Abstract
Purpose
The aim of this study was to categorize concealed penis and buried penis by preoperative physical examination including the manual prepubic compression test and to describe a simple surgical technique to correct buried penis that was based on surgical experience and comprehension of the anatomical components.
Materials and Methods
From March 2007 to November 2010, 17 patients were diagnosed with buried penis after differentiation of this condition from concealed penis. The described surgical technique consisted of a minimal incision and simple fixation of the penile shaft skin and superficial fascia to the prepubic deep fascia, without degloving the penile skin.
Results
The mean age of the patients was 10.2 years, ranging from 8 years to 15 years. The median follow-up was 19 months (range, 5 to 49 months). The mean penile lengths were 1.8 cm (range, 1.1 to 2.5 cm) preoperatively and 4.5 cm (range, 3.3 to 5.8 cm) postoperatively. The median difference between preoperative and postoperative penile lengths was 2.7 cm (range, 2.1 to 3.9 cm). There were no serious intra- or postoperative complications.
Conclusions
With the simple anchoring of the penopubic skin to the prepubic deep fascia, we obtained successful subjective and objective outcomes without complications. We suggest that this is a promising surgical method for selected patients with buried penis.
Keywords: Abnormality, Penis, Surgery
INTRODUCTION
The inconspicuous penis has a diverse etiology and clinical presentations [1]. The classification of the inconspicuous penis includes micropenis, webbed penis, trapped penis, concealed penis, and buried penis. Among them, micropenis, webbed penis, and trapped penis have a general consensus about terminology and etiology [2]. For concealed penis and buried penis, however, some confusion exists with the terminology and diverse etiology, including sinking of the penis under excessive suprapubic fat, tethering and shortening of the penis by abnormal fibrous bands of dartos fascia, poor penile skin fixation at the penile base, and deficient outer penile skin. Therefore, the operative techniques to correct concealed or buried penis vary according to its diverse etiology [3-6].
On the basis of our surgical experiences and comprehension of the anatomical components, we simply categorized concealed penis and buried penis by use of a preoperative physical examination including the manual prepubic compression test and applied our surgical method to patients diagnosed with buried penis. We describe our surgical method to correct buried penis, which includes a minimal incision and simple anchoring of the penopubic skin to the prepubic deep fascia without degloving the whole penile skin.
MATERIALS AND METHODS
From March 2007 to November 2010, we applied our new method to 17 patients diagnosed with buried penis after differentiation from concealed penis (Figs. 1, 2). None of the patients had undergone circumcision or other penile surgery. Concomitant genital anomalies, including hypospadias, chordee, and penoscrotal web, were excluded by careful examination.
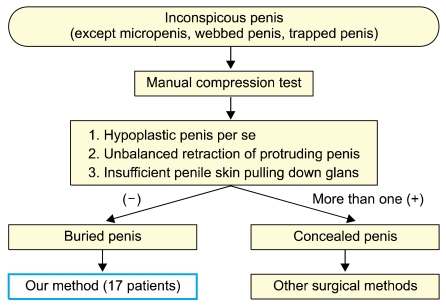
FIG. 1.
Categorization of concealed penis and buried penis by preoperative physical examination including the manual prepubic compression test.
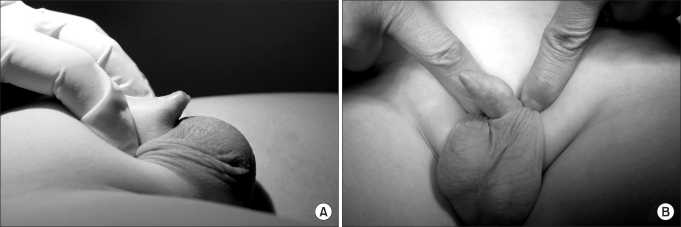
FIG. 2.
Comparison between concealed penis (A) and buried penis (B) by use of the manual prepubic compression test.
