Abstract
Purpose
To stratify complications of percutaneous nephrolithotomy (PCNL) in a single, tertiary hospital by use of the modified Clavien system.
Materials and Methods
From May 1987 to December 2010, 1,236 cases of PCNL were performed at our institute. Medical records were available for 826 cases of PCNL from 698 patients, from February 1995 to December 2010. Using multiple factors, we retrospectively reviewed and analyzed 698 patients for complication rates classified by the modified Clavien grading system, along with success rates.
Results
In 698 patients, staghorn stone patients accounted for 33.8% (236 patients). Initial and overall stone-free rates were 69.9% and 88.8%. A total of 297 complications were documented in 282 patients. According to the modified Clavien classification, grade I, II, IIIa, IIIb, IVa, IVb, and V complications were observed in 88 (12.6%), 145 (20.8%), 31 (4.4%), 5 (0.7%), 6 (0.9%), 4 (0.6%), and 3 (0.4%) patients, respectively. Transient peri-nephrostomy catheter urine leakage (15.2%) was the most common complication, followed by transient fever >38° (11%) and transfusion (6.9%). Other individual complications occurred in less than 1.5% of cases. In patients with staghorn stones, grade I, II, IIIb, and IVa complications were significantly more common, and all grade IVb and V complications occurred in patients with staghorn stones.
Conclusions
The modified Clavien classification provides a standardized grading system for complications of PCNL, although consensus on specific complications would prompt better comparison between centers. A shorter operation time is imperative to achieve less bleeding. Previous stone-related fever and staghorn stones are significant contributing factors for developing postoperative fever.
Keywords: Complications; Nephrostomy, percutaneous; Treatment outcome
INTRODUCTION
Numerous procedures are now available for the management of urinary stones. For the management of upper urinary calculi, the method of dilating the tract after percutaneous renal puncture to specifically remove urinary calculi was first established in 1976 by Fernstrom and Johansson [1]. Advances in surgical technique and equipment have further contributed to percutaneous nephrolithotomy (PCNL) becoming the recommended primary treatment option for most patients with large-volume renal and staghorn calculi [2].
The outcomes of PCNL can be interpreted in terms of success and complication rates. "Success" is often defined as the absence of residual stone fragments under conventional X-ray or computed tomography (CT) or when clinically insignificant residual fragments (CIRF) are observed. Although large-series PCNL results have been reported in the literature, standardized evaluation of "complications" is lacking. Recent attempts to report complication rates of PCNL have focused on stratifying them by severity by use of the Clavien grading system. First proposed in 1992 and modified in 2004, the modified Clavien grading system has been validated in a cohort of 6,336 patients [3,4].
In this article, we retrospectively reviewed our experience with PCNL to grade perioperative complications according to the modified Clavien classification.
MATERIALS AND METHODS
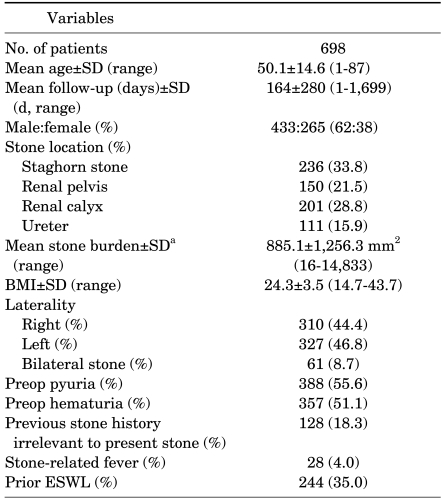
From May 1987 to December 2010, 1,236 cases of PCNL from 1,066 patients were performed in our center. Among these patients, medical records were available from February 1995 to December 2010. In this study, we retrospectively reviewed and analyzed 826 cases of PCNL from 698 patients, after the first 410 cases of PCNLs had already been performed. The stone was classified as a staghorn stone if a renal pelvic stone had calyceal branching into the major calyx [5]. Owing to the tertiary hospital setting of our center, numerous patients were referred from other hospitals, and 35% of patients had undergone prior extracorporeal shock wave lithotripsy therapy and 34% of patients were diagnosed as having staghorn stones. The patients' characteristics are further described in Table 1.
