Abstract
Objective
To determine the feasibility of gathering Complementary and Alternative Medicine (CAM) data directly from the patient via a computerized patient interview.
Design
A quantitative descriptive study was utilized to determine whether patients would be willing to self-report their CAM usage and whether the self-reported data complements clinicians perceptions and medical records.
Measurements
40 patients were recruited to test the computerized patient interview application. Clinicians and staff (n=15) were also surveyed to determine their perceived CAM usage. In addition, a retrospective chart review (n=100) was done to estimate the documented CAM usage rate.
Results
In this study, we had a 85% participation rate, suggesting patients are willing to share their CAM use through the computer application. The self reported usage rate was 85%, as compared to the chart documented usage rate of 9.5% and the average clinician/staff estimated usage rate of 43%.
Introduction
The use of CAM amongst patients in the US is well documented. CAM has grown to an estimated 50 billion dollar industry with an estimated 30–50% of patients utilizing some form of CAM in their healthcare 1–10. In spite of this trend, there appears to be a hesitance on the part of the patients to share this information with their healthcare provider 11, 12. Many patients have adopted an attitude of “if they don’t ask, I won’t offer” toward the communication on this topic with their primary care providers 12. On the other hand, there is a significant risk of herbal supplements interacting with prescriptions medications and causing harm to the patient 2–4, 13, 14. Given the potential for drug-herb interactions, it becomes increasingly important to document dietary supplement use along with prescription medications. The ability to search for potential interactions and to alert the patient and clinicians is dependent on the continuous maintenance of both lists.
To improve patient safety and better monitor CAM usage, we sought to study the feasibility and potential benefit of gathering this data from the patient utilizing a computerized patient interview system. Our research questions are 1) Are patients willing to disclose their CAM usage using the computer application? 2) Can the patient self-reported data complement the information gathered by clinicians and recorded in medical records? 3) Can this data be gathered with a level of quality that enables clinical decision support and therefore makes the effort worthwhile?
Materials and Methods
We developed a simple computer interview application to collect CAM usage data directly from patients. After a brief usability study and user interface (UI) improvements, we conducted a feasibility study of the application in an outpatient cardiology clinic. To measure the potential benefit of the self-reported data collected by the application, we surveyed clinician’s perceived CAM usage as well as reviewed a random sample of charts from the same clinic. The rates of CAM usage from the three sources (patients, clinicians, and chart review) were compared.
Setting
The study was completed in the Cardiovascular Clinic at the University of Utah.
Recruitment
Inclusion criteria were patients referred to the University Cardiovascular center for various reasons, excluding transplant patients. This includes consults, heart failure, congenital, and all other areas of cardiology except transplant. Transplant patients are excluded because 100% of those are taking dietary supplements and all are physician prescribed and very tightly monitored by the physician and the pharmacist. All other CV patients are included as CAM usage tends to be higher amongst the chronically ill. All patients were at least 18 years of age and English speaking.
CAM Interview Application
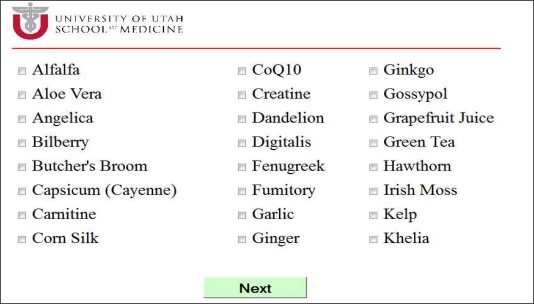
The interview application was implemented as a web portal displayed in a browser on an iPad, with a MySQL database backend for storage. The site was coded in Java/JSP. The first page is an introductory page, which explains why this study is important to the patient. This is followed by a description of the three categories of pills that a patient might take, to ensure that they understand the difference. These include prescription drugs, over-the-counter drugs, and dietary supplements. The dietary supplement information is what we are focusing on. Next, the application invites patients to select from a list of common dietary supplements (Figure 1). The list contains the supplements with known interactions to prescription cardiology drugs, along with a few of the most common dietary supplements taken by cardiac patients. We consulted the Natural Medicines Comprehensive Database to create the list.
Figure 1.
User Interface for Common Supplements Used by Cardiac Patients
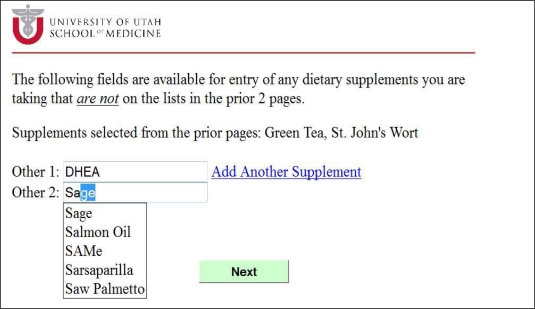
To provide for future functionality such as identifying additional interactions, as well as to avoid the inevitable question of why a patient’s supplements were not included in the list, a free-form data entry screen was also provided. Auto-suggest capability was built into the UI to decrease the typing required and to prevent spelling errors (Figure 2).