The primary objective outcome of our procedure was the improvement of penile length. A flaccid unstretched penile length was measured from the penopubic junction to the tip of the penis with the patient in the standing position. We assessed the penile length preoperatively and between 1 and 3 months postoperatively. The Wilcoxon signed-rank test was used to determine the difference in the preoperative and postoperative penile lengths.
For a retrospective review, a telephone follow-up was done for all patients. The subjective outcome was determined from a telephone questionnaire answered by the boy's parents. They were questioned about the level of satisfaction ("What do you think of the results after surgery?" with responses of unsatisfactory, good, or excellent) and the intention of recommendation ("Would you recommend the procedure to someone who suffered the same problem?" with the responses of yes or no).
For the surgical technique, the patient was placed in the supine position and local anesthesia was applied to the deep subcutaneous tissue from 9 to 3 o'clock at the penopubic junction. Because phimosis was usually present, a dorsal slit incision was made in the midline of the prepuce just long enough to expose the whole glans. An approximately 1 cm transverse incision was made near the penile base at 12 o'clock at the penopubic junction. Through the incision, blunt dissection was performed to identify the prepubic deep fascia and hardness of the pubic bone. About 1 or 2 mm stab incisions at just skin depth were made in the 9 and 3 o'clock positions lateral to the penile shaft. An additional large half-circled needle was tied up to the end of 4-0 nylon and passed through the deep fascia from the 3 o'clock tiny stab incision to the 12 o'clock skin incision. To avoid the penile deep fascia and tunica albuginea being involved in the stitch, the needle was passed under the index finger at 12 o'clock. The other end with the 4-0 nylon needle passed through the subcutaneous tissue from the 3 o'clock tiny stab incision to the 12 o'clock skin incision.
From the 9 o'clock tiny stab incision to the 12 o'clock incision, another anchoring was done in the same manner. After confirming that the penopubic junction was secured to the prepubic deep fascia in the stretched state, each side of the stitch was tied up under the 12 o'clock incision. The penopubic junction skin incision was closed with 1 or 2 stitches and the bilateral tiny stab wounds remained unsutured. Foreskin plasty was performed like circumcision. After resecting the redundant preputial skin, circumferential suturing was done. There were no cases of complex flaps due to insufficient foreskin tissue (Fig. 3).
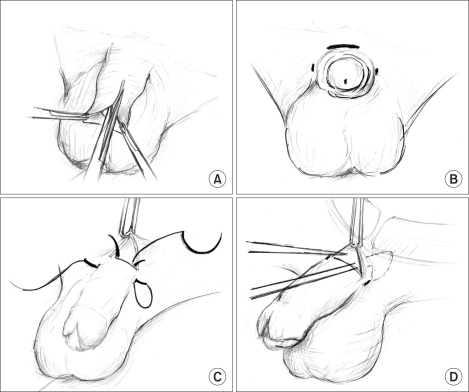
FIG. 3.
(A) A dorsal slit incision was made in the midline of the prepuce to expose the whole glans. (B) An approximately 1 cm transverse incision was made near the penile base at 12 o'clock at the penopubic junction. 1 or 2 mm stab incisions at just skin depth were made at the 9 and 3 o'clock positions lateral to the penile shaft. (C) An additional large half-circled needle was tied up to the end of 4-0 nylon and passed through the deep fascia from the 3 o'clock tiny stab incision to the 12 o'clock skin incision. The other end with a 4-0 nylon needle was passed through the subcutaneous tissue from the 3 o'clock tiny stab incision to the 12 o'clock skin incision. (D) After confirming that the penopubic junction was secured to the prepubic deep fascia in the stretched state, each side of the stitch was tied up under the 12 o'clock incision.
