Galvao et al.1 compare the effects of two high-fat diets, both 45% kcal but sourced from either polyunsaturated fatty acids (PUFA; linoleic and α-linolenic acids) or saturated fat (palmitate and stearate) in a male δ-sarcoglycan null Bio TO2 hamster model of heart failure. Surprisingly, the heart failure hamsters fed the diet high in saturated fat showed increased survival compared with hamsters fed a diet high in PUFA or the control standard diet (12% kcal from fat). Importantly, in all three diet groups, the hamsters developed dysfunction at both the left ventricle and cardiac mitochondria levels. Despite the lack of a cardiac function phenotype, the PUFA-fed hamsters showed elevated Ca2+-induced mitochondrial permeability transition pore opening rates compared with both the saturated fat and standard fed hamsters. The clear distinction in obesity effects differentially driven by high-fat diets from different lipid sources, in the context of heart failure, has not been previously studied. The present study is important because it reveals the strong impact of fat source on cardiovascular events and survival rates in the setting of existing heart failure.
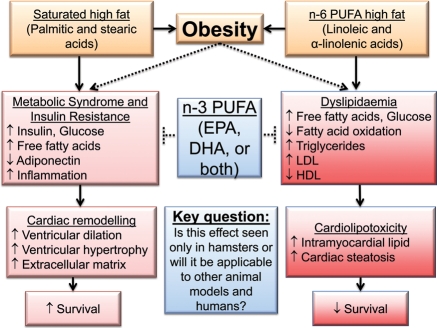
A diet high in saturated fat promotes obesity by stimulating an inflammatory response that can induce cardiac concentric hypertrophy and alter the stress response.2 Obesity resulting either from saturated or PUFA fat diets also initiates hyperlipidaemia, hypertension, and diabetes, which promote atherosclerosis, ischaemic heart disease, and eventually heart failure.3 In the context of the clinically established obesity paradox, where obese patients diagnosed with heart failure have significantly better survival than normal-weight heart failure patients,4 the study by Galvao et al. extends our current knowledge base. This paper focuses on the development of n-6-enriched PUFA-induced cardiac lipotoxicity (Figure 1), which may dominate over glucolipotoxicity in the setting of heart failure.5 While both n-3 and n-6 PUFA are considered lipoprotective,5 excessive n-6 PUFA intake dramatically increases serum plasma free fatty acids, which correlated with decreased survival in PUFA-fed hamsters by promoting cardiac lipotoxicity.
Figure 1.
The findings of Galvao et al. illustrate that effects of a high-fat diet on cardiac phenotype depend on the type, rather than the amount, of fat consumed. Their results illustrate that we need additional studies to compare n-6 PUFA with n-3 and n-6 PUFA diets and to a saturated fat diet to more completely understand the divergent roles of different fat types in regulating cardiac function, both in physiological and pathophysiological settings. The solid lines indicate known pathways while the dashed lines indicate relationships that remain to be fully elucidated. DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol; PUFA, polyunsaturated fatty acids.
Obesity is the result of an energy imbalance caused by the consumption of a high-calorie and high-fat diet combined with a sedentary lifestyle, and the incidence of obesity has reached epidemic numbers. The δ-sarcoglycan-deficient hamster, a genetic model of heart failure, offers an opportunity to study obesity in the setting of cardiac failure. Of note, glucose and free fatty acids were measured in non-fasting hamsters, which prevent our ability to know whether the animals were insulin-resistant. Right ventricle fatty acid analysis showed signs of lipotoxicity (increased linoleic acid, reduced oleic acid, and reduced total monounsaturated fatty acids) that may explain the reduced survival seen in the high PUFA-fed hamsters.
