Abstract
Aim
This paper is a report of an analysis of the concept of nursing surveillance.
Background
Nursing surveillance, a primary function of acute care nurses, is critical to patient safety and outcomes. Although it has been associated with patient outcomes and organizational context of care, little knowledge has been generated about the conceptual and operational process of surveillance.
Data sources
A search using the CINAHL, Medline and PubMed databases was used to compile an international data set of 18 papers and 4 book chapters published from 1985 to 2009.
Review methods
Rodger’s evolutionary concept analysis techniques were used to analyse surveillance in a systems framework. This method focused the search to nursing surveillance (as opposed to other medical uses of the term) and used a theoretical framework to guide the analysis.
Results
The examination of the literature clarifies the multifaceted nature of nursing surveillance in the acute care setting. Surveillance involves purposeful and ongoing acquisition, interpretation and synthesis of patient data for clinical decision- making. Behavioural activities and multiple cognitive processes are used in surveillance in order for the nurse to make decisions for patient safety and health maintenance. A systems approach to the analysis also demonstrates how organizational characteristics and contextual factors influence the process in the acute care environment.
Conclusion
This conceptual analysis describes the nature of the surveillance process and clarifies the concept for effective communication and future use in health services research.
Keywords: acute care, concept analysis, nurse, patient safety, surveillance, work environment
Introduction
An essential part of the acute care nurse’s role is to actively engage in the continuous process of keeping patients safe and preventing deterioration of their health (Institute of Medicine 2004). As the primary 24-hour professional presence in the hospital, nurses continuously use this process, known as nursing surveillance, with all patients, and in all acute care settings and specialties. Hallmarks of surveillance include collecting, analysing and interpreting information to make patient care decisions (Bulechek et al. 2008). In providing surveillance, nurses have the potential to minimize negative outcomes by preventing adverse events or deterioration in the patient’s status (Aiken et al. 2003). This potential to influence outcomes has led to an increased use of the hypothesized relationship between nursing surveillance and outcomes in health services research, especially in the acute care setting (Zeitz 2005, Shever et al. 2008, Kutney-Lee et al. 2009). Specifically, surveillance is hypothesized to precede and influence patient outcomes, such as failure-to-rescue, defined as the inability to prevent a hospitalized patient from dying after an adverse event (Clarke & Aiken 2003). Despite being a critical component of the care nurses provide, little is known about this complex concept and its potential significance on patient outcomes. The purpose of this concept analysis is to clarify and describe the multifaceted nature of nursing surveillance so that can be applied in the acute care environment.
Background
Across disciplines, the term surveillance has been used to describe a process of collecting, analysing and taking action based on facts and data (Schoneman 2002). The term surveillance has typically been described and used in aviation, military, intelligence/espionage and public health fields. In public health, surveillance is an intermittent process used for the purpose of information collection and dissemination (Thacker et al. 1989). The process, which can be described as either passive or active, is used as a tool to empower decision-making and identify needed public health interventions in populations, such as when disease outbreak occurs. Intelligence, on the other hand, uses an active process to avoid threats and minimize possible negative consequences (Dougherty 1999). The goal of intelligence and espionage surveillance is to obtain information and knowledge through observing, investigating, analysing and understanding data to identify and minimize threats (Chizek 2003). This type of data collection must be done systematically and by trained individuals. Threats are characterized according to the harm they can cause and are often picked up by technology and communication systems (Treverton 2001). Similar to nursing, the purposes of and primary function of the process is to reduce threats and promote health and safety.
While the term nursing surveillance was first introduced over two decades ago, (Dougherty 1985, Titler 1992) the use of the term surveillance to describe the care nurses provide has just recently come into vogue. Based on Dougherty’s (1985) early description of the concept, Titler’s (1992) research operationalized surveillance and facilitated the adoption of surveillance as an intervention into classification systems. Dougherty’s (1999) seminal definition described surveillance as the application of both cognitive and behavioural processes to make decisions and take action for the welfare of the patient. Many nursing language classification systems mirror this definition, and aim to capture the components of action, interpretation and synthesis functions performed by nurses (Martin et al. 1993, McCloskey & Bulechek 2000, AORN 2007). However, these definitions and classification systems fail to describe the concept of surveillance beyond an intervention consisting of behavioural and cognitive components. Nor has the nature of these components been expanded upon to describe thoroughly the activities or mental work involved in surveillance.
Recent literature demonstrates the continuous and comprehensive role of surveillance in the acute care environment. Previously, surveillance has been described as being synonymous with monitoring, with the words being used interchangeably when described at the intervention level (Dougherty 1999, Schoneman 2002). Today, nursing surveillance includes monitoring, but has been extended to describe a ‘process through which nurses monitor, evaluate, and act upon emerging indicators of a patient’s change in status’ (Kutney-Lee et al. 2009, p. 218). In addition to the function of monitoring, the nurse’s role of performing surveillance is extended to evaluating, analysing, interpreting, making decisions and taking action based on the conclusions made through the nurse’s analytical work. Because interventions are often described as actions or activities that describe surveillance (Titler 1992, Martin et al. 1993, Schoneman 2002), the comprehensive and continuous nature of surveillance is often missing from their definition. Describing surveillance as an ongoing process demonstrates how the role of surveillance extends beyond the activities to include the entire phenomenon in its ongoing fashion. Despite the recent literature and the expanding role in health services research, little is known about the structure, function and implications of the surveillance concept. Therefore, an in-depth concept analysis was conducted to clarify the nature and implications of surveillance for future health services research.
