Abstract
Background
Objective quantification of physical activity (PA) is needed to understand PA and sedentary behaviors in bariatric surgery patients, yet it is unclear whether PA estimates produced by different monitors are comparable and can be interpreted similarly across studies. We compared PA estimates from the Stayhealthy RT3 triaxial accelerometer (RT3) and the Sensewear Pro2 Armband (SWA) at both the group and individual participant level.
Methods
Bariatric surgery candidates were instructed to wear the RT3 and SWA during waking hours for seven days. Participants meeting valid wear time requirements (≥4 days of ≥8 hours/day) for both monitors were included in the analyses. Time spent in sedentary (<1.5 METs), light (1.5–2.9 METs), moderate-to-vigorous (MVPA; ≥3.0 METs), and total PA (TPA; ≥1.5 METs) according to each monitor was compared.
Results
Fifty-five participants (BMI: 48.4±8.2 kg/m2) met wear time requirements. Daily time spent in sedentary (RT3: 582.9±94.3; SWA: 602.3±128.6 min), light (RT3: 131.9±60.0; SWA: 120.6±65.7 min), MVPA (RT3: 25.9±20.9; SWA: 29.9±19.5 min), and TPA (RT3: 157.8±74.5; SWA: 150.6±80.7 min) was similar between monitors (p>0.05). While the average difference in TPA between the two monitors at the group level was 7.2±64.2 minutes; the average difference between the two monitors for each participant was 45.6±45.4 minutes.
Conclusions
At the group level, the RT3 and SWA provide similar estimates of PA and sedentary behaviors; however concordance between monitors may be compromised at the individual level. Findings related to PA and sedentary behaviors at the group level can be interpreted similarly across studies when either monitor is used.
Keywords: Physical activity, exercise, bariatric surgery, severely obese
Introduction
The role of physical activity (PA) for optimizing bariatric surgery outcomes has been receiving growing attention [1–2]. Results from studies using questionnaires to assess PA suggest that patients who report higher PA levels postoperatively [3] and greater pre- to postoperative increases in the amount [4–5] or intensity [6] of PA achieve more successful weight loss outcomes. However, self-report measures of PA typically overestimate actual PA in obese individuals [7–8], including those who have undergone bariatric surgery [9]. Consequently, objective monitors are increasingly being used to obtain more precise estimates of the amount and patterns of PA in bariatric surgery patients.
To date, three different types of objective monitors have been incorporated in studies of PA among individuals undergoing bariatric surgery: pedometers [4, 10], accelerometers [9, 11–13], and the Sensewear Pro2 Armband [14–15]. Pedometers count steps taken by detecting hip movement during ambulation, but typically do not allow for the duration and intensity of activities to be determined [16]. For this reason accelerometers and armbands, although more costly, may have a distinct advantage over pedometers given their capacity to capture minute-by-minute energy expenditure data. Accelerometers are worn on the waist and use microelectronic sensors to measure changes in velocity across multiple planes of movement (vertical, anterposterior and/or lateral), thus allowing for the quantification of time spent in sedentary, light, moderate, and vigorous intensity PA [16]. In addition, although not formally tested, it has been suggested that a newer monitoring technology, the Sensewear Pro2 Armband (SWA), may improve the accuracy of measuring PA by combining accelerometry with a unique combination of sensors that assess various physiological parameters (i.e., heat flux, galvanic skin response, skin temperature, and near body temperature).
Given the increasing use of objective monitors to assess PA in bariatric surgery patients, it is important to know whether data provided by different monitors, particularly those that are worn on different locations on the body, are comparable and can be interpreted similarly across studies. Thus, the purpose of this study was to evaluate agreement between the waist-worn Stayhealthy RT3 (Stayhealthy, Monrovia, CA) triaxial accelerometer and Sensewear armband at the group and individual level in time spent in sedentary, light-intensity PA, moderate-to-vigorous intensity PA (MVPA), and total physical activity (TPA) among bariatric surgery patients preoperatively. Additionally, we assessed whether adherence to minimal wear time requirements differed by monitor. Findings from this study will provide enhanced understanding of PA patterns among bariatric surgery patients and could help future investigators to make more informed decisions when designing studies to assess PA in this population.