Figure 2.
CAM Free-form Entry Screen
Usability Testing
A pre-study test phase included 4 patients, which was adequate to expose usability issues in the user interface. The patient was asked to navigate through the web site, indicating verbally any information that was not clear to them. The research assistant looked over their shoulder, noting any confusion on the part of the patient as to intended use and flow of the site. The discovered flaws were corrected.
Feasibility Testing
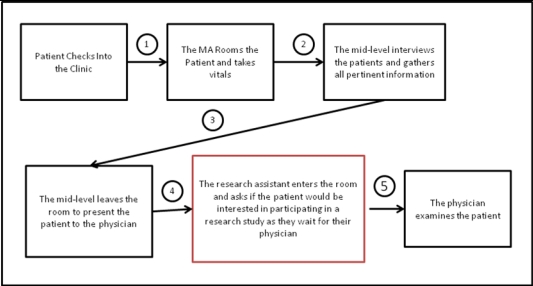
Each patient was interviewed in the examination room after the mid-level providers gathered the pertinent clinical data and before the physician entered the room for examination (Figure 3). The research assistant (RA) knocked on the door, entered the room, introduced herself and the study, and asked if the patient would be interested in participating in a research study as they waited for their physician.
Figure 3.
Recruitment Workflow
The patient was then presented with the study consent form that contained all the usual elements of a consent form, as well as a study ID field. This study ID was retrieved from the web site at the end of the online interview and noted in this field. This is the only link between the patient’s identifying information (from the signature field on the consent form) and the study data stored in the database.
After signing the consent form, the patient was presented with an iPad with the study home page displayed in the browser. Consenting patients then proceeded to the computer interview.
Survey of Clinician and Staff Perceptions of CAM Use
Physicians, mid-level providers, and MAs were surveyed in order to form some insight into their perceptions of the prevalence of CAM use in Cardiology. The goal here was to weigh these perceptions against the reality per the results of the actual prevalence as evidenced by patient self-reported use.
Chart Review to Determine CAM Use Documentation Rate
A random selection of 100 patients notes were examined from the cardiology clinic records via a retrospective chart review to determine the documentation rate of CAM usage in order to compare this percentage against the self-reported use as determined by the computerized patient interview.
Results
The recruitment rate proved to be extremely positive at 85% of the 47 patients approach, for a total of 40 participants. It is likely that this high rate is attributed to a minimally intrusive and carefully timed patient approach. Because the patient is waiting for their physician and also are ensured that their visit with the physician takes priority over the study interview process, the patients seemed to have a favorable attitude toward participation. Several patients went beyond that and expressed enthusiasm toward the study as either they or a loved one took a large number of dietary supplements along with their prescription drugs. Those patients expressed interest in a system that would allow them to maintain an up-to-date list of their dietary supplements which would ultimately be paired with their medication lists to detect potentially harmful interactions.
The preliminary findings from the usability study of the computerized patient interview system show the CAM usage rate to be approximately 85%. Unlike the results found in the chart review, 33% of the participants taking dietary supplements were taking at least 1 supplement from the known interactions list. One of those patients was taking 3 supplements from the interactions list and also reported taking 9 prescription drugs. One additional patient was taking 3 supplements from the interactions list, one taking 4, and one taking 5.
The age of the study participants ranged from 18 to 88 with a mean age of 55 years. The time spent searching for online health information seemed to be fairly evenly distributed between never, occasionally, and at least once per week. 79% of the participants had some college or were college graduates. The participants were fairly evenly distributed between male and female (Table 1).
Table 1:
Demographic profile of the 40 patients included in the study
| Age (years) | |
| Min. : 18.00 | |
| Mean : 55 | |
| Max. : 88.00 | |
| Education Level | |
| High School | 7 (18%) |
| Some college/technical school/vocational training | 12 (30%) |
| College graduate | 15 (38%) |
| Time spent searching for online health related information | |
| Never | 10 (25%) |
| Occasionally | 12 (30%) |
| Once/week | 10 (25%) |
| Gender Distribution | |
| Male | 23 (58%) |
| Female | 17 (42%) |
The survey of clinicians and staff showed differing perceptions of CAM usage amongst cardiac patients with the physicians falling below the mid-level providers and MAs in their estimates and with all those surveyed falling significantly below those percentages as discovered through the preliminary findings of the computerized patient interview (Table 2). The range for the perceived use was 10% to 80%.