Rodgers evolutionary concept analysis in a systems theoretical framework
Rodgers (2000) evolutionary view of concept analysis was used in a systems theoretical framework to evaluate nursing surveillance in the acute care nursing environment. The rationale for using this method was twofold. First, the philosophical underpinnings of an evolutionary approach align with the nature, utility and perspective of nursing surveillance. The concept is an abstract of common characteristics that are dynamic and contextual, rather than universal ideas that are absolute (Rodgers 2000). The current contextual use of surveillance varies from home health, to interventional use, to public health and to patient safety in acute care (Schoneman 2002). Therefore, in addition to an evolutionary approach, this analysis was guided by a systems theory framework to give focus and meaning to the concept analysis, rather than discuss all uses of the concept. Traditional concept analyses outline a process of identifying attributes, frequency of use, necessary conditions and case scenarios of the concept (Rodgers 2000, Fawcett 2005, Walker & Avant 2005) for the purpose of clarifying concepts that can then be used across theories. This methodology is not useful for analysing surveillance because many terms in nursing, including the term surveillance, have colloquial use in addition to their meaning applied to nursing. The process of including all uses of the term in analysis does little to clarify meaning and only adds to their ambiguity and vagueness (Paley 1996). Therefore, data searching and analysis requires focus in regard to the term’s use and the idea of analysing a concept for the purpose of building theory presents vagueness in the purpose of conceptual clarification. Instead, an alternative approach of presenting the concept in a theoretical framework gives meaning to the concept, allowing for a clearer contextual meaning with the possibility that the theory (and its interpretation of the concept) is open to competing interpretations (Paley 1996).
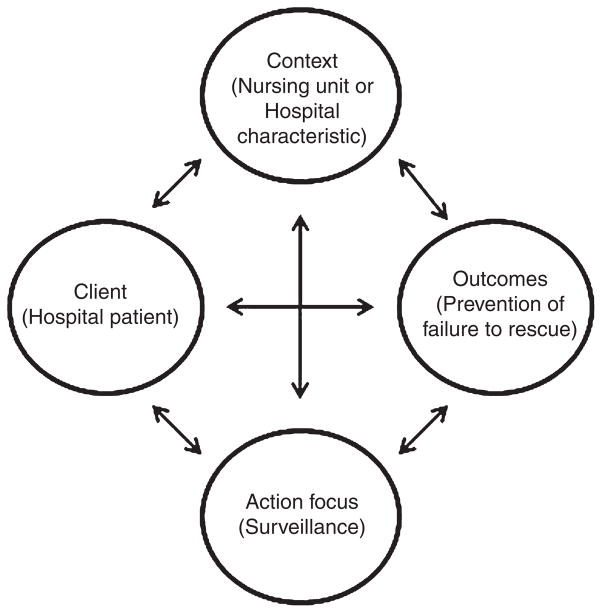
This analysis focused specifically on nursing surveillance in the acute care setting. To analyse the concept in a systems theory framework, it must be acknowledged that, in the acute care setting, individual parts function to create a dynamic whole. One framework, the Systems Research Organizing Model (SROM) (Brewer et al. 2008), accounts for factors in a healthcare system when explaining outcome responses. The SROM is based on the Quality Health Outcomes Model (QHOM), a conceptual framework that is used to explain and predict how system characteristics influence outcomes (Mitchell et al. 1998, Brewer et al. 2008). The major constructs of the QHOM include system, client, intervention and outcomes. The SROM model extends the systems perspective and relational propositions from the QHOM framework by changing the concept of systems to context, moving client to an antecedent position, creating a link between intervention and outcomes and changing the intervention construct to an action focus (Figure 1). These changes make the model unique to a systems perspective because it considers the parts that make up a whole system at an abstract level that can be used to study any phenomena of interest (Brewer et al. 2008). This model is useful in analysing surveillance because it reflects the role of surveillance in a complex acute care environment, rather than examining surveillance in isolation.
Figure 1.
Application of the systems research organizing model to nursing surveillance in the acute care setting (Brewer et al. 2008).
Data sources
Multiple searches were conducted using the CINAHL, Medline and PubMed databases producing an international dataset of literature from 1985 to 2009. Because the term ‘surveillance’ has many meanings in both colloquial and medical research language, an initial search began using the heading terms ‘Surveillance (Iowa NIC)’ and ‘Surveillance (Omaha)’. By limiting the search to these subject headers, research with other uses of the term, such as disease and infection control surveillance, was avoided. From these searches, a focused analysis of references and major and minor subject headings were used to obtain additional search criteria and relevant sources. All relevant abstract and titles were reviewed and literature that specifically used the concept of surveillance as an active process in relation to nursing and nursing care was included. Dissertation abstracts and symposia conference proceedings were excluded. The final sample of relevant literature consisted of 18 papers and 4 book chapters for analysis.