Materials and Methods
Participants and procedures
Seventy-nine severely obese individuals (BMI ≥ 35 kg/m2) presenting for bariatric surgery were recruited to participate in this study during their surgical consultation visit. Participants had to be ambulatory, non-smokers, and between the ages of 18 and 65. After informed consent was obtained, participants had their height and weight measured and completed a demographics questionnaire. These data were used to program the Stayhealthy RT3 accelerometer (RT3) and the Sensewear Pro2 Armband (SWA) for each individual. Participants were then fitted with these two monitors, and instructed to wear them during all waking hours (except while bathing or swimming) for seven consecutive days. Study procedures were approved by The Miriam Hospital Institutional Review Board (Providence, RI) and participants were compensated $15 for participation in this study.
Objective physical activity monitors
Stayhealthy RT3
The RT3 triaxial accelerometer (Stayhealthy, Inc, Monrovia, CA) was chosen given its use in both large scale clinical weight loss trials [17–18] and studies of PA in bariatric surgery patients [9, 12]. This monitor is similar in size to a pager, worn on the waist, and assesses PA by detecting movement in the vertical, horizontal, and anterior-posterior planes and converting these data into counts. Count values are then incorporated into proprietary algorithms and a metabolic equivalent (MET) is calculated for each minute the monitor is worn. METs are a method of expressing exercise intensity as a ratio of the energy cost of an activity compared to resting metabolic rate (RMR). Therefore, 1 MET is considered as the RMR and 3 METs represents any activity that has an energy cost that is three times greater than RMR and is equivalent to moderate-intensity PA.
Sensewear Pro2 Armband
The SWA (BodyMedia, Pittsburgh, PA) is worn on the back of the upper right triceps and assesses PA using a biaxial accelerometer and a unique combination of heat sensors (heat flux, galvanic skin response, skin temperature, and near body temperature). Data collected through these sensors is integrated into proprietary algorithms to provide minute-by-minute estimates of energy expenditure, assigning a MET value to each minute the monitor is worn. Energy expenditure estimates produced by the SWA have previously been shown to be valid when compared to indirect calorimetry [19] and doubly labeled water [20] in adult populations. In addition, when time spent in MVPA was assessed by indirect calorimetry and three different activity monitors, the mean difference between the SWA and indirect calorimetry was small (1.1 min of a 120-min exercise bout) and less than that seen with the other monitors [21]. The SWA has also been used to assess PA and sedentary behaviors in severely obese cohorts, including bariatric surgery patients [14–15, 22–23].
Assessment of wear time and quantification of physical activity
The Sensewear® Professional software (Version 6.1) and the Stayhealthy Software, were used to calculate SWA and RT3 wear time respectively. RT3 wear time was determined by taking 1440 minutes (total number of minutes in a day) and subtracting any periods of non-wear time, defined as any period ≥ 30 consecutive minutes of zero counts (permitting intervals of up to 2 consecutive minutes registering 1–100 counts/min). SWA wear time was provided directly via the computer software.
The Sensewear® Professional software (Version 6.1) and the Stayhealthy Software were also used to calculate the number of days and hours participants wore the SWA and RT3, respectively. Time spent in sedentary activities (<1.5 METs) and light (1.5 to <3.0 METs), moderate-to-vigorous (MVPA; ≥ 3.0 METs), and total (TPA; ≥ 1.5 METs) PA were expressed in minutes and also as a percentage of total wear time. Moderate-to-vigorous intensity PA is equivalent to activities such as brisk walking or bicycling whereas light PA is similar to easy household chores. Only those participants meeting valid wear time requirements (≥ 4 days and ≥ 8 hours/day) were included in the analyses. In addition, only days in which the monitor was worn for ≥ 8 hours were used when processing the data.
Statistical analysis
Descriptive statistics were generated and expressed as mean ± standard deviation for continuous variables and as a proportion for categorical variables. Paired-sample t-tests were used to examine differences in wear time, sedentary behaviors, light, MVPA and TPA between monitors. A Bland-Altman plot was developed to determine the individual level of agreement in TPA between the SWA and RT3. Analyses were performed using SPSS for Windows (14.0).
