Abstract
Background:
Traumatic Brain Injury (TBI) is a “signature” injury of the current wars in Iraq and Afghanistan. Structured electronic data regarding TBI findings is important for research, population health and other secondary uses but requires appropriate underlying standard terminologies to ensure interoperability and reuse. Currently the U.S. Department of Veterans Affairs (VA) uses the terminology SNOMED CT and the Department of Defense (DOD) uses Medcin.
Methods:
We developed a comprehensive case definition of mild TBI composed of 68 clinical terms. Using automated and manual techniques, we evaluated how well the mild TBI case definition terms could be represented by SNOMED CT and Medcin, and compared the results. We performed additional analysis stratified by whether the concepts were rated by a TBI expert panel as having High, Medium, or Low importance to the definition of mild TBI.
Results:
SNOMED CT sensitivity (recall) was 90% overall for coverage of mild TBI concepts, and Medcin sensitivity was 49%, p < 0.001 (using McNemar’s chi square). Positive predictive value (precision) for each was 100%. SNOMED CT outperformed Medcin for concept coverage independent of import rating by our TBI experts.
Discussion:
SNOMED CT was significantly better able to represent mild TBI concepts than Medcin. This finding may inform data gathering, management and sharing, and data exchange strategies between the VA and DOD for active duty soldiers and veterans with mild TBI. Since mild TBI is an important condition in the civilian population as well, the current study results may be useful also for the general medical setting.
Background
The current study examines the adequacy of concept coverage for a case definition of mild traumatic brain injury (TBI) among two leading health care terminologies, SNOMED CT® used by the Department of Veterans Affairs (VA) and Medcin® used by the Department of Defense (DOD).
TBI has been labeled a “signature” injury of the Operation Enduring Freedom-Afghanistan (OEF) and Operation Iraqi Freedom (OIF) campaigns in which the United States (U.S.) military participate.[1–3] Since 2001, more than 1.7 million U.S. troops have been deployed under OEF /OIF.[4] During the nearly ten year history of the wars in Iraq and Afghanistan, an estimated 20% or more of U.S. service members have sustained TBI, making it one of the most common injuries among our military personnel.[4–7] In the current military campaigns, the frequent use of improvised explosive devices (IEDs) and other events leading to explosion-related injuries contribute to the relatively high incidence of TBI in deployed personnel.[6,8]
TBI severity is defined by symptoms at the time of injury.[9] Mild TBI, commonly referred to as “concussion”, is by far the most frequent type of TBI sustained during deployment to OEF/OIF, and by civilians.[6,9] Initial symptoms of the injury may be brief alteration of consciousness or loss of consciousness lasting only seconds to minutes. In most cases, the sequelae of mild TBI resolve in days to a few months. However, in some patients, post-concussive symptoms persist and may lead to long-term functional limitations.[4,6] Symptoms are more likely to be persistent among those people who experience multiple TBIs.[6]
Despite understanding that mild TBI is the most commonly sustained form of TBI, reports estimating prevalence of mild TBI, or prevalence of mild TBI as a subset of all TBI, vary in the literature. Reporting discrepancies are in part due to variation in the definitions used for mild TBI versus moderate and severe TBI, and in part due to variations in clinical terminology used to describe mild TBI.[10] Hoge et al [1] reported an overall incidence of mild TBI of nearly 15% in a study of 2,525 soldiers returning from Iraq. Jackson et al [7] reported estimates that almost 50% of soldiers injured in combat return with some form of TBI, and further noted that in the general population an estimated 80% of individuals who sustain TBI are classified as mild. In a 2003 report to Congress, the CDC Mild Traumatic Brain Injury Work Group noted that mild TBI as accounting for at least 75 percent of all traumatic brain injuries in the U.S.[11]
While our study intended to develop and assess terminology concept coverage for a diagnosis of mild TBI in OEF/OIF soldiers and veterans, most signs and symptoms of mild TBI are the same as those manifested by civilians who sustain mild TBI. The experience of the general medical community in diagnosing, managing, and reporting mild TBI has informed the current management of mild TBI in soldiers and veterans.[12] In turn, military and media attention on mild TBI as a prevalent injury among our OEF/OIF soldiers has caused renewed attention to the importance of the disorder in the U.S. general population, a concern well known to our nation’s emergency room personnel. 1.7 million traumatic brain injuries occur annually in the U.S., accounting for more than 1.3 million emergency room visits, the vast majority being for mild TBIs.[13–14] Common causes of TBI in the general population include falls, motor vehicle accidents, and “struck by” injuries such as may occur in sports-related activities. Documented sports-related concussions alone account for an estimated 300,000 cases of mild TBI annually.[12] In tandem with our military population, there is heightened awareness of sequelae of mild TBI among professional, college, and high school athletes who participate in sports such as football that carry high risk of head injury.[14–18]
