Abstract
Background
Although direct medical costs for constipation related medical visits are thought to be high, to date there have been no studies examining longitudinal resource utilization in adults with constipation.
Aim
To estimate the incremental direct medical costs associated with constipation in women.
Methods
This is a nested case-control study. The study population consisted of all mothers of 5,718 children in the population-based birth cohort born during 1976-1982 in a community. The cases presented to the medical facilities with constipation. The controls were randomly selected and matched to cases in a 2:1 ratio. Direct medical costs for constipated women and controls were collected for the years 1987-2002.
Results
We identified 168 women with a diagnosis of constipation. The total direct medical costs over a 15-year period for constipated subjects were more than double those of controls ($63,591 [95%CI: 49,786- 81,396]) vs. $24,529 [95%CI: 20,667-29,260]). The overall outpatient costs for constipated women were $38,897 (95% CI: 31,381-48,253) compared to $15,110 (95% CI: 12,904-17,781) for controls. The median annual outpatient visits for constipated women was 0.16 compared to 0.11 for controls.
Conclusion
Women with constipation have significantly higher medical care utilization and expenditures compared to women without constipation.
Keywords: chronic constipation, direct costs, case-control study
Introduction
Constipation is a chronic and common disorder, which presents as difficult, infrequent stool passage or a feeling of incomplete evacuation.1-3 The prevalence of constipation from population-based studies in North America has been estimated to be as high as 27% in adults, depending on definition, demographic factors, and sampling.1-7 In a systemic review of the burden of digestive diseases in the United States (U.S.) using a national database in 2004,8 Everhart et al. showed that constipation was the second most common ambulatory care diagnosis (6.3 million visits) among digestive diseases, after gastroesophageal reflux disease.
The evidence suggests that many patients have constipation-associated symptoms on a long-term basis.9, 10 Johanson and Kralstein9 reported that about 70% patients had constipation for more than two years using the web-based survey of the Knowledge Networks Panel. Talley et al.10 determined that in the general population, 89% of adults surveyed reported no change in their gastrointestinal symptoms during an intervening 12-20 month period. Thus, constipated subjects may present repeatedly for constipation over a prolonged period of time, which would likely contribute to an increased number of outpatient visits, diagnostic evaluations, and inpatient admissions. Although direct medical costs for constipation-related medical visits are thought to be high, to date there is no study examining longitudinal resource utilization in adults with constipation. The majority of studies, in fact, have relied on cross sectional medical costs for constipation.8, 11, 12 Sonnenberg et al.12 estimated that visits for constipation resulted in costs of $29 million (1985 value) for ambulatory visits. In a recent review,8 Everhart et al. estimated that in the U.S., the direct cost for constipation was $1.6 billion in 2004 (using the Verispan database).
In order to accurately estimate the longitudinal medical costs of a particular disease or disorder, a large well-defined cohort with a long duration of follow up as well as direct data on the medical costs is required. However, many longitudinal cohorts including the Framingham Heart Study13 and Nurses' Health Study14 do not have information on medical resource utilization or economic costs. The Rochester Epidemiology Project (REP) has captured all diagnoses and procedures of residents in a local community since 1966.15, 16 Using the REP, we created a birth cohort17-19 which consisted of all children born from 1976 and 1982 to mothers who were residents of the community; we have previously reported that the incidence of constipation in children in this birth cohort was 3.9 per 1000 person-years, and children with constipation at an early age repeatedly presented for medical visits due to constipation.19 The aim of the present study was to estimate incremental direct medical costs and type of health care associated with constipation in women over a prolonged period of time in a community.
Methods
Setting
Olmsted County, Minnesota, is a metropolitan and rural area 90 miles southeast of Minneapolis, Minnesota. Census data from the 1990 population, representing the years the children from this birth cohort were in school, indicated the population was 70,745 (75% were age <45 years), and estimated to be 96% Caucasian; sociodemographically, the community is similar to the U.S. Caucasian population.15, 16 Over 95% of county residents receive their medical care from one of the two group practices in the community (Mayo Clinic and Olmsted Medical Center). Mayo Clinic has maintained a common medical record system with its two affiliated hospitals (Saint Marys and Rochester Methodist) for over 90 years.15, 16 Recorded diagnoses and surgical procedures are indexed, including the diagnoses made for outpatients seen in office or clinic consultations, emergency room visits or nursing home care, as well as the diagnoses recorded for hospital inpatients, at autopsy examination or on death certificates. This system was further developed by the REP, which created similar indices for the records of other providers of medical care to local residents, most notably the Olmsted Medical Group and its affiliated Olmsted Community Hospital. Thus, details of the medical care provided to the residents of Olmsted County are available for study. Annually, over 80% of the entire population is attended by one or both of these two practices, and nearly everyone is seen at least once during any given three-year period.15 Therefore, the REP medical records linkage system also provides what is essentially an enumeration of the population from which samples can be drawn.
