Abstract
The Abbreviated Injury Scale (AIS) is commonly used to score injury severity and describe types of injuries. In 2005, the AIS-Head section was revised to capture more detailed information about head injuries and to better reflect their clinical severity, but the impact of these changes is largely unknown. The purpose of this study was to compare AIS-1998 and AIS-2005 coding of traumatic brain injuries (TBI) using medical records at a single Level I trauma center. We included patients with severe TBI (Glasgow Coma Scale 3–8) after blunt injury, excluding those who were missing medical records. Detailed descriptions of injuries were collected, then manually coded into AIS-1998 and AIS-2005 by the same Certified AIS Specialist. Compared to AIS-1998, AIS-2005 coded the same injuries with lower severity scores [p<0.01] and with decreased mean and maximum AIS-Head scores [p<0.01]. Of the types of traumatic brain injuries, most of the changes occurred among cerebellar and cerebral injuries. Traumatic hypoxic brain injury secondary to systemic dysfunction was captured by AIS-2005 but not by AIS-1998. However, AIS-2005 captured fewer loss of consciousness cases due to changes in criteria for coding concussive injury. In conclusion, changes from AIS-1998 to AIS-2005 result in significant differences in severity scores and types of injuries captured. This may complicate future TBI research by precluding direct comparison to datasets using AIS-1998. TBIs should be coded into the same AIS-version for comparison or evaluation of trends, and specify which AIS-version is used.
INTRODUCTION
Accurate representation of patient injuries is essential to contemporary trauma research and public health initiatives. The Abbreviated Injury Scale (AIS) has earned widespread acceptance as a gold standard for scoring injury severity since its development in 1971 and subsequent revisions [Committee, 1971], [Wang and Gennarelli, 2009]. The most recent revision, AIS-2005, modified the Head section to capture details of head injuries, such as size of hematoma, to better reflect clinical severity of head injuries, and to improve the accuracy of coding concussive TBI [Gennarelli and Wodzin, 2006]. These revisions may have introduced major changes in coding the severity of the same traumatic brain injuries, and may have changed the types of injuries captured by AIS codes.
Although a few studies have addressed possible changes in injury coding between AIS revisions, these studies did not specifically address traumatic brain injury (TBI), one of the areas where specific changes were made. Salottolo et al analyzed AIS scores for all body regions and found AIS-2005 derived Injury Severity Scores (ISS) were significantly lower than those from AIS-1998. Another study found a significant reduction in maximum AIS score using AIS-2005 compared to AIS-1990 [Barnes, Hassan, and Cuerden, et al, 2009]. Prior studies have not evaluated direct changes in scoring and coding of specific traumatic brain injuries between AIS-1998 and AIS-2005. The objective of this study was to compare AIS-1998 and AIS-2005 coding of TBI using medical records at a single Level I trauma center.
METHODS
Study Setting
We selected patients who sustained a severe blunt TBI during a 1-year period at a single Level I trauma center since all patients with a severe TBI routinely undergo head computed tomography (CT) per clinical protocol. In addition, these patients are admitted to the hospital and are more likely to have more thorough documentation of injuries than patients who are not admitted to the hospital and patients who have milder blunt TBI. Since AIS coding instructions specifically state that injuries must be verified by CT or other diagnostic studies, we selected this study population to best assess changes in coding from AIS-1998 to AIS-2005. Severe TBI was defined as an admission Glasgow Coma Scale (GCS) of 3 to 8. Patients with penetrating injuries or missing medical records were excluded. To select the study population, we reviewed all medical records of patients undergoing a head CT in the study period. The mechanism of injury, patient demographics, and traumatic brain injury characteristics were abstracted from the medical records and radiology reports.
Data Abstraction
A standardized abstraction form was created in conjunction with the Certified AIS Specialist prior to medical records review. Detailed information for all TBI was recorded to fulfill injury description standards in AIS-1998 and AIS-2005. We defined “head” as superior to the supraorbital ridge; lateral to the orbit of the eye and superior to the zygomatic arch; or posterior to the angle of the mandible and overlying the skull. Injuries to portions of bones not contributing to the base or vault of the skull, bones of the face, and superficial areas of the face were excluded.
AIS-1998 and AIS-2005 Coding
A single Certified AIS Specialist manually coded all TBIs into AIS-2005 and AIS-1998. All codes were assigned based solely on the information provided by the medical record reviewers. The coder did not have access to the medical records.
