Abstract
Background & Aims
In the United States, the use of abdominopelvic computed tomography (APCT) by emergency departments for patients with abdominal pain has increased, despite stable admission rates and diagnosis requiring urgent intervention. We proposed that trends would be similar for patients with Crohn’s disease (CD).
Methods
We conducted a retrospective study of data from 648 adults with CD who presented at 2 emergency departments (2001–2009; 1572 visits). Trends in APCT use were assessed with Spearman’s correlation coefficient. We compared patient characteristics and APCT findings during 2001–2003 and 2007–2009.
Results
APCT use increased from 2001 (used for 47% of encounters) to 2009 (used for 78% of encounters; P=.005), whereas admission rates were relatively stable, at 68% in 2001 and 71% in 2009 (P=.06). The overall proportion of APCTs with findings of intestinal perforation, obstruction, or abscess was 29.0%; 34.9% of APCTs were associated with urgent diagnoses, including those unrelated to CD. Between 2001–2003 and 2007–2009, the proportions of APCTs that detected intestinal perforation, obstruction, or abscess were similar (30% vs 29%, P=.92), as were the proportions used detecting any diagnosis requiring urgent intervention, including those unrelated to CD (36% vs 34%, P=.91).
Conclusions
Despite the increased use of APCT by emergency departments for patients with CD, there were no significant change in admission rates between the periods of 2001–2003 and 2007–2009. The proportion of APCTs that detected intestinal perforation, obstruction, abscess, or other urgent conditions not related to CD remained high.
Keywords: inflammatory bowel disease, abdominal imaging, hospital admission
BACKGROUND & AIMS
Crohn’s disease (CD) is a multisystem disorder characterized primarily by discontinuous transmural and sometimes granulomatous inflammation involving any portion of the gastrointestinal tract. The disease most commonly involves the distal small bowel and proximal colon, and can be complicated by stricture, fistula, abscess and perforation1. The diagnosis is confirmed by endoscopic or surgical biopsies. However, imaging modalities including barium studies, computed tomography (CT) and magnetic resonance imaging are useful in diagnosis and evaluation of disease extent, complications and extra-intestinal findings2.
Despite the benefits of diagnostic imaging in CD management, there are concerns about overuse, particularly of CT, because of the cost and potential risks of contrast nephropathy3 and radiation exposure4–8. Several studies have examined radiation exposure from diagnostic imaging in patients with inflammatory bowel disease (IBD). In an Irish cohort of 399 patients with CD, 15.5% received a very high cumulative effective dose of radiation from diagnostic imaging (>75 millisieverts). Furthermore, abdominopelvic CT (APCT) contributed 77.2% of the total radiation dose9. The increased risk of radiation exposure primarily from APCT in patients with CD has been confirmed in several other studies10–12.
As a result of mounting evidence regarding increasing CT use13 and the concern over cost and radiation risk, both the Food and Drug Administration14 and the American College of Gastroenterology15 have advocated for the need for better clinical decision-making tools to guide the appropriate use of CT. In the United States, the emergency department (ED) has been identified as a setting with dramatic increases in CT use in general16 and for the evaluation of abdominal pain17. While these studies were not limited to patients with CD, another study documented a 165% increase in ED visits related to IBD in 2003–2005 compared with 1994–1996, particularly among young patients with CD18. However, there are limited data on APCT use in the CD population and the impact of APCT on clinical management in the ED setting.
In this study we demonstrate that ED use of APCT for patients with CD has significantly increased in the last decade. However, this increase may not reflect overuse of APCT, as we demonstrate that approximately one-third of APCTs in the ED setting identified findings that warranted urgent or emergent intervention.
METHODS
Participants, setting and study design
A retrospective cross-sectional study was conducted examining ED encounters for patients with CD who presented to two University of Pennsylvania Health System (UPHS) EDs with gastrointestinal complaints between January 1, 2001 and December 31, 2009. The study protocol was approved by the Institutional Review Board of the University of Pennsylvania on May 20, 2010. The Hospital of the University of Pennsylvania (HUP) and Penn Presbyterian Medical Center (PPMC) are tertiary care academic medical centers affiliated with the University of Pennsylvania, although both also serve as community hospitals for West Philadelphia residents. The HUP and PPMC EDs respectively treat approximately 60,000 and 36,000 patients annually. The Penn Inflammatory Bowel Disease Program is a tertiary referral center located at both the HUP and PPMC and is staffed by five clinicians who specialize in IBD.
We used data from the Emergency Medicine Tracking and Charting System (EMTRAC) and the Pennsylvania Integrated Clinical and Administrative Research Database (PICARD). EMTRAC is a computerized charting and order entry system that is used at both study sites. EMTRAC was not fully implemented at one study site (PPMC) until 2003, so PPMC encounters were limited to January 1, 2003 through December 31, 2009. Data available in EMTRAC include demographics, physician orders and notes, diagnoses, laboratory and radiology results. PICARD is a compilation of data that includes the ambulatory electronic health record, the laboratory results reporting system, clinical microbiology, laboratory, radiology and ED data.