Study subjects from the 1976-1982 Rochester Birth Cohort
A cohort of all women who were residents of Rochester, Minnesota and who had children born between January 1, 1976 and December 31, 1982, was utilized. As approved by the Institutional Review Boards of the Mayo Clinic and Olmsted Medical Center, we used this system previously to draw the birth cohort which consisted of all children born between 1976 and 1982, to mothers residing in Olmsted County, Minnesota, comprising the Minnesota Independent School District 535 (n= 8548) in the city of Rochester.17-19 Subjects were identified through computerized birth certificate information from the Minnesota Department of Health, Division of Vital Statistics. The target population for this study consisted of 4075 women, not actively denying research authorization, whose children at or after the age of 5 years all still lived in Rochester. The women's length of follow-up was confirmed utilizing the REP.
Identification of cases with constipation
Through the REP, all diagnoses and surgical procedures recorded at Rochester medical facilities are indexed continuously for automated retrieval. This diagnostic index expedites retrieval of the unit (or dossier) medical record, which includes the history of all encounters in the hospital, community and ambulatory medical and social services, emergency department, outpatient clinics, and home visits, as well as laboratory and psychologic test results from birth until patients no longer reside within the community.
Case and control ascertainment
Constipation Cases
The cases included mothers who presented to Olmsted County medical facilities with constipation from the birth cohort. All mothers diagnosed with constipation were identified by using the diagnostic index developed by the REP. The constipation cases were identified as having one or more of the following diagnostic or surgical codes: constipation, H-ICDA-8 (Hospital Adaptation of the International Classification of Diseases) 05640112 or ICD-9 564; obstipation, H-ICDA-8 05640111; constipation (functional), ICD-0 564.9. The diagnostic index was designed to be sensitive and thus this search should capture all clinically diagnosed cases.
Controls
For each identified and reviewed case, we randomly selected two age-matched controls from the pool of mothers in the birth cohort who did not meet the constipation definition; that is, did not have one of the relevant HICDA or ICD-9 diagnoses for constipation. Thus, the controls were matched to cases in a 2:1 ratio, matching on age and years of follow-up.
Cost and Utilization Data
Beginning in January 1987, resource use and associated charges data from Mayo Clinic and Olmsted Medical Center were collected. This claims-based database contains information on medical resource utilization, associated charges, and estimated economic costs for patients receiving care at either the Olmsted Medical Group or the Mayo Clinic and their associated inpatient facilities. The Olmsted County Healthcare Expenditure and Utilization Database (OCHEUD) provides a standardized inflation-adjusted estimate of costs for each service or procedure provided locally in constant dollars. Specifically, using a “bottom-up” (also referred to as micro-costing) costing approach, OCHEUD groups resource utilization into the Medicare Part A and B classification system. Part A billed charges are adjusted by using hospital cost-to-charge ratios and Part B physician services are valued by using Medicare reimbursement rates.
Although the services provided represent the clinical practice patterns of Mayo Clinic and Olmsted Medical Center providers, the value of each unit of service has been adjusted to national norms by use of widely accepted valuation techniques.20 OCHEUD provides an estimated economic cost for each line item in the billing record and allows the aggregation of costs into categories deemed relevant to a particular study.20
Data collection
Techniques for data collection have been previously described.18, 19, 21 Detailed sociodemographic factors were collected at birth in the 1976-1982 birth cohort. To determine factors that may influence medical presentation for a condition, birth certificate information was evaluated.
For the selected comorbidities status in the cases and controls, comorbidities were defined as an occurrence of at least one diagnosis within the time frame of the study. The diagnostic or surgical codes (Table 1) were selected based on our a priori expectation that they could have an impact on constipation status and medical costs, and were prevalent in the population.
Table 1. Medical index for disease (ICD-9 codes).
| Disease | ICD-9 codes |
|---|---|
| GI disease | |
| GERD or heartburn | 530.1, 787.1 |
| Dyspepsia | 536.8 |
| Abdominal pain | 789.0 |
| Peptic ulcer disease | 533. x |
| Non GI disease | |
| Headache, tension or migraine | 784.0, 307.81, 346, 625.4, 784.0 |
| Thyroid disorder | 245, 240.9, 244.2 |
| Diabetes mellitus | 250.0 |
| Depression | 296.2×, 296.89, 298.0, 300.4, 311 |
| Back pain | 724.1, 724.2 |
| Limb pain | 729.5, 729.4, 729.5 |
| Anxiety | 300.00, 300.02, 300.09, 309.21 |
GERD=gastroesophageal reflux disease
Statistical Analyses
Descriptive statistics on baseline factors (e.g. age, gender, proportion of cesarean births, etc.) as well as sociodemographic factors are presented as means with standard deviations or frequencies with percentages. All categorical descriptive variables were compared using the Chi-square test statistic or Fisher's exact when appropriate. Continuous variables were compared using the Wilcoxon rank sum test. The unadjusted mean cost per year is presented for descriptive purposes only, as is the interquartile range and the range per patient per year for the entire time frame.
