 months, in frequent pain in the past 12 months and in disabling pain in the past month. All IRRs are mutually adjusted and also adjusted for age, sex and occupation.
| Pain in the past 12 months |
Frequent pain in the past 12 months |
Disabling pain in the past month |
||
|---|---|---|---|---|
|
| ||||
| IRR (95%CI) | IRR (95%CI) | IRR (95%CI) | ||
| Somatisation symptoms | ||||
| 0 symptoms | 1.0 | 1.0 | 1.0 | |
| 1 symptom | 1.2 (1.0-1.4) | 2.3 (1.6-3.4) | 1.8 (1.2-2.7) | |
| 2+ symptoms | 1.7 (1.5-2.0) | 4.5 (3.3-6.3) | 4.3 (3.2-5.8) | |
| TAS-20 score | ||||
| Normal | 1.0 | 1.0 | . | |
| Grey zone | 0.8 (0.7-1.0) | 0.6 (0.4-0.9) | ||
| Alexithymia | 1.1 (0.9-1.3) | 1.0 (0.7-1.3) | ||
| Job satisfaction | ||||
| Low | 1.0 | . | 1.0 | |
| High | 0.9 (0.8-1.0) | 0.7 (0.6-0.9) | ||
| Job support | ||||
| Low | . | . | 1.0 | |
| High | 0.8 (0.6-1.0) | |||
| Physical load score | ||||
| 0 | 1.0 | 1.0 * | 1.0 | |
| 1 | 1.7 (0.9-3.1) | 2.1 (0.5-9.1) | 4.8 (0.6-35.7) | |
| 2 | 2.1 (1.1-3.7) | 2.0 (0.5-8.4) | 5.7 (0.8-41.1) | |
| 3 | 2.0 (1.1-3.5) | 1.9 (0.5-7.9) | 5.4 (0.7-39.3) | |
| 4 | 2.3 (1.3-4.1) | 3.0 (0.7-12.5) | 6.0 (0.8-44.0) | |
| 5 | 2.5 (1.3-4.5) | 2.6 (0.6-11.2) | 8.0 (1.1-58.3) | |
| Work causation beliefs | ||||
| Weak | 1.0 | 1.0 | . | |
| Moderate | 1.1 (0.9-1.3) | 1.4 (0.9-2.1) | ||
| Strong | 1.2 (1.0-1.4) | 1.4 (1.0-1.9) | ||
p-value for trend= 0.05
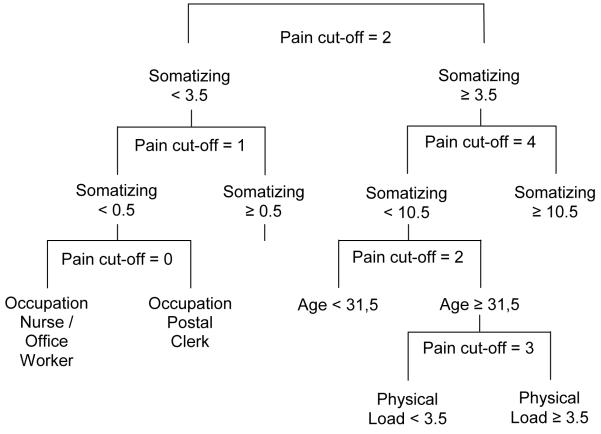
Figure 1 shows the classification and regression tree (CART) model for determinants of pain at multiple sites. Number of painful anatomical sites in the last 12 months was entered as a discrete variable with levels from 0 to 6. The analysis indicated an optimal tree with six splits and 7 terminal nodes, in which somatizing tendency was the main variable differentiating pathways that led to few or multiple sites of pain. For each split, the figure shows the risk factor (and its level) that discriminated between the two subsets of workers distinguished by the split, and a cut-point in the number of sites of pain that characterized the distinction between the two subsets. The optimal tree had a relatively low sensitivity of 14% on the test sets indicating that while this analysis identifies discrete causal pathways, they explain only part of the variation in the population. Not surprisingly (on the basis of results from the multivariate analysis), the first split was based on somatizing tendency. Occupation seemed to be an important discriminant between subjects with no or only one painful site (left pathway in the Figure). Subjects with high somatizing scores were further split according to age and level of somatizing score, distinguishing groups of subjects with pain at different numbers of multiple sites. Somatizing appeared as the main determinant in subjects with the highest number of multiple pains (right pathway in the Figure), while a complex grouping of risk factors including psychological and physical load could be discerned for subjects with intermediate levels of somatizing scores and number of multiple pains. The interaction between physical load and somatizing tendency was not statistically significant (likelihood ratio test, p-value for interaction=0.21).