The study population included patients age ≥ 18 years with a previous CD diagnosis and a gastrointestinal chief complaint at ED triage. Patients were identified by ambulatory or inpatient diagnoses with International Classification of Diseases (ICD-9) codes for CD (555*) dated prior to the ED visit. EMTRAC includes a standardized list of triage complaints, which were searched to identify the following complaints: abdominal pain or distention, small bowel obstruction, nausea, vomiting, diarrhea, rectal bleeding, gastrointestinal bleed, fever or chills. Exclusion criteria included lack one of the above triage complaints, lack of a diagnosis of CD prior to the ED encounter, or an incomplete ED encounter. Incomplete ED encounters mainly resulted from patients leaving before evaluation or against medical advice. Following an initial electronic query based on ICD-9 code and triage complaint, the EMTRAC notes were manually reviewed to ensure all encounters met inclusion criteria.
Demographics and ED disposition (hospital admission vs. discharge) for patients with eligible encounters were available in PICARD. Patient-reported home medications were manually reviewed in EMTRAC for use of aminosalicylates, corticosteroids, immunomodulators (thiopurines, methotrexate, cyclosporine), biologics (infliximab, adalimumab, certolizumab, natalizumab), narcotics, metronidazole and ciprofloxacin.
An electronic query of EMTRAC searched eligible ED encounters for APCT orders, and ED notes were subsequently manually reviewed to confirm whether APCT was performed. One investigator reviewed APCT reports for the years 2001–2003 and 2007–2009 and characterized diagnoses into four categories: negative, cannot rule out, suspicious for/possible/probable, and definite. The latter two categories were defined as a positive finding, and the former two categories were defined as a negative finding. The diagnoses were further characterized as new, worsening or stable findings compared with the previous APCT.
A composite outcome that included new or worsening perforation, obstruction or abscess on APCT was termed “POA.” The primary outcome of “POANCD” included the above findings and other clinically significant non-CD related APCT scan findings warranting urgent care in the ED. These included cholecystitis, appendicitis, diverticulitis, ischemia or vascular emergencies, pyelonephritis, pancreatitis, new neoplasms, complicated urolithiasis or gynecologic emergencies. A second investigator reviewed 40 APCT reports to calculate inter-rater agreement for the outcomes of POA and POANCD.
Statistical analysis
The percentage of eligible encounters that included APCT was calculated for 2001–2009, and a Spearman’s correlation coefficient was used to determine the statistical significance of the percentage change over time. The individual CT diagnoses and the composite outcomes of POA and POANCD for 2001–2003 and 2007–2009 were calculated as percentage of the total eligible encounters. A Cohen’s kappa coefficient was calculated to determine inter-rater agreement for POA and POANCD. Patient characteristics and APCT findings were compared between 2001–2003 and 2007–2009, using robust variance estimates with generalized estimating equations to compute p-values. The robust variance estimates were used to account for repeated measures, as some patients had multiple visits within the 2001–2003 or 2007–2009 periods.
RESULTS
Subject and encounter characteristics
In 2001–2009, there were 1,572 ED encounters among 648 patients. Table 1 describes the patient characteristics. There were 86 different ED providers with a mean of 18.1 (SD 18.9) encounters per provider. Overall, 67% of ED encounters resulted in hospital admission.
Table 1.
Patient characteristics (n=648)
| Patient characteristic | Count (%) or Median (range) |
|---|---|
| Median age at first encounter (range) | 35.2 (18.0–87.8) |
|
| |
| Sex | |
| Female | 343 (52.9%) |
| Male | 305 (47.1%) |
|
| |
| Race | |
| White | 457 (70.5%) |
| Black | 166 (25.6%) |
| Other | 25 (3.9%) |
|
| |
| Number of ED encounters | |
| 1 | 380 (58.6%) |
| 2 | 108 (16.7%) |
| 3 | 52 (8.0%) |
| >3 | 108 (16.7%) |
| Range | 1–42 |
|
| |
| Number of ED APCTs from 2001–2009 | |
| 1 | 312 (59.8%) |
| 2 | 93 (17.8%) |
| 3 | 50 (9.6%) |
| >3 | 67 (12.8%) |
| Range | 1–21 |
|
| |
| Triage complaint* | |
| Abdominal pain | 1078 (68.6%) |
| Nausea or vomiting | 173 (11.0%) |
| Gastrointestinal bleed | 126 (8.0%) |
| Fever or chills | 84 (5.3%) |
| Diarrhea | 68 (4.3%) |
| Abdominal distention | 20 (1.3%) |
| Rectal pain | 16 (1.0%) |
| Small bowel obstruction | 7 (0.5%) |
Denominator is total number of ED encounters (n=1572) among the 648 patients
The number of ED encounters increased each year. At HUP, ED encounters increased from 78 in 2001 to 134 in 2009. At PPMC, ED encounters increased from 62 in 2003 to 112 in 2009. The admission rate at HUP was slightly higher than at PPMC (69.1 vs. 63.6%, p=.03), but there were no significant differences in patients’ age, sex, race, or chief complaint between the two centers.