The effect of constipation on total costs during a given year on all women was assessed using two-part models to account for the zero values during a given year.22 For the two-part model specifications, logistic regression was used in part 1 to estimate the probability of costs conditional on patient characteristics; part 2 was employed with an inverse Gaussian distribution function with log link in cost models. Confidence intervals of estimated costs were generated by bootstrapping method.23 Three time frames were chosen and adjusted by comorbid conditions. The only comorbid conditions that were counted were those that had been found within the given year or previous to the year being analyzed.
The Tian and Huang24 method was used to assess the overall mean estimated costs. It is a two-part model for censored medical costs. The first part assumes a parametric model, in this case logistic regression for the probability of having a positive cost over 15 years with covariates. The second part uses a linear regression model for the positive costs. The censoring caused by incomplete follow up is addressed by applying the inverse probability weighting method to the two part model. This method allows for testing to see if a covariate has any effect on the total medical costs as well an estimation of the mean medical costs for individuals.
Similarly, this two-part model was employed to evaluate the predictors of costs within a multivariate model for those patients with constipation. Each comorbid condition that contained measurable counts was entered into the model predicting outpatient and total costs. For each variable entered into the model, an estimate of the percentage change in costs associated with each clinical characteristic is generated, contingent upon whether patients have positive costs. However, 4 (2.4%) patients did not have a positive value for total costs in the cohort, and 4 (2.4%) had no outpatient costs.
All calculated p-values were two-sided and p-values less than 0.05 were considered statistically significant. Statistical analyses was performed using SAS (SAS Institute, Cary, NC) and R - General (R Development core Team [2008)] software packages.25
Results
A total of 4075 women were eligible for this study. Among the women who did not deny research authorization, a total of 168 subjects with a medical diagnosis of constipation were identified. The mean age of cases when medical costs were first available was 33.2 years (± 5.7), and the mean age of controls was 33.2 years (± 5.7) (table 2).
Table 2. A comparison of sociodemographic characteristics for subjects with constipation versus controls.
| Cases N=168 | Controls N=336 | P-Value | |
|---|---|---|---|
| Age of women in 1987, Mean (± SD) | 33.2 (5.8) | 33.2 (5.7) | 0.9777 |
| Follow-up years, Mean (± SD) | 12.6 (2.5) | 12.4 (2.6) | 0.4079 |
| Non legitimate birth (out of wedlock) | 19 (11.3%) | 34 (10.1%) | 0.6813 |
| Less than 18 at time of birth | 6 (3.6%) | 13 (3.9%) | 0.8687 |
| Maternal education level at child's birth < High School | 15 (8.9%) | 19 (5.7%) | 0.1672 |
| Prenatal visits, Mean (± SD) | 11.4 (2.6) | 11.1 (2.9) | 0.2591 |
| Proportion of cesarean delivery | 14 (8.3%) | 36 (10.7%) | 0.3993 |
| Complication of Delivery | 64 (38.1%) | 138 (41.1%) | 0.5204 |
Table 2 summarizes the sociodemographic characteristics and comorbid conditions in constipated women and controls. There were no significant differences between sociodemographic comparisons such as education level, proportion with cesarean delivery, complications of delivery, legitimate births, or prenatal visits.
Medical visits and comorbid conditions
Annual medical visits and comorbid conditions of constipated women between 1987 and 2002 versus controls are summarized in Table 3. Cases used more of all types of medical services than their matched controls. Emergency department visits were the most frequently used type of services by constipated subjects, followed by outpatient care and inpatient care. In addition, more constipated women used hospital outpatient and inpatient care and the emergency department compared with controls. Notably, the mean annual number of emergency department visits for constipated women were 0.24 compared to 0.15 for controls (p<0.0001) (Table 3). Interestingly, 15.5 % of constipated subjects received no medical diagnosis for one of the selected comorbid conditions compared with 33.6% of the matched controls (p < .0001) (Table 3). Moreover, constipated women were more likely to present for co-morbid abdominal pain, as well as somatic and psychological conditions during the 15-year period.
