Abstract
Telemedicine holds great promise for increased access to specialty care services for safety net clinic patients. However, the adoption of these technologies is not a seamless transition for clinicians working in resource-poor settings. Previous research has analyzed workflow issues that arise in primary care settings when adopting telehealth tools but has not examined the unique workflow challenges facing specialists who provide assessments to safety net clinics. Findings are presented from a case study that employed qualitative methodologies as part of an assessment of a teleretinal screening program in Los Angeles urban safety net clinics. The program utilizes external ophthalmologists to perform retinal readings. The case study provides insights into how difficulties that arise in reader workflow are resolved and identifies unique factors requiring consideration when highly trained specialists perform teleretinal readings. The discussion outlines important issues to address when developing telehealth workflow protocols for the safety net, specifically, and their broader applicability in telemedicine.
Introduction
In order to care for an expanding uninsured and underinsured patient population, the United States relies on the health care safety net, a diffuse and, in the case of Los Angeles County, fragmented network composed of community health clinics and county emergent and specialty care facilities.1 Safety net clinics, though usually able to offer their patients primary care, medications, and medical supplies, are often unable to offer specialty services on-site.2 For these, patients must turn either to the private health care market, an option not affordable to the vast majority, or join long referral queues for limited county specialty services. In effect, Los Angeles’ urban safety net offers almost no access to specialty expertise.3 Telehealth technologies, often associated with rural areas where patients are separated from specialists by geographic distance4,5, also hold great promise for increasing access to urban underserved patients.6,7
The urban safety net patient population, due to various socio-economic factors resulting in a systematic lack of access to preventative medical care, is at high risk for developing unregulated chronic conditions and related complications.8,9 One example is the increased prevalence of Type II diabetes mellitus in Latinos and African-Americans.9,10 Poorly managed, this chronic disease can result in diabetic retinopathy, a condition in which excess glucose in the bloodstream causes damage to the blood vessels of the retina. These structurally and physiologically damaged vessels can rupture and hemorrhage within and around the retina, resulting in irreversible blindness. Diabetic retinopathy is the leading cause of blindness in the United States with more than 100,000 new cases identified each year.11 When subject to regular surveillance and timely treatment, however, 90–95% of patients retain vision. Thus, best practices require diabetic patients be screened for retinopathy annually.12,13 Teleretinal screening, when effectively implemented, has the potential to help the safety net meet this goal.
In the typical retinal screening process a care provider uses a camera to photograph the retina and evaluates the images on-site. If evidence of disease is found, the patient is referred to an ophthalmological specialist for treatment. In the Los Angeles safety net this process means that all patients must be referred to county specialty services for their annual retinal screening. Alternatively, in teleretinal screening a trained photographer captures the retinal images and sends them via the internet to a trained reader capable of recommending referral to an ophthalmologist who can provide a definitive diagnosis.14 On-site teleretinal screening allows safety net clinics to identify and forward to county specialty services only those patients requiring treatment and care, greatly reducing the burden on limited county resources while also ensuring patients have realistic access to the recommended annual screenings.
It is well established that the adoption of telemedicine into routine workflows in any health care setting is not a straightforward transition.14,15,16 In urban safety net clinics this process is even more complex.15,16,17 On one hand, telemedicine provides specialty access at primary care clinic locations to a population that previously had negligible access. On the other, clinics’ limited financial, human, and technical resources create high barriers to the adoption of telemedicine.15,16,17 In addition, telemedical practices draw together new and geographically dispersed teams of providers who are unfamiliar with one another, subject to unique local work cultures, and have few opportunities to build clear communicative rapport or trust through face-to-face interactions. These conditions are problematic in developing standardized workflows and patient care protocols. Due to scarce resources, the success of teleretinal screening in the urban safety net rests largely upon human factors, specifically those affecting new collaborations.
Previous studies have addressed teleretinal workflows in primary care clinics serving insured patients, an integrated health system, and rural areas serving both underinsured and private patients.5,14,18 However, little inquiry has been directed toward workflow requirements in a fragmented urban safety net; this paper addresses that gap. Rather than focusing on the primary care clinic workflow, the Los Angeles case study discussed below examines the unique issues faced by external readers who are a critical component of teleretinal screening care. The paper investigates the role that readers - in this case ophthalmologists who provide retinal image assessments - play in the successful implementation of an urban safety net teleretinal screening study. Three themes emerge from study results; (1) The significant role readers play in developing efficient workflow practices and protocols for care delivery, (2) The impact teleretinal screening has on the traditional relationship between the specialist-reader and the primary care facility managing the patient, and (3) How the perception of malpractice liability affects the adoption of telemedicine utilizing external specialty expertise for safety net clinics.