TABLE 1.
Patient characteristics
BMI: body mass index, ESWL: extracorporeal shock wave lithotripsy, a: Surface area (length x height)
All patients underwent preoperative laboratory exams, including blood tests and urinalysis. All patients also underwent simple X-ray of the kidney-ureter-bladder, along with CT or intravenous urography. Once the operation day was chosen, third-generation oral cephalosporin or quinolone was administered for more than 5 days to prevent postoperative sepsis, if pyuria was present in the urinalysis.
With the patient under general endotracheal anesthesia, a 5 to 6 Fr occlusion balloon catheter was inserted in the ipsilateral ureter, which later allowed for injection of contrast material for opacification and distension of the collecting system to aid in making an appropriate puncture. After ureteral catheterization, the patient's position was changed to the prone position on a C-arm compatible table. Once access was gained with a sheathed needle, the stylet was removed and a guidewire was inserted, through which tract dilatation was performed with either an Amplatz dilator or a dilating balloon catheter (Cook Urological Inc., Indianapolis, IN, USA). Using a rigid nephroscope, stone fragmentation using ballistic or ultrasonic devices was done and the stone was evacuated by using forceps. Although some question the need for a nephrostomy catheter, it was routinely inserted for tamponade of bleeding and urine drainage in our center [6,7].
The success rate was defined as the absence of residual stone fragments under conventional X-ray or CT or when CIRF was observed. CIRF was defined as residual fragments that were smaller than 4 mm, asymptomatic, nonobstructive, and noninfectious [8]. Success was further classified as the initial stone-free rate, which was evaluated immediately after a single PCNL procedure, and the overall stone-free rate, which was evaluated 3 months after the initial PCNL and further ancillary procedure had been performed.
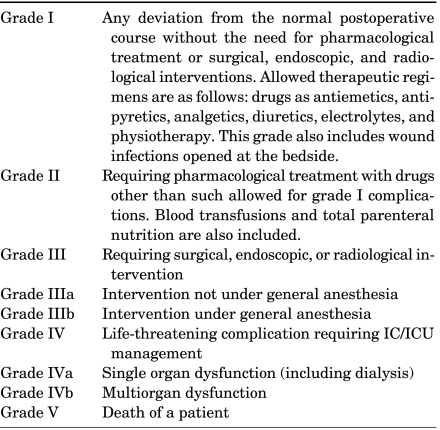
Perioperative complications were classified by using the modified Clavien system, which was stratified into five grades (Table 2). Past medical history such as hypertension (n=221), diabetes (n=105), pulmonary tuberculosis (n=30), cerebrovascular accident (n=21), and skeletal abnormalities (n=12) were included as variables. Urologic anatomical factors such as diverticular stone (n=42), ureteropelvic junction obstruction (n=25), single kidney (n=13), megaureter (n=9), duplicated ureter (n=5), horseshoe kidney (n=4), and infundibular stricture (n=3) were also entered as variables. A p-value <0.05 in the multivariate logistic regression analysis was considered significant. Odds ratios (ORs) and 95% confidence intervals (CIs) are presented. All analyses were performed by using the SAS System for Windows ver. 9.1 (SAS Institute Inc, Cary, NC, USA).
TABLE 2.
Classification of surgical complications according to the modified clavien grading system
IC: intermediate care, ICU: intensive care unit
RESULTS
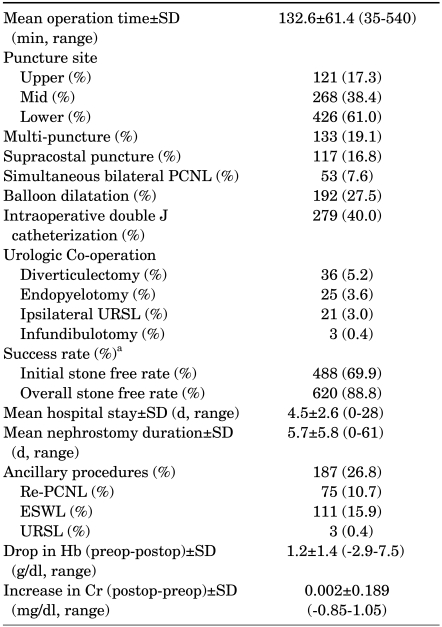
Perioperative data are listed in Table 3. The initial stone-free rate was 69.9% (488 patients), and the overall stone-free rate was 88.8% (620 patients). The mean hospital stay was 4.5±2.6 days after the operation. The lowest initial success rate was observed in the staghorn stone group (46%, p<0.0089). Furthermore, mean operation time (157.91±76.85 days, p<0.0037) and hospital stay (5.18±3.12 days, p<0.0095) were significantly longer in the staghorn stone group.