Results
Related concepts
The work of nursing has been described through terms like observing, assessing and monitoring; however, these terms fail to capture the complex and autonomous nature of today’s evolved nursing role. Dougherty (1999) describes how observing and assessment are different from surveillance. Observing is a passive process and does not include evaluation of collected data. Assessment describes the collection and evaluation of data, but only at a single point in time, and focuses solely on patient data, excluding any family or other important data sources. Monitoring has been described as similar to surveillance in that it describes the mental or unseen work of nurses by including evaluation and analysis functions conducted by nurses (Dougherty 1999). However, it does not incorporate the analytic and decision-making skills involved in nursing surveillance.
As an example, consider a nurse who is taking a patient’s vital signs. Observing and assessing the vital signs would involve capturing and recording the information, noting abnormalities or changes. These terms have typically been used to capture the single act and physical process involved with the task and not the continuous process, mental work or associated care involved. Monitoring better describes the evaluation component of the process where the nurse compares the vital signs against the patient’s previous vital signs and evaluates for any trends or patterns. What is most unique about the term surveillance is that it captures the application of both the cognitive and behavioural processes, to demonstrate nurse’s early recognition and identification of emerging indicators of changes in the patient’s status (Dougherty 1999, Kutney-Lee et al. 2009). In this example, the nurse is performing surveillance by not only assessing and comparing previous vital sign values but also by interpreting current data in the context of other known variables, such as medications administered, and then makes a decision on whether or not to initiate a change in the plan of care.
The terms vigilance and attentiveness are also used to describe the care and emphasis nurses place on detection and prevention of errors for the purpose of patient safety (Meyer & Lavin 2005, Bitz et al. 2009). Through vigilance, a nurse attaches meaning to collected data and is able to inform actions that result from proper vigilance. Attentiveness attaches a responsibility in the nurse’s role to the patient’s safety (i.e. the nurse is being attentive to changes in the patient’s status). The accountability and responsibility associated with attentiveness describes how nursing care moves beyond task oriented care to legal, ethical and moral obligations associated with their role as a nurse (Bitz et al. 2009). In some instances, surveillance and attentiveness are used interchangeably. For example, ‘a major threat to attentiveness and surveillance for all health care workers is sleep deprivation and fatigue’ (Bitz et al. 2009, p. 59). On the other hand, attentiveness and vigilance are more frequently described as components of practice that inform the surveillance process through recognizing patient problems, having awareness of potential danger, and being ready and able to respond to changes in the patient’s status (Meyer & Lavin 2005, Bitz et al. 2009). While this describes many of the cognitive processes, the term surveillance seeks to encompass the behavioural components as well.
Attributes
Distinguishing the attributes of a concept involves identifying a cluster of characteristics that define the concept (Rodgers 2000). The first set of attributes has to do with how the concept is used in the acute care setting. Although surveillance has many different meanings in healthcare, surveillance in the acute care setting is described as an active process with an action component of actively keeping patients safe. This process is described through the behavioural component of applying surveillance (Dougherty 1999); however, little research has further examined the elements or operationalization of this process. Surveillance is also described as an action or set of activities in its use as an intervention label or intervention scheme in classification systems. These categorizations are used in standardized languages to guide nursing practice documentation and description. As an intervention, surveillance is identified in four classification systems (Nursing Intervention Classification, Omaha System, Perioperative Nursing Data Set, and Public Health Intervention Model) as related to a specific diagnosis or phenomenon of concern (Martin et al. 1993, Schoneman 2002, Dochterman et al. 2005). The International Classification for Nursing Practice uses the term surveying as an intervention label in conjunction with monitoring and observing, noting that surveying is a type of monitoring and monitoring is a type of observing (Schoneman 2002). The action terms provide usefulness in documentation; however, the limited description often fails to explain the full extent of the surveillance process.
Another set of attributes related to surveillance was associated with the timing and frequency of how the process is used. Nursing in the acute care setting is unique in that it is a 24-hour a day service provided to patients, meaning that surveillance is frequent and ongoing for the patient (Dougherty 1999, Clarke & Aiken 2003, Dochterman et al. 2005, Zeitz 2005, Forster et al. 2006). While the nurse is not continuously present with the patient, surveillance describes activities nurses use to monitor the clinical patient’s status (Rubenstein et al. 1992). To effectively conduct surveillance, data collection is required from multiple sources and cumulatively across nurses and time (Dougherty 1999, Kutney-Lee et al. 2009). In a systems perspective view of an acute care work environment, patient outcomes are collectively influenced by multiple factors. For example, increased nursing workload might affect the frequency with which the nurse can physically visit the patient, potentially influencing patient outcomes. Analysing the frequency and timing associated with surveillance must account for contextual system influences that can affect both the surveillance process and outcomes.