Trends in APCT use
APCT was obtained in 69.1% of ED encounters among patients with CD who presented with a gastrointestinal triage complaint, and in 74.3% of encounters with a triage complaint of abdominal pain. APCT was obtained in 77.5% of ED encounters in which patients were admitted to the hospital and in 52% of encounters in which the patients were discharged.
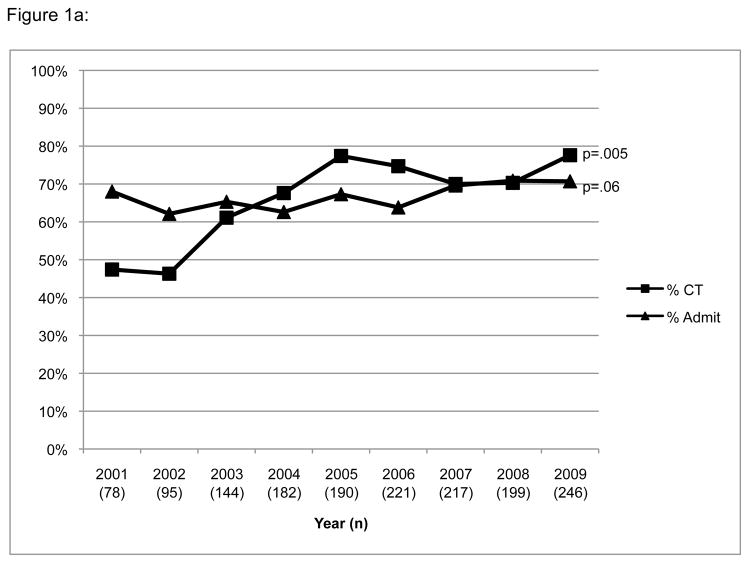
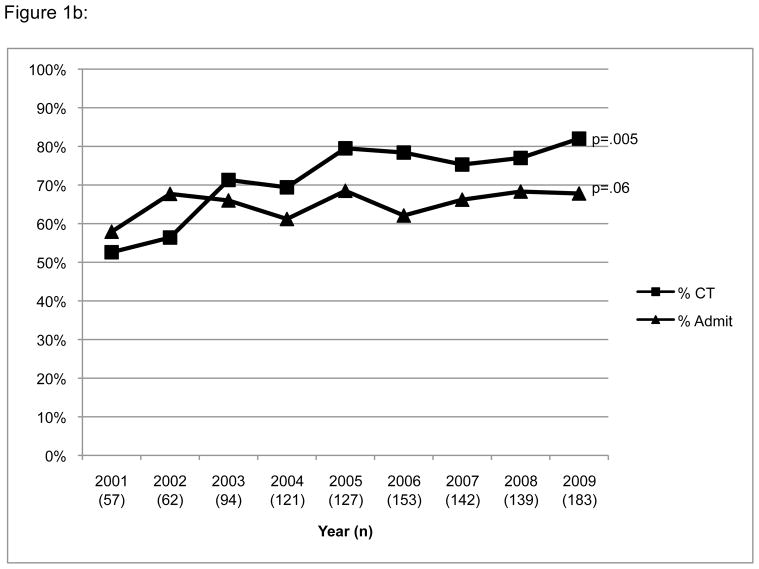
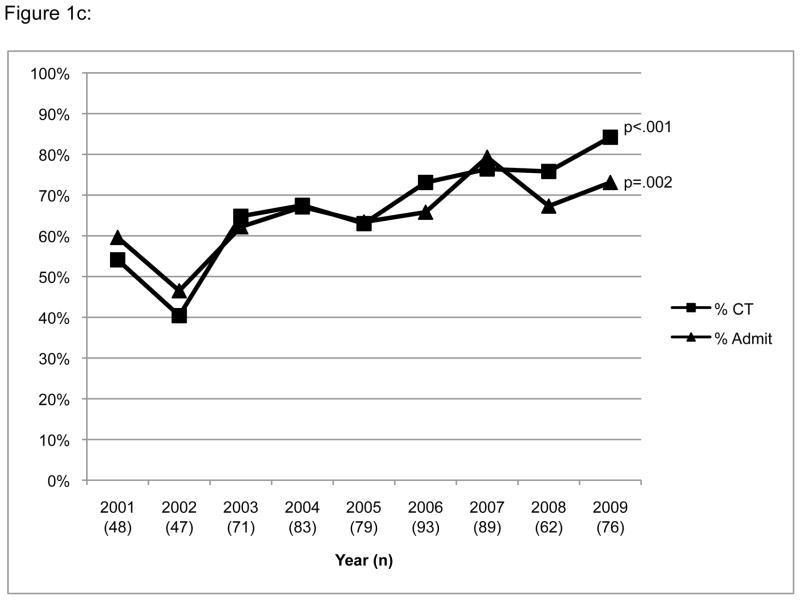
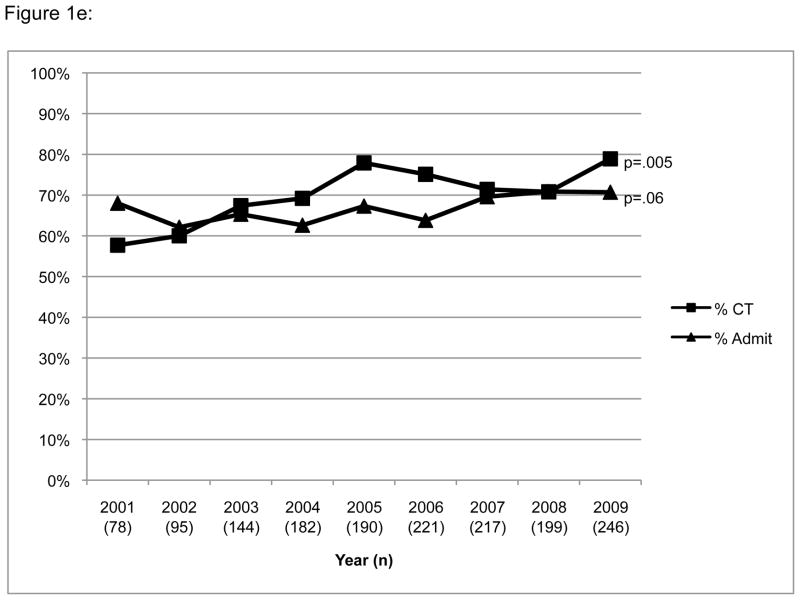
There was a significant increase in ED use of APCT from 47.1% in 2001 to 77.5% in 2009 (p=.005) (Figure 1a). Hospital admission rates, however, remained relatively stable. The results were similar when the analysis was limited to patients with abdominal pain (Figure 1b) and when limited to each patient’s first ED encounter (Figure 1c), except that admission rates increased over time when limited to the patient’s first encounter (p=.002).
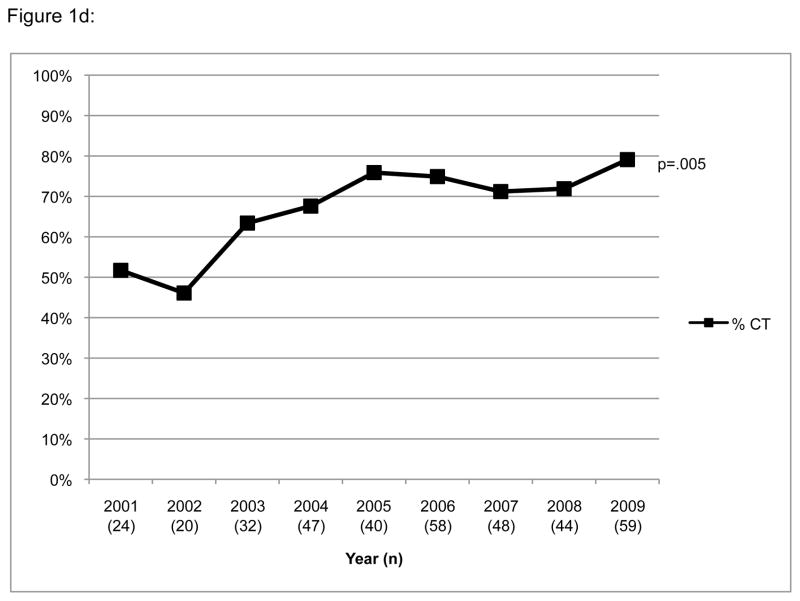
Figure 1.