Table 3. Proportion and Type of Co-morbid Medical Visits in Women with constipation or controls between 1987-2002.
| Cases N=168 | Controls N=336 | P-value | |
|---|---|---|---|
| # of non-users (1987-2002 Mayo) | 4 (2.4%) | 7 (2.1%) | 0.8293 |
| # of Patients with an Outpatient Visit(s) | 129 (76.8%) | 219 (65.2%) | 0.0079 |
| # of Patients with a Hospitalization(s) | 126 (75.0%) | 208 (61.9%) | 0.0034 |
| # of Patients with a ER Visit(s) | 138 (82.1%) | 233 (69.4%) | 0.0021 |
| Outpatient visits per patient per year, Mean (± SD) | 0.17 (0.39) | 0.12 (0.34) | <0.0001 |
| Inpatients stays per patient per year, Mean (± SD) | 0.13 (0.33) | 0.09 (0.28) | <0.0001 |
| ER Visits per patient per year, Mean (± SD) | 0.24 (0.43) | 0.15 (0.35) | <0.0001 |
| Comorbidities | 142 (84.5%) | 223 (66.4%) | <0.0001 |
| GI disease | 79 (47.0%) | 83 (24.7%) | <0.0001 |
| GERD or heartburn | 19 (11.3%) | 23 (6.9%) | 0.0874 |
| Dyspepsia | 14 (8.3%) | 20 (6.0%) | 0.3151 |
| Abdominal pain | 64 (38.1%) | 65 (19.4%) | <0.0001 |
| Peptic ulcer disease | 4 (2.4%) | 3 (0.9%) | 0.2291 |
| Non GI disease | 136 (81.0%) | 214 (63.7%) | <0.0001 |
| Headache, tension or migraine | 63 (37.5%) | 81 (24.1%) | 0.0017 |
| Thyroid disorder | 19 (8.3%) | 14 (5.7%) | 0.2518 |
| Diabetes mellitus | 5 (3.0%) | 12 (3.6%) | 0.7271 |
| Depression | 71 (42.3%) | 64 (19.1%) | <0.0001 |
| Back pain | 88 (52.4%) | 105 (31.3%) | <0.0001 |
| Limb pain | 97 (57.7%) | 116 (34.5%) | <0.0001 |
| Anxiety | 39 (23.2%) | 37 (11.0%) | 0.0003 |
GERD=Gastroesophageal reflux disease; ER=Emergency Room
Estimated direct medical costs and comorbid conditions
The medical costs over the entire time period for cases ($63,591 [95%CI: 49,786- 81,396]) were more than double those of controls ($24,529 [95%CI: 20,667-29,260]) for the total direct medical costs over 15-year period. The overall outpatient costs for constipated women were also more than double those of controls ($38,897 [95% CI: 31,381-48,253] vs. $15,110 [95% CI: 12,904-17,781]) (Table 4). Moreover, based on the mean total costs, the average costs per patient per year were higher than those of controls ($3,131 vs. $1,858, Table 4). Furthermore, the estimated average annual outpatient cost of cases was $1,791 compared to $964 for controls (Table 4).
Table 4. Estimated Costs of women with constipation versus controls.
| Cases N=168 | Controls N=336 | |
|---|---|---|
| Total Cost per Patient per Year1 | ||
| Mean | $3,130.76 | $1,858.34 |
| Q1-Q3 | (1038.87, 3726.77) | (490.83, 2186.12) |
| Range | (0, 44529.76) | (0, 37879.79) |
|
| ||
| Outpatient Cost per Patient per Year1 | ||
| Mean | $1,791.23 | $963.90 |
| Q1-Q3 | (788.94, 2254.25) | (364.41, 1140.20) |
| Range | (0, 27916.58) | (0, 12170.80) |
|
| ||
| Inpatient Cost per Patient per Year1 | ||
| Mean | $1,294.08 | $863.68 |
| Q1-Q3 | (0, 1527.71) | (0, 856.75) |
| Range | (0, 16369.97) | (0, 36861.19) |
|
| ||
| Estimated Total Costs (All years)2 | $63, 590.69 (49786.11, 81395.56) | $24,529.25 (20666.73, 29260.46) |
|
| ||
| Estimated Outpatient Costs (All years)2 | $38,897.27 (31380.72, 48253.02) | $15,109.52 (12904.16, 17780.99) |
|
| ||
| Estimated total cost at 1990, Mean (95% CI) 3, 4 | $2,162.88 (2094.59, 2239.16) | $1,765.47 (1727.72, 1810.25) |
|
| ||
| Estimated total cost at 1995 3, 4 | $3,545.55 (3295.75, 3821.43) | $1,550.43 (1476.22, 1630.85) |
|
| ||
| Estimated total cost at 20003, 4 | $3,171.02 (3008.95, 3350.69) | $1,718.39 (1652.93, 1784.48) |
Unadjusted Cost
Adjusted by Case vs. Control only.
Adjusting for case vs. control, abdominal pain, and back pain
CI calculating using bootstrap method
Figure 1 shows the total annual observed mean costs of constipated women and controls according to the year. Overall, cases consistently had higher health care costs between 1987 and 2002, even after adjusting for other comorbid conditions such as abdominal pain and back pain. Figure 2 shows the annual observed outpatient medical costs for constipated women and controls. Similarly, cases consistently had higher outpatient care costs after adjusting for other comorbid conditions over a 15-year period.