Results
Participants
Seventy-nine bariatric surgery candidates were instructed to wear the RT3 and SWA during waking hours for 7 days. A similar number of participants met the minimal wear time requirements (≥4 days of ≥ 8 hours of wear time per day) for the RT3 (n=64; 81%) and SWA (n=69; 87%; p>0.05). To appropriately compare the monitors in time spent in PA and sedentary behaviors, only those participants who met valid wear time requirements for both instruments (n=61; 77% of sample) were included in subsequent analyses. An additional 6 participants were excluded because they wore one of the two monitors during non-waking hours (defined by ≥ 18 hours/day). Subsequent analyses focus on the remaining 55 participants. Eighty-five percent of these participants were female, they averaged 42.8 ± 9.6 years of age, had a mean BMI and weight of 48.4 ± 8.2 kg/m2 and 131.4 ± 22.8 kg respectively, and 76% were non-Hispanic white. Participants wore the RT3 and SWA for a similar (p>0.05) number of days (RT3: 6.44 ± 0.9 vs. SWA: 6.31 ± 1.1 days) and hours per day (RT3: 12.4 ± 1.2 vs. SWA: 12.6 ± 1.6 hours/day).
Level of agreement between SWA and RT3 at group level
The RT3 and SWA monitors were significantly correlated with one another for time spent in sedentary activities (r=0.60), light PA (r=0.67), MVPA (r=0.48), and TPA (r=0.66; p<0.001). As shown in Table 1, both monitors produced similar (p>0.05) estimates of daily time and percentage of daily wear time spent in each of these activity categories. The mean difference between monitors was approximately 19 minutes for sedentary behaviors, 11 minutes for light PA, 4 minutes for MVPA, and 7 minutes for TPA.
Table 1.
Comparison of Sensewear Pro Armband (SWA)- and Stayhealthy RT3- monitored time spent in sedentary, light, moderate-to-vigorous (MVPA), and total physical activities (TPA)