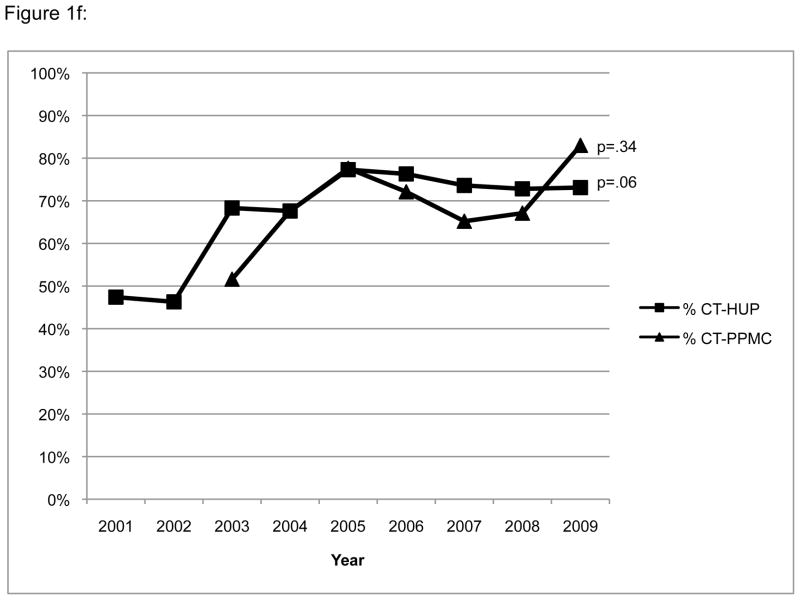
Trends in ED APCT use and hospital admission over time. This figure demonstrates the annual percentage of ED encounters during which an APCT was ordered, and the percentage of encounters that resulted in hospital admission from 2001–2009. In the overall population (a), and in the analysis limited to patients with abdominal pain (b), APCT use increased (p=.005) and admission rates remained relatively stable (p=.06). When limiting the analysis to the first ED encounter (c), APCT rates were slightly higher overall, and there were significant increases in APCT use (p<.001) and admission rates (p=.002) over time. Among patients with abdominal pain who were discharged (d), there was a significant rise in APCT use (p=.005). Including inpatient APCTs performed within two days of triage (e) resulted in findings similar to the primary analysis. Trends in APCT use stratified by study site (f) demonstrates a borderline significant increase in APCT use at HUP (p=.06), and a non-significant increase (p=.34) at PPMC.