Nursing surveillance is known to consist of behavioural and cognitive components; however, recent literature broadens the surveillance concept to describe its multifaceted nature. The behavioural process is associated with attributes of systematic data collection and data gathering activities that are conducted through a variety of actions. These activities are incorporated into the nursing actions of assessing, diagnosing, intervening and evaluating (Meyer et al. 2007). Nurses study, interpret and analyse data for indicators of factors that might influence a situation or cues to a change in patient status (Dougherty 1999, Dochterman et al. 2005). In addition to the physical component, nurses effectively use multiple cognitive processes during surveillance to ‘digest’ collected information to recognize subtle changes or early warning signs (Aiken et al. 2003, Clarke & Aiken 2003, Institute of Medicine 2004). The cognitive processes used to describe surveillance include applying clinical judgment (Aiken et al. 2003, Meyer et al. 2007) and decision-making (Dochterman et al. 2005, Kutney-Lee et al. 2009). These processes are the ‘mental work’ of nursing that is required of today’s evolving nursing role. These components explain how nurses use the surveillance process to systematically collect information to make judgments and predictions about a patient’s health status.
Antecedents
Walker and Avant (2005) warn that antecedents should not be dealt with lightly, as they have considerable context implications for the concept’s use. This holds true when analysing nursing surveillance where antecedents were categorized into either RN antecedents (prepossessed abilities, knowledge, or training that the RN holds that influences the concept) or Work Environment antecedents (contextual influences of the practice environment that influence the concept). Arguably, the most influential nurse antecedent seen in the literature is nursing expertise (Clarke & Aiken 2003, Clarke 2004, Manojlovich & Talsma 2007, Kutney-Lee et al. 2009). Clinically expert nurses are identified by their ability to see the situation as a whole or realize the ‘big picture’, whereas novice nurses view processes as linear and do not recognize patterns (Brykczynski 1998, Meretoja et al. 2002, Orsolini-Hain&Malone 2007). To practice holistically, expert nurses use pattern recognition to distinguish problems and intervene appropriately (Orsolini-Hain & Malone 2007). Expertise in nursing is a subjective combination of knowledge and experience (Baker et al. 2006). Therefore, expertise is not only attained by having more years of experience but by knowledge enhancement. Additionally, knowledge alone is not sufficient to define expertise, but experience can enhance knowledge.
Dougherty (1999) described the importance of the nurse’s ability to ‘relate sensory stimuli to a knowledge base or to a previous experience’ (p. 526) as critical to the surveillance process. This form of intuitive knowledge is often described as a ‘gut feeling’, by nurses who are actually using experience and knowledge for the purpose of decision-making (Hansten & Washburn 2000, Smith 2007). Intuition is linked to perception and judgment, relying not only on the presence of stimuli but also on the ability to perceive and integrate the stimuli, giving it meaning from past experience or knowledge (Effken 2001). This process involves using knowledge, experience and clinical data about the given context to generate opinions and make judgments, whether logic and evidence support the decision or not. As an antecedent of surveillance, intuition is associated with the nurse’s recognition of a complication or downward turn in the patient’s status, whether or not clinical data indicates the turn in the patient’s status. Nurses describe a fear or anxiety for the patient’s health and a heightened sense of awareness to understand the patient’s condition to detect changes (Minnick & Harvey 2003). Intuitive feelings and surveillance have the same purpose of identifying threats to the patient and deciding to take action. Nurses identify patterns in collected data, often seeking more information when their intuition seeks to confirm a feeling (Leners 1992).
If the goal of nursing surveillance is to detect a downturn or complication in the patient’s health status, a major antecedent for the nurse is the ability to recognize that downturn or complication early. Early recognition skills describes the ability to recognize ‘ominous events early and take corrective action,…[to] prevent further decline in a patient’s status and increase the likelihood of a positive health outcome’ (Minnick & Harvey 2003, p. 291). Nurses with these skills use a decision-making process that applies clinical judgment and intuitive knowledge when subtle changes and variations are identified. Enhanced by expertise, this process aligns with what has been described as nurse’s ability to future think, or the ability to think about the patient’s situation to anticipate potential problems and solutions (Benner 2001).
Additional nurse antecedents have been identified but the research association with surveillance is limited. These include nurse’s level of education (Aiken et al. 2003, Batcheller et al. 2004, Kutney-Lee et al. 2009), fatigue (Manojlovich & Talsma 2007), competency (Institute of Medicine 2004) and the ability to take action and mobilize resources (Clarke & Aiken 2003). In the surveillance process, nurses are described as the ‘frontline of patient defense…[ and] key instruments for carrying out such vigilance in health care’ (Institute of Medicine 2004, p. 35). It is important that the significance of the nurses’ attributes in the role of surveillance is not overlooked.