Figure 1.
Classification Tree for number of sites in pain during the past 12 months. For each split, the figure shows the risk factor (and its level) that discriminated between the two subsets of workers distinguished by the split, and a cut-point in the number of sites of pain that characterized the distinction between the two subsets.
Discussion
Regional musculoskeletal pain was common in all three of the Greek occupational groups studied, as was pain at multiple sites. Two-thirds of the study sample reported pain in at least two body sites in the past 12 months, and in 23%, more than three sites were affected. The number of painful anatomical sites was strongly related to both physical load at work and somatizing tendency, and was also significantly associated with work-related psychosocial factors, and beliefs about work causation. The CART analysis suggested that in the population studied, the leading determinant of the number of painful body sites was somatizing tendency.
Our study had several methodological strengths. The study sample targeted was representative of the occupational groups investigated, in that the nurses were a random sample of nursing personnel of the University Hospital of Heraklion, while all postal clerks in Crete and all university office workers at Heraklion were invited to take part, provided they met the inclusion criteria of age and duration of employment. Moreover a high response rate was achieved from eligible subjects. The BSI, on which we based our assessment of somatizing tendency, has predictive validity for incident and persistent regional pain (5, 6, 35) and correlates with disability attributed to multi-site pain (48); the SF-36 is a well recognized and widely used standard instrument (34); we adapted the Fear Avoidance Belief Questionnaire designed originally to assess back pain; and the Toronto Alexithymia Scale and BDI-II have both been used extensively, and have been validated for application in the Greek population (38, 39) .
Our findings should, however, be considered in the context of several limitations of study design. Data collection was based on interviewer-administered questionnaires, and as in many other studies, no clinical measures of pain or disability were used. Reliance was placed on the ability and willingness of respondents to recall symptoms over a period of up to 12 months, although, reassuringly, similar associations were found for disabling pain in the past month, which should have been recalled more accurately.
In addition, the cross-sectional design of the study leaves open questions about the direction of causation for some of the associations demonstrated. For example, job satisfaction, perception of support in the workplace, and beliefs about work as a cause of musculoskeletal complaints might all be modified by the occurrence of regional pain. The presence of musculoskeletal symptoms could make a worker more aware of the physical demands of his or her job, and therefore more likely to report such activities. However, it seems less likely that the occurrence of musculoskeletal pain would increase people’s propensity to report other somatic symptoms such as “nausea or upset stomach”, “trouble getting your breath” and “hot or cold spells”. Thus, the associations that were found with somatizing tendency are unlikely to be distorted by reverse causation. In support of this, in longitudinal studies, somatizing tendency and other psychological factors have been found to predict the future incidence and persistence of musculoskeletal pain (49)(5, 50).
When these potential sources of bias are taken into account, it seems reasonable to conclude that somatizing tendency is a major determinant of multi-site regional pain. The exact contribution of stressful physical activities and psychosocial aspects of work is more difficult to gauge, but is probably smaller. It is important to note that classification of a subject as having multi-site pain in our study did not necessarily imply that pain occurred at several sites simultaneously, only that several anatomical sites were affected by pain at some time during the relevant time period (past year or past month).