Unger and colleagues6 delineated the role of fatty acid accumulation in non-adipose tissues, including the myocardium, but clinical markers for lipotoxic cardiomyopathy remain to be fully developed. Interestingly, cardiac steatosis is associated with left ventricle hypertrophy and dysfunction, and cardiolipotoxicity precedes the impaired glucose tolerance and onset of type 2 diabetes, indicating that a PUFA-enriched fat has a more immediate effect on cardiac function.6 Excessive lipid deposition in non-adipose organs is a major contributor in both obesity and type 2 diabetes.7
During the twentieth century, essential linoleic acid (n-6 PUFA) consumption increased 1000-fold in Western diets.8 An increased n-6 PUFA (linoleic acid) intake elevates oxidized LDL levels to stimulate atherosclerotic plaque growth.9 Arachidonic acid is produced by the metabolism of linoleic acid, and arachidonic acid-derived eicosanoids are involved in many physiological and pathophysiological responses, including inflammation and thrombosis. The combination of n-3 and n-6 PUFA, compared with n-6 PUFA alone, has different cardiac effects.10 Replacement of a saturated fat with a diet of mixed n-3 and n-6 PUFAs reduces coronary heart disease (CHD) risk, whereas a diet of only n-6 PUFA increases CHD risk.10 Chronic linoleic acid consumption cumulatively affects CHD mortality risk by stimulating inflammation, thrombosis, and LDL oxidation. As the American Heart Association (AHA) has recommended a diet rich in PUFA, this study and future studies examining the effects of n-6 vs. n-3 and n-6 PUFA diets may help the AHA to refine their statement.10 While n-6 PUFA has been recommended for the prevention of CHD, based on pre-clinical and clinical studies, most studies measure only total PUFA consumption and do not distinguish between n-3 and n-6 PUFA sources.11 In addition, the effects of different types of n-3 PUFA sources on cardiac function have not been investigated. For example, the dietary supplement fish oil is widely used as a source of n-3 PUFA, and fish oil contains eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) as two distinct n-3 fatty acids. Whether both components will reduce risk in high-risk patients has not been explored.12 Previous reports from the Stanley laboratory indicate that the primary cardioprotective effect is attributed to DHA rather than EPA,13 and this provides a strong rationale for further examining the effects of consumption of different n-3 and n-6 PUFA types on CHD.
Where do we need to go from here? Experiments that are still needed include studies that (i) assess how n-3 and n-6 PUFA vs. n-6 PUFA alone induce different or similar obesity effects on cardiac function,14 (ii) determine how gender and ageing may alter the response to high-fat diets from different sources, and (iii) evaluate how n-3 and n-6 vs. n-6 PUFA-induced obesity alters cardiac function when superimposed on inflammatory conditions such as arthritis or lupus and in response to cardiac pathology including myocardial infarction.15 The future integration of lipidomic, metabolomic, proteomic, and genomic data in these studies will also contribute towards a better understanding of how lipids from different sources modulate cardiovascular disease.
In summary, Galvao et al. demonstrate that a high intake of saturated fat improves survival in a hamster heart failure model without altering cardiac function. This study reveals the need to further explore how saturated fat vs. PUFA-enriched diets contribute to obesity and what their impact is on cardiac remodelling in heart failure.
Conflict of interest: none declared.
Funding
We acknowledge support from NIH NCCAM K99 AT006704 to G.V.H.; from NSF 0649172, NIH EB009496, and NIH 1SC2 HL101430 to Y.-F.J.; and from NHLBI HHSN 268201000036C (N01-HV-00244) for the UTHSCSA Cardiovascular Proteomics Center and R01 HL075360, the Max and Minnie Tomerlin Voelcker Fund, and the Veteran's Administration (Merit) to M.L.L.