Figure 1.
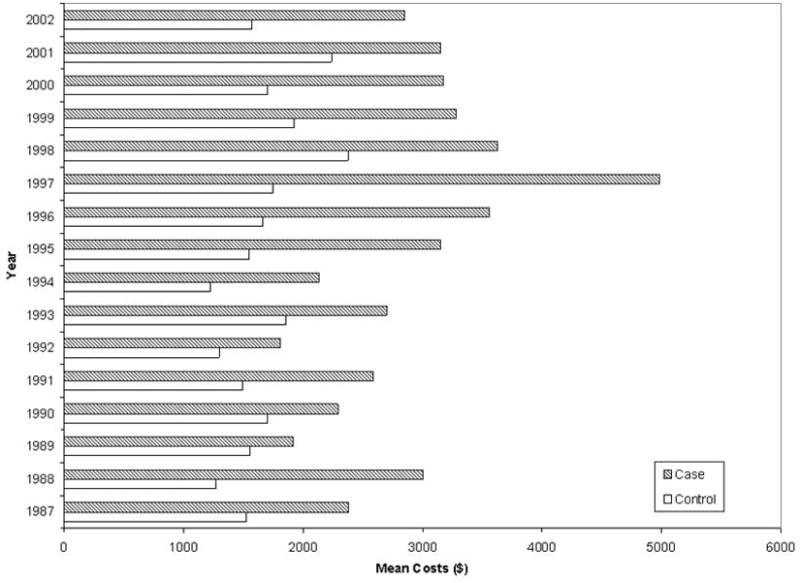
Mean observed annual total costs for women with constipation versus controls according to year.
Figure 2.
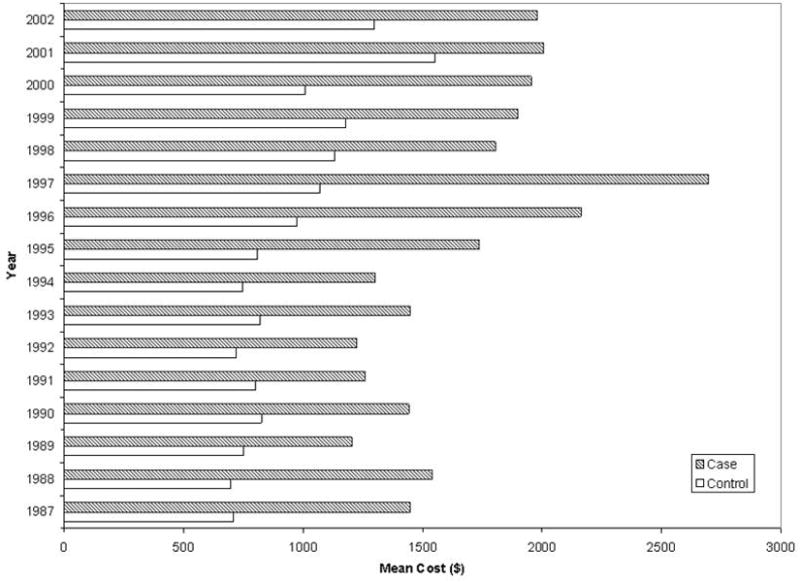
Mean observed annual outpatient costs of women with constipation versus controls
Table 5 summarizes the impact of comorbid conditions on direct medical costs. After adjusting for other comorbid conditions, depression and dyspepsia were all significantly associated with both total and outpatient medical costs. The association of abdominal pain and heartburn/GERD were borderline significantly associated with outpatient medical costs (Table 5). Depression was associated with a 56% increase in total costs and 50% in outpatient medical costs. However, dyspepsia was found to have a decrease in medical costs (-77% in total and -84% in outpatient). Thyroid disorders, anxiety, back pain and headache were not significantly related to direct medical costs (Table 5).
Table 5. Multivariable predictors of costs for Cases.