RESULTS
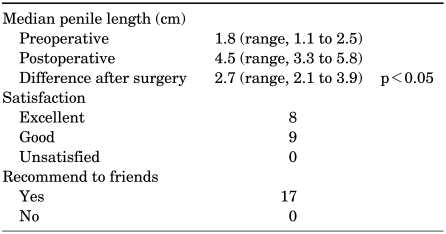
The mean age of the patients was 10.2 years, ranging from 8 years to 15 years. The median follow-up was 19 months (range, 5 to 49 months). There were no serious intraoperative or postoperative complications. Remarkable postoperative problems were distal penile skin edema and a skin dimple at the penopubic junction. The distal penile skin edema subsided without an additional procedure after several days and the skin dimples were noted in 6 patients, but no one complained about it. The mean penile lengths were 1.8 cm (range, 1.1 to 2.5 cm) preoperatively and 4.5 cm (range, 3.3 to 5.8 cm) postoperatively (Fig. 4). The median difference between preoperative and postoperative penile lengths was 2.7 cm (range, 2.1 to 3.9 cm). There was a statistically significant difference between the penile lengths before and after surgery (p<0.05) (Table 1).
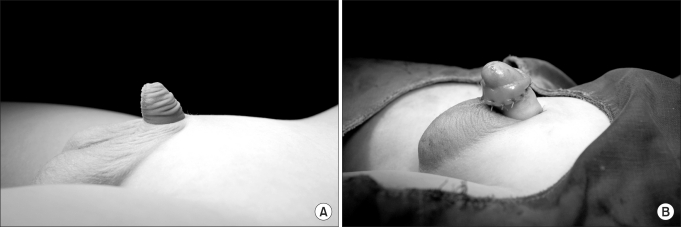
FIG. 4.
(A) Preoperative appearance of the buried penis. (B) Immediate postoperative appearance of the buried penis.
TABLE 1.
Objective and subjective surgical outcomes
The level of satisfaction was excellent in 8 patients, good in 9 patients, and unsatisfactory in none. All the boys' parents answered yes to the question about the intention of recommendation (Table 1).
DISCUSSION
Since the first description of concealed penis as the apparent absence of the penis by Keyes in 1919 [7], there has been some confusion with terminology: what should this anomaly be called, concealed penis or buried penis or something else? Maizels et al classified concealed penis into buried, webbed, and trapped penis and micropenis [2]. They further subdivided buried penis into conditions due to poor skin suspension in children and localized adiposity in adolescents. Elder classified inconspicuous penis into webbed penis, concealed penis (synonymous with buried penis), and trapped penis and micropenis as a different entity [8]. He described that concealed penis (synonymous with buried penis) was caused by inelasticity of the dartos fascia in infants and young children and abundant fat on the abdominal wall in older children and obese adolescents.
In a recent study, Oh et al classified inconspicuous penis as concealed, buried, webbed, and entrapped penis. They suggested that a concealed penis is due to deficient outer penile skin or inelasticity of the dartos fascia and a buried penis is due to poor penile skin fixation at the penile base or excessive suprapubic fat. A webbed penis is characterized by a ventral fold of skin that joins the distal shaft and scrotum, obscuring the penoscrotal angle. An entrapped penis is covered by scar tissue that occurred secondarily after circumcision. Those authors expected that this classification would be helpful in deciding on a treatment strategy [9].
We also think that this classification is helpful in further understanding the anatomical etiology of concealed penis and buried penis. Accordingly, in our study, we tried to differentiate between buried penis due to poor penile skin fixation at the penile base or excessive suprapubic fat and concealed penis due to deficient outer penile skin or inelasticity of the dartos fascia by use of the manual compression test. Shaeer and Shaeer selected patients on the basis of improvement of the flaccid unstretched length by manually pushing the mons pubis backwards [10], and Wood and Woodhouse suggested that gentle pressure around the penis will often push back the suprapubic tissues and reveal an underlying normal penis [11]. In our opinion, through the manual compression test, confirming a normally grown penis, that is, an effectually protruding penile shaft without unbalanced retraction and sufficient penile skin, is an essential step in diagnosing buried penis.
Various surgical techniques have been described for correction of the concealed penis and buried penis. These techniques include removal of excessive suprapubic fat, release of the dartos tethering bands by degloving the penile skin, anchoring the suprapubic skin to define the penopubic angle, and shaft skin reconstruction with various skin-covering methods to correct for the sparse shaft skin [12-14]. However, we have had some questions: Is degloving the whole penile skin needed in all patients? Where should the penopubic skin be anchored to the prepubic deep fascia or penile shaft?