Methods
Study Setting
Institutional Review Board approval was obtained from the Charles Drew University of Medicine (CDU). The study involves six safety net primary care clinics in South Los Angeles with active screening of diabetic patients occurring over a one year period (August 2010 through September 2011). These clinics primarily serve immigrant Latino and African-American patients, with 28% of the population living below the federal poverty level.19 Like many other Los Angeles safety net clinics, the six in this study face such obstacles as high staff turnover, stressed financial resources, limited on-site access to specialty care, and no formal, integrated relationship with county facilities. The research study targets all Type II diabetes mellitus patients, 18 years of age and older within these clinics. Prior to the introduction of teleretinal screening, patients waited long periods after a safety net clinic referral to receive an initial retinal examination, diagnosis, and treatment when necessary, through Los Angeles county hospital facilities. Primary care clinic staff and county hospital administrators estimate that the typical South Los Angeles patient requiring ophthalmological care waits between four and eight months from the date of a clinic referral to the date of a county hospital appointment. For many patients, this appointment consists of an initial visit to an optometrist or a general ophthalmologist who examines and diagnoses the patient. Follow-up care might be rendered immediately or could require referral to another specialist. Given the delay, complications such as proliferative diabetic retinopathy can worsen and, in some cases, result in permanent vision loss. A constant challenge is that the workflow and institutional cultures of the primary care clinics function independently from those in the county facilities.
Four of the six participating clinics had a teleretinal screening program in place prior to the study and used board-certified optometrists to read and assess patient cases for diabetic retinopathy. The other two clinics did not have previous experience with teleretinal screening. The CDU study is structured to fit into the daily culture of these safety net clinics with minimal disruption. It provides two clinics with digital nonmydriatic fundus cameras and all clinics are given access to teleophthalmology software and ongoing staff training. In order to conduct a screening, clinic staff take six retinal images and two external images of a patient’s eyes. The patient’s case, images, and basic biometric data, are then uploaded into EyePACS, a teleophthalmological viewing software developed at UC Berkley and already in use in many California safety net clinics.20
The CDU study also provides for three board-certified ophthalmologists to be contracted as image readers. These ophthalmologist-readers were trained to use EyePACS and provide their services to the study for a limited compensation. The ophthalmologists fill in a report that includes an assessment of the patient’s case and asks the reader to rate the quality of the retinal images provided, determine whether the information was sufficient for interpretation, and fill in free text fields labeled “Diagnosis” and “Referral Status.” Ophthalmologists were selected for the study based upon previous exposure to telemedicine (OP2, OP3) and interest and experience in working with medically underserved patients (OP1, OP2, OP3). One ophthalmologist (OP1) had previous experience working with teleophthalmology in a developing country and had some knowledge of its use in the United States, whereas, another (OP3) had participated for several years in an urban safety net teleretinal screening program.
Approach and Procedures
The case study’s qualitative descriptive method21 consisted of semi-structured interviews with all of the project’s readers (3 ophthalmologists or 100% of this category) as well as informal observations of clinic workflow related to teleretinal screenings. Similar interviews were also conducted with clinic staff and focus groups are being conducted with patients to understand the experience of these parties. However, those data will be the subject of future publications as the present discussion focuses on the experiences of ophthalmologist-readers. Prior to all research activities informed consent was collected from each respondent.
Though data in the current discussion are limited to a singular case study with a limited sample size, results are informative regarding the impact of local context on the provision of telemedicine-based care. Case studies are appropriate where they illustrate a new phenomenon in a manner that expands existing understandings of practices that are so complex as to only be understood through an investigation of the local context.22 The intricate and fragmented health care network that serves the safety net patient population is indeed this sort of complex environment, described by a participating clinic’s medical director as requiring a “Machiavellian approach” to negotiate. Interviews with the ophthalmologists ranged from 45 to 92 minutes (average 69 minutes) and were open-ended discussions. The main categories addressed included: (1) Ophthalmologist’s experiences providing medical expertise for teleretinal screening, (2) Ophthalmologist’s interactions with each other and with clinic health care providers and staff, and (3) Ophthalmologist’s experiences with telemedicine. Within these domains, ophthalmologists were asked to describe their relationship to patients receiving teleretinal readings and the primary care physicians at the safety net clinics. They were then asked to discuss their understanding of how these relationships, brokered through telemedicine, were differentiated from situations where they had face-to-face interactions with patients. As background to these interviews, CDU researchers observed workflows facilitating the use of the technology and held unstructured discussions with clinic staff during weekly scheduled visits, as recorded in field notes. As it became clear to CDU researchers that clinic workflow and other issues were impacting reader workflow, an exploration of reader concerns was built into the interviews with ophthalmologists.