TABLE 3.
Peri- and postoperative data
PCNL: percutaneous nephrolithotomy, URSL: ureterorenoscopic lithotripsy, ESWL: extracorporeal shock wave lithotripsy, Hb: hemoglobin, Cr: creatinine, a: Based on simple X-ray
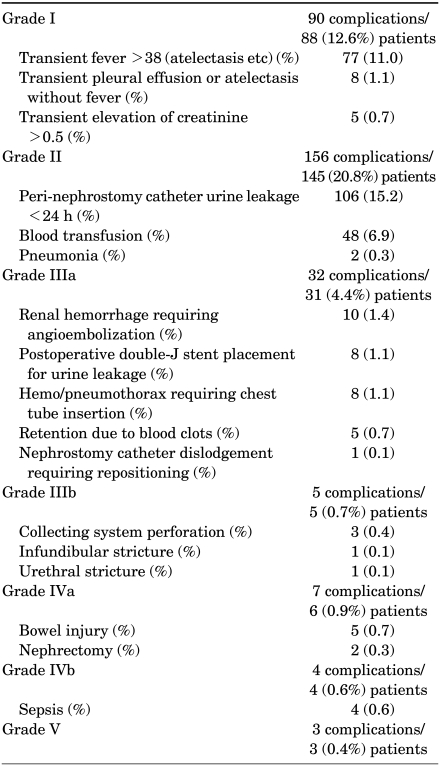
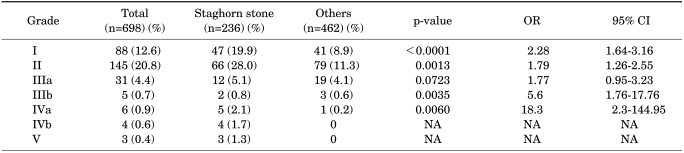
Table 4 lists postoperative complications classified by the modified Clavien grading system. A total of 297 complications were documented. Grade I complications were recorded in 88 (12.6%), grade II in 145 (20.8%), grade IIIa in 31 (4.4%), grade IIIb in 5 (0.7%), grade IVa in 6 (0.9%), grade IVb in 4 (0.6%), and grade V in 3 (0.4%) patients.
TABLE 4.
Complications
Transient peri-nephrostomy catheter urine leakage for less than 24 hours, requiring only simple dressing, was observed in 106 (15.2%) patients. Fever, defined as at least a single episode spiking more than 38℃, was the next common complication (77 patients, 11.0%). Transfusion was required in 48 patients (6.9%). Other individual complications accounted for less than 1.5%. Comparison of complications between staghorn stone patients and others are outlined in Table 5. Grade I, II, IIIb, and IVa complications were significantly more common in the staghorn stone group. All grade IVb and V complications occurred in staghorn stone patients.
TABLE 5.
Comparison of complications between staghorn stone patients and others as stratified by the modified clavien system
OR: odds ratio, CI: confidence interval, NA: not applicable
All four patients who developed postoperative sepsis were staghorn stone patients. All four patients had both pyuria and hematuria in preoperative urinalysis, and thus preoperative oral antibiotics were given for more than 5 days. None of these patients were febrile before the operation.
Three patients with staghorn stones died after PCNL. Of the two patients who died of septic shock, one eventually developed brain edema after continuous renal replacement therapy. The other patient who died of septic shock had a history of Parkinson's disease and eventually developed stress-induced cardiomyopathy. One patient died from hypoxemia and respiratory acidosis caused by pulmonary embolism despite mechanical ventilation.