In their 31 cases of buried penis, Redman reported no observation of any tethering bands or any abnormality of the tunica dartos [5]. Yu et al reported that 26 of 62 patients acquired an improved appearance of the penis by application of pressure at the base of the penile shaft [4]. It seemed that not the abnormal fibrous bands but the insufficient exposure of the penile shaft and poor fixation of the penile skin resulted in the abnormal appearance of the penis in those patients.
In our experience, buried penis seems to be the result of not abnormal tethering bands but inadequate attachment of the skin and superficial fascia to the deep fascia or excessive suprapubic fat pushing up the skin of the penopubic junction. These anatomical etiologic factors might cause the distorted penopubic angle that is located more distally at the level of the penile tip.
To correct this anatomical defect, we simply anchored the elevated penopubic angle to the prepubic deep fascia and defined the new penopubic angle more downward to the pubic bone. Concerning where to anchor the skin, anchoring the prepubic skin to the penile shaft should disrupt the normal gliding movement of the penile shaft in its covering skin structure. That is why we anchored the prepubic skin to the prepubic deep fascia.
Even though obesity is mentioned as a major contributor, no definitions of body mass index (BMI) cutoffs were found in a search of Medline. According to Mattson et al's experience with obese patients, grade I and II obesity (defined by the World Health Organization [WHO] as a BMI >30-35 and a BMI >35-40, respectively) were not associated with severity or incidence of the buried penis, but in cases of extreme or morbid obesity (WHO grade III, BMI >40), it becomes common and the incidence increases [15]. In our series, there were no extremely or morbidly obesity patients who required simultaneous removal of excess suprapubic fat such as lipectomy or liposuction. Some authors reported that they could get satisfactory results in obese patients without lipectomy or liposuction [1,16]. Moreover, Borsellino et al stated that excision of the prepubic fat pad in severely obese boys can create an ugly appearance with an unnatural suprapubic ledge [17]. We also think that performing additional surgical procedures to remove the suprapubic fat pad is not essential in most cases.
Our procedure is much simpler than other previously described procedures and does not require a drain, compression dressing, or catheter placement, which is a notable difference compared with other procedures in which degloving the penile skin is done for the whole penis, thus interrupting the lymphatic drainage and causing significant edema or disastrous skin necrosis postoperatively. We performed this procedure as an outpatient procedure under local anesthesia.
There has been some argument over the timing and indication of surgery in cases of buried penis. Wood et al described that buried penis patients should definitely not have surgery until they have completed puberty, because with growth and development, the suprapubic fat pad may decrease considerably and these steps are important to avoid operating on patients either prematurely or unnecessarily [11]. Moon et al suggested that the timing of surgery should be determined by the severity of buried penis, the feelings of the patient, and the opinions of the parents [13]. Oh et al also suggested that surgery or additional treatment to correct buried penis should be performed between childhood and puberty after comprehensive consideration of factors such as the etiology, presence of psychological stress, and the degree of accompanying suprapubic fat pad [9].
We also think that important factors that affect the performance of surgery are the embarrassment of the patient, pessimistic thoughts about their penis, and anxiety of the parents in addition to voiding problems, urinary tract infection, and poor hygiene. Furthermore, it should not be overlooked that the incidence of buried penis in childhood and adolescence is increasing as a result of the increase in obesity in children. In this regard, if we could get competent results without complications by use of a minimally invasive surgical method, we think it would be worthwhile to apply the surgical treatment.
Our method was primarily aimed at improving penile length with minimal invasiveness and minimal complications in selected patients with buried penis. We achieved successful surgical outcomes through this simple procedure.
CONCLUSIONS
With the simple anchoring of the penopubic skin to the prepubic deep fascia, we obtained successful subjective and objective outcomes without complications. We think that this is a promising surgical method for selected patients with buried penis.