Evaluations such as objective evidence of brain injury on brain scan or neurological examination and objective deficits on neuropsychological testing often are diagnostic for moderate and severe TBI, but frequently are not useful in the diagnosis of mild TBI.[9] Discussions regarding mild TBI, particularly in the U.S. Veteran population, have appeared in recent medical literature with varying criteria for detection and diagnosis.[1, 19–22] The civilian and military medical communities have worked together to gain consensus on a diagnostic definition of mild TBI [6,7,12,22–28], to close “knowledge gaps” regarding TBI [27], and to understand how best to assess the true prevalence and relative importance of various symptoms that comprise the sequelae of the condition.[4,6,29–33] A clinical practice guideline for mild TBI was recently released jointly by the VA and DOD.[9]
Mild TBI has been referred to as the “silent epidemic” precisely because the consequences that arise from it often are not overtly visible [11], and because some of the symptoms (e.g., fatigue or headache) are seen commonly due to other causes in both the general and military populations. At the time of injury, the absence of external injury or immediate disabling symptoms may allow an injured soldier to continue daily duties with only brief clinical evaluation or without seeking any medical attention at all. Over time, in soldiers and veterans in particular, symptoms of mild TBI may overlap with symptoms of Post Traumatic Stress Disorder, posing a significant challenge to accurately diagnosing mild TBI.[5,26,34] The importance of screening vigorously for TBI among soldiers and veterans only recently has received priority attention.[9,7,22,35]
The DOD electronic health record (EHR) system uses Medcin, a clinical terminology designed to support medical documentation entry. Introduced in 1978, Medcin now contains 280,000 concepts.[36] Following recommendations of the Consolidated Health Informatics Council and the National Committee on Vital and Health Statistics, the VA is committed to using SNOMED CT for problem lists and other functions of its EHR. Licensed for U.S.-wide use in 2003 and evaluated in 15 Medline indexed studies in 2006, SNOMED CT is maintained and distributed by the International Health Terminology Standards Development Organisation (IHTSDO).[36 IHTSDO] SNOMED CT includes approximately 370,000 concepts with greater than 1 million synonyms.
The current study seeks to understand which of these health care terminologies provides the most appropriate concept coverage for mild TBI, a diagnosis of increasing importance among our soldiers and veterans.
Methods
To evaluate how well mild TBI case definition terms could be represented by SNOMED CT and Medcin, the current study first used consensus methods[40] to develop a clinical case definition of mild TBI, and then applied methods previously described [41–43] to measure coverage for mild TBI concepts by the two terminologies. We performed additional analysis based upon whether the concepts were rated by a TBI expert panel as having High, Medium, or Low importance to the definition of mild TBI.
For the first step in our study, we convened a workgroup of 15 clinicians, researchers, and informaticists, including 6 TBI content experts from five institutions nationally. Using published literature endorsed by the convened workgroup, we developed a working case definition of mild TBI. The case definition we developed comprehensively includes criteria from the Brief Traumatic Brain Injury Screen (BTBIS) [22,23], the Neurobehavioral Symptom Inventory [23], the ICD-10 Criteria for Postconcussional Syndrome [23, the Mayo TBI Severity Classification System [28], and the CDC (Centers for Disease Control) TBI definitions and symptoms.[38,39] Our goal in engaging an expert panel to pool content from all of the aforementioned definitions was to approach an exhaustive list of terms relevant to mild TBI, and to make sure that the list included all terms important to the presentation of mild TBI in the military and veteran populations. Jones and Hunter have provided a basic justification for the use of consensus methods in health services research, including the “expert panel” (nominal group technique).[40] Expert panels and reviewers have been used extensively to develop and validate terminological systems.[41–46]
For the second step in our study, we engaged another panel of six TBI clinical experts to review our mild TBI case definition. The specialty areas of these experts include clinical neuropsychology/cognition, brain injury/polytrauma, neurosciences/head trauma, physical medicine/war trauma, and trauma surgery. Specifically, the expert panel rated 60 clinical terms from the case definition based on how much they agreed or disagreed that the term should be included in a working case definition of mild TBI, using a 5 point Likert scale (5 = Strongly Agree, 4 = Agree, 3 = Neither Agree nor Disagree, 2 = Disagree, 1 = Strongly Disagree).
Additionally, a team of 3 clinicians (2 physicians, 1 nurse) searched for variations on mild TBI terms by performing detailed human review of 10 VA Compensation and Pension (C&P) examination records of OIF/OEF era veterans who had been evaluated for possible mild TBI. These records were content rich with mild TBI terms expressed specifically in the records of veterans and soldiers. The 3 clinical experts identified 8 commonly occurring terms that represented synonyms felt by the clinicians to be important to the definition of mild TBI in soldiers and veterans, and these terms were added to our case definition. For example, our original clinical case definition included the term “Blast Injury”. We added the term “Explosion Injury” to the final working definition to account for the likely appearance of the term in a recorded clinical evaluation of a soldier or veteran. By including symptoms and terms specific to mild TBI among veterans of OIF/OEF military “theatre”, our case definition both encompasses and extends the criteria most commonly used to diagnose mild TBI in the general population.