| Activity intensity (METs)* |
Daily Minutes | Daily Percentage of Time | ||||
|---|---|---|---|---|---|---|
| SWA | RT3 | P value | SWA | RT3 | P value | |
| Sedentary (min/d) | 602.3 ± 128.6 | 582.9 ± 94.3 | 0.174 | 79.6 ± 11.5 | 78.6 ± 10.1 | 0.465 |
| Light (min/d) | 120.6 ± 65.7 | 131.9 ± 60.0 | 0.108 | 16.3 ± 9.3 | 17.8 ± 8.0 | 0.148 |
| MVPA (min/d) | 29.9 ± 19.5 | 25.9 ± 20.9 | 0.149 | 4.1 ± 2.8 | 3.5 ± 2.9 | 0.172 |
| TPA (min/day) | 150.6 ± 80.7 | 157.8 ± 74.5 | 0.408 | 20.4 ± 11.5 | 21.3 ± 10.1 | 0.458 |
Values are mean ± standard deviation.
Activity intensity (METs) thresholds = sedentary (< 1.5 METs), light (1.5–2.9 METs), MVPA (≥ 3.0 METs), TPA (≥ 1.5 METs)
Level of agreement between SWA and RT3 at individual level
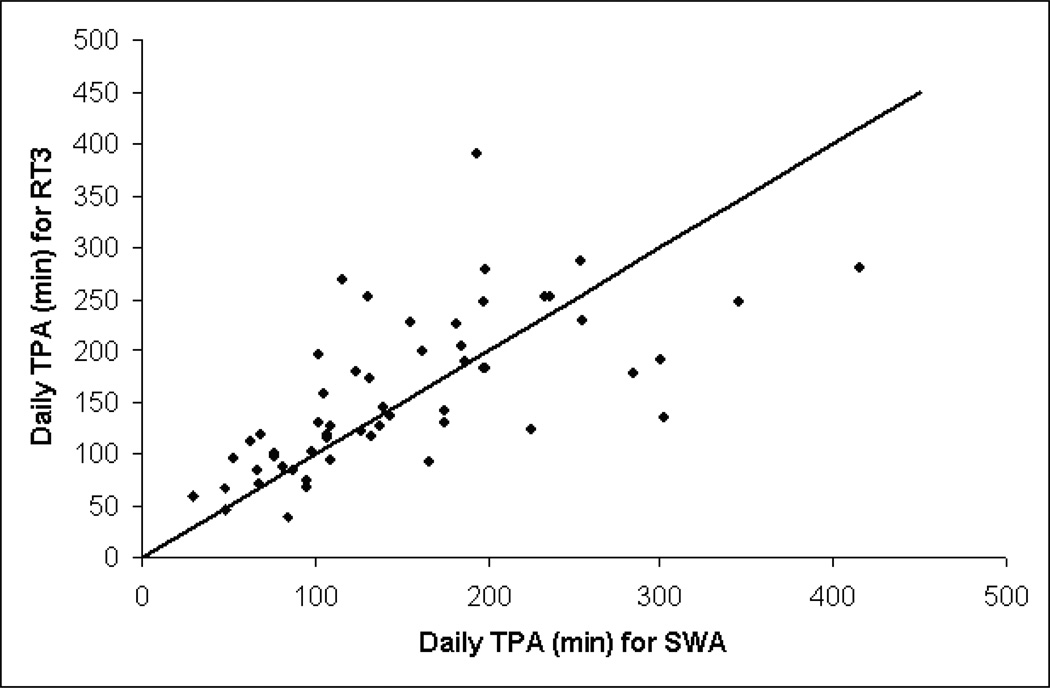
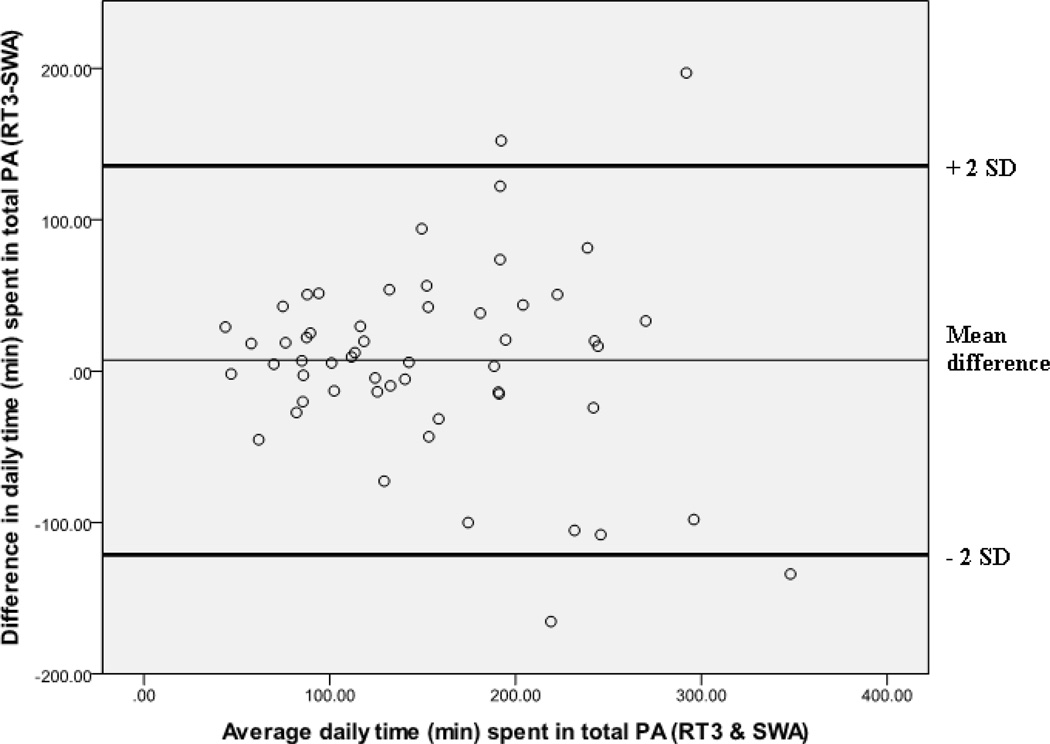
Figure 1 illustrates the individual differences in total PA as assessed by each monitor. The mean difference in TPA between SWA and RT3 was 7.2 minutes; however the mean absolute error (computed using the absolute value of the discrepancy between monitors) was 45.6 ± 45.4 minutes, and the relative difference ranged from −165 to 197 minutes. The two monitors estimated TPA to be within 15, 30 and 60 minutes of one another 29%, 53%, and 76% of the time respectively. In 60% of participants, the RT3 produced higher estimates of TPA. To evaluate systematic bias, a Bland-Altman plot was generated for TPA (Figure 2). The correlation between the average in TPA and the difference in TPA between the RT3 and SWA was r=−0.106 (p=0.44), suggesting that the bias between monitors was not related to TPA minutes.
Figure 1. Relationship between daily physical activity minutes measured by the Sensewear Pro Armband (SWA) and Stayhealthy RT3.