Data Analysis
Interviews were audio-recorded and transcribed by a professional transcription company. Given the sample size, all transcripts were read in their entirety. Open coding was used to identify similar topics and themes in the interviews. The transcripts were examined line-by-line for code assignment, without predetermined categories influencing what would be coded. After the transcripts had been coded, the codes were grouped into thematic categories and transcripts reviewed again. To ensure validity and reliability of analyst interpretations, two investigators with expertise in qualitative methods analyzed the data and discussed the results. Interview data was corroborated with the first author’s direct observations of workflow in the clinics and CDU study personnel’s experiences providing support to clinic staff. Finally, the results were discussed with the entire project team at weekly meetings.
Results
Challenges to the Expected Workflow in the CDU Teleretinal Screening Study
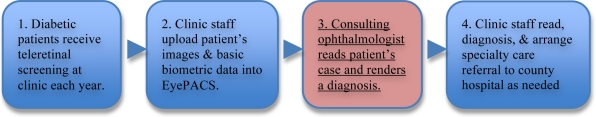
The original workflow envisioned in the study design (see Figure 1 on next page) consisted of the following process: (1) Diabetic patients receiving treatment at a participating clinic obtain a teleretinal screening for diabetic retinopathy at least once a year from clinic staff who explain the process to them; (2) Clinic staff conducting the screening upload the patient’s images and basic health information into EyePACS; (3) External ophthalmologists read and review each patient’s case and describe their findings in an EyePACS report; and (4) Clinic staff read the EyePACS report, share and explain the results with patient, and arrange for a referral to the county hospital, should treatment be recommended. The expected workflow was shared and vetted with clinic administrators and ophthalmologists at the start of the study. Once put into motion, CDU researchers discovered that the third step, involving reader workflow, required further exploration, discussion, and re-organization. CDU researchers worked with the ophthalmologists to rearticulate and improve the overall teleretinal screening process.
Figure 1:
Anticipated Workflow
Under the project contract, the investment of ophthalmologists was limited to reviewing all cases uploaded by the clinics participating in the project within two weeks of entry into EyePACS. For the first few months (beginning in August 2010) the reader workflow advanced smoothly with cases receiving assessments within the expected time frame. However, in mid-November 2010 through mid-December, 2010, CDU researchers noted that both the ophthalmologists and clinic staff were expressing concerns with the teleretinal screening process. Specific problems included: (1) Some ophthalmologists were reviewing more cases than others, (2) Reviews were occurring at erratic time frames, (3) Cases uploaded by certain clinic staff were not being reviewed by any ophthalmologist, (4) Ophthalmologists regularly reported being unable to render a complete assessment based on poor quality of the images and noted discomfort with this situation, and (5) Length of time to completed reading appeared to be increasing past the two week mark on several individual cases.
For a short period of time in late November 2010, these problems culminated in the ophthalmologists stopping case reviews and expressing concerns in a more systematic manner to CDU researchers. These concerns can be broadly grouped into two domains. The first domain relates to the lack of adequate information contained in cases uploaded into EyePACS. Specifically, ophthalmologists were concerned about (1) poor quality retinal and external eye images and (2) missing patient biometric information (e.g., hemoglobin A1C, height, weight, and number of years with the disease). Ophthalmologists considered both these kinds of information necessary for a full interpretation of a patient’s case. In a second domain, the ophthalmologists expressed concern as to whether adequate and timely treatment would be provided to the patients they had determined to require care. The ophthalmologists felt that failure to deliver such care would have important ethical, moral, and legal implications and desired clarification before continuing to read cases. Despite these workflow issues it is significant to note that as of February 24, 2011, project ophthalmologists had reviewed and read 1,028 patient cases, resulting in recommendations for 167 referrals to county facilities for specialty care. Detailed results are presented from the interviews in the two domains.
Lack of Adequate Information:
For the ophthalmologists “information” necessarily included images of the eye and retina, as well as accompanying biometric data. Ideally, they hoped that each case would have eight high quality images and complete biometric data. However, in practice this was rarely the case. For example, biometric data are not required fields for the submission of a patient case through EyePACS and were often missing. None of the ophthalmologists knew why these fields were blank and found this frustrating. Though not formally presented in the current discussion, initial findings from staff interviews indicate that the lack of clinic resources, common to the safety net setting, is a major factor. One ophthalmologist (OP1) said, “[H]alf the information that you’re requesting isn’t even there. I have no vision [of the images and] I don’t know what their blood sugars are … [Y]ou can’t really make a full assessment … so it turns into, well, let me just screen them to see if I see anything abnormal.” The lack of adequate image quality was also frustrating for this ophthalmologist who, in his residency, had used similar equipment and recognized the criteria for photo quality. For OP1, “sometimes [it is] very, very difficult… as [I]’ve gone through more of these [images], [I am] like, ‘Oh, they’re all artifacts.’ There’s no way that 700 people in the world are going to have cotton wool spots [in the exact same place]. So it has to be a smudge on the lens or [the camera is] not focused.”