In all, the authors identified 68 terms that represent clinical symptoms or findings of mild TBI (Table 1). Of these 68 terms, 60 were the clinical terms from our working case definition and 8 were the terms that appeared commonly in review of actual veteran clinical records.
Table 1.
Clinical Terms for Mild TBI Case Definition
| Fragment Injury | Shrapnel Injury | Bullet Injury |
| Vehicular Injury | Airplane Injury | Helicopter Injury |
| Humvee Injury | Fall Injury | Blast Injury |
| Explosion Injury | Blast Injury due to Improvised | Blast Injury due to Rocket |
| Explosive Device | Propelled Grenade | |
| Blast Injury due to Grenade | Blast Injury due to Land Mine | Dazed |
| Confused | Seeing stars | Blacked out |
| Amnesia for event | Loss of Consciousness | Knocked out |
| Losing consciousness for less than a minute | Losing consciousness for 1 to 20 minutes | Losing consciousness for longer than 20 minutes |
| Symptoms of concussion after injury | Headache after injury | Dizziness after injury |
| Irritability after injury | Head Injury | Head Trauma |
| Skull fracture | Dizziness | Balance problems, Imbalance |
| Ringing in the ears, Tinnitus | Poor coordination | Clumsy |
| Headaches | Nausea | Vision problems, Trouble seeing |
| Blurring, Blurry Vision | Sensitivity to light | Hearing difficulty |
| Sensitivity to noise | Numbness in parts of body | Tingling in parts of body |
| Change in taste | Change in smell | Increased appetite |
| Decreased appetite | Poor concentration, Cannot pay attention, Easily distracted | Forgetfulness, Cannot remember things |
| Difficulty making decisions | Slowed thinking | Difficulty getting organized |
| Cannot finish things | Fatigue, Loss of energy, Getting tired easily | Difficulty falling asleep |
| Difficulty staying asleep | Feeling anxious | Feeling tense |
| Feeling depressed | Feeling sad | Easily annoyed, Irritability |
| Poor frustration tolerance | Feeling easily overwhelmed by things | Reduced tolerance to alcohol |
| Problems with emotional control, Emotional dyscontrol, Disinhibition | Not remembering the injury, Cannot recall injury, Amnesia for injury |
For the next step of the study, and applying a method employed and described in prior investigations [41–44], we used both manual and automated processes to map the 68 terms from our final mild TBI case definition separately to SNOMED CT and to Medcin. First, we used an automated natural language processor, the Multi-threaded Clinical Vocabulary Server (MCVS) [43], to map the 68 terms to each terminology. The MCVS is a set of tools that facilitates health vocabulary indexing, and provides automatic concept mappings from free-text phrases to clinical terminologies.[43,44] The results of the automated mappings were given to two independent physician reviewers who then used the MCVS terminology browser manually to search SNOMED CT and Medcin prior to declaring any concept a “non-match” in either terminology. A third independent physician reviewer adjudicated a final decision whenever the first two reviewers disagreed.
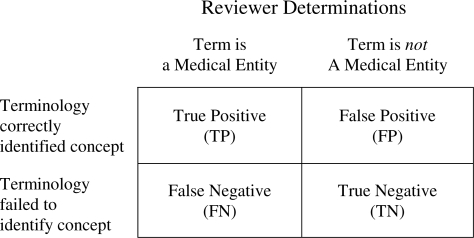
A term was considered valid for coding in a medical terminology if all reviewers agreed that it was a medically reasonable and unambiguous term. For each term being evaluated, the reviewers judged SNOMED CT or Medcin as “positive” when the terminology contained concepts represented by the study terms, and “negative” when the terminology did not contain concepts represented by the study terms. Reviewers judged each terminology’s coverage as being: “True Positive” (TP) if the term was a reasonable medical entity and the terminology contained a concept to represent the term; “False Positive” if the term was not felt to be a valid medical entity but the terminology contained a concept that matched the term; “True Negative” if the term was not a medical entity and the terminology did not map to any term; and “False Negative” when the term was a reasonable medical entity but the terminology failed to have a concept to represent the term appropriately. The schema for reviewer determinations is depicted in Figure 1.
Figure 1.