Total physical activity (TPA) is defined as activities of light-intensity or higher (≥ 1.5 METs).
Solid line indicates line of identity (y=x).
Figure 2. Bland Altman plot of total daily physical activity measured by the Sensewear Pro Armband (SWA) and Stayhealthy RT3.
Total physical activity is defined as activities of light-intensity or higher (≥ 1.5 METs)
Discussion
Given the importance of quantifying physical activity in bariatric surgery patients as well as the rapidly emerging field of objective physical activity measurement, it is important to determine whether PA estimates produced by different objective monitors are comparable and can be interpreted similarly across studies. This study utilized two increasingly popular PA monitors, the RT3 accelerometer and the Sensewear Pro2 armband, and found that at the group level, both monitors provided similar estimates of time spent in sedentary, light, MVPA, and total PA. However, concordance between the monitors at the individual level varied significantly, with the RT3 reporting higher estimates of total PA approximately 60% of the time.
While it has previously been shown that self-reported and objectively-measured PA estimates differ considerably in bariatric surgery patients [9], the current study is the first to examine if there are differences in PA estimates between two different objective PA monitors in a bariatric surgery population. The RT3 accelerometer has been used to assess PA in a free-living environment within several large scale studies [17–18]; however some investigators suggest that hip-mounted accelerometers cannot capture highly static activities or complex movement patterns [24–25]. Therefore, the Sensewear armband may be advantageous because it is worn on the upper arm and incorporates physiological parameters as well as accelerometry [25]. However, findings from the current study suggest that the RT3 and SWA provided similar estimates of PA for the sample as a whole, with only small differences in daily time spent in sedentary, light, MVPA, and TPA between monitors. On average, participants spent approximately 20% of their day at a MET level ≥ 1.5 METs and total physical activity was approximately 7 minutes higher when assessed via the RT3 compared to the SWA.
Although our findings suggest that these monitors are in agreement at the group level, we found greater variability in estimates at the individual level, with differences between monitors for TPA ranging from −165 minutes (SWA higher) to 197 minutes (RT3 higher). This large degree of individual variability between the RT3 and SWA is consistent with other studies comparing different objective monitors in a non-surgical population [26–27] and reflects a short-coming in the use of such monitors to measure PA. Reasons for varying estimates between the SWA and RT3 are unclear. It is possible that the two monitors incorporate different estimates of resting energy expenditure, which subsequently alter MET values. However, we do not have access to proprietary algorithms to confirm this information. Another explanation is that the monitors may be picking up extra movement or too little movement due to differences in monitor location (e.g. upper arm vs. waist-mounted) or as a result of wear-related issues associated with excess body weight. Further validation studies for both monitors in a severely obese population are needed. However, taken as a whole, our data suggest that for research purposes and for quantifying PA at a group level in a bariatric surgery population, both the SWA and RT3 will provide equivalent estimates of PA and sedentary time. However, when dealing with individual patients in clinical practice, using these monitors to measure PA may be more of a concern given the large individual variability seen between monitors.
From a feasibility standpoint, it is important to choose a PA monitor that is acceptable for wear by the participant to ensure that sufficient data is collected to perform necessary analyses. It has previously been suggested that ≥ 4 days of ≥ 8 hours/day is an adequate minimum wear time threshold when assessing daily activity patterns in groups of individuals [28]. This study is the first to demonstrate that bariatric surgery candidates are equally compliant to wearing the RT3 and SWA with 81% and 87% of participants respectively achieving the minimum acceptable wear time. Furthermore, the criterion of ≥ 1 valid day has previously been employed in large population studies [23, 29]. When our data were analyzed using this criteria, 91% and 95% of participants met the criteria for the RT3 and SWA respectively. Together these data demonstrate that both monitors have satisfactory rates of compliance, especially considering that participants received little compensation for participation in this study and they were not invested to the researchers as is the case with intervention studies.