| Predictor | Outpatient Costs | Total Costs | ||
|---|---|---|---|---|
| Predicted Change in Costs (%) | P-Value | Predicted Change in Costs (%) | P -Value | |
| Abdominal Pain | 28.35 | 0.09 | 32.50 | 0.10 |
| Heartburn/GERD | 32.61 | 0.07 | 2.30 | 0.88 |
| Dyspepsia | -84.26 | <0.0001 | -76.79 | 0.0009 |
| Depression | 50.29 | 0.008 | 55.72 | 0.03 |
| Anxiety | -12.41 | 0.37 | -24.02 | 0.18 |
| Thyroid | 4.02 | 0.89 | -20.23 | 0.53 |
| Headache | -3.08 | 0.84 | -24.68 | 0.17 |
| Back Pain | -4.58 | 0.82 | 1.34 | 0.96 |
| Limb Pain | 42.35 | 0.029 | 17.09 | 0.50 |
GERD=Gastroesophageal reflux disease
Interactions between co-morbid conditions and constipation were examined for both total medical costs and outpatient medical costs. Only dyspepsia was found to have a significant interaction with constipation status. Among constipated women, patients with dyspepsia were found to have a decrease in both their total (36.7%) and outpatient (55.4%) costs compared to those without dyspepsia. However, women without constipation (controls) had a marginal increase in costs (1.2% and 2.9%, respectively) in patients with dyspepsia versus those without dyspepsia.
Discussion
This is to our knowledge the first population-based longitudinal study to present U.S. data on the costs related with constipation over a 15-year timeframe. We observed that women with a diagnosis of constipation consistently used more of all types of medical services, from outpatient clinics to inpatient hospitalizations and emergency department visits, compared to matched controls. Moreover, women with constipation were more likely to present for abdominal pain or for somatic or psychological co-morbid conditions over a 15-year period. Overall, women with constipation consistently had higher health care costs over time; specifically, the overall annual medical costs for women with constipation are more than twice that of controls.
Constipation is one of the most common digestive disorders in the United States.2, 26, 27 Choung et al.27 showed that the cumulative incidence of chronic constipation over 12 years was almost one in six. Moreover, physician office visit related to constipation have dramatically increased.28 Shah et al.28 studied the national trends in physician office visits associated with constipation between 1993 and 2004 using National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Care Survey (NHAMCS) in USA. They showed that ambulatory visits for constipation increased from 4 million (95% CI 3.3–4.7 million) ambulatory visits for constipation annually during 1993–1996 period to 7.95 million (95% CI 6.6–9.4 million) visits during the 2001–2004 period. Not surprisingly, in a recent database analysis by Everhart et al.8 on the burden of digestive diseases in the U.S., constipation was the second most common ambulatory care diagnosis after gastroesophageal reflux disease among gastrointestinal diseases. They also showed that hospitalizations for chronic constipation were uncommon. Our study has confirmed these observations; we found a relatively lower number of hospitalizations compared to other medical services and a relatively higher number of outpatient clinic visits. However, all medical services were more frequently used by constipated women. In addition, our study showed that outpatient medical visits for comorbid somatic pain, abdominal pain, and psychological conditions are disproportionately higher for women who present with constipation. This is consistent with other data. Mason et al.29 studied psychological morbidity in women with constipation; they reported that patients with constipation had significantly increased psychological and social morbidity (anxiety, depression, and social dysfunction) and increased somatization. Other studies have shown that constipation is linked to comorbid conditions, including somatic pain, psychologic conditions, abdominal pain, and other digestive diseases.27, 29-31 Thus, it is conceivable that constipation directly and indirectly contributes to high usage of health care resources. Our study showed that women with dyspepsia and constipation actually had lower total (36.7%) and outpatient (55.4%) costs compared to those without dyspepsia, but dyspepsia is unlikely to have had any effects on incremental medical costs because only 14 patients out of 168 constipated women had dyspepsia. Confounding variables might explain less consulting behavior in patients with dyspepsia, such as younger age, although we tried to adjust for confounding.32, 33
Martin et al.34 studied the economic burden of constipation based on an analysis of three national surveys (the 2001 National Ambulatory Medical Care Survey, the 2001 National Hospital Ambulatory Medical Care Survey, and the 2001 National Hospital Discharge Survey). They reported that the costs associated with medical care for constipation totaled $235 million in 2001.34 This estimate does not include the costs of over-the-counter and prescription drugs or the cost of care when constipation was determined to be a complication of other disease or a comorbid condition. In another study using the California Medicaid program (Medi-Cal), Singh et al.35 showed that constipation-related total Medi-Cal reimbursement over a 15-month period was $18,891,008, representing a substantial economic loss for the Medicaid system. We obtained data on the incremental medical costs for women with constipation compared to matched controls in longitudinal observations over 15 years. In the current study, the average annual incremental total medical costs over a 15-year period in a woman with constipation was $1,272 more than controls, and the average annual incremental medical costs of outpatient care in a woman with constipation was $ 827 more than controls. Because our study compared constipated subjects to controls, it is reasonable to conclude that constipation contributes to significant incremental medical costs.