Reviewer Determinations schema
Finally, we compared concept coverage between SNOMED and Medcin. The SNOMED and Medcin classifications provided matched data. To account for matching and compare SNOMED and Medcin performance, McNemar’s chi square was used to test SNOMED with Medcin sensitivity for the overall clinical case definition of mild TBI. We performed additional analysis based upon the importance rating given by our expert panel. Since no term was rated below a weighted score of 3, we divided the range of ratings into 3 scoring classifications: Low (score <= 3.67), Medium (score > 3.67 and <= 4.33), and High (score > 4.33). Sensitivity and positive predictive value of SNOMED and Medcin were calculated for each of the 3 categories of import.
Results
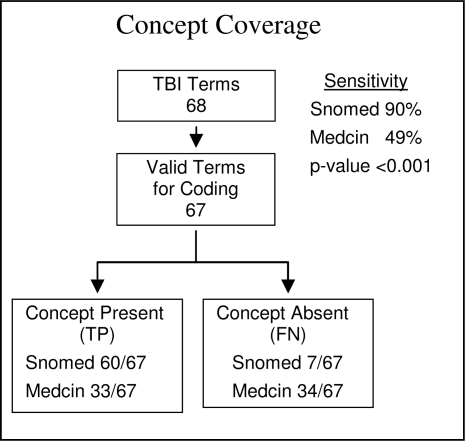
Concept coverage and classification of results are shown in Figure 1. We found 67 of the 68 terms (Table 1) in our mild TBI case definition to be valid for attempting to code in a medical terminology. The term “seeing stars” was not coded because our independent manual reviewers determined that the term was too ambiguous (e.g., seeing stars after sustaining head trauma, versus literally seeing stars upon sky gazing).
SNOMED CT’s sensitivity (recall) as a candidate terminology for our case definition of mild TBI was 90%, and positive predictive value (PPV) (precision) was 100%. By contrast, Medcin’s sensitivity was 49%, with a PPV of 100%. The superior performance of SNOMED CT over Medcin was statistically significant with a p-value of <0.001 (using McNemar’s chi square). Table 2 contains detailed results of the performance of each terminology.
Table 2.
Analysis of SNOMED CT vs Medcin Content Coverage for entire set of Mild TBI Clinical Concepts (n=67). PPV: positive predictive value. NPV: negative predictive value.
| TP | TN | FP | FN | Sensitivity (recall) | Specificity | PPV (precision) | NPV | |
|---|---|---|---|---|---|---|---|---|
| SNOMED CT | 60 | 1 | 0 | 7 | 90% | 100% | 100% | 13% |
| Medcin | 33 | 1 | 0 | 34 | 49% | 100% | 100% | 3% |
Of the 67 terms considered valid, our TBI expert panel had rated 59 terms for their relative importance to the clinical definition of mild TBI (as described in the Methods section, the final 8 terms were added to the definition following the expert panel completing its ratings). We performed sub-group analysis based on the three categories of import (Table 3). SNOMED CT outperformed Medcin in every category of import.
Table 3.
Subgroup analysis of Content Coverage based on Expert Evaluation of Clinical Import of 59 TBI Terms
| Total (n = 67) | High Import (n = 18) | Medium Import (n = 30) | Low Import (n = 11) | |||||
|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | Specificity | Sensitivity | Specificity | Sensitivity | Specificity | |
| SNOMED | 90% | 100% | 83% | 100% | 93% | na | 100% | na |
| Medcin | 49% | 100% | 35% | 100% | 57% | na | 55% | na |
Discussion
DOD and VA operate two of the nation’s largest health care systems, providing health care to service members and veterans often in a shared capacity. Currently, DOD and VA are engaged in collaborative initiatives, including development of the Virtual Lifetime Electronic Health Record (VLER), that are dependent on their ability to fully share electronic health information.[47] The VA and DOD each have well-established but quite separate patient electronic health records (EHRs). The ability to retrieve and apply structured, codified data from their EHRs can promote data sharing activities, and enhance important secondary uses such as health services research, quality improvement activities and surveillance, and population health. In very recent years, in an effort to better characterize, understand, and treat the condition, both agencies have increased specific screening for mild TBI.[5,7,9,11,23,34,48] Demonstrating how well mild TBI can be represented using current terminology systems is a first step toward ensuring that accurate data may be extracted for this purpose from the EHR both for individual clinical and population health purposes.
SNOMED CT, the terminology supporting components of the VA’s EHR system, was significantly better able to represent TBI concepts than Medcin, the terminology underpinning of AHLTA, the DOD’s EHR system. SNOMED CT outperformed Medcin in overall sensitivity for concepts in a comprehensive case definition of mild TBI (90% vs 49%, p<0.001), and in sensitivity for concept coverage independent of import rating by our TBI experts. In a prior study, SNOMED CT also outperformed Medcin as a reference terminology and as an interface terminology for representation of a VA general medical examination template.[41]
In the current study, SNOMED CT has a sensitivity or recall of 90% which is similar to the 92.3% sensitivity found by Elkin et al for clinical problems.[43] Many of the concepts necessary for TBI surveillance fall under the Disorders and Findings Hierarchy, which was the definition of clinical problems used in Elkin’s earlier study.