One novel aspect of our analysis was the use of the Classification Trees (CART) technique to identify subgroups of subjects with importantly differing risks, defined by combinations of risk factors. The findings from this analysis supported the view that within our study population, somatizing tendency was a major determinant of multi-site pain. However, it is of interest that within the subset of participants who were likely to have pain at fewer than two sites, discrimination between those with and without pain appeared to depend more on their occupation. It is possible that isolated pain at a single anatomical site is often a consequence of locally stressful physical activity, whereas somatizing tendency tends to generate report of pain at multiple sites. This could be tested further in other data sets.
In conclusion, this study suggests that symptom rates are high in the three Greek occupational groups studied. Moreover, pain at multiple anatomical sites is common, more so than single-site pain. Our findings also indicate that somatizing tendency plays a particularly important role in multi-site pain, with the possibility that the relative importance of psychological as compared with physical risk factors is different for widespread as compared with localized pain. Future studies should explore the distinction between risk factors for musculoskeletal pain at multiple anatomical sites as compared with pain at only a single site.
Acknowledgments
The study in Crete was partly supported by a research grant from the Colt Foundation (a registered charity). We thank Katerina Fanouraki for assisting in the interviews.
References
- 1.Smith A, Jones A. News release: Work-related musculoskeletal disorders are fast becoming the greatest health and safety challenge for Europe. European Agency for Safety and Health at Work. 2000 [Google Scholar]
- 2.Bernard B. Musculoskeletal Disorders and Workplace Factors. A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity and Low Back. U.S. Department of Health and Human Services; Cincinnati: 1997. NIOSH Publication No. 97-141. [Google Scholar]
- 3.Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25(16):2114–25. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- 4.Bongers PM, Kremer AM, ter Laak J. Are psychosocial factors, risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist? A review of the epidemiological literature. Am J Ind Med. 2002;41(5):315–42. doi: 10.1002/ajim.10050. [DOI] [PubMed] [Google Scholar]
- 5.Palmer KT, Calnan M, Wainwright D, Poole J, O’Neill C, Winterbottom A, et al. Disabling musculoskeletal pain and its relation to somatization: a community-based postal survey. Occup Med (Lond) 2005;55(8):612–7. doi: 10.1093/occmed/kqi142. [DOI] [PubMed] [Google Scholar]
- 6.Palmer KT, Reading I, Linaker C, Calnan M, Coggon D. Population-based cohort study of incident and persistent arm pain: role of mental health, self-rated health and health beliefs. Pain. 2008;136(1-2):30–7. doi: 10.1016/j.pain.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miranda H, Viikari-Juntura E, Heistaro S, Riihimaki H. A Population Study on Differences in the Determinants of a Specific Shoulder Disorder versus Nonspecific Shoulder Pain Without Clinical Findings. Am J Epidemiology. 2005;161(9):847–855. doi: 10.1093/aje/kwi112. [DOI] [PubMed] [Google Scholar]
- 8.Ryall C, Coggon D, Peveler R, Poole J, Palmer K. A prospective cohort study of arm pain in primary care and physiotherapy-prognostic determinants. Rheumatology (Oxford) 2007;46(3):508–515. doi: 10.1093/rheumatology/kel320. [DOI] [PubMed] [Google Scholar]
- 9.Madan I, Reading I, Palmer KT, Coggon D. Cultural differences in musculoskeletal symptoms and disability. Int J Epidemiol. 2008;37(5):1181–9. doi: 10.1093/ije/dyn085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexopoulos EC, Burdorf A, Kalokerinou A. A comparative analysis on musculoskeletal disorders between Greek and Dutch nursing personnel. Int Arch Occup Environ Health. 2006;79(1):82–8. doi: 10.1007/s00420-005-0033-z. [DOI] [PubMed] [Google Scholar]