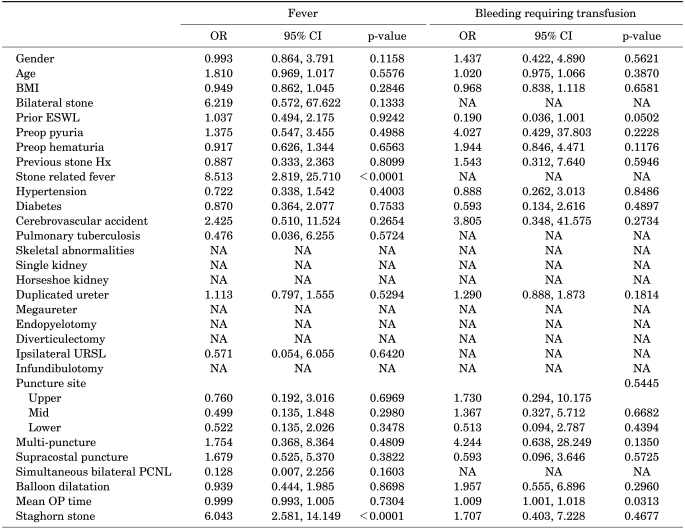
To identify determinants of each complication, multivariate analysis was performed. Prior stone-related fever and staghorn stones were found to be significant contributing factors for postoperative fever >38℃. Mean operation time was found to be significant for bleeding requiring transfusion (Table 6). For other objective complications (embolization, chest tube insertion, collecting system perforation, bowel injury, nephrectomy, sepsis, death), determinants could not be identified because of the small number of cases. To identify risk factors for developing complications classified as grade IIIa or greater according to the Clavien system, multivariate logistic regression analysis was performed by using the same variables. Only operation time was considered a significant contributing factor in the univariate analysis (OR, 0.994; 95% CI, 0.989-0.999; p=0.0255), but it failed to remain a significant factor in the multivariate analysis (OR, 0.993; 95% CI, 0.984-1.000; p=0.1071).
TABLE 6.
Multivariate determinants for postoperative fever >38° and bleeding requiring transfusion
OR: odds ratio, CI: confidence interval, BMI: body mass index, NA: not applicable, URSL: Ureterorenoscopic lithootripsy, ESWL: extracorporeal shock wave lithotripsy, PCNL: percutuneous nephrolithotomy, OP: operation
DISCUSSION
Percutaneous nephrolithotomy is an established technique used to treat large and complex renal calculi [9]. The 2005 American Urological Association (AUA) and 2008 European Association of Urology (EAU) guidelines on the management of staghorn calculi recommend PCNL as the first-line treatment for staghorn calculi, any renal stone that exceeds 20 mm in diameter, and lower calyceal stones [2,10].
In Korea, the first PCNL was performed in July 1984 by Koh et al [11]. Since May 1987, our center has begun to treat calculi of the upper urinary tract by use of the PCNL technique. In the first 50 cases, the complication rate reached 53.1%, compared with 20% after the initial 50 patients. At that time, we attributed the complication rates mainly to inexperience and improper technique [12].
The most recent Korean report of PCNL performed in single large center was published in 2009 by Kwon et al [13]. In their retrospective report comprising 610 patients, the initial stone-free rate was 57.6% and the overall stone-free rate was 84.9%. In our center, these were 69.9% and 88.8%, respectively. Transfusion was required in 8.7% of patients, similar to the 6.9% in our study. Chest tube insertion for thoracic complications was necessary in 1.1% of cases, which was the same as in our study. Bleeding requiring embolization occurred in 0.8% and sepsis occurred in 1.0% (vs. 1.4% and 0.6% in our study).
Reporting a surgical outcome requires not only success rates, but also complication rates. Success rates in PCNL are easily defined and most articles use the concept of CIRF to define success. However, defining complications is difficult, and without a standardized method of classifying them, comparing complication rates in one study with those in another may be problematic, especially when certain factors are not classified as complications, such as fever or urine leakage.