Comparison of Head Injuries, AIS-1998 versus AIS-2005
Detailed information for all head injuries was abstracted from the medical records for the following categories as defined by AIS-1998 and AIS-2005.
Scalp Injury:
Scalp injuries were defined as any abrasion, contusion, laceration, or avulsion of soft tissue overlying the head, as previously defined. Descriptions of superficial injuries were categorized to match AIS-1998 and AIS-2005 injury descriptions.
Skull Fracture
Skull was defined as any component of the vault [parietal bone, frontal bone, temporal bone-squamous portion, occipital bone-squamous portion, and sphenoid bone-greater wing) or skull base [occipital bone, except squamous portion; temporal bone, except squamous portion; sphenoid bone, except greater wing; ethmoid bone-crista galli, and ethmoid bone-cribriform plate]. For each fracture, we recorded the bones involved, and the extent and morphology of the fracture. In the case of multiple skull fractures, each fracture was separately recorded.
Intracranial Injury:
Intracranial injuries were defined as any injury to the internal contents of the skull, including the meninges, brainstem, cerebellum, and cerebrum. We included all intracranial injuries that were documented on a head CT. Injuries noted in the clinical progress notes were not coded unless also noted in a head CT or in an operative report.
Changes in TBI Coding and Definitions: AIS-1998 versus AIS-2005
Hypoxic or Ischemic Brain Damage:
AIS-2005 introduced new codes to capture hypoxic or ischemic brain damage not directly attributable to head trauma. There are no equivalent codes in AIS-1998 to account for hypoxic brain injury secondary to systemic hypoxemia, hypotension, or shock.
Concussive Injury:
Both AIS-1998 and AIS-2005 include codes to capture concussive injury, all of which include the presence and duration of loss of consciousness. Coding loss of consciousness under AIS-1998 requires that, “[…] the level of consciousness and its duration must be observed by emergency or medical personnel.” (emphasis added) However, the definition of loss of consciousness changed in AIS-2005 to require “convincing evidence of head trauma and the diagnosis is made by a physician or recorded by a physician based on EMS corroboration.” (emphasis added) for the diagnosis of concussive injury.
We defined duration of LOC from the earliest explicit physician documentation of “LOC” or GCS <9 (clinically comatose) until the medical record indicated the patient either regained consciousness or died. Duration of LOC was categorized to fit AIS-1998 and AIS-2005 injury descriptions. “Regained consciousness” was defined as the time of any documentation of a patient being “awake,” “following commands,” or an improved GCS to 9 or more. Death before regaining consciousness was noted from the discharge summary or death certificates. In the case of absent, insufficient, or conflicting records, LOC duration was noted as “unknown.”
Data Analysis
Head injuries not codable into both AIS-1998 and AIS-2005 and injuries receiving AIS Score 9 [“unknown”] were excluded from analysis of AIS score distribution and change in mean and maximum AIS score. Due to non-normality of the AIS score distributions, the nonparametric Wilcoxon signed-rank test was used to test for differences in severity score distribution between AIS-1998 and AIS-2005, and differences in maximum AIS severity scores between the two AIS revisions. Statistical significance was defined as p-value ≤0.01. Statistical analysis was performed using Stata Release 10 (StataCorp, College Station, TX USA). This study was approved by the Institutional Review Board of the Medical College of Wisconsin.
RESULTS
In 2008, 147 individuals sustained a severe TBI. After chart review, we excluded 2 patients with isolated loss of consciousness reported by emergency or medical personnel and no other TBI because these patients did not have any AIS-2005 codes for comparison. AIS-2005 requires explicit physician diagnosis or documentation of loss of consciousness (LOC) in order to code concussive injury. In contrast, AIS-1998 allows LOC to be coded when reported by emergency or medical personnel without physician corroboration. The group’s mean age was 42 years and the median GCS was 3. The most common mechanism of injury was automobile crash (N=60), followed by fall (N=31). Most patients had multiple injuries; the 145 patients represented 807 traumatic brain injuries coded into AIS-1998 and AIS-2005 (Table 1).