In addition to RN antecedents, the work environment plays a large role in refining the defining attributes of surveillance. Antecedents of the work environment include staffing adequacy, skill mix, work load and practice environment. As staffing ratios have been linked with outcomes, the effects of nurse surveillance are also enhanced when more nurses are available to conduct the process (Aiken et al. 2003, Batcheller et al. 2004, Kalisch 2006, Manojlovich & Talsma 2007, Kutney-Lee et al. 2009). In the same regard, skill mix has an effect on surveillance (Aiken et al. 2003). While not as specifically delineated, the work environment has been negatively associated with the surveillance process through heavy workloads, constrained resources, inadequate nurse–physician relationships, and lack of proximity to patients being cared for (Clarke 2004, Kalisch 2006, Kutney-Lee et al. 2009). From a systems perspective, the effects of staffing, skill mix and the work environment are often seen as a collective effort at the unit level, which should be taken into consideration when evaluating surveillance. While surveillance is conceptually discussed as the individual care provided by the nurse to the patient, in the acute care environment patient care is the product of multiple nurses over time and is influenced by contextual factors. These issues must be evaluated when considering the antecedents of the work environment to nursing surveillance. Nurses prepossessed abilities, knowledge and training in conjunction with the healthcare work environment have potential to enhance the surveillance process by refining defining attributes and creating contexts where surveillance is optimized.
Consequences
Consequences associated with nursing surveillance were positive in association when adequate surveillance occurred and the negative consequence was avoided. Inadequate or a lack of surveillance is often associated with failure-to-rescue (Clarke 2004, Institute of Medicine 2004, Manojlovich & Talsma 2007, Kutney-Lee et al. 2009), defined as the inability to save a hospitalized patient’s life after the occurrence of an adverse event (Clarke & Aiken 2003). As a quality indicator, failure-to-rescue has been linked with nursing care quality with the notion that surveillance is the phase that precedes a failure-to-rescue event (Clarke 2004, Manojlovich & Talsma 2007). Multiple studies report the prevention and avoidance of a ‘rescue’ situation as the ultimate goal of the surveillance process, including avoiding harm, decreasing adverse events, optimizing health outcomes and increasing chances of positive patient outcomes (Dougherty 1999, Schoneman 2002, Batcheller et al. 2004, Manojlovich & Talsma 2007). However, nursing processes and research are often analysed by their absence or the effects of poor outcomes (Clarke 2004). On that note, negative consequences are more frequent in the literature and associated with inadequate or lack of surveillance. These include increased adverse events, the need for rescue when a complication occurs, increased life-threatening conditions and higher mortality rates (Dougherty 1999, Clarke & Aiken 2003, Institute of Medicine 2004, Kalisch 2006, Kutney-Lee et al. 2009). There has also been an association between cost and the amount of surveillance. When a high compared to low level of surveillance was delivered, costs per patient hospitalization increased. However, the benefits of increasing surveillance ultimately resulted in cost savings through avoidance of adverse events (Shever et al. 2008). A summary of the related concepts, attributes, antecedents and consequences of nursing surveillance is given in Table 1.
Table 1.
Summary of analysis of nursing surveillance in the acute care setting
| Attributes | Antecedents | Consequences | Related concepts |
|---|---|---|---|
| Process | RN: | Positive: | Observing |
| Application of behavioural and cognitive processes | Expertise Intuition | Prevention of failure-to-rescue | Assessment Monitoring |
| Intervention Continuous/frequent | Early recognition skills | Decrease in adverse events | Vigilance Attentiveness |
| Data collection | Work environment: | Negative: | |
| Data digestion | Staffing adequacy | Adverse events | |
| Skill mix | Failure-to-rescue | ||
| Work/patient load | Death | ||
| Practice environment |
Theoretical definition of nursing surveillance
In the acute care setting, nursing surveillance is a process to primarily identify threats to patient health and safety through purposeful and ongoing acquisition, interpretation and synthesis of patient data for clinical decision-making. In addition to the physical activities associated with providing nursing care, nurses use their expertise, intuition and early recognition skills to identify changes in the patient’s status and decide when to act upon their judgments. The surveillance process is influenced by characteristics of the nurses, such as education, and the context of work environment, such as staffing. In general, outcomes are directly related to surveillance (e.g. better surveillance constitutes better outcomes and vice versa). This definition clarifies the breadth and multifaceted nature of nursing surveillance. In addition, this definition identifies surveillance as an antecedent to outcomes for the purpose of identifying threats to patient safety. Finally, this definition identifies the specific environment for which this analysis is examining nursing surveillance.
Discussion
Study limitations
This analysis is limited in its scope to acute care nursing and the systems perspective. In addition, the data sources only included published, peer reviewed literature.
Implications
The purpose of this concept analysis was to examine nursing surveillance in the acute care environment to describe and develop its dimensions. Rodger’s framework was chosen to describe the concept in a specific setting and context, using a dynamic process to recognize shared meaning in concepts; however, this analysis was narrowed by using a systems framework to limit the concept from its other colloquial uses and give meaning to the concept in theory. Although this approach limits the concept to a specific setting and population in nursing, the generalizability of these results are universal to acute care nursing, providing international relevance for the use of surveillance.
The SROM is the foundational framework from which systems research and the relationship between the concepts can be propositioned, allowing for theory to incorporate system influences in explaining outcomes. Using the SROM framework has the potential to enhance the understanding of outcomes by examining nursing surveillance in relation to its system influences, rather than in isolation. Derived constructs in the SROM model would include patient characteristics, unit or hospital characteristics and outcomes (Clarke & Aiken 2003, Kutney-Lee et al. 2009). As an action focus, nursing surveillance is an antecedent to outcomes, influenced by both patient outcomes and hospital characteristics, which includes organizational features. The structure of this model demonstrates how surveillance can not only contribute to patient outcomes, but also the relationship and influence of hospital and environmental factors on surveillance.