For another ophthalmologist (OP2) the question of image quality was one of trust because this factored significantly in her ability to render an accurate diagnosis. According to OP2, “[Y]ou’re trusting an image … because there’s a level of trust there of the photographer I think that you’re kind of trusting this person got the best possible image and the best possible views and if they saw something over on the edge that they went and captured that. That their desire to be comprehensive would be there… You’re giving a diagnosis without actually seeing a patient to the best of your ability and that’s sort of a larger issue or I should say, sort of a higher struggle, if you will, because in the end these patients are getting an exam that they probably wouldn’t get otherwise.” Through repeated virtual interactions on cases uploaded into EyePACS, OP2 felt that she built a relationship of trust, measured in image quality, with individual photographers, “Well it’s interesting because I don’t know them, but I do know their names and I know their pictures and so you get to know their style and honestly you’re more relieved whenever… it’s the person that takes good pictures”. For these cases OP2 felt reading was, “much less of a struggle than it is if it’s one of the people that really don’t seem to care much or for whatever reason don’t take very good images repeatedly.” Interestingly, OP2 suggests here that image quality may indicate the photographers’ level of investment.
In controlling for poor quality images and lack of information, two project ophthalmologists described how they attempted to read in a manner that might partially compensate. One ophthalmologist (OP2) described a system of reading poor quality photographs in which she tracked back and forth between images to distinguish between spots due to artifacts on the lens, such as dust or lint, versus what might be a cotton wool spot, pathology indicative of diabetic retinopathy. For this ophthalmologist, her purpose is to identify whether any, “impending bad things [are] about to happen” and she adjusted her reading of the images to assess for such potential while, at the same time, controlling for poor quality information.
The third project specialist (OP3) relied upon her knowledge of the community and tendencies within particular populations to help compensate for inadequate information. According to OP3, “[O]nce I click on a patient, I look at their name, because sometimes they say ethnicity not specified. And I like to know the ethnicity of my patients because demographics mean a lot. You know that if a patient is Hispanic they might have some diabetic retinopathy. If they’re African American, they might have some glaucoma. So there’s certain disease prevalence that the demographics help me a lot. I look at their age [and they number of years they have had diabetes] … I like the background stories…So sometimes if you don’t get a lot of information, it just gives me an idea…”
Though all ophthalmologists felt that, for the most part, they were able to compensate for the lack of information and poor image quality, at least for the purposes of recommending a referral for further examination, most felt that this required extra time and was not a good use of resources. Specifically, poor image quality led each ophthalmologist to give conservative assessments leading to a greater number of recommendations for referrals than was probably necessary. Thus, while the teleretinal screening provided did reduce total number of referrals by more than 80%, the ophthalmologists felt an even greater benefit could be easily realized with improved image quality.
In using EyePACS, readers typically review cases using a large screen desktop or laptop computer. To examine an image a reader clicks on a small thumbnail of the picture that then loads a medium or large image. Given the need to compensate for poor image quality, this limited range of sizes made it difficult for ophthalmologists to move easily around the photograph and identify potential problems. Moreover, the time that the computers took to enlarge and load images lengthened the process. In trying to ameliorate the loss of time due to low image quality and the high patient load, one ophthalmologist (OP3) developed a workaround by using her personal iPad to view the images. The iPad allows magnification of images without reloading, which was not possible on her usual computer. Furthermore, it had WI-FI connectivity, allowing portability and greater convenience. OP3 felt the range of enlarging options offered by the iPad allowed her to concentrate on specific points within the image and to target these points more rapidly. According to OP3, “Now that I have my iPad it makes [reading images] much easier [than] doing it with a desktop and a mouse… I can do per patient maybe five minutes whereas before it would take easily ten minutes… and the image quality is much better.” Of additional interest, OP3 reported sharing this workaround with OP1 who, she believes, is now also using an iPad.
In summary, the ophthalmologists felt inadequate information inhibited their ability to render a full assessment of disease severity, making it difficult to fully realize study objectives. Two of the three ophthalmologists (OP2, OP3) deemed this unfortunate because their readings likely would be the only access to ophthalmological care that the majority of these patients would have. For this reason, these individuals felt it was especially important to give the patient as complete an assessment as possible, for which image quality was a significant factor. However, each ophthalmologist developed different workarounds for dealing with these problems based on personal knowledge, use of additional technology and previous experiences practicing medicine in the underserved community.