Table 1:
TBI Codable in Both AIS-1998 and AIS-2005
| INJURY | N | % |
|---|---|---|
| Scalp Injury | 118 | 14.6% |
| Skull Fracture | 88 | 10.9% |
| Base Fracture | 61 | 7.6% |
| Vault Fracture | 27 | 3.3% |
| Intracranial Injury | 508 | 62.9% |
| Brainstem | 51 | 6.3% |
| Cerebellum | 30 | 3.7% |
| Cerebrum | 427 | 52.9% |
| Concussive Injury | 93 | 11.5% |
| Total TBIs* | 807 |
numbers are rounded and may not add to 100%
Comparison of Head Injuries, AIS-1998 versus AIS-2005
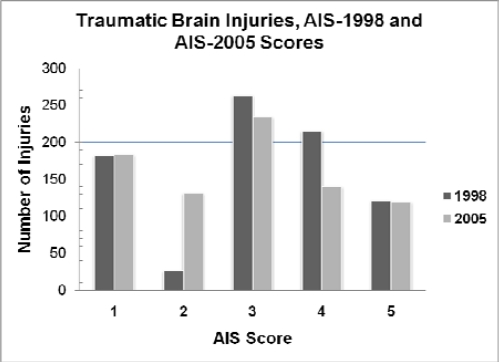
The majority (79.4%) of AIS scores were unchanged between AIS-1998 and AIS-2005. However, the AIS score distribution was significantly shifted to a lower score from AIS-1998 to AIS-2005 (p < 0.01) (Figure 1). The mean AIS score was also significantly lower by AIS-2005 (2.85, 95% CI: 2.76–2.95) than by AIS-1998 (3.08, 95% CI: 2.99–3.18) (p < 0.01). Finally, we found that for a given patient, the maximum AIS score for TBI was significantly decreased (p <0.01).
Figure 1:
Number of Injuries by AIS Score, AIS-1998 vs. AIS-2005
The AIS score distributions and mean AIS scores for scalp injuries and skull fractures were not significantly changed in AIS-2005 versus AIS-1998. However, most of the changes in AIS scores were noted in intracranial injuries, and, specifically, in cerebral and cerebellar injuries (Table 2). AIS-2005 cerebral injuries had a significantly decreased AIS score distribution and lower mean score (AIS-2005 3.37, 95% CI: 3.27–3.46; AIS-1998 3.74, 95% CI: 3.67–3.81) (p<0.01). Of 427 cerebral injuries, 140 (32.8%) had a decrease in AIS score. Similarly, the AIS-2005 cerebellar AIS score distribution and mean score were significantly decreased (AIS-2005 2.63, 95% CI: 2.33–2.94; AIS-1998 3.33, 95% CI: 3.11–3.56).
Table 2.
Changes in AIS Score by Injury, AIS-1998 vs. AIS-2005
| INJURY DESCRIPTION | AIS-1998 SCORE | AIS-2005 SCORE |
|---|---|---|
| *Cerebellum: contusion, single or multiple: tiny; <1cm diameter | 3 | 2 |
| Cerebellum: hematoma (hemorrhage): epidural or extradural: NFS | 4 | 3 |
| *Cerebellum: hematoma (hemorrhage): epidural or extradural: tiny; <0.6cm thick | 4 | 2 |
| Cerebellum: hematoma (hemorrhage): intracerebellar including petechial and subcortical: NFS | 4 | 3 |
| *Cerebellum: hematoma (hemorrhage: intracerebellar including petechial and subcortical: tiny; <0.6cm diameter [includes radiographic “shearing” lesions] | 4 | 2 |
| Cerebellum: hematoma (hemorrhage): subdural: NFS | 4 | 3 |
| *Cerebellum: hematoma (hemorrhage): subdural: tiny; <0.6cm thick | 4 | 2 |
| Cerebellum: laceration [not from penetrating injury]: NFS | 4 | 3 |
| Cerebellum: laceration [not from penetrating injury]: ≤2cm length or depth Cerebellum: subarachnoid hemorrhage |
4 3 |
3 2 |
| Cerebellum: subpial hemorrhage | 3 | 2 |
| *Cerebrum: contusion: single: tiny; <1cm diameter | 3 | 2 |
| *Cerebrum: contusion: multiple, on same side: tiny; each <1cm diameter | 3 | 2 |
| *Cerebrum: contusion: multiple, at least one on each side: tiny: each <1cm diameter | 3 | 2 |
| Cerebrum: diffuse axonal injury: NFS | 5 | 4 |
| Cerebrum: diffuse axonal injury: confined to white matter or basal ganglia | 5 | 4 |
| Cerebrum: hematoma (hemorrhage): NFS or “extra axial” | 4 | 3 |
| Cerebrum: hematoma (hemorrhage):epidural or extradural: NFS | 4 | 3 |
| *Cerebrum: hematoma (hemorrhage):epidural or extradural: tiny; <0.6cm thick | 4 | 2 |