Among the encounters with a triage complaint of abdominal pain that resulted in ED discharge (Figure 1d), there was a similar increasing trend over time (51.7% in 2001 to 79.1%, in 2009 p=.005) in APCT use.
To determine whether the trend of increasing APCT use could be attributed to increased availability of APCT in the ED in the later years, a sensitivity analysis included APCT ordered in the ED or during hospitalization within 2 days of triage. During the study period, there were 34 inpatient APCTs ordered within 2 days of triage among patients who did not undergo APCT in the ED. Including these APCTs in the outcome did not appreciably change the trend of increased APCT use over time (57.7% in 2001 to 78.5% in 2009, p=.005) (Figure 1e).
Figure 1f stratifies APCT rates by clinical site. The frequency of APCT use was similar at both sites. The test for trend over time did not reach statistical significance for PPMC, perhaps secondary to fewer years of observation. Furthermore, for the HUP site, the greatest increase in APCT use occurred from 2001–2003.
APCT Results
The characteristics of the patients with ED encounters that included APCT in the 2001–2003 versus 2007–2009 are compared in Table 2. There were no significant differences in sex, age, race or admission rate. Abdominal pain was the most common triage complaint, and the percentage of patients with this complaint did not change significantly over time. There was no significant difference in rates of triage complaints of nausea/vomiting, gastrointestinal bleeding, fever/chills, diarrhea or small bowel obstruction (data not shown). More patients had a triage complaint of abdominal distention in 2001–2003 vs. 2007–2009 (4.1% vs. 1.0%, p=.03), but the total number of patients with this complaint was only 12. In 2001–2003 vs. 2007–2009 visits, patients were more often taking aminosalicylates and narcotics, and less often using biologic drugs. There was no significant difference in antibiotic, immunomodulator or steroid use.
Table 2.
Characteristics of ED encounters that included APCT
| Characteristics | 2001–2003 (n=169) | 2007–2009 (n=482) | p-value |
|---|---|---|---|
| Female gender (%) | 53.2 | 52.1 | .86 |
|
| |||
| Median age (range), years | 37.1 (18.5–83.1) | 34.9 (18.3–84.8) | .13 |
|
| |||
| % Caucasian | 61.5 | 64.5 | .66 |
|
| |||
| Triage complaint abdominal pain (%) | 78.1 | 75.3 | .44 |
|
| |||
| Admission rate (%) | 72.8 | 78.2 | .17 |
|
| |||
| Home medications (%) | |||
| Aminosalicyates | 57.4 | 35.1 | .0001 |
| Steroids | 34.9 | 25.8 | .06 |
| Immunomodulators | 22.5 | 14.3 | .06 |
| Biologics | 6.5 | 19.5 | .003 |
| Antibiotics | 11.2 | 8.5 | .39 |
| Narcotics | 40.2 | 28.5 | .03 |
Table 3 describes the findings on the 169 APCTs in 2001–2003 and the 482 APCTs in 2007–2009. The Cohen’s kappa coefficient for inter-rater agreement on the outcomes of POA and POANCD was .79. POA and POANCD were found in 29.0% and 34.9% of APCTs, respectively. After adjusting for differences in medication use, there were no significant differences in the proportion of APCTs with POA (p=.92) or POANCD (p=.91) between the two time periods (Table 4). The results were similar in analyses limited to the patient’s first ED encounter (POA- 28.6% in 2001–2003 vs. 29.7% in 2007–2009, p=.83 and POANCD – 38.1% in 2001–2003 vs. 36.7% in 2007–2009, p=.81), ED encounters for abdominal pain (POA – 31.1% vs. 28.4%, p=.59 and POANCD – 37.9% vs. 35.3%, p=.63), or if we included new or worsening bowel wall thickening in the outcome (POA – 55.6% vs. 63.7%, p=.31 and POANCD – 60.9% vs. 66.8%, p=.50).
Table 3.