The SROM also identifies relationships between concepts. The QHOM model has reciprocal relationships that recognize feedback between some but not all of the concepts (Mitchell et al. 1998). The SROM extends these relationships further by linking all of the concepts, including the intervention/ action focus and outcomes, directly (Brewer et al. 2008). The reciprocal relationships in the model support interactions, interdependence, and feedback between nursing, the environment and outcomes. For example, consider the outcome failure-to-rescue. When such an event occurs in an acute care environment, the outcome is affected not only by the nurse’s surveillance but also by contextual influence, patient characteristics and the interactions between them as demonstrated in Figure 1. It could be hypothesized that with adequate surveillance a failure-to-rescue event could be prevented.
While traditional concept analyses attempt to build theory, the goal of this analysis was to give meaning to the concept in context, allowing for competing interpretations of theory. Rather than adopting a single theory to describe the surveillance process, clarifying the concept of surveillance in a contextual systems framework will help describe its fit so that it can be adopted into theory. Even with clarification, there is the possibility that the concept will be adopted into another theory that conflicts with previous uses of the term (Paley 1996). Using the defined framework, the theories can then be tested in the conceptual model to allow for conceptual clarification.
Conclusion
Developing the concept of nursing surveillance has implications at both the individual and organizational level. So far, studies have only examined the effects or influence of surveillance on outcomes and organizational characteristics (Aiken et al. 2003, Shever et al. 2008, Kutney-Lee et al. 2009). This review clarifies the concept of surveillance in the acute care setting, recognizing the complex and multifaceted nature of surveillance to lay a foundation for operationalizing the concept in research and studying and developing the concept for practice.
Analysing surveillance can give insight for direct care nurses, educators and administrators. Nurses in practice must recognize the combination of behavioural and cognitive processes involved in surveillance. Task oriented care and cognitive processing time are not two mutually exclusive processes and nurses should be aware of intuitive feelings or early recognition signs that come as a result of surveillance activity. In addition, debriefing, or reflecting on near misses, can help identify activities that guide early recognition or decision-making. Educators and administrators can enhance these skills in both classroom and postgraduate education and training through activities designed to increase awareness and advance these skills. For example, debriefing rapid response situations can help describe the surveillance process, including activities and decisions that preceded the event, possibly enhancing early recognition skills and intuitive thinking through discussion and awareness.
This concept analysis has provided insight into the definition and breadth of surveillance based on literature. This article is meant to provide a clearer understanding of nursing surveillance by describing its multifaceted nature and the purpose of nursing surveillance in the acute care setting. As research continues in the health services arena about outcomes and nursing’s contribution, surveillance should be communicated more effectively to develop and operationalize the concept. The SROM conceptual framework can be used to guide the examination of surveillance and outcomes. From a systems perspective, structure and organization are influential forces on the process and outcomes of patient care. Furthermore, the nursing work environment and organizational characteristics create a social context from which nursing processes and outcomes are influenced in a way that requires careful consideration where measurement is concerned. This analysis has hopefully provided clarification of the surveillance process and the influential effects of the system context.
What is already known about this topic
Nursing surveillance, which is critical to maintaining patient safety in the acute care setting, is often described in simpler terms, such as observation or monitoring.
Previous definitions of nursing surveillance include the application of cognitive and behavioural processes, without further discussion of the breadth or nature of these components.
While the concept of nursing surveillance is increasingly being used, it is not well defined or communicated effectively, limiting its role in research and its ability to be studied and developed.
What this paper adds
Attributes of surveillance demonstrate that it is a continuous and ongoing process in the acute care setting that is conducted both individually and cumulatively across nurses for the purpose of patient safety.
Surveillance extends beyond monitoring by describing the ability of the nurse to study, interpret, analyse and act upon data, including subtle changes and cues from the patient.
Antecedents to surveillance are characteristics of the nurse, such as level of expertise and early recognition skills, and components of the work environment, such as staffing levels. Consequences frequently occur with an inadequate or lack of surveillance and include adverse events, failure-to-rescue, or death.
Implications for practice and/or policy
Clarifying the concept of surveillance in a systems theoretical framework creates a context to operationalize surveillance for research. Continued research using the surveillance concept in health services research should increase knowledge and awareness about the complex role of the acute care nurse.
Nurses can analyse their capacity to conduct surveillance by debriefing on events, such as rapid response calls or ‘near-misses’, and discussing the associated task and thought processes that were taking place during those events.
Educators and administrators can be aware of and optimize staffing and work environment characteristics to enhance surveillance.
Acknowledgments
Funding
This study was supported by funding from the National Institute for Nursing Research, National Institutes of Health – Advanced Training in Nursing Outcomes Research (T32-NR-007104, Aiken, PI).
Footnotes
Conflict of interest
No conflict of interest has been declared by the authors.