To compare overall complication rates and the severity of complications, a standard grading system has been adopted. In the field of urology, the Clavien system has been applied to radical prostatectomy [14-16] and radical cystectomy [17]. Tefekli et al first adopted the modified Clavien classification system to stratify complications of PCNL in 2007 [18]. In their series of 811 PCNLs, Tefekli et al reported overall complications in 29.2% (vs. 33.4% in our study) [18]. Grade I, II, IIIa, IIIb, IVa, IVb, and V complications occurred in 4%, 16.3%, 6.6%, 2.8%, 1.1%, 0.3%, and 0.1%, respectively. Recently, de la Rosette et al collected prospective data from the Clinical Research Office of the Endourological Society (CROES) for 5,803 consecutive patients who were treated with PCNL at centers around the world during November 2007 through December 2009 [19]. In their report, the distribution of scores in the modified Clavien grade was I (11.1%), II (5.3%), IIIa (2.3%), IIIb (1.3%), IVa (0.3%), IVb (0.2%), and V (0.03%). Staghorn stones were present in 27.5% of patients, compared with 33.8% in our study. In their report, however, the number of specific complications in each grade was not provided.
Tefekli et al accounted for the lower incidence of grade I complications in their study as being biased by the retrospective nature of their study and the omission of certain minor complications [18]. In our study, grade I complications were evident in 14% of patients. The most common grade I complication in our study was fever, occurring in up to 11% of cases. In a study by Tefekli et al fever accounted for 2.8% of complications [18]. They attributed such a low incidence of fever to the use of prophylactic antibiotics and the separate classification of other complications that may cause fever (i.e., blood transfusion, sepsis, etc). We also used prophylactic antibiotics in patients with pyuria, but did not distinguish transient fever that may have been caused by events such as blood transfusion, because that may further contribute to selection bias in a retrospective study such as ours. In the CROES study, fever of more than 38.5 degrees occurred in 10.5% of cases, similar to our study [19]. In the literature, fever is reported in up to 32% of cases after PCNL [20]. Both the AUA and EAU guidelines recommend antibiotic prophylaxis for all patients who are undergoing PCNL [21,22]. The AUA guidelines report the benefits of a single dose of antibiotics. Because we have observed death from septic shock, the importance of preoperative antibiotics cannot be emphasized enough.
Grade II complications occurred in 22.3% of our patients, and most were transient peri-nephrostomy catheter urine leakage (15.2%). This complication was managed by simple dressing only, but prolonged the hospitalization period (5.48±3.31 days vs 4.35±2.38 days, p<0.05) and therefore was classified as a grade II complication, as in the study by Tefekli et al [18]. However, transient urine leakage occurred in only 4% of cases in a report by Tefekli [18]. Again, the retrospective design of both studies may contribute to such differences because such minor complications may have been omitted during data collection.
Blood transfusion, the second most common grade II complication, was necessary in 6.9% of cases in our study. Perhaps the most significant complication of PCNL, bleeding requiring transfusion has been reported to have an incidence as high as 23% [23]. In the CROES study, transfusion was administered in 5.7% of patients [20]. Bleeding can occur in every step of PCNL from percutaneous access to tract dilation to stone disintegration [24]. This may be why in our series, only the mean operation time was found to be significant for bleeding requiring transfusion [25].
Moreover, 8 patients (1.1%) in our study required selective angioembolization because of uncontrolled bleeding. We could not identify any risk factors in the multivariate analysis because of the relatively small number of patients. However, El-Nahas et al, in their retrospective study of 3,878 PCNLs to identify risk factors for extensive post-PCNL hemorrhage requiring selective embolization, found that upper calyceal puncture, solitary kidney, staghorn stone, multiple punctures, and inexperienced surgeon were significant risk factors. The incidence of extensive post-PCNL hemorrhage was 1% in their study [26]. A similar study by Srivastava et al reported that 1.4% of patients required angiography or embolization for bleeding control. They concluded that only stone size was a significant risk factor [27].