| Cerebrum: hematoma (hemorrhage): intracerebral: NFS | 4 | 3 |
| * Cerebrum: hematoma (hemorrhage): intracerebral: tiny; single or multiple <1cm diameter | 4 | 2 |
| * Cerebrum: hematoma (hemorrhage): intracerebral: petechial hemorrhage(s) [includes radiographic “shearing” lesions] | 4 | 2 |
| * Cerebrum: hematoma (hemorrhage): intracerebral: petechial hemorrhage(s) [includes radiographic “shearing” lesions]; not associated with coma >6 hours | 4 | 2 |
| Cerebrum: hematoma (hemorrhage): intracerebral: small; ≤30cc or ≤15cc if age ≤ 10; 1–4cm diameter or ≤1cm if ≤age 10; subcortical hemorrhage: not associated with coma >6 hours | 4 | 3 |
| Cerebrum: hematoma (hemorrhage): subdural: NFS | 4 | 3 |
| Cerebrum: hematoma (hemorrhage): subdural: tiny; <0.6cm thick [includes tentorial (subdural) blood one or both sides] | 4 | 3 |
| Cerebrum: hematoma (hemorrhage): subdural: small; moderate; ; ≤50cc or ≤25cc if age ≤10; 0.6–1cm thick: bilateral [both sides 0.6–1.0cm thick] | 5 | 4 |
| Cerebrum: laceration [not from penetrating injury]: NFS Cerebrum: laceration [not from penetrating injury]: ≤2cm length or depth |
4 4 |
3 3 |
| Cerebrum: intraventricular hemorrhage: NFS | 4 | 2 |
| Cerebrum: intraventricular hemorrhage: not associated with coma >6 hours | 4 | 2 |
| **Cerebrum: ischemic brain damage directly related to head trauma: associated with coma >6 hours | 3 | 5 |
| Cerebrum: subarachnoid hemorrhage: NFS Cerebrum: subarachnoid hemorrhage: not associated with coma >6 hours |
3 3 |
2 2 |
| Cerebrum: subpial hemorrhage: NFS | 3 | 2 |
| Cerebrum: subpial hemorrhage: not associated with coma >6 hours | 3 | 2 |
| Cerebral Concussion: NFS | 2 | 1 |
New injury descriptor in AIS-2005, captured by AIS-1998 code with less specific size discrimination;
AIS-2005 Score increased versus AIS-1998 Score; NFS = Not Further Specified
Changes in TBI Coding and Definitions: AIS-1998 versus AIS-2005
Hypoxic or Ischemic Brain Damage:
AIS-2005 allowed for coding of 3 cases of hypoxic or ischemic traumatic brain injury not codable in AIS-1998 with AIS-2005 140703.9. Both AIS-1998 and AIS-2005 have similar codes for ischemic brain damage “directly related to head trauma.” However, AIS-1998 lacks codes accounting for ischemic brain injury secondary to systemic dysfunction and “[…] not directly related to head trauma.” These injuries are assigned AIS score 9 in AIS-2005 and, accordingly, do not affect AIS score distributions.
Concussive Injury:
Due to differences in standards of evidence for coding concussive injuries and loss of consciousness, 7 out of 100 cases of AIS-1998 concussive injuries were not codable in AIS-2005 because they had emergency or medical personnel reports of loss of consciousness (AIS-1998 criteria) but lacked physician diagnosis or documentation of loss of consciousness (AIS-2005 criteria).
Diffuse Axonal Injury:
The coding of diffuse axonal injury (DAI) was extensively revised in AIS-2005 to differentiate it from other injuries with similar presentations. In AIS-2005, certain individual traumatic brain findings are not coded in patients with a confirmed diagnosis of DAI and corroborating evidence on imaging. As a result, one brainstem shearing injury, 2 cases of intraventricular hemorrhage, and 4 cases of subarachnoid hemorrhage coded in AIS-1998 [140206.5, 140678.4 and 140684.3, respectively] were not individually coded in AIS-2005 in patients with DAI.