Our findings build upon the growing research in the area of assessing PA in a bariatric surgery population using objective measures. A major strength of this study is that it is the first to compare two PA monitors in their ability to measure PA and sedentary time in a free living environment. However, this study is limited by the fact that it was not a validation study, and we are therefore unable to determine which monitor is most accurate. A validation study would be nearly impossible to conduct under free-living conditions given that doubly labeled water methods can not differentiate sedentary, light PA, and MVPA and indirect calorimetry is impractical. However future lab-based studies are needed to determine the validity of these monitors during various types of sedentary, light, and moderate-to-vigorous intensity activities, in both surgical and non-surgical obese populations. Additionally, although adherence to wear time requirements was adequate, it is unclear why some participants did not wear each monitor for the full seven days. It is possible that they simply forgot to wear the monitor or it may have been uncomfortable or restricting to wear. However, given that research has previously demonstrated that surgical patients tend to exhibit poor compliance with behavioral recommendations [30], the fact that over 80% of the sample met the wear time requirements for one of the two monitors is encouraging for future research. Future studies should begin to examine the validity of these monitors in a severely obese cohort by comparing RT3 and SWA-assessed estimates of PA against indirect calorimetry during different types of PA. Such studies could lead to the development of algorithms that are specific to a severely obese population which could potentially reduce some of the individual variability seen between PA monitors. In addition, qualitative data should be collected to examine individual preferences for wearing a waist-mounted monitor versus a monitor that is worn on the arm.
In conclusion, this study showed that the SWA and RT3 provide similar estimates of physical activity at the group level, but concordance between these monitors may be compromised when examining estimates at the individual level. Our findings suggest that PA and sedentary time in a bariatric surgery population can be compared across studies when either of these monitors is utilized. Although the location where the monitor is worn differed (waist vs. upper arm), time spent in various activity categories remained the same. Thus as the use of objective PA monitors become increasingly utilized, these data will inform future research efforts by contributing to our knowledge surrounding the acceptability of these monitors in a severely obese population. Furthermore, these findings will enhance our understanding of PA and sedentary behaviors in a surgical population and allow investigators to make more informed decisions when choosing a PA measurement tool.
Acknowledgements
This research was funded by grants from The Warren Alpert Medical School of Brown University’s Center of Excellence in Women’s Health and the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK083438-01) awarded to Drs. Wing and Bond, respectively. Appreciation is expressed to Richard Daniello, B.A. for his assistance in processing the RT3 and SWA data.
Footnotes
Conflict of Interest
Dr. Jakicic received a grant from BodyMedia, Inc. (Pittsburgh, PA) to conduct a non-related study using the armband technology. Dr. Jakicic is also a scientific advisor to Free & Clear. All other authors declare no conflicts of interest.
References
- 1.Livhits M, Mercado C, Yermilov I, et al. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20:657–665. doi: 10.1007/s11695-010-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobi D, Ciangura C, Couet C, et al. Physical activity and weight loss following bariatric surgery. Obes Rev. 2010 doi: 10.1111/j.1467-789X.2010.00731.x. [DOI] [PubMed] [Google Scholar]
- 3.Evans RK, Bond DS, Wolfe LG, et al. Participation in 150 min/wk of moderate or higher intensity physical activity yields greater weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2007;3:526–530. doi: 10.1016/j.soard.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Colles SL, Dixon JB, O'Brien PE. Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obes Surg. 2008;18:833–840. doi: 10.1007/s11695-007-9409-3. [DOI] [PubMed] [Google Scholar]