Table 2:
Perceived CAM Use by Clinicians and Staff
| Role | Average Estimated CAM Usage |
|---|---|
| Physician | 34% |
| Mid-level | 48% |
| Medical Assistant | 52% |
Of the 100 charts reviewed, 9.5% included notes about dietary supplement use, which is well below the usage being reported by the patients during the online interview. Of those 9.5%, only 2 listed a dietary supplement that has been identified as having known and potentially harmful interactions with some cardiac drugs. However, just as in the medications lists, it is not likely that these lists are complete or up to date. The most common supplements listed in the charts included calcium, fish oil, vitamin D, and glucosamine/chondroitin. Some of these particular supplements are often clinician recommended therapies and might not be considered CAM.
Discussion
Although the sample size of these preliminary findings was small, the numbers look very promising from the perspective of patient participation as well as the ability of the patient to use a computerized interview system at almost any age.
The participation rate was 85% with approximately 15% of those participants expressing enthusiasm for the CAM data gathering and interaction detection system.
The limitations of the study include a small sample size of 40 patients. However, this small sample size is only for the usability portion of the study. Subsequent studies that link to the patient’s medication list for medication reconciliation as well as CAM data gathering are planned. In both the chart reviews and patient entered CAM data, it’s difficult to determine what is truly CAM and what is physician recommended. Finally, the validity portion of the study is still underway, so it still remains to be seen how accurate patient entered CAM data is.
Early indications are that it is feasible to ask patients to enter and review their CAM data in their record and it is assumed that this can be extended to include medication reconciliation. It remains to be seen how valid this data is. This will be measured through a return visit where the patient is asked to bring all of their prescription medications as well as their dietary supplements. The data entered during this return visit will be input by the RA, not by the patient.
Various interview workflows were considered and tested. These included approaching patients in the waiting area, as soon as they were roomed, before their time with their mid-level and physician, and after their office visit/before they left the clinic.
The concerns with approaching the patient in the waiting area included either jeopardizing their privacy by interviewing them publicly, or causing concern with or interrupting clinic workflow by pulling them out of the waiting area and into a more private setting. This would cause delays and frustrations to the front office staff by requiring that they come to the interview room to retrieve the patient, especially during high traffic periods.
Another workflow considered was to either have the MA or mid-level recruit for us as they either roomed or examined the patient. What we discovered was that as supportive and well-intentioned as the staff were, they rarely remembered to do this as it is not part of their normal workflow or daily responsibilities. In light of this, the recruitment rate was approximately 3 patients per week.
As far as approaching the patient at the end of their appointment, although not tested, there is little doubt that the recruitment rate would also be low with this method. By the time they waited in the reception area, in the examination room, and were visited by multiple clinicians and support staff such as MAs, mid-levels, physicians, and phlebotomists, they are unlikely to be willing to extend their visit to talk to students and participate in a study.
Careful attention was paid to ensure that the clinic workflow was not affected at any level. Each step in the clinic workflow was carefully studied to determine the optimal time to insert the patient interview with no interruption. This careful analysis and choice of timing is credited to both maximum staff support of the study and extremely high participation rates. 90% of the time, the RA had completed the interview and left the room before the physician entered. When this was not the case, the interview was completed as soon as the physician stepped out of the room.
The pre-study phase proved to be very helpful in identifying usability issues in the UI and once those were addressed, the feasibility study was much more successful. Only minor UI issues were uncovered, with the exception of unintended behaviors from the iPad such as entering cut/paste mode and magnification mode. Both of these behaviors were most often encountered on the free-form data entry screen while the user was trying to click into and begin data entry. They then became frustrated and did not know how to get out of that mode, or even what mode they were in. Because of these unintended behaviors, we will be most likely not be utilizing the iPad in the next phase of the study. We will instead look into one of the many kiosk options available today.
Future work in the this area will include the review of the medication list for the sake of medication reconciliation, a validity study to ensure not only that the patient would be willing to enter or review this data, but also that they can do so with a reasonable level of accuracy. Finally, a clinical decision support system will be built to detect the known interactions between prescription drugs and dietary supplements as well as the scientific evidence of and severity of the interaction. That severity will be used to determine whether an alert will be generated. However, a physician note can be generated in the patients record to alert both the patient and the clinician to the potential interaction at any severity.
The validity portion of the study will involve either an in-person interview or over the phone where the patient has the supplement bottles in front them. They will be asked to read each label including manufacturer and full product name. This commercial product information can then be used to retrieve the component breakdown from the NMCD. This supplement list is stored in a different database table from the original list and compared against what the patient entered from memory in the clinic. A check box could also be included here to indicate whether this is physician recommended. A text field could also be included to gather information from the patient as to why they take and feel each supplement is helpful to them. This data could be compared against NMCD and literature data on efficacy.