- 11.Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129(3):332–42. doi: 10.1016/j.pain.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 12.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. Jama. 1998;280(2):147–51. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 13.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002;27(5):E109–20. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 14.Croft P, Schollum J, Silman A. Population study of tender point counts and pain as evidence of fibromyalgia. BMJ. 1994;309(6956):696–9. doi: 10.1136/bmj.309.6956.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kamaleri Y, Natvig B, Ihlebaek CM, Bruusgaard D. Localised or widespread musculoskeletal pain: does it matter? Pain. 2008;138(1):41–6. doi: 10.1016/j.pain.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Kamaleri Y, Natvig B, Ihlebaek CM, Benth JS, Bruusgaard D. Number of pain sites is associated with demographic, lifestyle, and health related factors in the general population. Eur J Pain. 2008;12(6):742–8. doi: 10.1016/j.ejpain.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Keenan AM, Tennant A, Fear J, Emery P, Conaghan PG. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Rheum. 2006;55(5):757–64. doi: 10.1002/art.22239. [DOI] [PubMed] [Google Scholar]
- 18.Carnes D, Parsons S, Ashby D, Breen A, Foster NE, Pincus T, et al. Chronic musculoskeletal pain rarely presents in a single body site: results from a UK population study. Rheumatology (Oxford) 2007;46(7):1168–70. doi: 10.1093/rheumatology/kem118. [DOI] [PubMed] [Google Scholar]
- 19.Andersson HI. The epidemiology of chronic pain in a Swedish rural area. Qual Life Res. 1994;3(Suppl 1):S19–26. doi: 10.1007/BF00433371. [DOI] [PubMed] [Google Scholar]
- 20.Walker-Bone K, Reading I, Coggon D, Cooper C, Palmer KT. The anatomical pattern and determinants of pain in the neck and upper limbs: an epidemiologic study. Pain. 2004;109(1-2):45–51. doi: 10.1016/j.pain.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Nyman T, Grooten W, Wiktorin C, Liwing J, Norrman L. Sickness absence and concurrent low back and neck-shoulder pain: results from the MUSIC-Norrtalje study. Eur Spine J. 2007;16(5):631–638. doi: 10.1007/s00586-006-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morken T, Riise T, Moen B, Hauge SH, Holien S, Langedrag A, et al. Low back pain and widespread pain predict sickness absence among industrial workers. BMC Musculoskelet Disord. 2003;4:21. doi: 10.1186/1471-2474-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexopoulos EC, Burdorf A, Kalokerinou A. Risk factors for musculoskeletal disorders among nursing personnel in Greek hospitals. Int Arch Occup Environ Health. 2003;76(4):289–294. doi: 10.1007/s00420-003-0442-9. [DOI] [PubMed] [Google Scholar]
- 24.Nahit ES, Hunt IM, Lunt M, Dunn G, Silman AJ, Macfarlane GJ. Effects of psychosocial and individual psychological factors on the onset of musculoskeletal pain: common and site-specific effects. Ann Rheum Dis. 2003;62(8):755–760. doi: 10.1136/ard.62.8.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernard BP, editor. Musculoskeletal Disorders and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati: 1997. NIOSH Publication No. 97-141. [Google Scholar]
- 26.Holmberg S, Thelin A, Stiernstrom EL, Svardsudd K. Low back pain comorbidity among male farmers and rural referents: a population-based study. Ann Agric Environ Med. 2005;12(2):261–268. [PubMed] [Google Scholar]
- 27.Hagen EM, Svensen E, Erikse HR, Ihlebaek C, Ursin H. Comorbid Subjective Health Complaints in Low Back Pain. Spine. 2006;31(12):1491–95. doi: 10.1097/01.brs.0000219947.71168.08. [DOI] [PubMed] [Google Scholar]
- 28.Eriksen W. The prevalence of musculoskeletal pain in Norwegian nurses’ aides. Int Arch Occup Environ Health. 2003;76(8):625–30. doi: 10.1007/s00420-003-0453-6. [DOI] [PubMed] [Google Scholar]