In our study, grade IIIb, IVa, IV, and V complications were extremely rare, each occurring in less than 1% of patients. In fact, the probability of developing a complication of a grade higher than IIIb in our center was only 2.6% (18/698). Two patients had undergone nephrectomy, one because of uncontrolled bleeding and the other because of xanthogranulomatous pyelonephritis.
The conclusions of this study may be limited by its retrospective design. A few variables were missed during data collection, and this may have contributed to selection bias. Another flaw of this retrospective study is that very few patients underwent postoperative CT imaging, because of its cost-effective nature in the clinical setting. Because our definition of success mainly depended on plain X-ray films and the need for CT imaging was based mainly on the patient's symptoms and laboratory findings, some unsuccessful PCNLs may have been misclassified as successful. In the literature, these limitations are apparent in most retrospective reports concerning outcomes of PCNL.
Although the modified Clavien classification provides an objective, stratified grading system for complications, there are some drawbacks. For instance, there is a debate over whether to include ancillary treatments as grade IIIa/b complication [18]. Furthermore, when comparing the complication rate from one center to another, certain minor complications such as atelectasis or urine leakage may not have been recorded. Therefore, we believe that a consensus is needed to specify certain complications that should not be omitted. Some may assume that certain complications, especially those classified in lower grades, are inherent to general anesthesia or the operation itself. Although accurate for obvious complications in higher grades, the disparity in lower-grade complications between centers can be partly explained by this phenomenon.
CONCLUSIONS
The modified Clavien system provides excellent classification of complications of PCNL stratified by their severity. A consensus in describing minor complications and in whether to include ancillary treatment, along with prospective data collection, may facilitate this classification becoming the most objective, unified classification system yet known.
The risks of developing clinically significant complications, such as bowel injury, sepsis, and death, remain low. Patients with previous stone-related fever and staghorn stone patients are at risk of developing postoperative fever. Blood and urine cultures should be obtained in these patients preoperatively to facilitate targeted antibiotic therapy, especially when sepsis develops. A shorter operation time, and thus less manipulation of the pelvocaliceal system, is necessary to achieve less bleeding. Therefore, a skilled surgical team and proper equipment are imperative.
Footnotes
The authors have nothing to disclose.
References
- 1.Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10:257–259. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 2.Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolfe JS, Jr AUA Nephrolithiasis Guideline Panel. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 3.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complication of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 4.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of a 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Nahas AR, Eraky I, Shokeir AA, Shoma AM, El-Assmy AM, El-Tabey NA, et al. Long-term results of percutaneous nephrolithotomy for treatment of staghorn stones. BJU Int. 2011;108:750–754. doi: 10.1111/j.1464-410X.2010.09942.x. [DOI] [PubMed] [Google Scholar]
- 6.Etemadian M, Soleimani MJ, Haghighi R, Zeighami MR, Najimi N. Does bleeding during percutaneous nephrolithotomy necessitate keeping the nephrostomy tube? A randomized controlled clinical trial. Urol J. 2011;8:21–26. [PubMed] [Google Scholar]
- 7.Hwang TK. Percutaneous nephroscopic surgery. Korean J Urol. 2010;51:298–307. doi: 10.4111/kju.2010.51.5.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skolarikos A, Papatsoris AG. Diagnosis and management of postpercutaneous nephrolithotomy residual stone fragments. J Endourol. 2009;23:1751–1755. doi: 10.1089/end.2009.1546. [DOI] [PubMed] [Google Scholar]