Author contributions
LK and DV were responsible for the study conception and design. LK performed the data collection. LK and DV performed the data analysis. LK was responsible for the drafting of the manuscript. LK and DV made critical revisions to the paper for important intellectual content. DV provided administrative, technical or material support. DV supervised the study.
Contributor Information
Lesly Kelly, Center for Health Outcomes and Policy, Research, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Deborah Vincent, College of Nursing, University of Arizona, Tucson, Arizona, USA.
References
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational level of hospital nurses and surgical patient mortality. Journal of the American Medical Association. 2003;290(12):1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AORN. Perioperative Nursing Data Set: The Perioperative Nursing Vocabulary. 2. Association of Operating Room Nurses; Denver, CO: 2007. [DOI] [PubMed] [Google Scholar]
- Baker JA, Lovell K, Harris N. How expert are the experts? An exploration of ‘expert’ within Delphi panel techniques. Nurse Researcher. 2006;14(1):59–70. doi: 10.7748/nr2006.10.14.1.59.c6010. [DOI] [PubMed] [Google Scholar]
- Batcheller J, Burkman K, Armstrong D, Chappell C, Carelock JL. A practice model for patient safety: the value of the experienced registered nurse. Journal of Nursing Administration. 2004;34(4):200–205. doi: 10.1097/00005110-200404000-00008. [DOI] [PubMed] [Google Scholar]
- Benner P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice. Prentice Hall; Upper Saddle River, NJ: 2001. Commemorative edn. [Google Scholar]
- Bitz K, Goettsche V, Benner P. Practice breakdown: attentiveness/surveillance. In: Benner PE, Malloch K, Sheets V, editors. Nursing Pathways for Patient Safety. Mosby Elsevier; St Louis, MO: 2009. pp. 58–75. [Google Scholar]
- Brewer BB, Verran JA, Stichler JF. The systems research organizing model: a conceptual perspective for facilities design. Health Environments Research and Design. 2008;1(4):7–19. doi: 10.1177/193758670800100402. [DOI] [PubMed] [Google Scholar]
- Brykczynski KA. Clinical exemplars describing expert staff nursing practices. Journal of Nursing Management. 1998;6:351–359. doi: 10.1046/j.1365-2834.1998.00088.x. [DOI] [PubMed] [Google Scholar]
- Bulechek GM, Butcher HK, Dochterman JM. Nursing Intervention Classification (NIC) System. 5. Mosby; St Louis, MO: 2008. [Google Scholar]
- Chizek JD. Report for Congress No RL31425. Congressional Research Service; The Library of Congress: 2003. Military Transformation: Intelligence, Surveillance and Reconnaissance. [Google Scholar]
- Clarke SP. Failure to rescue: lessons from missed opportunity in care. Nursing Inquiry. 2004;11(2):67–71. doi: 10.1111/j.1440-1800.2004.00210.x. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Aiken LH. Failure to rescue. American Journal of Nursing. 2003;103:42–47. doi: 10.1097/00000446-200301000-00020. [DOI] [PubMed] [Google Scholar]
- Dochterman J, Titler M, Wang J, Reed D, Pettit D, Mathew-Wilson M, Budreau G, Bulechek G, Kraus V, Kanak M. Describing use of nursing interventions for three groups of patients. Journal of Nursing Scholarship. 2005;37(1):57–66. doi: 10.1111/j.1547-5069.2005.00003.x. [DOI] [PubMed] [Google Scholar]
- Dougherty DM. Surveillance. In: Bulechek GM, McCloskey JC, editors. Nursing Interventions: Effective Nursing Treatments. 2. Saunders; Philadelphia, PA: 1985. p. 301. [Google Scholar]
- Dougherty DM. Surveillance. In: Bulechek GM, McCloskey JC, editors. Nursing Interventions: Effective Nursing Treatments. 3. Saunders; Philadelphia, PA: 1999. pp. 524–532. [Google Scholar]
- Effken J. Informational basis for expert intuition. Journal of Advanced Nursing. 2001;34(2):246–255. doi: 10.1046/j.1365-2648.2001.01751.x. [DOI] [PubMed] [Google Scholar]
- Fawcett J. Contemporary Nursing Knowledge: Analysis and Evaluation of Nursing Models and Theories. 2. F.A. Davis; Philadelphia, PA: 2005. [Google Scholar]
- Forster AJ, Fung I, Caughey S, Oppenheimer L, Beach C, Shojania KG, van Walraven C. Adverse events detected by clinical surveillance on an obstetric service. Obstetrics & Gynecology. 2006;108(5):1073–1083. doi: 10.1097/01.AOG.0000242565.28432.7c. [DOI] [PubMed] [Google Scholar]
- Hansten R, Washburn M. Intuition in professional practice: executive and staff perceptions. Journal of Nursing Administration. 2000;30(4):185–189. doi: 10.1097/00005110-200004000-00009. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Keeping Patients Safe: Transforming the Work Environment. The National Academy Press; Washington, DC: 2004. [Google Scholar]