- 29.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med. 2004;61(5):398–404. doi: 10.1136/oem.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petzke F, Gracely RH, Park KM, Ambrose K, Clauw DJ. What do tender points measure? Influence of distress on 4 measures of tenderness. J Rheumatol. 2003;30(3):567–74. [PubMed] [Google Scholar]
- 31.Schochat T, Raspe H. Elements of fibromyalgia in an open population. Rheumatology (Oxford) 2003;42(7):829–35. doi: 10.1093/rheumatology/keg199. [DOI] [PubMed] [Google Scholar]
- 32.Harkness EF, Macfarlane GJ, Nahit E, Silman AJ, McBeth J. Mechanical injury and psychosocial factors in the work place predict the onset of widespread body pain: a two-year prospective study among cohorts of newly employed workers. Arthritis Rheum. 2004;50(5):1655–64. doi: 10.1002/art.20258. [DOI] [PubMed] [Google Scholar]
- 33.Karasek R. Job demands, job decision latitude and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285–307. [Google Scholar]
- 34.Ware J. SF-36 Health Status Questionnaire. Institute for the Improvement of Medical Care and Health, New England Medical Center Hospital, Quality Quest Inc; Boston, MA: 1989. [Google Scholar]
- 35.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 36.Bagby M, Taylor G, Parker J. The revised Toronto Alexithymia Scale: Some reliability, validity and normative data. Psychotherapy & Psychosomatics. 1992;57(1-2):34–41. doi: 10.1159/000288571. [DOI] [PubMed] [Google Scholar]
- 37.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 38.Donias S, Demertzis I. Greek validation of depressive symptomatology with the Beck Depression Inventory. 10th Greek conference on Neurology and Psychiatry; Thessaloniki, Greece. 1983. pp. 486–492. [Google Scholar]
- 39.Donias S, Demertzis I. Investigation of depression in a Greek random mixed psychiatric population with the Beck Depression Inventory. 10th Greek conference on Neurology and Psychiatry; Thessaloniki, Greece. 1983. pp. 470–485. [Google Scholar]
- 40.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 41.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–7. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 42.Solidaki E. Master’s thesis: Pilot study in Crete for an international survey on musculoskeletal disorders. 2006 Available at: http://mph.med.uoc.gr/files/Dissertations/2006_Solidaki.pdf.
- 43.Brauer C, Thomsen JF, Loft IP, Mikkelsen S. Can we rely on retrospective pain assessments? Am J Epidemiol. 2003;157(6):552–557. doi: 10.1093/aje/kwg017. [DOI] [PubMed] [Google Scholar]
- 44.Frome EL, Checkoway H. Epidemiologic programs for computers and calculators. Use of Poisson regression models in estimating incidence rates and ratios. Am J Epidemiol. 1985;121(2):309–23. doi: 10.1093/oxfordjournals.aje.a114001. [DOI] [PubMed] [Google Scholar]
- 45.Tsou TS. Robust poisson regression. Journal Stat Plan Infer. 2006;136(9):3173–3186. [Google Scholar]
- 46.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and Regression Trees. Chapman & Hall (Wadsworth Inc.); New York: 1984. [Google Scholar]
- 47.Lewis RJ. An introduction to classification and regression tree (CART) analysis. Annual Meeting of the Society for Academic Emergency Medicine; San Francisco, California. 2000. [Google Scholar]
- 48.McBeth J, Macfarlane GJ, Benjamin S, Silman AJ. Features of somatization predict the onset of chronic widespread pain: results of a large population-based study. Arthritis Rheum. 2001;44(4):940–6. doi: 10.1002/1529-0131(200104)44:4<940::AID-ANR151>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 49.Croft P. The epidemiology of pain: the more you have, the more you get. Ann Rheum Dis. 1996;55(12):859–60. doi: 10.1136/ard.55.12.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palmer KT, Reading I, Calnan M, Linaker C, Coggon D. Does knee pain in the community behave like a regional pain syndrome? Prospective cohort study of incidence and persistence. Ann Rheum Dis. 2007;66(9):1190–4. doi: 10.1136/ard.2006.061481. [DOI] [PMC free article] [PubMed] [Google Scholar]