These preliminary findings show the prevalence of CAM usage to be significantly higher than indicated in the literature. One reason for this could be the location of the study. Utah is major producer of CAM products such as dietary supplements, essential oils, etc. Consequently, Utahns might use these products at a higher rate than in other parts of the country. The prevalence could also be higher due to the clinic from which the data was gathered. CAM usage tends to be higher amongst the chronically ill such as those interviewed in the cardiovascular clinic.
Conclusion
It is feasible to involve the patient in the maintenance of their CAM data in their medical record. The timing of the request is important to ensure that they agree to review their records and to ensure that they do not abandon the process before they have made all the necessary updates, thereby decreasing validity. Patients expect delays upon check in to the clinic and after being roomed, so these provide excellent opportunities for such requests.
A simplified UI and touch screen also proved to be critical to the usability of such a tool across all patient demographics. Some options still need to be weighed and evaluated such as a kiosk option in the waiting room as well as the use of the iPad due to some fairly consistent problems experienced by the patients.
The paper increases awareness of the importance of including this information as part of a patient’s medication record. Information on CAM in the patient’s record (chart) is important to contribute to overall information that considers patient safety.
References
- 1.Desylvia D, Stuber M, Fung CC, Bazargan-Hejazi S, Cooper E. The knowledge, attitudes and usage of complementary and alternative medicine of medical students. Evid Based Complement Alternat Med. 2008 Dec 10; doi: 10.1093/ecam/nen075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saxe GA, Madlensky L, Kealey S, Wu DP, Freeman KL, Pierce JP. Disclosure to physicians of cam use by breast cancer patients: Findings from the women’s healthy eating and living study. Integr Cancer Ther. 2008 Sep;7(3):122–9. doi: 10.1177/1534735408323081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krasuski RA, Michaelis K, Eckart RE. The cardiovascular patient’s perceptions of complementary and alternative medicine. Clin Cardiol. 2006 Apr;29(4):161–4. doi: 10.1002/clc.4960290407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta DH, Gardiner PM, Phillips RS, McCarthy EP. Herbal and dietary supplement disclosure to health care providers by individuals with chronic conditions. J Altern Complement Med. 2008 Dec;14(10):1263–9. doi: 10.1089/acm.2008.0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the united states. Prevalence, costs, and patterns of use. N Engl J Med. 1993 Jan 28;328(4):246–52. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 6.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006 Sep 1;98(5):673–80. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 7.Wood MJ, Stewart RL, Merry H, Johnstone DE, Cox JL. Use of complementary and alternative medical therapies in patients with cardiovascular disease. Am Heart J. 2003 May;145(5):806–12. doi: 10.1016/S0002-8703(03)00084-X. [DOI] [PubMed] [Google Scholar]
- 8.Chagan L, Bernstein D, Cheng JW, Kirschenbaum HL, Rozenfeld V, Caliendo GC, et al. Use of biological based therapy in patients with cardiovascular diseases in a university-hospital in new york city. BMC Complement Altern Med. 2005;5:4. doi: 10.1186/1472-6882-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson DL, Shane-McWhorter L, Crouch BI, Andersen SJ. Prevalence and patterns of alternative medication use in a university hospital outpatient clinic serving rheumatology and geriatric patients. Pharmacotherapy. 2000 Aug;20(8):958–66. doi: 10.1592/phco.20.11.958.35257. [DOI] [PubMed] [Google Scholar]
- 10.Bailey RL, Gahche JJ, Lentino CV, Dwyer JT, Engel JS, Thomas PR, et al. Dietary supplement use in the united states, 2003–2006. Journal of Nutrition. 2010;141(2):261–6. doi: 10.3945/jn.110.133025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kennedy J, Wang CC, Wu CH. Patient disclosure about herb and supplement use among adults in the us. Evid Based Complement Alternat Med. 2008 Dec;5(4):451–6. doi: 10.1093/ecam/nem045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shelley BM, Sussman AL, Williams RL, Segal AR, Crabtree BF. ‘They don’t ask me so i don’t tell them’: Patient-clinician communication about traditional, complementary, and alternative medicine. Ann Fam Med. 2009 Mar-Apr;7(2):139–47. doi: 10.1370/afm.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol. 2010 Feb 9;55(6):515–25. doi: 10.1016/j.jacc.2009.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clement YN, Williams AF, Khan K, Bernard T, Bhola S, Fortune M, et al. A gap between acceptance and knowledge of herbal remedies by physicians: The need for educational intervention. BMC Complement Altern Med. 2005;5:20. doi: 10.1186/1472-6882-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]