This study had some potential limitations. First, the study could not include all subjects with constipation in a community, because subjects with symptoms not seeking medical attention would not be identified. Thus, our study likely underestimates the actual direct cost burden of constipation. In this study we were unable to look at indirect costs, such as workday absences or drug use, and thus our cost estimations probably underestimate the impact of the disorder. Moreover, the high medical costs in constipated women might be related to other medical conditions or treatments such as opioid use, surgery, or chemotherapy, etc. However, we still observed higher medical costs in constipated women compared to controls over a 15-year period after adjusting for other comorbid conditions including abdominal pain, depression, and headache. Second, these data are only generalizable to the white U.S. population because the racial composition of this community is predominantly Caucasian.15 Moreover, the services and the utilization patterns in Olmsted County may not be totally generalizable to other settings due to a higher proportion of the working population being employed in the health care industry and the correspondingly slightly higher education level.
Thus, we conclude from this population-based study that subjects with constipation are greater utilizers of all types of medical services, and this is not explained by comorbid conditions. Interventions to reduce the burden of constipation may be cost saving.
Acknowledgments
The authors wish to thank Lori R. Anderson for her assistance in the preparation of the manuscript.
Grant Support: This investigator initiated study was supported by Takeda Pharmaceuticals, who were not involved in the design, analysis or interpretation of the findings. This study was made possible in part by the Rochester Epidemiology Project (Grant #R01-AR30582 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases).
Abbreviations
- REP
Rochester Epidemiology Project
- ICD
International Classification of Diseases
- H-ICDA
Hospital Adaptation of the International Classification of Diseases
- OCHEUD
Olmsted County Healthcare Expenditure and Utilization Database
- U.S.
United States
Footnotes
Disclosures: No conflict of interest to disclose for all authors.
Specific Author Contributions: Rok Seon Choung, Denesh Chitkara, Nilay D. Shah, G. Richard Locke III, and Nicholas J. Talley participated in the design, analysis, and writing of the manuscript. Slavica K. Katusic participated in acquisition of the data and material support. Nilay Shah and Megan E. Branda provided the statistical analysis and assisted in writing the manuscript.
Writing Assistance: None
References
- 1.Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L. An epidemiological survey of constipation in canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol. 2001;96:3130–7. doi: 10.1111/j.1572-0241.2001.05259.x. [DOI] [PubMed] [Google Scholar]
- 2.Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ., 3rd Functional constipation and outlet delay: a population-based study. Gastroenterology. 1993;105:781–90. doi: 10.1016/0016-5085(93)90896-k. [DOI] [PubMed] [Google Scholar]
- 3.Sandler RS, Jordan MC, Shelton BJ. Demographic and dietary determinants of constipation in the US population. Am J Public Health. 1990;80:185–9. doi: 10.2105/ajph.80.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–80. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 5.Stewart WF, Liberman JN, Sandler RS, Woods MS, Stemhagen A, Chee E, Lipton RB, Farup CE. Epidemiology of constipation (EPOC) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol. 1999;94:3530–40. doi: 10.1111/j.1572-0241.1999.01642.x. [DOI] [PubMed] [Google Scholar]
- 6.van den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006;101:2401–9. doi: 10.1111/j.1572-0241.2006.00771.x. [DOI] [PubMed] [Google Scholar]
- 7.Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750–9. doi: 10.1111/j.1572-0241.2004.04114.x. [DOI] [PubMed] [Google Scholar]
- 8.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology. 2009;136:741–54. doi: 10.1053/j.gastro.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Johanson JF, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther. 2007;25:599–608. doi: 10.1111/j.1365-2036.2006.03238.x. [DOI] [PubMed] [Google Scholar]
- 10.Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ., 3rd Onset and disappearance of gastrointestinal symptoms and functional gastrointestinal disorders. Am J Epidemiol. 1992;136:165–77. doi: 10.1093/oxfordjournals.aje.a116483. [DOI] [PubMed] [Google Scholar]
- 11.Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, Coyne K. The health-related quality of life and economic burden of constipation. Pharmacoeconomics. 2005;23:461–76. doi: 10.2165/00019053-200523050-00006. [DOI] [PubMed] [Google Scholar]