References
- 1.Galvao TF, Brown BH, Hecker PA, O'Connell KA, O'Shea KM, Sabbah HN, et al. High intake of saturated fat, but not polyunsaturated fat, improves survival in heart failure despite persistent mitochondrial defects. Cardiovasc Res. 2012;93:24–32. doi: 10.1093/cvr/cvr258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thakker GD, Frangogiannis NG, Bujak M, Zymek P, Gaubatz JW, Reddy AK, et al. Effects of diet-induced obesity on inflammation and remodeling after myocardial infarction. Am J Physiol Heart Circ Physiol. 2006;291:H2504–H2514. doi: 10.1152/ajpheart.00322.2006. [DOI] [PubMed] [Google Scholar]
- 3.Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–313. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 4.Lavie CJ, Milani RV, Artham SM, Patel DA, Ventura HO. The obesity paradox, weight loss, and coronary disease. Am J Med. 2009;122:1106–1114. doi: 10.1016/j.amjmed.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Taegtmeyer H, Stanley WC. Too much or not enough of a good thing? Cardiac glucolipotoxicity versus lipoprotection. J Mol Cell Cardiol. 2011;50:2–5. doi: 10.1016/j.yjmcc.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Szczepaniak LS, Victor RG, Orci L, Unger RH. Forgotten but not gone: the rediscovery of fatty heart, the most common unrecognized disease in America. Circ Res. 2007;101:759–767. doi: 10.1161/CIRCRESAHA.107.160457. [DOI] [PubMed] [Google Scholar]
- 7.Unger RH. Lipotoxic diseases. Annu Rev Med. 2002;53:319–336. doi: 10.1146/annurev.med.53.082901.104057. [DOI] [PubMed] [Google Scholar]
- 8.Blasbalg TL, Hibbeln JR, Ramsden CE, Majchrzak SF, Rawlings RR. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am J Clin Nutr. 2011;93:950–962. doi: 10.3945/ajcn.110.006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsimikas S, Philis-Tsimikas A, Alexopoulos S, Sigari F, Lee C, Reaven PD. LDL isolated from Greek subjects on a typical diet or from American subjects on an oleate-supplemented diet induces less monocyte chemotaxis and adhesion when exposed to oxidative stress. Arterioscler Thromb Vasc Biol. 1999;19:122–130. doi: 10.1161/01.atv.19.1.122. [DOI] [PubMed] [Google Scholar]
- 10.Ramsden CE, Hibbeln JR, Majchrzak SF, Davis JM. N-6 fatty acid-specific and mixed polyunsaturate dietary interventions have different effects on CHD risk: a meta-analysis of randomised controlled trials. Br J Nutr. 2010;104:1586–1600. doi: 10.1017/S0007114510004010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ, et al. Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the American Heart Association nutrition subcommittee of the council on nutrition, physical activity, and metabolism; council on cardiovascular nursing; and council on epidemiology and prevention. Circulation. 2009;119:902–907. doi: 10.1161/CIRCULATIONAHA.108.191627. [DOI] [PubMed] [Google Scholar]
- 12.Saravanan P, Davidson NC, Schmidt EB, Calder PC. Cardiovascular effects of marine omega-3 fatty acids. Lancet. 2010;376:540–550. doi: 10.1016/S0140-6736(10)60445-X. [DOI] [PubMed] [Google Scholar]
- 13.Khairallah RJ, O'Shea KM, Brown BH, Khanna N, Des Rosiers C, Stanley WC. Treatment with docosahexaenoic acid, but not eicosapentaenoic acid, delays Ca2+-induced mitochondria permeability transition in normal and hypertrophied myocardium. J Pharmacol Exp Ther. 2010;335:155–162. doi: 10.1124/jpet.110.170605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halade GV, Rahman MM, Williams PJ, Fernandes G. High fat diet-induced animal model of age-associated obesity and osteoporosis. J Nutr Biochem. 2010;21:1162–1169. doi: 10.1016/j.jnutbio.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halade GV, Rahman MM, Bhattacharya A, Barnes JL, Chandrasekar B, Fernandes G. Docosahexaenoic acid-enriched fish oil attenuates kidney disease and prolongs median and maximal life span of autoimmune lupus-prone mice. J Immunol. 2010;184:5280–5286. doi: 10.4049/jimmunol.0903282. [DOI] [PMC free article] [PubMed] [Google Scholar]