Ethical, Moral, and Legal Concerns Relating to Provision of Treatment after Teleretinal Screening:
In addition to inadequate information uploaded to EyePACS, project ophthalmologists were concerned that if they determined a patient requireed follow-up treatment, they had no way to ensure that an opportunity would be provided. In large part, this concern gravitated around the ophthalmologists’ perceptions of the legal, ethical, and moral obligations that they had as physicians to the safety net patients for whom they were providing care. In describing his priorities, OP1 said, “So [my] number one [priority] is to identify pathology that I think may cause blindness… to identify that and make sure that they get some type of follow-up treatment.” OP1 felt that he was unable to fully achieve the latter goal because he could only indicate the length of time until referral should be completed but could not ensure that the outcome. This doctor defined the completion of a referral as ensuring that a patient received an appointment for care, not necessarily that the patient received care. Moreover, OP1 felt he could ensure this in a regular retinal screening not involving telemedicine because he would have physical access to the patient. In trying to expedite care for emergent cases discovered through study screenings, OP1 even attempted to refer patients requiring immediate attention directly to himself when he was scheduled at the local county facility, rather than using the county’s electronic referral system. However, for administrative reasons, the county would not allow OP1 to continue direct referrals in this manner. After being informed that he could not bypass the county referral system, OP1 said that he now, “just use[s] very vague guidelines. They need to be seen within six months. They need to be seen within four months or... This is an urgent referral that needs to be seen within a month. That’s as far as I go.” Though morally uncomfortable with simply letting a patient in need leave his “virtual” care without ensuring an appointment for follow up services, OP1 felt his hands were tied. Moreover, for OP1, “it should not fall to doctors to administrate”.
In teasing out the issues presented by OP1 above, OP3 differentiated between her moral and ethical duties, a distinction that hinged partially on her physical access to the patient. According to OP3, “I think from a moral standpoint, yes [I have a duty to ensure care]. From an ethical standpoint, no. Because my responsibility is to read the images and interpret the images. And it’s very different than having a patient there in front of you that can walk out of your office with an appointment … when the patient is sitting there in front of me I know the patient will be taken care of. No doubt, no question. If I had to walk them to the retina specialist that’s just how I am. Whereas [with teleretinal screening] from an ethical perspective I feel like my responsibility is to interpret the images, the people on the other end, it’s their responsibly to get them through wherever they need to get them through.”
What OP3 discusses in terms of her ethical obligations also entails a significant connection to legal considerations voiced by other project ophthalmologists and most concisely described by OP1 who said, “I mean there is liability involved. As long as I am seeing a patient that I feel needs to be seen urgently!” In this regard OP3 mentioned, “even OP1 and I were talking about this a little bit. We were talking about, well… should we call our malpractice people and see what coverage we have under teleophthalmology?... Because really, what is – is it our responsibility once – I’m not sure, it’s a gray area… I would really like to find that out.” Of particular concern to the ophthalmologists was their uncertainty about the protocols for delivery of recommended care, “on the other side of the equation” (OP3), i.e., at the primary care clinics, given that teleretinal screening is a fairly recent introduction to this care setting. For each of the ophthalmologists in the study, the practice of telemedicine produces a tenuous relationship between the specialist acting as an image reader, other care providers, and the patient. At one extreme OP1 simply said, “there isn’t a relationship.” However, when pressed further OP1 acknowledged that a relationship with the patient begins when he first opens a case file and is completed when he submits the report through EyePACS. This conceptualization was similar to that voiced by both OP2 and OP3.
The preference for all ophthalmologists would be to ensure that a patient needing care would have an opportunity for a follow up appointment, something that OP1 felt could be easily built into the teleretinal screening protocol. OP1 believes teleretinal screening has, “got great potential … [but] there needs to be a – I guess a catch net or a protocol or something in place that will allow these individuals that have been identified as sick to be either treated or seen in a timely fashion. That it’s built into the system so that if you grade a person as severe, very severe diabetic retinopathy, and you click on it, the [EyePACS] system should automatically generate or prompt the physician, ‘This patient qualifies as severe diabetic. Would you like to make a referral?’ If so, within what time frame? One week, two weeks… three months, one month? And that would really help hone in on [the problems].”
Developing and Implementing a Pragmatic Workflow Protocol
In order to resolve the issues discussed above the ophthalmologists took two actions. First, they requested that the three clinic staff with the worst images ratings at two of the clinics receive retraining on the use of the digital fundus camera. The staff complied and coordinated visits with other clinics and received retraining from other photographers. In some cases the clinic staff were not compensated for the time required for retraining. Preliminary data collection indicates that clinic staff assumed the additional workload because of their desire to provide quality care to safety net patients. After the retraining, the ophthalmologists began to review cases by all clinic staff, with many of those who had been retrained receiving higher quality ratings. It is also important to note that the retrained clinic staff had been working with cameras that were discovered to be faulty in February, a complication that may have led to the original low ratings. Secondly, the ophthalmologists clarified their responsibility vis-à-vis the patients with a supervising medical officer and county administrators and collaborated amongst themselves to design a workflow to ensure that all patients received assessments and that cases requiring immediate care would be flagged. Specifically, this system change incorporates a calendar that assigns each day to a single ophthalmologist who is then responsible for reviewing and assessing every case uploaded into EyePACS on that day. In addition, OP2 is working with EyePACS designers to develop a standardized system indicating the level of severity of a patient’s disease and the requisite timing of follow up care. While the standardized system of referrals has yet to be developed, the expectation is that it could help the triage process by more emphatically identifying patients needing further care and the appropriate timeliness of treatment.