Footnotes
The authors have nothing to disclose.
References
- 1.Lee T, Suh HJ, Han JU. Correcting congenital concealed penis: new pediatric surgical technique. Urology. 2005;65:789–792. doi: 10.1016/j.urology.2004.10.075. [DOI] [PubMed] [Google Scholar]
- 2.Maizels M, Zaontz M, Donovan J, Bushnick PN, Firlit CF. Surgical correction of the buried penis: description of a classification system and a technique to correct the disorder. J Urol. 1986;136:268–271. doi: 10.1016/s0022-5347(17)44837-3. [DOI] [PubMed] [Google Scholar]
- 3.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161:455–459. [PubMed] [Google Scholar]
- 4.Yu W, Cheng F, Zhang X, Ruan Y, Yang S, Xia Y. Minimally invasive technique for the concealed penis lead to longer penile length. Pediatr Surg Int. 2010;26:433–437. doi: 10.1007/s00383-010-2576-7. [DOI] [PubMed] [Google Scholar]
- 5.Redman JF. Buried penis: congenital syndrome of a short penile shaft and a paucity of penile shaft skin. J Urol. 2005;173:1714–1717. doi: 10.1097/01.ju.0000154781.98966.33. [DOI] [PubMed] [Google Scholar]
- 6.Wollin M, Duffy PG, Malone PS, Ransley PG. Buried penis. A novel approach. Br J Urol. 1990;65:97–100. doi: 10.1111/j.1464-410x.1990.tb14667.x. [DOI] [PubMed] [Google Scholar]
- 7.Frenkl TL, Agarwal S, Caldamone AA. Results of a simplified technique for buried penis repair. J Urol. 2004;171:826–828. doi: 10.1097/01.ju.0000107824.72182.95. [DOI] [PubMed] [Google Scholar]
- 8.Elder JS. Abnormalities of the genitalia in boys and their surgical management. In: Wein AJ, Kavoussi LR, Novik AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. pp. 3745–3760. [Google Scholar]
- 9.Oh CY, Lee Hy, Hong CH, Han Sw. Long-term outcome and parents satisfaction after the correction of concealed penis. Korean J Pediatric Urol. 2009;1:58–63. [Google Scholar]
- 10.Shaeer O, Shaeer K. Revealing the buried penis in adults. J Sex Med. 2009;6:876–885. doi: 10.1111/j.1743-6109.2008.01162.x. [DOI] [PubMed] [Google Scholar]
- 11.Wood D, Woodhouse C. Penile anomalies in adolescence. ScientificWorldJournal. 2011;11:614–623. doi: 10.1100/tsw.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim JS, Seo IY. Surgical correction of concealed penis by suprapubic lipectomy and a modification of johnston's principle under local anesthesia. Korean J Urol. 2000;41:1023–1032. [Google Scholar]
- 13.Moon SY, Jung GW, Yoon JH. New method of correction for severe or recurrent concealed penis after operation by conventional method. Korean J Urol. 1998;39:1047–1050. [Google Scholar]
- 14.Park SW, Lee SD. Long-term parental satisfaction after surgical treatment of concealed penis. Korean J Urol. 2008;49:627–632. [Google Scholar]
- 15.Mattsson B, Vollmer C, Schwab C, Padevit C, Horton K, John H, et al. Complications of a buried penis in an extremely obese patient. Andrologia. 2011 doi: 10.1111/j.1439-0272.2011.01194.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Brisson P, Patel H, Chan M, Feins N. Penoplasty for buried penis in children: report of 50 cases. J Pediatr Surg. 2001;36:421–425. doi: 10.1053/jpsu.2001.21605. [DOI] [PubMed] [Google Scholar]
- 17.Borsellino A, Spagnoli A, Vallasciani S, Martini L, Ferro F. Surgical approach to concealed penis: technical refinements and outcome. Urology. 2007;69:1195–1198. doi: 10.1016/j.urology.2007.01.065. [DOI] [PubMed] [Google Scholar]