- 5.Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring) 2009;17:78–83. doi: 10.1038/oby.2008.501. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberger PH, Henderson KE, White MA, et al. Physical Activity in Gastric Bypass Patients: Associations with Weight Loss and Psychosocial Functioning at 12-Month Follow-Up. Obes Surg. 2010 doi: 10.1007/s11695-010-0283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lichtman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 8.Jakicic JM, Polley BA, Wing RR. Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Med Sci Sports Exerc. 1998;30:634–638. doi: 10.1097/00005768-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self report vs. objective measures. Obesity (Silver Spring) 2010;18:2395–2397. doi: 10.1038/oby.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2010;6:361–366. doi: 10.1016/j.soard.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 11.King WC, Belle SH, Eid GM, et al. Physical activity levels of patients undergoing bariatric surgery in the Longitudinal Assessment of Bariatric Surgery study. Surg Obes Relat Dis. 2008;4:721–728. doi: 10.1016/j.soard.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bond DS, Jakicic JM, Vithiananthan S, et al. Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surg Obes Relat Dis. 2010;6:72–78. doi: 10.1016/j.soard.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim RBL, Jones DB, Rooks D, Lin H, Schneider B, Dushay J, Wollner S, Blackburn GL. Can Healthcare Providers Increase Preoperative Physical Activity Levels in Bariatric Surgery Patients. Obesity and Weight Management. 2010;6:119–122. [Google Scholar]
- 14.Bond DS, Unick JL, Jakicic JM, et al. Objective Assessment of Time Spent Being Sedentary in Bariatric Surgery Candidates. Obes Surg. 2010 doi: 10.1007/s11695-010-0151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Josbeno DA, Kalarchian M, Sparto PJ, et al. Physical Activity and Physical Function in Individuals Post-bariatric Surgery. Obes Surg. 2010 doi: 10.1007/s11695-010-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corder K, Brage S, Ekelund U. Accelerometers and pedometers: methodology and clinical application. Curr Opin Clin Nutr Metab Care. 2007;10:597–603. doi: 10.1097/MCO.0b013e328285d883. [DOI] [PubMed] [Google Scholar]
- 17.Jakicic JM, Gregg E, Knowler W, et al. Activity patterns of obese adults with type 2 diabetes in the look AHEAD study. Med Sci Sports Exerc. 2010;42:1995–2005. doi: 10.1249/MSS.0b013e3181e054f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young DR, Jerome GJ, Chen C, et al. Patterns of physical activity among overweight and obese adults. Prev Chronic Dis. 2009;6:A90. [PMC free article] [PubMed] [Google Scholar]
- 19.Jakicic JM, Marcus M, Gallagher KI, et al. Evaluation of the SenseWear Pro Armband to assess energy expenditure during exercise. Medicine and science in sports and exercise. 2004;36:897–904. doi: 10.1249/01.mss.0000126805.32659.43. [DOI] [PubMed] [Google Scholar]
- 20.Johannsen DL, Calabro MA, Stewart J, et al. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Medicine and science in sports and exercise. 2010;42:2134–2140. doi: 10.1249/MSS.0b013e3181e0b3ff. [DOI] [PubMed] [Google Scholar]
- 21.Berntsen S, Hageberg R, Aandstad A, et al. Validity of physical activity monitors in adults participating in free-living activities. Br J Sports Med. 2010;44:657–664. doi: 10.1136/bjsm.2008.048868. [DOI] [PubMed] [Google Scholar]
- 22.Goodpaster BH, Delany JP, Otto AD, et al. Effects of Diet and Physical Activity Interventions on Weight Loss and Cardiometabolic Risk Factors in Severely Obese Adults: A Randomized Trial. JAMA. 2010 doi: 10.1001/jama.2010.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanhecke TE, Franklin BA, Miller WM, et al. Cardiorespiratory fitness and sedentary lifestyle in the morbidly obese. Clin Cardiol. 2009;32:121–124. doi: 10.1002/clc.20458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bouten CVC, Koekkoek KTM, Verduin M, et al. A triaxial accelerometer and portable data processing unit for the assessment of daily physical activity. Biomedical Engineering. 1997;44:136–147. doi: 10.1109/10.554760. [DOI] [PubMed] [Google Scholar]
- 25.Ward DS, Evenson KR, Vaughn A, et al. Accelerometer use in physical activity: best practices and research recommendations. Medicine and science in sports and exercise. 2005;37:S582–S588. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 26.Welk GJ, Blair SN, Wood K, et al. A comparative evaluation of three accelerometry-based physical activity monitors. Medicine and science in sports and exercise. 2000;32:S489–S497. doi: 10.1097/00005768-200009001-00008. [DOI] [PubMed] [Google Scholar]
- 27.Tudor-Locke C, Ainsworth BE, Thompson RW, et al. Comparison of pedometer and accelerometer measures of free-living physical activity. Medicine and science in sports and exercise. 2002;34:2045–2051. doi: 10.1097/00005768-200212000-00027. [DOI] [PubMed] [Google Scholar]
- 28.Chen C, Jerome GJ, Laferriere D, et al. Procedures used to standardize data collected by RT3 triaxial accelerometers in a large-scale weight-loss trial. J Phys Act Health. 2009;6:354–359. doi: 10.1123/jpah.6.3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American journal of epidemiology. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas JG, Bond DS, Ryder BA, et al. Ecological momentary assessment of recommended postoperative eating and activity behaviors. Surg Obes Relat Dis. 2011;7:206–212. doi: 10.1016/j.soard.2010.10.007. [DOI] [PubMed] [Google Scholar]