Discussion
From the qualitative findings, three significant themes emerged regarding the role of specialists as readers for teleretinal screenings in safety net settings. The first theme relates to the development of efficient reader workflow practices and protocols for care delivery. In this study, the ophthalmologists took the initiative to develop workaround processes when the need arose, including comparison across images to differentiate between visual artifacts and actual pathology, and adopting additional technologies, such as the iPad for viewing retinal images. Moreover, the ophthalmologists shared their individual workarounds with one another and, in some cases, learned, adopted, adapted, and improved on these innovations. In developing other workflow solutions, the ophthalmologists were aided by CDU researchers who helped to coordinate workarounds such as clinic staff retraining and the implementation of a calendaring system.
These positive outcomes speak to the need for collaborative approaches amongst care providers at multiple levels, particularly in the provision of spatially fragmented telemedicine care. In large part, such collaboration occurred organically in this teleretinal screening study, building from intermittent discussions that ophthalmologists had with one another while working at the same clinic or that were initiated through telephone or email conversations with CDU researchers. That the ophthalmologists took advantage of such opportunities accords well with the high levels of motivation that each expressed when describing his or her commitment to serving the safety net population of urban Los Angeles. Because similar spontaneous communications among readers in teleretinal screening programs might not always occur and not all may be as highly motivated, it would be advisable that such opportunities for communication among providers be built into future teleretinal screening program protocols. Possibilities include monthly or quarterly meetings, an email listserv, or structured and continuing training and feedback interchanges with health care providers in similar projects. Such forums could also prove valuable for individual innovators to share their personal creative and effective workarounds. Case study results also suggest that similarly allowing for dialogue between the different levels of care providers – primary care, specialty care, consulting readers - involved in a teleretinal screening would also more comprehensively enhance these programs. Strengthened avenues of communication would improve readers’ understanding of circumstances at the primary care safety net clinic. The net result should increase readers’ awareness of the constraints that such resource-poor settings face, build trust levels between different care providers and clinic staff working with the same patient, allow problems to be addressed with greater speed, and provide better overall care to the patients.
The second theme that emerged relates to the manner in which teleretinal screening impacts the traditional relationships between a specialist-reader and the primary care facility managing the patient. Specifically, the results show that the ophthalmologists feel this relationship becomes attenuated when telemedicine allows the specialist to be “virtually” present in the patient examination room. On the one hand, this situation is advantageous for the provision of specialty care to a diffuse and underserved patient population: it allows ophthalmological expertise to be brought into multiple locations, such as the six safety net clinics in this study, at the same time. On the other hand, inherent complications must be taken into account when specialists transition away from “face-to-face” interaction. Specifically, the ophthalmologists expressed frustration that they had very little control with overall workflow protocols except in the way they read photos. In response, they developed new processes for themselves and then let loose their assessments into the system in an act of faith that all would somehow work out and the patients would receive care. The ophthalmologists desired to offer the patients a similar level of care as in a face-to-face screening where they would be able to offer a full assessment and opportunity for treatment. However, as readers the ophthalmologists were limited to the role of a an assessment consultant rather than a physician managing the patient. The ophthalmologists did not automatically differentiate between these roles and, in this study, this difference required clarification. Specialists providing readings may benefit from a formal orientation as to the contours of their role as reader and how this concretely differs from their role as a physician managing care. The content of the orientation might vary with readers’ level of expertise (e.g., an ophthalmologist might require a different orientation than an optometrist).
The third theme relates to the ophthalmologists’ perception of the possibility of malpractice liability and how this might impact the adoption of telemedicine in safety net settings. Medical malpractice liability, a tort defined through state laws, is triggered when, after a physician-patient relationship is formed, the physician fails to deliver the accepted standard of care common in local medical practice.23 Malpractice as applied to telemedicine has yet to be clearly defined.24,25 Under California state law, physicians involved in use of telemedicine are required to render an equitable standard of care no matter how that care is provided, whether it be virtual or face-to-face (Cal. Bus. & Prof. Code 2290.5). In terms of economic damages (e.g., medical costs, loss of wages, and burial costs), under California law, medical malpractice awards are subject to joint and several liability, meaning that an injured plaintiff can pursue any defendant for the total amount. Defendants, if there are multiple parties, such as a primary care provider, a clinic, and a specialist, are responsible for apportioning blame amongst themselves and this determination is the subject of a separate action. Though non-economic damages (e.g., pain and suffering or negligence) are subject to several liability, meaning each defendant is apportioned a percent of blame and is solely responsible for the corresponding fraction of the award (CA Civil Code § 1431.2), for various strategic reasons all potential parties are often joined in the suit. Because costs associated with malpractice lawsuits and awards can be substantial, physicians tend to practice “defensive” medicine to avoid individual and institutional liability. It follows that physicians behave conservatively and are reticent to adopt new technologies that might increase their exposure to liability. Furthermore, in California a physician working as part of a care provider team must necessarily be concerned with the actions of the other doctors as he may potentially be held responsible for damages related to their actions. Ophthalmologists acting as readers on teleretinal screening programs are, therefore, understandably concerned even though it is clear that the bulk of the liability rests with the primary care clinic that is managing the patients. These specialists would, therefore, necessarily feel personally invested with establishing workflows and protocols that clearly delimit their responsibilities to the patient and, ideally, ensure that the patient receives care.