- 9.Segura JW, Patterson DE, LeRoy AJ, Williams HJ, Jr, Barrett DM, Benson RC, Jr, et al. Percutaneous removal of kidney stones: review of 1,000 cases. J Urol. 1985;134:1077–1081. doi: 10.1016/s0022-5347(17)47633-6. [DOI] [PubMed] [Google Scholar]
- 10.Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M, et al. Guidelines on urolithiasis. Eur Urol. 2001;40:362–371. doi: 10.1159/000049803. [DOI] [PubMed] [Google Scholar]
- 11.Koh SK, Cho JP, Yoon DK, Cha IH. Percutaneous nephrolithotripsy. Korean J Urol. 1984;25:739–745. [Google Scholar]
- 12.Hwang TK, Hong YK. Complications of percutaneous endoscopic surgery and the effect of surgical techique on complications. Korean J Urol. 1996;37:903–909. [Google Scholar]
- 13.Kwon T, Bang JK, Kim SC, Shim M, Ha SH, Hong B, et al. Percutaneous nephrolithotomy: A single center experience of 610 cases. Korean J Urol. 2009;50:669–674. [Google Scholar]
- 14.Constantinides CA, Tyritzis SI, Skolarikos A, Liatsikos E, Zervas A, Deliveliotis C. Short- and long-term complications of open radical prostatectomy according to the Clavien classification system. BJU Int. 2009;103:336–340. doi: 10.1111/j.1464-410X.2008.08080.x. [DOI] [PubMed] [Google Scholar]
- 15.Stolzenburg JU, Rabenalt R, Do M, Kallidonis P, Liatsikos EN. Endoscopic extraperitoneal radical prostatectomy: the University of Leipzig experience of 2000 cases. J Endourol. 2008;22:2319–2325. doi: 10.1089/end.2008.9714. [DOI] [PubMed] [Google Scholar]
- 16.Murphy DG, Kerger M, Crowe H, Peters JS, Costello AJ. Operative details and oncological and functional outcome of robotic-assisted laparoscopic radical prostatectomy: 400 cases with a minimum of 12 months. Eur Urol. 2009;55:1358–1366. doi: 10.1016/j.eururo.2008.12.035. [DOI] [PubMed] [Google Scholar]
- 17.Donat SM, Shabsigh A, Savage C, Cronin AM, Bochner BH, Dalbagni G, et al. Potential impact of postoperative early complications on the timing of adjuvant chemotherapy in patients undergoing radical cystectomy: a high-volume tertiary cancer center experience. Eur Urol. 2009;55:177–185. doi: 10.1016/j.eururo.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 18.Tefekli A, Ali Karadag M, Tepeler K, Sari E, Berberoglu Y, Barkal M, et al. Classification of percutaneous nephrolithotomy complications using the modified Clavien grading system: looking for a standard. Eur Urol. 2008;53:184–190. doi: 10.1016/j.eururo.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 19.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, et al. The clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–17. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 20.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 21.Wolf JS, Jr, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ. Urologic Surgery Antimicrobial Prophylaxis Best Practice Policy Panel. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379–1390. doi: 10.1016/j.juro.2008.01.068. [DOI] [PubMed] [Google Scholar]
- 22.Grabe M, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Naber KG, et al. Guidelines on Urological Infections (update 2009) European Guidelines Office (publ) Available at: http://www.uroweb.org/fileadmin/tx_eauguidelines/2009/Pocket/Urological_Infections.pdf.
- 23.Stoller ML, Wolf JS, Jr, St Lezin MA. Estimated blood loss and transfusion rates associated with percutaneous nephrolithotomy. J Urol. 1994;152:1977–1981. doi: 10.1016/s0022-5347(17)32283-8. [DOI] [PubMed] [Google Scholar]
- 24.Lee KL, Stoller ML. Minimizing and managing bleeding after percutaneous nephrolithotomy. Curr Opin Urol. 2007;17:120–124. doi: 10.1097/MOU.0b013e328010ca76. [DOI] [PubMed] [Google Scholar]
- 25.Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J Endourol. 2004;18:715–722. doi: 10.1089/end.2004.18.715. [DOI] [PubMed] [Google Scholar]
- 26.El-Nahas AR, Shokeir AA, El-Assmy AM, Mohsen T, Shoma AM, Eraky I, et al. Post-percutaneous nephrolithotomy extensive hemorrhage: a study of risk factors. J Urol. 2007;177:576–579. doi: 10.1016/j.juro.2006.09.048. [DOI] [PubMed] [Google Scholar]
- 27.Srivastava A, Singh KJ, Suri A, Dubey D, Kumar A, Kapoor R, et al. Vascular complications after percutaneous nephrolithotomy: are there any predictive factors? Urology. 2005;66:38–40. doi: 10.1016/j.urology.2005.02.010. [DOI] [PubMed] [Google Scholar]