Abdominopelvic CT Results (n=651)
| Finding | Number (%) |
|---|---|
| Bowel wall thickening* | 322 (49.5) |
|
| |
| Obstruction | 130 (20.0) |
|
| |
| Fistula* | |
| Perianal | 13 (2.0) |
| Other | 46 (7.1) |
|
| |
| Abscess (not perianal) or perforation* | 67 (10.3) |
|
| |
| Perianal abscess* | 3 (0.5) |
|
| |
| Pneumonia | 14 (2.1) |
|
| |
| Urolithiasis | 12 (1.8) |
|
| |
| Appendicitis | 4 (0.6) |
|
| |
| Non-intestinal neoplasm** | 4 (0.6) |
|
| |
| Gynecologic emergency | 4 (0.6) |
|
| |
| Pyelonephritis | 4 (0.6) |
|
| |
| Diverticulitis | 3 (0.5) |
|
| |
| Cholecystitis | 3 (0.5) |
|
| |
| Pancreatitis | 3 (0.5) |
|
| |
| Intestinal ischemia | 3 (0.5) |
|
| |
| Colon cancer | 3 (0.5) |
|
| |
| Vascular emergency | 2 (0.3) |
|
| |
| POA*** | 189 (29.0) |
|
| |
| POANCD**** | 227 (34.9) |
Worse or new compared with prior APCT
Renal cell carcinoma (1), Lung carcinoma vs. metastasis (2), PTLD vs. lymphoma (1), pancreatic mass (1)
Perforation, obstruction or abscess
Perforation, obstruction, abscess, complicated urolithiasis, appendicitis, neoplasm, gynecologic emergency, pyelonephritis, diverticulitis, cholecystitis, pancreatitis, intestinal ischemia, vascular emergency
Table 4.
Abdominopelvic CT results in 2001–2003 and 2007–2009
| 2001–2003 (n=169) | 2007–2009 (n=482) | P value* | |
|---|---|---|---|
| Inflammation or bowel wall thickening | 65(38.5%) | 257 (53.3%) | .003 |
|
| |||
| Obstruction | 35 (20.7%) | 95 (19.7%) | .90 |
|
| |||
| Abscess or perforation | 17 (10.1%) | 50 (10.4%) | .12 |
|
| |||
| Fistula | |||
| Perianal | 4 (2.4%) | 9 (1.9%) | .36 |
| Other | 17 (10.1%) | 29 (6.0%) | .20 |
|
| |||
| Non-CD urgent/emergent diagnoses | 11 (6.5%) | 34 (7.0%) | .99 |
|
| |||
| POA | 51 (30.2%) | 138(28.6%) | .92 |
|
| |||
| POANCD | 61 (36.1%) | 166 (34.4%) | .91 |
Multivariable model adjusted for differences in aminosalicylate and biologic medication use
We conducted additional analyses to assess for the effect of age on the outcomes. Patients under the age of 60 comprised 92% of the patients who underwent APCT. When using age cutoffs of 40, 50 and 60, there was a statistically significantly higher rate of POA and POANCD in the older age groups. However, among these different age groups, there was no statistically significant difference in the rates of POA or POANCD in the 2001–2003 vs. 2007–2009 time periods (p>.2 for all comparisons).
We conducted secondary analyses to assess for potential bias introduced by the missing 2001–2002 data for the PPMC study site. Using robust variance estimates to calculate p-values, there was no significant difference in the rate of APCT use between the study sites (p=.74). The rates of POA and POANCD between the study sites were also nearly identical (data not shown). Thus, missing data from PPMC in 2001–2002 are unlikely to have significantly biased the results.
DISCUSSION
This study clearly demonstrates increasing APCT use in the ED in patients with CD. This trend is consistent with national trends of increasing use of CT in ED patients in general16 and specifically in ED patients with abdominal pain17. In a national sample of ED patients with abdominal pain, the annual rates increased from 10.1% to 22.5% between 2001 and 200517. The rates in the present study of 47% in 2001 and 77% in 2005 were expectedly higher, given our population included only patients with CD. Since patients with CD have a chronic disease that leads to higher lifetime radiation exposure and frequent ED visits, the high rate of APCT use is of greater potential concern than use in the general ED population.
Despite the increase in ED APCT use in this population, admission rates remained relatively stable over time. This finding suggests that the increasing APCT use is not explained by a worsening in CD severity among ED patients. Similarly, the stable rate of urgent APCT diagnoses also suggests that worsening disease severity does not explain the rising rate of APCT use. Furthermore, accounting for the 34 APCTs performed shortly after hospitalization did not appreciably change the results, indicating that the rate of APCT use is truly rising rather than shifting from the inpatient to ED setting as a result of increasing ED availability of APCT.
If the increase in APCT use was truly unwarranted, one might expect the proportion of normal APCTs to increase with a corresponding decrease over time in the frequency of urgent APCT findings. However, this dilutional effect could be countered by advances in CT technology that occurred during the study period. In 2006 at PPMC and in late 2003 at HUP, new CT scanners were installed, and multiplanar CT imaging was incorporated into routine CT interpretation. These and other advances afforded by the improved scanning instruments could have improved the sensitivity of APCT to detect subtle microperforations, fistulae, obstructions and abscesses. Thus there could have been both a lower threshold to order CT as well as an increased sensitivity for POA and POANCD in the later years, thereby resulting in a stable rather than decreased proportion of APCTs with POA and POANCD in 2007–2009 compared with 2001–2003. Another explanation for the stable proportion of APCTs with POA and POANCD despite the increased rate of APCT use is that the CD severity among the ED patients increased over time, albeit we would have expected increasing admission rates were this the case.