In this teleretinal screening study, the ophthalmologists demonstrated a desire to clearly delimit their relationships both to the patient and to the primary care clinics. In this sense, all ophthalmologists indicated that telemedicine weakened their relationship to the patient by confining it to the five to fifteen minutes it took them to open a case on EyePACS, evaluate the images and read the case, and write a review. After the review was entered into the system, all ophthalmologists considered the physician-patient relationships terminated. The only exception might be if a primary care provider attempted to contact the specialist, a situation that had not occurred in the CDU study. Though each ophthalmologist expressed this view when talking about liability issues, two of them were concerned about whether this was the correct legal interpretation. This last finding has real and important implications for the participation of specialists in telemedical programs serving safety net populations. These specialists work not for high rates of monetary remuneration, but because of other motivations, such as a personal attachment to the local community. Left unclarified, the perceived threat of malpractice liability may discourage participation in telemedical programs by specialists, who are either unpaid or underpaid for their work in the safety net. To seek solutions, it would be advisable to directly address this issue with readers, especially those who are ophthalmological specialists and who could have heightened perceptions of liability. Specifically, these concerns could be covered in a specialized reader orientation that directs readers toward evaluating images for evidence of disease and writing EyePACS reports without diagnosing pathology. Teleretinal screening could then be used to bring ophthalmological expertise into the safety net clinic with fewer disruptions while continuing to function effectively as triage.
Conclusion
This case study is limited in its scope and localized nature. The research is nevertheless valuable in illuminating reader workflow issues that are integral to the successful implementation of teleretinal screening in the urban safety net. As the case illustrates, unresolved workflow issues have the potential to stop or slow new and innovative telemedical practices even if all parties agree that these programs have great potential. Moreover, the concerns raised are particularly relevant for safety net health care providers who, already operating in settings where resources are stretched past capacity, cannot run the risk of additional costs or liability. In this sense, these settings that have the most to benefit from successful adoption of telemedicine also run the greatest risk and, therefore, may be conservative adopters of such technologies. To encourage successful adoption, the problematic issues must be taken into account when developing new workflows around telemedicine and resources allocated accordingly.
The exact parameters of the socio-medical and legal relationships formed through telemedical practice are, as yet, ill-defined. Care providers, aware of this uncertainty, will act conservatively in allocating resources and adopting programs when success or outcomes appear questionable. Because this tendency may prevent full implementation of programs that can bring great benefit to patients, the workflow issues raised in this CDU case study deserve urgent attention. Several innovative solutions have had positive results within the confines of this study. Broader resolution of these issues for the safety net setting is essential for two reasons. First, underserved patients with little access to face-to-face specialty care at point of primary care could receive a form of consultation through timely and effective telemedicine. Secondly, the special needs of these patients for rapid diagnosis could be met as a prerequisite to referral for care, delivery of which often requires a several month wait time in long queues for the overburdened county hospital system. To better realize the promise of teleretinal screening in providing timely access to critical specialty care in safety net settings efforts should be increased to; enable specialists to understand their specific roles in screening, to collaborate more effectively with co-providers, and to resolve fears regarding legal and ethical principles.
Acknowledgments
This work was sponsored by the NIH under grant U54RR026138-01S2.