The difference in performance of the terminologies in this study is due, in part, to size. SNOMED CT (370,000 concepts) is a larger terminology than Medcin (280,000 concepts). Therefore the content coverage of SNOMED CT when used as a pre-coordinated terminology would exceed that of Medcin. In addition, SNOMED CT was able to match many terms with compositional expressions (22 terms), while Medcin is not compositional. We allowed Boolean combinations of Medcin concepts and using this technique we matched only 2 terms linked by Boolean operators (i.e. And, Or, Not). SNOMED contains more reusable atomic concepts than Medcin, as well as linking semantics that can be used to create post-coordinated expressions. Medcin by contrast contains many pre-coordinated terms, but lacks formal mechanisms for post-coordination. The performance difference between the two terminologies may reflect the flexibility and power of post-coordination for content representation. Medcin has been described by the company that created and maintains it as “a robust database of medical concepts with methods for presenting and documenting relevant symptoms, history, physical findings, tests, diagnoses and therapy for virtually any patient presentation.”[36] Until we performed our study, we could not know whether Medcin’s population of pre-coordinated terms would be sufficient to represent the terms important to a case definition of mild TBI.
Lastly, our reviewers noted that Medcin contained some terms that were more granular than would be required for our case definition, but Medcin more often than SNOMED CT failed to have appropriate organizing concepts to cover the term. Example clinical terms and the differences in the ability of SNOMED CT versus Medcin to cover the term are shown in Table 4.
Table 4.
Terminology Mapping Example
| Clinical Term | SNOMED CT Concept | MEDCIN Concept |
|---|---|---|
| Bullet Injury | Bullet, device (physical object) [86122002] [K] Traumatic injury (disorder) [417746004][K] |
‘Bullet’ – not matched. TRAUMA [33713][K] |
| Difficulty falling asleep | Initial insomnia (disorder) [59050008] [K] | Initial insomnia (disorder) [59050008] [K] |
| Difficulty staying asleep | Middle insomnia (disorder) [67233009] [K] | No match |
Andrews et al [49] pointed out challenges in achieving consistency in coding among experts specifically when utilizing SNOMED CT for clinical research concepts, but urged that “Determining the extent and consistency to which concepts embedded in clinical research can be represented by SNOMED CT will help illuminate unmet needs and inherent complexities that may impede semantic interoperability and effective clinical research data management.”[49] Our study results are consistent with Andrews’ ultimate opinion that “SNOMED CT is a viable and appropriate data standard for clinical research”. In our study, SNOMED CT appears a viable and appropriate data standard for surveillance of mild TBI in particular.
Study Limitations
The main limitation of this manuscript is that it is a study of the content coverage of mild TBI-related surveillance terms. As next steps we would need to validate the model against real data to determine the level of accuracy that our model affords us with respect to biosurveillance for mild TBI. This validation stage may produce other important concepts that require coverage in order to have built a sensitive and specific generalizable model
Another limitation of our study concerns the size of our panel of six TBI clinical experts who reviewed our case definition to rate how much they agreed or disagreed that each term should be included in a case definition of mild TBI. The panel size was not large enough for the panel’s ratings to have statistical power (which would only serve to strengthen study results). The contribution of our expert panel’s ratings nonetheless is supported by justification offered by Jones and Hunter for use of consensus methods in health services research, including the expert panel.[40], and by prior studies that have used expert panels and reviewers to develop and validate terminological systems.[41–46].
A third study limitation was that the human review of medical records that was performed to identify synonyms particular to the presentation of mild TBI in the records of soldiers and veterans, was performed on only a small number of records (due to the labor intensity of the task), and the 8 terms identified by record review were not included in the expert panel ranking of the import of our other terms to the clinical definition of mild TBI. Therefore, although our case definition was quite comprehensive with respect to validated sources from the clinical literature, mild TBI terms important to veterans’ clinical histories may have been missed, and we cannot know how either terminology would have covered terms that might have been identified had review of a larger number of medical records been conducted.
Conclusion
Overall, SNOMED CT outperformed Medcin in concept coverage for a comprehensive case definition of mild Traumatic Brain Injury. Medcin has many useful precoordinated terms. We believe that Medcin would benefit by having more atomic concepts and by providing a mechanism to support post-coordination. Our results help inform the VA and DOD regarding the utility of their respective tools for mapping terms relevant to a clinical diagnosis that is of great concern to both entities, and more generally may help inform the two agencies as they address data sharing challenges in the context of their current activities to share electronic health record data.