The highest rates of APCT use and the most dramatic increase in use over time were observed when limiting the analysis to the first ED encounter during the study period. There was also a significant increase in admission rates when limiting the analysis to the first ED encounter. This analysis minimizes the effect of patients who are frequent ED visitors. The likely explanation for this finding is that frequent ED visitors may lack primary care and use the ED for minor gastrointestinal complaints, or may exhibit drug-seeking behavior. Furthermore, frequent ED visitors may have had APCT during recent visits and thus the providers may have deemed APCT to be unnecessary or not worth the potential risks of radiation and contrast exposure. There were stable rates of POA and POANCD in 2001–2003 versus 2007–2009 among first ED encounters, so the increased rates of APCT and hospital admission are less likely to be explained by an increase in the number of patients with more severe CD in later years.
This study is also novel in documenting the APCT findings among patients with CD who present to the ED. A 1987 study of 80 patients with CD who underwent CT found that unexpected findings changed patient management in 28% of cases19. Our overall rates of 29% for POA and 34.9% for POANCD were slightly higher, which may be explained by the increasing sensitivity of CT over time and the inclusion of only ED patients. Although the prevailing sentiment is that APCT is overused in the ED, it could be argued that the increasing rate of testing may be justifiable in a population where one-third of ED APCTs reveal urgent diagnoses.
It is also important to note that the APCT ordering pattern in the ED does not exclusively reflect the medical decision-making of ED providers. Some APCTs were likely requested by the consulting gastroenterologist, surgeon or admitting team. Therefore, efforts to bring evidence-based decision-making to ED APCT use among patients with CD should target all providers who care for patients with CD.
A potential study limitation is that the university medical center setting may not be generalizable to other ED settings. The patients at tertiary referral centers may be sicker, and practice patterns may differ from a community setting. In an academic setting, CT scans may be ordered more frequently because of the training environment, or less frequently because of increased experience in assessing patients with CD. However, our study included two different hospitals, both of which serve as community hospitals for local residents and tertiary referral centers. Furthermore, there were 86 ED providers during the study period, and all providers were unlikely to follow the same ordering behavior. In addition, our results are consistent with two prior studies of ED APCT use in nationally representative samples16, 17.
Our primary definition of significant APCT findings did not include bowel wall thickening, which could represent acute inflammation or fibrosis. In this study, bowel wall thickening was noted in approximately 50% of APCTs. However, this finding may also be seen in asymptomatic patients with CD. In contrast, the diagnoses included in POA and POANCD require specific medical or surgical management and can potentially worsen if the patient is simply treated for a CD flare. Furthermore, we elected not to include bowel wall thickening in the outcome since radiation-free tests such as colonoscopy or MR enterography can be used to establish this diagnosis on a less emergent basis.
Although there has been a significant increase in APCT use over time with stable rates of urgent diagnoses, the yield of APCT in this population of patients with CD has remained high. In 2007–2009, 34% of the APCTs detected urgent or emergent diagnoses. These numbers reflect the fact that patients with CD are at high risk for complications given the nature of the disease and the risks of immunosuppression. Furthermore, a normal APCT is often useful in the ED when making triage decisions. There have been mandates from the federal government14 and within the field of gastroenterology15 to reduce unnecessary radiation exposure from diagnostic imaging in all patients, as well as in CD patients in particular20. Although radiation exposure in patients with CD is a concern, clinicians must also weigh the risk of missing a potential urgent diagnosis when they forego a CT. Our findings reflect a high yield of significant disease among patients with CD for whom a provider felt that an APCT was warranted. Nonetheless, two-thirds of patients without POA or POANCD could potentially have avoided radiation exposure. Further research is needed to determine if clinical predictors can identify patients at low risk for POA and POANCD in order to allow clinicians to make evidence-based decisions regarding use of APCT.
Acknowledgments
Grant Support: National Institutes of Health T32-DK007740 and K24-DK078228
Abbreviations
- APCT
Abdominopelvic computed tomography
- CD
Crohn’s disease
- CT
Computed tomography
- ED
Emergency department
- EMTRAC
Emergency Medicine Tracking and Charting System
- HUP
Hospital of the University of Pennsylvania
- ICD
International Classification of Diseases
- IBD
Inflammatory bowel disease
- PICARD
Pennsylvania Integrated Clinical and Research Database
- POA
Perforation, obstruction or abscess
- POANCD
Perforation, obstruction, abscess or non-Crohn’s disease related urgent or emergent abdominopelvic computed tomography findings
- PPMC
Penn Presbyterian Medical Center
- SD
Standard deviation
- UPHS
University of Pennsylvania Health System
Footnotes
Disclosures: The authors have no financial, professional or personal conflicts of interest that are relevant to the manuscript
Writing assistance: None provided
Author contributions: Caroline Kerner conceived of the project, wrote the research proposal and the IRB application and was involved in all aspects of data collection and data analysis. Caroline Kerner also wrote the first draft of the paper. Kathleen Carey abstracted data including all of the results from the CT reports. Angela Mills provided extensive feedback for the research proposal, assisted with access to and interpretation of the data, and extensively edited the manuscript. Wei Yang was the statistics mentor for the project, and advised Caroline Kerner regarding the statistical analyses. Marie Synnestvedt and Mark Weiner created the database for the study. Susan Hilton devised the coding system for the CT results and provided feedback about the radiologic aspects of the research proposal and manuscript. James Lewis mentored Caroline Kerner through all aspects of the project and was extensively involved in advising her regarding the research proposal, data collection and analysis, and manuscript editing.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Caroline Kerner, University of Pennsylvania Division of Gastroenterology, Philadelphia, PA.