References
- 1.Wasserman J, Asch S, Bamezai A, Wynn B, Ringel J, Fulton B, et al. Los Angeles County. Los Angeles, CA: Rand Institute; 2004. Financing the Health Services “Safety Net”. [Google Scholar]
- 2.Gusmano MK, Fairbrother G, Park H. Exploring the limits of the safety net: community health centers and care for the uninsured. Health Aff. 2002;21(6):188–194. doi: 10.1377/hlthaff.21.6.188. [DOI] [PubMed] [Google Scholar]
- 3.George SM, Hamilton A, Baker R. Pre-experience perceptions about telemedicine among African Americans and Latinos in South Central Los Angeles. Telemed J E Health. 2009;15(6):525–530. doi: 10.1089/tmj.2008.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fleischer LD, Dechen JC. Telemedicine and E-Health Law. New York: Law Journal Press; 2006. [Google Scholar]
- 5.Puskin DS. Opportunities and challenges to telemedicine in rural America. J Med Syst. 1995;19:59–67. doi: 10.1007/BF02257191. [DOI] [PubMed] [Google Scholar]
- 6.Chang BL, Bakken S, Brown SS, Houston TK, Kreps GL, Kukafka R, Safran C, Stavri PZ. Bridging the digital divide: reaching vulnerable populations. JAMIA. 2004;11(6):448–457. doi: 10.1197/jamia.M1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shea S, Starren J, Weinstock RS, Knudson PE, Teresi J, Holmes D, et al. Columbia University’s Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. JAMIA. 2002;9(1):49–62. doi: 10.1136/jamia.2002.0090049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams DR. Race, Socioeconomic status, and health: The added effects of racism and discrimination. Ann NY Acad Sci. 1999;896:173–178. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 9.Baker RS. Diabetic retinopathy in African Americans: vision impairment, prevalence, incidence, and risk factors. Int. Ophthalmol. Clin. 2003;43(4):105–22. doi: 10.1097/00004397-200343040-00011. [DOI] [PubMed] [Google Scholar]
- 10.Baker RS, Watkins NL, Wilson MR, Bazargan M, Flowers CW. Demographic and clinical characteristics of patients with diabetes presenting to an urban public hospital. Ophthalmology. 1998 Aug;105(8):1373–9. doi: 10.1016/S0161-6420(98)98015-0. [DOI] [PubMed] [Google Scholar]
- 11.Bernardes R, Dias J, Cunha-Vaz J. Mapping the human blood-retinal barrier function. IEEE Transactions on Biomedical Engineering. 2005;52(1):106–115. doi: 10.1109/TBME.2004.839801. [DOI] [PubMed] [Google Scholar]
- 12.Ferris FL. How effective are treatments for diabetic retinopathy? JAMA. 1993;269(10):1290–91. [PubMed] [Google Scholar]
- 13.Wang F, Javitt JC. “Eye care for elderly American with diabetes mellitus. Failure to meet current guidelines”. Ophthalmology. 1996;103(11):1744–50. doi: 10.1016/s0161-6420(96)30432-6. [DOI] [PubMed] [Google Scholar]
- 14.Yogesan K, Kumar S, Goldschmidt L, Cuadros J. Teleophthalmology. Berlin: Springer; 2006. [Google Scholar]
- 15.May C, Harrison R, Finch T, MacFarlan A, Mair F, Wallace P. Understanding the normalization of telemedicine services through qualitative evaluation. JAMIA. 2003;10:596–604. doi: 10.1197/jamia.M1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanriverdi H, Iacono CS. Diffusion of telemedicine: a knowledge barrier perspective. Telemedicine J. 1999 Fall;5(3):223–244. doi: 10.1089/107830299311989. [DOI] [PubMed] [Google Scholar]
- 17.George S, Garth B, Fish A, Baker R. Perceptions of health information technology in community clinics. Poster presentation. 12th Research Centers in Minority Institutions International Symposium on Health Disparities; Nashville,TN. December 6–9, 2010. [Google Scholar]
- 18.Conlin P, Fisch B, Orcutt JC, Hetrick BJ, Darkins AW. Framework for a national teleretinal imagining program to screen for diabetic retinopathy in Veterans Health Administration patients. J Rehabil Res Dev. 2006 Sep-Oct;43:741–48. doi: 10.1682/jrrd.2005.08.0146. [DOI] [PubMed] [Google Scholar]
- 19.Department of Public Health, Los Angeles County Racial/Ethnic Distribution of Population by Geographic Area – 2000. Found at http://publichealth.lacounty.gov/spa6/stats/tables/spa6_appendix_a_table_01.htm. Visited on March 13, 2011.
- 20.Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3(3):509–16. doi: 10.1177/193229680900300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Health. 33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]; Ragin CC. The distinctiveness of case-oriented research. Health Services Research. 1999;34:1137–1151. [PMC free article] [PubMed] [Google Scholar]
- 22.Garner BA, editor. Black’s Law Dictionary. 6th Ed. St Paul: West Group; 1990. Medical malpractice liability; p. 959. [Google Scholar]
- 23.Leung ST, Kaplan K. Medicolegal aspects of telepathology. Human Pathology. 2009;40:1137–1142. doi: 10.1016/j.humpath.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Stanberry B. Legal and ethical aspects of telemedicine. J of Telemedicine and Telecare. 2006;12:166–175. doi: 10.1258/135763306777488825. [DOI] [PubMed] [Google Scholar]