While the current study focuses on a case definition of mild TBI that would be certain to contain terms relevant to the condition in U.S. soldiers and veterans, mild TBI also is of concern in the general civilian population, and we believe that our case definition contains the terms relevant to the disorder in the civilian population. Examples include many participants in contact sports and a high proportion of unbelted motor vehicle accidents. TBI is a serious disorder, and mild cases are routinely missed.[10] An accurate case definition has the potential to improve biosurveillance among both the military and civilian populations. Improved detection, early detection, and treatment offer the potential to lessen the impact of mild TBI sequelae on vulnerable populations.
Future research should validate this model against a population at risk for mild TBI.
Figure 2.
Classification scheme and results
Acknowledgments
This work was supported by VA Medical Informatics Fellowship Program (Sponsored by OAA, OHI, and HSR&D), VA Tennessee Valley Healthcare System, Vanderbilt University Department of Biomedical Informatics, VA Tennessee Valley GRECC, VA TVHS Health Service Research (TREP), VISN 6 MIRECC, VA Mid-Atlantic Healthcare System, and in part by grants CDC PH000022 (PLE), CDC HK00014 (PLE),VA SAF03-223-3 (PLE), and NLM: K22 5LM008576-03.
The authors would like to thank Luka Bajzer for technical assistance provided for this research.
References
- 1.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008 Jan 31;338:5. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 2.Independent Review Group Rebuilding the trust: Independent Review Group report on rehabilitative care and administrative processes at Walter Reed Army Medical Center and national Naval Medical Center. Apr, 2007. Available at: http://www.ha.osd.mil/dhb/recommendations/2007/IRG-Report-Final.pdf.). Accessed March 14, 2008.
- 3.Hayward P. Traumatic brain injury: the signature of modern conflicts. The Lancet Neurology. 2008;7:200–201. doi: 10.1016/S1474-4422(08)70032-2. [DOI] [PubMed] [Google Scholar]
- 4.Lew HL, Pogoda TK, Baker E, Stolzmann KL, Meterko M, Cifu DX, Amara J, Hendricks AM. Prevalence of dual sensory impairment and its association with traumatic brain injury and blast exposure in OEF/OIF veterans. J Head Trauma Rehabil. 2011 Mar 7;26(2) doi: 10.1097/HTR.0b013e318204e54b. 201; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Donnelly KT, Donnelly JP, Dunnam M, Warner GC, Kittleson CJ, Constance JE, Bradshaw CB, Alt M. Reliability, sensitivity, and specificity of the VA Traumatic Brain Injury Screening Tool. J Head Trauma Rehabil. 2011 Mar 7;26(2) doi: 10.1097/HTR.0b013e3182005de3. 201; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Carlson KF, Kehle SM, Meis LA, Greer N, MacDonald R, Rutks I, Sayer NA, Dobscha SK, Wilt TJ. Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: a systematic review of the evidence. J Head Trauma Rehabil. 2011;26(2):103–115. doi: 10.1097/HTR.0b013e3181e50ef1. [DOI] [PubMed] [Google Scholar]
- 7.Jackson GL, Hamilton NS, Tupler LA. Detecting traumatic brain injury among veterans of Operations Enduring and Iraqi Freedom. NC Med J. 2008;69(1):43–47. [PubMed] [Google Scholar]
- 8.Warden D. Military TBI during Iraq and Afghanistan wars. J Head Trauma Rehabil. 2006;21:398–402. doi: 10.1097/00001199-200609000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Management of Concussion/mTBI Working Group VA/DoD Clinical Practice Guideline for Management of Concussion/Mild Traumatic Brain Injury. J Rehabil Res Dev. 2009;46:CP1–CP68. [PubMed] [Google Scholar]
- 10.Powell JM, Ferraro JV, Dikmen SS, Temkin NR, Bell KR. Accuracy of mild traumatic brain injury diagnosis. Arch Phys Med Rehabil. 2008;89:1550–5. doi: 10.1016/j.apmr.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control, National Center for Injury Prevention and Control Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem, Sept. 2003 Available at: http://www.cdc.gov/traumaticbraininjury/pdf/mtbireport-a.pdf. Accessed March 12, 2009 and July 15, 2011.
- 12.Lew HL, Thomander D, Chew KTL, Bleiberg J. Review of sports-related concussion: potential application in military settings. J Rehabil Res Dev. 2007;44(7):963–9734. doi: 10.1682/jrrd.2006.12.0169. [DOI] [PubMed] [Google Scholar]
- 13.Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Injury. 2005;19(2):85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control, National Center for Injury Prevention and Control How many people have TBI? Available at: http://www.cdc.gov/TraumaticBrainInjury/statistics.html. Accessed March 17, 2011.