All of these patients had other TBI that could be coded into both AIS-1998 and AIS-2005 and, therefore, were included in our study population (Table 3).
Table 3.
| AIS-1998 | AIS-2005 | N= |
|---|---|---|
| 140206.5 | NONCODABLE | 1 |
| 140678.4 | NONCODABLE | 2 |
| 140684.3 | NONCODABLE | 4 |
| 160210.4 | NONCODABLE | 5 |
| 160214.5 | NONCODABLE | 1 |
| 160802.2 | NONCODABLE | 1 |
| NONCODABLE | 140703.9 | 3 |
All patients with codes in Table 3 also had other TBI codable in both AIS-1998 and AIS-2005;
May not be codable due to specifics of individual case
DISCUSSION
In comparing AIS-1998 to AIS-2005, we found a significant decrease in AIS-2005 scores, reflected by a shift in AIS score distribution to lower severity, a lower mean AIS score, and by patient, a lower maximum AIS score. Our results suggest that the differences in AIS score distribution from AIS-1998 to AIS-2005 arise from changes to the scoring of cerebellar and cerebral injuries, generally, and finer discrimination of lesion size and LOC duration, specifically, in the coding rubric of AIS-2005. For example, under AIS-2005, a subarachnoid hemorrhage (SAH) associated with coma <6 hrs receives AIS Score 2 while a SAH with coma >6 hrs is given AIS Score 3. Such discrimination of SAH by duration of coma did not exist in AIS-1998, and all SAH were AIS Score 3. AIS-2005 captures ischemic TBI secondary to systemic dysfunction not codable in AIS-1998. While AIS-1998 and AIS-2005 have comparable codes for ischemic brain injury due to head trauma, AIS-1998 lacks the ability to capture ischemic brain injuries secondary to systemic dysfunction and not directly attributable to head trauma. However, AIS-2005 captures fewer cases of loss of consciousness than AIS-1998 due to changes in standards of evidence required to code a concussive injury under AIS-2005. The AIS-1998 explicitly allows the use of non-physician documentation of LOC to substantiate coding of LOC, even in the absence of a physician’s diagnosis or documentation corroborating the LOC. In contrast, AIS-2005 specifically disallows the use of non-physician diagnoses of LOC in the absence of physician diagnosis or physician documentation. While the phrasing change is subtle, its ramifications are material to LOC coding in practice and underlie the exclusion of two cases of LOC from our study. These LOC cases were captured under the less specific “emergency or medical personnel” clause of AIS-1998, but not under the more stringent AIS-2005 requirement for physician diagnosis or documentation. As reported in our results, an additional 7 cases of LOC captured by AIS-1998 were not codable under the more stringent standards for LOC under AIS-2005.
Although our study is limited by a relatively small number of subjects in a single Level I trauma center, we were able to abstract detailed injury descriptors for a large number of individual head injuries that might not be available in larger, multicenter datasets. We also abstracted data for the Certified AIS Specialist who did not have direct access to the medical records. In practice, most coders use the entire medical record. However, our data abstraction purposely included the information that the AIS coder would obtain from the medical records. In addition, the AIS Specialist had direct access to clinicians for clarification; this may not be the case at most centers. In addition, we used GCS to select our study population. GCS is often confounded by sedation.
Terminology used to describe injuries may vary greatly between centers [Gennarelli, et al, 2006] and similar terminology is likely employed within a single institution. Although we found certain terms were used interchangeably to describe similar injuries, several terms did not correspond with AIS injury descriptions. For example, the terms “hematoma,” “contusion,” and “hemorrhagic contusion” were used interchangeably in head CT reports describing parenchymal lesions. However, AIS codes distinguish between hematoma and contusion, and the scores may differ for hematomas and contusions of the same size. For example, a “small hematoma <30cc” is AIS 4 but a “small contusion <30cc” is AIS 3. Hemorrhagic contusions are not clearly defined and often will be categorized according to the coder’s discretion. Similar difficulty arose with the use of “complex” and “massive” in regard to skull fractures. These phrases were rarely used in the radiology reports for head injuries, but may affect the AIS score. Standardization of terminology might help clarify AIS coding.