- 12.Sonnenberg A, Koch TR. Physician visits in the United States for constipation: 1958 to 1986. Dig Dis Sci. 1989;34:606–11. doi: 10.1007/BF01536339. [DOI] [PubMed] [Google Scholar]
- 13.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–90. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 14.Colditz GA, Manson JE, Hankinson SE. The Nurses' Health Study: 20-year contribution to the understanding of health among women. J Womens Health. 1997;6:49–62. doi: 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- 15.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 16.Melton LJ., 3rd The threat to medical-records research. N Engl J Med. 1997;337:1466–70. doi: 10.1056/NEJM199711133372012. [DOI] [PubMed] [Google Scholar]
- 17.Katusic SK, Colligan RC, Barbaresi WJ, Schaid DJ, Jacobsen SJ. Potential influence of migration bias in birth cohort studies. Mayo Clin Proc. 1998;73:1053–61. doi: 10.4065/73.11.1053. [DOI] [PubMed] [Google Scholar]
- 18.Chitkara DK, Talley NJ, Weaver AL, Katusic SK, De Schepper H, Rucker MJ, Locke GR., 3rd Incidence of presentation of common functional gastrointestinal disorders in children from birth to 5 years: a cohort study. Clin Gastroenterol Hepatol. 2007;5:186–91. doi: 10.1016/j.cgh.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Chitkara DK, Talley NJ, Locke GR, 3rd, Weaver AL, Katusic SK, De Schepper H, Rucker MJ. Medical presentation of constipation from childhood to early adulthood: a population-based cohort study. Clin Gastroenterol Hepatol. 2007;5:1059–64. doi: 10.1016/j.cgh.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 20.Lipscomb J, Ancukiewicz M, Parmigiani G, Hasselblad V, Samsa G, Matchar DB. Predicting the cost of illness: a comparison of alternative models applied to stroke. Med Decis Making. 1998;18:S39–56. doi: 10.1177/0272989X98018002S07. [DOI] [PubMed] [Google Scholar]
- 21.Choung RS, Shah ND, Chitkara D, Branda ME, Van Tilburg MA, Whitehead WE, Katusic SK, Locke GR, 3rd, Talley NJ. Direct Medical Costs of Constipation in Children Older Than 15 Years: A Population-based Birth Cohort. J Pediatr Gastroenterol Nutr. doi: 10.1097/MPG.0b013e3181e67058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 23.Campbell MK, Torgerson DJ. Bootstrapping: estimating confidence intervals for cost-effectiveness ratios. Qjm. 1999;92:177–82. doi: 10.1093/qjmed/92.3.177. [DOI] [PubMed] [Google Scholar]
- 24.Tian L, Huang J. A two-part model for censored medical cost data. Stat Med. 2007;26:4273–92. doi: 10.1002/sim.2847. [DOI] [PubMed] [Google Scholar]
- 25.R Development Core Team. R Foundation for Statistical Computing. Vienna, Austria: 2008. R: A language and environment for statistical computing. URL http://www.R-project.org., 2008. [Google Scholar]
- 26.Shaheen NJ, Hansen RA, Morgan DR, Gangarosa LM, Ringel Y, Thiny MT, Russo MW, Sandler RS. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–38. doi: 10.1111/j.1572-0241.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- 27.Choung RS, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Cumulative incidence of chronic constipation: a population-based study 1988-2003. Aliment Pharmacol Ther. 2007;26:1521–8. doi: 10.1111/j.1365-2036.2007.03540.x. [DOI] [PubMed] [Google Scholar]
- 28.Shah ND, Chitkara DK, Locke GR, Meek PD, Talley NJ. Ambulatory care for constipation in the United States, 1993-2004. Am J Gastroenterol. 2008;103:1746–53. doi: 10.1111/j.1572-0241.2008.01910.x. [DOI] [PubMed] [Google Scholar]
- 29.Mason HJ, Serrano-Ikkos E, Kamm MA. Psychological morbidity in women with idiopathic constipation. Am J Gastroenterol. 2000;95:2852–7. doi: 10.1111/j.1572-0241.2000.02313.x. [DOI] [PubMed] [Google Scholar]
- 30.Talley NJ, Lasch KL, Baum CL. A gap in our understanding: chronic constipation and its comorbid conditions. Clin Gastroenterol Hepatol. 2009;7:9–19. doi: 10.1016/j.cgh.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 31.Belsey J, Greenfield S, Candy D, Geraint M. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 31:938–49. doi: 10.1111/j.1365-2036.2010.04273.x. [DOI] [PubMed] [Google Scholar]
- 32.Ahlawat SK, Richard Locke G, Weaver AL, Farmer SA, Yawn BP, Talley NJ. Dyspepsia consulters and patterns of management: a population-based study. Aliment Pharmacol Ther. 2005;22:251–9. doi: 10.1111/j.1365-2036.2005.02525.x. [DOI] [PubMed] [Google Scholar]
- 33.Meineche-Schmidt V, Krag E. Dyspepsia in general practice in Denmark. A 1-year analysis of consulters in general practice Scand. J Prim Health Care. 1998;16:216–21. doi: 10.1080/028134398750002981. [DOI] [PubMed] [Google Scholar]
- 34.Martin BC, Barghout V, Cerulli A. Direct medical costs of constipation in the United States. Manag Care Interface. 2006;19:43–9. [PubMed] [Google Scholar]
- 35.Singh G, Lingala V, Wang H, Vadhavkar S, Kahler KH, Mithal A, Triadafilopoulos G. Use of health care resources and cost of care for adults with constipation. Clin Gastroenterol Hepatol. 2007;5:1053–8. doi: 10.1016/j.cgh.2007.04.019. [DOI] [PubMed] [Google Scholar]