- 15.Sosnoff JJ, Broglio SP, Sunghoon S, Ferrara MS. Previous mild traumatic brain injury and postural-control dynamics. J Athletic Training. 2011;46(1):85–91. doi: 10.4085/1062-6050-46.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slobounov SM, Zhang K, Pennell D, Ray W, Johnson B, Sebastianelli W. Functional abnormalities in normally appearing athletes following mild traumatic brain injury: a functional MRI study. Exp Brain Res. 2010 Apr;202(2):341–354. doi: 10.1007/s00221-009-2141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson J, Sebastianelli W, Slobounov S. EEG and postural correlates of mild traumatic brain injury in athletes. Neuroscience Letters. 2005;377(3):158–163. doi: 10.1016/j.neulet.2004.11.090. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control, National Center for Injury Prevention and Control Concussion and sports. Available at: http://www.cdc.gov/concussion/sports/index.html. Accessed March 17, 2011.
- 19.Centers for Disease Control, National Center for Injury Prevention and Control Traumatic Brain Injury Available at: http://www.cdc.gov/TraumaticBrainInjury/index.html. Accessed March 16, 2011.
- 20.Centers for Disease Control, National Center for Injury Prevention and Control What are the signs and symptoms of concussion? Available at: at http://www.cdc.gov/concussion/signs_symptoms.html. Accessed March 16, 2011.
- 21.Malec JF, Brown AW, Leibson CL, Flaada JT, Mandrekar JN, Diehl NN, Perkins PK. The Mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007 Sep;24:1417–1424. doi: 10.1089/neu.2006.0245. [DOI] [PubMed] [Google Scholar]
- 22.Schwab KA, Bager G, Ivins BJ, Sluss-Tiller M, Lux W, Warden D. The Brief Traumatic Brain Injury Screen (BTBIS): Investigating the validity of a self-report instrument for detecting traumatic brain injury (TBI) in troops returning from deployment in Afghanistan and Iraq. Neurology. 2006 Mar;66(5)(Supp. 2):A235. [Google Scholar]
- 23.Schwab KA, Ivins B, Cramer G, Johnson W, Sluss-Tiller M, Kiley K, Lux W, Warden D. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: Initial investigation of the usefulness of a short screening tool for traumatic brain injury. J Head Trauma Rehabil. 2007 Nov-Dec;22(6):377–389. doi: 10.1097/01.HTR.0000300233.98242.87. [DOI] [PubMed] [Google Scholar]
- 24.Saatman KE, Duhaime A, Bullock R, Maas AIR, Valadka A, Manley GT. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25:719–738. doi: 10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Summary of Meeting Proceedings International State-of-the Science Meeting on Non-Impact, Blast-Induced Mild Traumatic Brain Injury, Herndon, Virginia. May 12–14, 2009. Available at: http://www.dvbic.org/images/pdfs/Summary-of-Meeting-Proceedings---Non-Impact,-Blast.aspx. Accessed online Mar 17, 2011.
- 26.Kuppersmith J, Lew HL, Ommaya AK, Jafee M, Koroshetz WJ. Guest Editorial. Traumatic brain injury research opportunities: results of Department of Veterans Affairs consensus conference. J Rehabil Res Dev. 2009;46(6):vii–xv. doi: 10.1682/jrrd.2009.06.0079. [DOI] [PubMed] [Google Scholar]
- 27.Kuppersmith J, Ommaya AK, Selzer ME, Ruff RL, Lew HL. Guest Editorial. Traumatic brain injury research state-of the-art conference. J Rehabil Res Dev. 2009;46(6):xvii–xviii. doi: 10.1682/jrrd.2009.06.0085. [DOI] [PubMed] [Google Scholar]
- 28.Malec JF, Brown AW, Leibson CL, Flaada JT, Mandrekar JN, Diehl NN, Perkins PK. The Mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007 Sep;24:1417–1424. doi: 10.1089/neu.2006.0245. [DOI] [PubMed] [Google Scholar]
- 29.Nelson LA, Yoash-Gantz RE, Pickett TC, Campbell TA. Relationship between processing speed and executive functioning performance among OEF/OIF veterans: implication for postdeployment rehabilitation. [DOI] [PubMed]
- 30.MacGregor AJ, Dougherty AL, Galarneau MS. Injury-specific correlates of combat-related traumatic brain injury in Operation Iraqi Freedom. J Head Trauma Rehabil. 2010 Aug 30; doi: 10.1097/HTR.0b013e3181e94404. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 31.Weichel ED, Colyer MH, Bautista BS, Bower KS, French LM. Traumatic brain injury associated with combat ocular trauma. [DOI] [PubMed]
- 32.Sullivan K, Garden N. A comparison of the psychometric properties of 4 postconcussion syndrome measures in a nonclinical sample. J Head Traum Rehabil. 2011;26(2):170–176. doi: 10.1097/HTR.0b013e3181e47f95. [DOI] [PubMed] [Google Scholar]
- 33.Sim A, Terryberry-Spohr L, Wilson KR. Prolonged recovery of memory functioning after mild traumatic brain injury in adolescent athletes. J Neurosurg. 2008;108(3):511–516. doi: 10.3171/JNS/2008/108/3/0511. [DOI] [PubMed] [Google Scholar]
- 34.Lew HL, Vanderploeg RD, Moore DF, Schwab K, Friedman L, Yesavage J, Keane TM, Warden DL, Sigford BJ. Guest Editorial. Overlap of mild TBI and mental health conditions in returning OIF/OEF service members and veterans. J Rehabil Res Dev. 2008;45(23):xi–xvi. [PubMed] [Google Scholar]
- 35.Basu New in-theatre clinical guidelines instituted for TBI. U.S. Medicine. 2010;46(3):1. [Google Scholar]
- 36.Medicomp Systems: Medcin Engine Available at http://www.medicomp.com/medcin.html. Accessed online March 17, 2011.