Kathleen Carey, University of Pennsylvania School of Medicine, Philadelphia, PA.
Angela M. Mills, Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA.
Wei Yang, Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia, PA.
Marie B. Synnestvedt, Office of Human Research, University of Pennsylvania, Philadelphia, PA.
Susan Hilton, Department of Radiology, University of Pennsylvania, Philadelphia, PA.
Mark G. Weiner, Department of Medicine, University of Pennsylvania, Philadelphia, PA.
James D. Lewis, Gastroenterology Division and Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia, PA.
References
- 1.Sleisenger MH, Feldman M, Friedman LS, Brandt LJ. Sleisenger & Fordtran’s gastrointestinal and liver disease: pathophysiology, diagnosis, management. 8. Philadelphia: Saunders; 2006. [Google Scholar]
- 2.Carucci LR, Levine MS. Radiographic imaging of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:93–117. ix. doi: 10.1016/s0889-8553(01)00007-3. [DOI] [PubMed] [Google Scholar]
- 3.Mehran R, Nikolsky E. Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int Suppl. 2006:S11–5. doi: 10.1038/sj.ki.5000368. [DOI] [PubMed] [Google Scholar]
- 4.Berrington de Gonzalez A, Mahesh M, Kim K-P, et al. Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007. Arch Intern Med. 2009;169:2071–7. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 6.Council NR. Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. Washington, D.C: National Academies Press; 2006. [PubMed] [Google Scholar]
- 7.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361:849–57. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation Dose Associated With Common Computed Tomography Examinations and the Associated Lifetime Attributable Risk of Cancer. Arch Intern Med. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desmond AN, O’Regan K, Curran C, et al. Crohn’s disease: factors associated with exposure to high levels of diagnostic radiation. Gut. 2008;57:1524–9. doi: 10.1136/gut.2008.151415. [DOI] [PubMed] [Google Scholar]
- 10.Kroeker K, Lam S, Birchall IW, Fedorak RN. Patients with IBD Are Exposed to Potentially Serious Excesses of Ionizing Radiation. Digestive Disease Week; 2009 June 1, 2009; Chicago, Illinois. 2009. [Google Scholar]
- 11.Peloquin JM, Pardi DS, Sandborn WJ, et al. Diagnostic ionizing radiation exposure in a population-based cohort of patients with inflammatory bowel disease. Am J Gastroenterol. 2008;103:2015–22. doi: 10.1111/j.1572-0241.2008.01920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levi Z, Fraser E, Krongrad R, et al. Factors associated with radiation exposure in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2009;30:1128–36. doi: 10.1111/j.1365-2036.2009.04140.x. [DOI] [PubMed] [Google Scholar]
- 13.Bhargavan M, Sunshine JH. Utilization of radiology services in the United States: levels and trends in modalities, regions, and populations. Radiology. 2005;234:824–32. doi: 10.1148/radiol.2343031536. [DOI] [PubMed] [Google Scholar]
- 14.Administration USFaD; Health CfDaR. Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging. 2010. [Google Scholar]
- 15.Katz PO, Kefalas CH. Re: Device Improvements to Reduce Unnecessary Radiation Exposure from Medical Imaging; Requests for Comments (FDA-2010-N-0080) Bethesda, MD: American College of Gastroenterology; 2010. Apr 15, p. 2010. [Google Scholar]
- 16.Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP. National Trends in CT Use in the Emergency Department: 1995–2007. Radiology. 2011;258:164–73. doi: 10.1148/radiol.10100640. [DOI] [PubMed] [Google Scholar]
- 17.Pines JM. Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain. Med Care. 2009;47:782–6. doi: 10.1097/MLR.0b013e31819748e9. [DOI] [PubMed] [Google Scholar]
- 18.Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Trends in ambulatory and emergency room visits for inflammatory bowel diseases in the United States: 1994–2005. Am J Gastroenterol. 2010;105:363–70. doi: 10.1038/ajg.2009.580. [DOI] [PubMed] [Google Scholar]
- 19.Fishman EK, Wolf EJ, Jones B, Bayless TM, Siegelman SS. CT evaluation of Crohn’s disease: effect on patient management. AJR Am J Roentgenol. 1987;148:537–40. doi: 10.2214/ajr.148.3.537. [DOI] [PubMed] [Google Scholar]
- 20.Sahani DV, Kambadakone AR. Crohn’s disease and radiation exposure: it’s time we got our act together? Inflamm Bowel Dis. 2009;15:1278–80. doi: 10.1002/ibd.20836. [DOI] [PubMed] [Google Scholar]