Few studies have compared AIS-2005 to prior AIS versions. Salottollo et al retrospectively studied AIS scores of trauma patients admitted to two separate trauma centers. For all body regions, they found a significant decrease in mean AIS score. They also found 29% of AIS scores decreased in the AIS-2005 Head section. Barnes et al retrospectively analyzed the United Kingdom Cooperative Crash Injury Database and compared AIS-2005 to AIS-1990. For the head/neck, thorax, and extremity body regions, they found a significant decrease in maximum AIS score. Similarly, we found significant decreases in AIS-2005 scores compared to AIS-1998 with specific focus on detailed head injuries. We also found that most of the changes in scoring arose from cerebral and cerebellar injuries in the intracranial injury section. Our detailed injury analysis also allowed us to identify injuries such as concussive injury or hypoxic brain injury secondary to systemic dysfunction that were not captured or were defined differently in AIS-2005 compared to AIS-1998.
CONCLUSIONS
The AIS-2005 revision significantly decreases the scoring distribution for TBI compared to AIS-1998. Most AIS score changes are attributable to scoring changes in cerebral and cerebellar injuries. AIS-2005 also includes coding for hypoxic TBI and changes in concussive injury definitions. These changes may complicate future TBI research by precluding direct comparison to data sets that use AIS-1998. Injuries should be recoded into the same AIS version for comparison or for evaluation of trends, and studies should specify which AIS revision was used in their methodology.
Acknowledgments
This project was funded by the Medical College of Wisconsin, Department of Neurosurgery. Clare E. Guse is partially supported by CDC grant R49/CE001175. The authors would like to thank Judeen Richlen, RN for her assistance and the manuscript reviewers for their comments and suggestions.
REFERENCES
- Adekoya N, Thurman DJ, White DD, Webb KW. Surveillance for Traumatic Brain Injury Deaths—United States, 1989–1998. MMWR Surveill Summ. 2002;51(10):1–14. [PubMed] [Google Scholar]
- AAAM . The Abbreviated Injury Scale-2005 Revision, Update 2008. Des Plaines, IL: 2008. [Google Scholar]
- AAAM . The Abbreviated Injury Scale-1990, Update 1998. Des Plaines, IL: 2008. [Google Scholar]
- Barnes J, Hassan A, Cuerden R, Cookson R, Kohlhofer J. Comparison of injury severity between AIS 2005 and AIS 1990 in a large injury database. AAAM. 2009;53:83–89. [PMC free article] [PubMed] [Google Scholar]
- Committee on Medical Aspects of Automotive Safety Rating the Severity of Tissue Damage I. The Abbreviated Scale. JAMA. 1971;215(2):277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- Gennarelli TA, Wodzin E. AIS 2005: A Contemporary Injury Scale. Injury. 2006;37(12):1083–91. doi: 10.1016/j.injury.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Hsiao KY, Hsiao CT, Weng HH, Chen KH, Lin LJ, Huang YM. Factors predicting mortality in victims of blunt trauma brain injury in emergency department settings. Emerg Med J. 2008;25(10):670–673. doi: 10.1136/emj.2007.053405. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths; Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006. [Google Scholar]
- Salottolo K, Settell A, Uribe P, Akin S, Slone DS, O’Neal E, Mains C, Bar-Or D. The impact of the AIS 2005 revision on injury severity scores and clinical outcome measures. Injury. 2009;40(9):999–1003. doi: 10.1016/j.injury.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Skaga NO, Eken T, Hestnes M, Jones JM, Steen PA. Scoring of anatomic injury after trauma: AIS 98 versus AIS 90—do the changes affect overall severity assessment. Injury. 2007;38(1):84–90. doi: 10.1016/j.injury.2006.04.123. [DOI] [PubMed] [Google Scholar]
- Sosin DM, Sniezek JE, Waxweiler RJ. Trends in death associated with traumatic brain injury, 1972 through 1992. Success and failure. JAMA. 1995;273(22):1778–1780. [PubMed] [Google Scholar]
- Wang MC, Gennarelli TA. Classification Systems. In: Jallo J, Loftus CM, editors. Neurotrauma and Critical Care of the Brain. New York, NY: Thieme Medical Publishers; 2009. pp. 87–96. [Google Scholar]