- 37.International Health Terminology Standards Development Organisation About Snomed CT. Available at http://www.ihtsdo.org/index.php?id=snomed-ct0. Accessed July 15, 2011.
- 38.Centers for Disease Control, National Center for Injury Prevention and Control What is Traumatic Brain Injury? Available at: http://www.cdc.gov/ncpip/tbi/TBI.htm. Accessed March 3, 2008.
- 39.Centers for Disease Control, National Center for Injury Prevention and Control TBI Signs and Symptoms. Available at: http://www.cdc.gov/ncpip/tbi/Signs_and_Symptoms.htm. Accessed March 3, 2008.
- 40.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brown SH, Rosenbloom ST, Bauer BA, Wahner-Roedler D, Froehling DA, Bailey KR, Lincoln MJ, Montella D, Fielstein E, Elkin P. Direct comparison of MEDCIN® and SNOMED CT® for representation of a general medical evaluation template. AMIA Annu Symp Proc; 2007 Nov; [PMC free article] [PubMed] [Google Scholar]
- 42.Brown SH, Elkin PL, Bauer BA, Whaner-Roedler D, Husser CS, Temesgen Z, Hardenbrook SP, Fielstein EM, Rosenbloom ST. SNOMED CT: Utility for a General Medical Evaluation Template. AMIA Annu Fall Symp Proc. 2006:101–105. [PMC free article] [PubMed] [Google Scholar]
- 43.Elkin PL, Brown SH, Husser CS, Bauer BA, Wahner-Roedler D, Rosenbloom ST, et al. Evaluation of the content coverage of SNOMED CT for clinical problem lists. Mayo Clin Proc. 2006;81(6):741–8. doi: 10.4065/81.6.741. [DOI] [PubMed] [Google Scholar]
- 44.Rosenbloom ST, Brown SH, Froehling D, Bauer BA, Wahner-Roedler DL, Gregg WM, Elkin PL. Using SNOMED CT to Represent Two Interface Terminologies. JAMIA. 2009;16(1):81–88. doi: 10.1197/jamia.M2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bug WJ, Ascoli GA, Grethe JS, Gupta A, Fennema-Notestine C, Laird AR, Larson SD, Rubin D, Shepherd GM, Turner JA, Martone ME. The NIFSTD and BIRNLex Vocabularies: Building Comprehensive Ontologies for Neuroscience. Neuroinformatics. 2008;6(3):175–194. doi: 10.1007/s12021-008-9032-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chiang MF, Hwang JC, Yu AC, Casper DS, Cimino JJ, Starren J. Reliability of SNOMED-CT coding by three physicians using two terminology browsers. Proc AMIA. 2006:131. [PMC free article] [PubMed] [Google Scholar]
- 47.U.S. Government Accountability Office Report to Congressional Committees Electronic Health Records: DoD and VA Should Remove Barriers and Improve Efforts to Meet Their Common System Needs. Feb 2, 2011. Available at: http://www.gao.gov/new.items/d11265.pdf. Accessed online on March 17, 2011.
- 48.Sayer NA, Nelson D, Nugent S. Evaluation of the Veterans Health Administration traumatic brain injury screening program in the upper Midwest. J Head Trauma Rehabil. 2011 Mar 7; doi: 10.1097/HTR.0b013e3181ff393c. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 49.Andrews JE, Richesson RL, Krischer J. Variation of SNOMED CT Coding of Clinical Research Concepts among Coding Experts. JAMIA. 2007;14(4):497–506. doi: 10.1197/jamia.M2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belanger H, Uomoto M, Vanderploeg RD. The Veterans Health Administration system of care for mild traumatic brain injury: costs, benefits, and controversies. J Head Trauma Rehabil. 2009;24(1):4–13. doi: 10.1097/HTR.0b013e3181957032. [DOI] [PubMed] [Google Scholar]