- Kalisch BJ. Missed nursing care: a qualitative study. Journal of Nursing Care and Quality. 2006;21(4):306–313. doi: 10.1097/00001786-200610000-00006. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Lake ET, Aiken LH. Development of the hospital nurse surveillance capacity profile. Research in Nursing & Health. 2009;32:217–228. doi: 10.1002/nur.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leners DW. Intuition in nursing practice: deep connections. Journal of Holistic Nursing. 1992;10(2):137–153. doi: 10.1177/089801019201000205. [DOI] [PubMed] [Google Scholar]
- Manojlovich M, Talsma A. Identifying nursing processes to reduce failure to rescue. Journal of Nursing Administration. 2007;37(11):504–509. doi: 10.1097/01.NNA.0000295608.94699.3f. [DOI] [PubMed] [Google Scholar]
- Martin KS, Scheet NJ, Stegman MR. Home health clients: characteristics, outcomes of care, and nursing interventions. American Journal of Public Health. 1993;83(12):1730–1734. doi: 10.2105/ajph.83.12.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey JC, Bulechek GM, editors. Nursing Interventions Classification. 3. Mosby; St Louis, MO: 2000. [Google Scholar]
- Meretoja R, Eriksson E, Leino-Kilpi H. Indicators for competent nursing practice. Journal of Nursing Management. 2002;10:95–102. doi: 10.1046/j.0966-0429.2001.00299.x. [DOI] [PubMed] [Google Scholar]
- Meyer G, Lavin MA. Vigilance: the essence of nursing. Online Journal of Issues in Nursing, [Online] 2005;10(1) Retrieved from http://www.nursingworld.org/MainMenuCategories/ANA-Marketplace/ANAPeriodicals/OJIN/TableofContents/Volume102005/No3Sept05/ArticlePreviousTopic/VigilanceTheEssenceofNursing.aspx on 26 October 2009. [PubMed]
- Meyer G, Lavin MA, Perry A. Is it time for a new category of nursing diagnosis? International Journal of Nursing Terminologies and Classifications. 2007;18(2):45–50. doi: 10.1111/j.1744-618X.2007.00049.x. [DOI] [PubMed] [Google Scholar]
- Minnick P, Harvey S. The early recognition of patient problems among medical-surgical nurses. Medsurg Nursing. 2003;12(5):291–297. [PubMed] [Google Scholar]
- Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. Image Journal of Nursing Scholarship. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. [DOI] [PubMed] [Google Scholar]
- Orsolini-Hain L, Malone RE. Examining the impending gap in clinical nursing expertise. Policy, Politics & Nursing Practice. 2007;8(3):158–169. doi: 10.1177/1527154407309050. [DOI] [PubMed] [Google Scholar]
- Paley J. How not to clarify concepts. Journal of Advanced Nursing. 1996;24:572–578. doi: 10.1046/j.1365-2648.1996.22618.x. [DOI] [PubMed] [Google Scholar]
- Rodgers BL. Concept analysis: an evolutionary view. In: Rodgers BL, Knafl KA, editors. Concept Development in Nursing: Foundations, Techniques and Applications. 2. Saunders; Philadelphia, PA: 2000. pp. 77–117. [Google Scholar]
- Rubenstein LV, Chang BL, Keeler EB, Kahn KL. Measuring the quality of nursing surveillance activities for five diseases before and after implementation of the DRG-based prospective payment system. Patient Outcomes Research: Examining the Effectiveness of Nursing Practice; Proceedings of the State of the Science Conference; September 11–13; Rockville: United States Department of Health and Human Services Public Health Service; 1992. pp. 39–53. [Google Scholar]
- Schoneman D. The intervention of surveillance across classification systems. International Journal of Nursing Terminologies and Classifications. 2002;13(4):137–147. doi: 10.1111/j.1744-618x.2002.tb00417.x. [DOI] [PubMed] [Google Scholar]
- Shever LL, Titler MG, Kerr P, Qin R, Kim T, Picone DM. The effect of high nursing surveillance on hospital costs. Journal of Nursing Scholarship. 2008;40(2):161–169. doi: 10.1111/j.1547-5069.2008.00221.x. [DOI] [PubMed] [Google Scholar]
- Smith A. Measuring the use of intuition by registered nurses in clinical practice. Nursing Standard. 2007;21(47):35–41. doi: 10.7748/ns2007.08.21.47.35.c4591. [DOI] [PubMed] [Google Scholar]
- Thacker SB, Berkelman RL, Stroup DF. The science of public health surveillance. Journal of Public Health Policy. 1989;10(2):187–203. [PubMed] [Google Scholar]
- Titler MG. Interventions related to surveillance. Nursing Clinics of Nurse America. 1992;27(2):495–502. [PubMed] [Google Scholar]
- Treverton GF. Reshaping National Intelligence for an Age of Information. Cambridge University Press; Cambridge, MA: 2001. [Google Scholar]
- Walker LO, Avant KC. Strategies for Theory Construction in Nursing. 4. Pearson Prentice Hall; Upper Saddle River, NJ: 2005. [Google Scholar]
- Zeitz K. Nursing observations during the first 24 hours after a surgical procedure: what do we do? Journal of Clinical Nursing. 2005;14:334–343. doi: 10.1111/j.1365-2702.2004.01071.x. [DOI] [PubMed] [Google Scholar]